Abstract
Purpose
The purpose of this study was to investigate the prevalence and characteristics of glaucoma in the population of the rural Korean town, Sangju.
Methods
Residents of Sangju aged greater than 50 years old were included in this study. Participants completed an interview examining their medical and ophthalmic history Information was collected on the participants' uncorrected and best corrected vision scores, slit lamp examination results, angle width measurements using the Van Herick technique, gonioscopy if the angle width was less than 1 / 4 angle, intraocular pressure (IOP) assessed with the Goldmann applanation tonometry, optic disc examination results, and a visual field test results using frequency-doubling perimetry in cases in which glaucoma was suspected. Glaucoma was diagnosed according to the criteria described by the International Society for Geographic and Epidemiological Ophthalmology.
Results
1,118 residents aged greater than 50 years were examined initially from a population of 2,984 people. Of these, 671 subjects (60%) participated in this study. The prevalence of glaucoma was determined to be 3.4% (95% confidence interval [CI], 2.1-4.8). Open-angle glaucoma with low IOP was determined to be the most common form with a prevalence rate as high as 2.5% (95% CI, 1.8-3.7). Additionally, primary angle closure glaucoma was determined to have a prevalence rate of 0.3% (95% CI, 0.1-0.9). Open-angle glaucoma with low IOP accounted for 94.4% of the open-angle glaucoma cases.
Conclusions
The prevalence of glaucoma among the population of rural Sangju was 3.4%, and open-angle glaucoma with low IOP was the most common form accounting for 94.4% of the total number of cases.
Keywords: Epidemiology, Glaucoma, Open angle glaucoma, Prevalence
Glaucoma is the second most prevalent cause of vision loss worldwide. Specifically, it has been estimated that 60.5 million people will be diagnosed with glaucoma by 2010 [1]. However, research has shown that the prevalence of glaucoma varies according to both geographical region and race [2]. Knowledge of the distributions of the specific types of glaucoma and the characteristics of each type will be aid in the understanding of glaucoma among particular races and countries, as well as in assigning a diagnosis and treatment plan.
Africa, Japan, and Latin America have been shown to have higher rates of primary open angle glaucoma (POAG) than patients in China or India [1]. Moreover, a study by Tajimi reported that patients with POAG and intraocular pressure (IOP) under 21 mmHg were more common than other types of patients in Japan [3].
Although prevalence rates of glaucoma in Korea have been reported to range from 2.04% to 4.7% [4-8], previous studies have been associated with methodological limitations. Specifically, the diagnostic criteria and methods were not clearly described in these studies, and international standards for diagnosis were not used. More importantly, previous studies have been conducted in hospitals or health centers, and a population-based epidemiological study of glaucoma has not been conducted in Korea.
For this study, a population-based study of glaucoma prevalence in Oeso-myeon, Sangju in Korea was conducted. The International Society of Geographical and Epidemiological Ophthalmology (ISGEO) criteria were used [9]. The ISGEO is a widely accepted scheme for reporting the prevalence of glaucoma in epidemiologic research.
Materials and Methods
Sampling of subjects
This study used a population-based prevalence survey to examine the rates of glaucoma among residents of Oeso-myeon, Sangju city, an inland, rural, agricultural area of 88.19 km2 located in central South Korea who were aged greater than 50 years. This city was selected for the survey because of its stable, older population and its socioeconomic profile which is representative of rural areas of South Korea.
Residents aged 50 years or older who had lived in the city for more than 1 year were selected for participation in the study. Using the Household Resident Register record kept by the district government, households with eligible participants were identified according to address, name of the head of the household, name of the potential participant, and the potential participant's date of birth. Potential participants were invited to the base clinic to complete a survey and ocular examinations. Informed consent was obtained after providing the potential participant with a description of the purpose of the study. The study was carried out in accordance with the guidelines set forth by the World Medical Association's Declaration of Helsinki and the municipal laws of Sangju city.
Survey and ocular examinations
A site was developed in the community for the examinations which was less than thirty minutes walking distance for most potential participants. Participants' identities were verified using government issued identity cards with an official photograph. A standard questionnaire was administered by a trained interviewer in order to obtain detailed information regarding the participant's family history of glaucoma and ocular disease, surgical history, general medical history, income, and education history.
Visual acuity was measured using the Hahn Chun Suk eye chart as well as the Korean version of the Snellen chart with a standard illumination box at 4 meters. For those participants who presented with visual acuity score of less than 0.6, corrected visual acuity was measured using auto-refraction. Refraction was measured with a handheld auto-refractor (ARK-30; Nidek Corp., Gamagori, Japan). For those participants with corrected visual acuity of less than 0.8, the best corrected visual acuity was measured using the necessary subjective refinement.
All ophthalmologic procedures were performed by an experienced ophthalmologist. Intraocular pressure was measured using Goldmann applanation tonometry under local anesthesia resulting in two independent measurements for each eye which were obtained from right to left. A slit lamp examination was completed to identify abnormalities of the anterior segment, including iris changes and lens opacities. Gonioscopy was performed using a Sussman 4-mirror lens when the angle width measured by the Van Herick technique was less than ¼ the angle depth. The Spaeth grading system was used. The optic disc was determined using a +90 diopters (D) lens at 16 × magnification without the use of pupil dilatation. The vertical cup-to-disc ratio (VCDR) was used as the index for structural glaucomatous change. If the stereo view was not satisfactory due to the opacity of the lens or due to restrictions of pupil size, then the pupil was dilated using 0.5% tropicamide and 0.5% phenylephrine hydrochloride, and the optic disc was examined with an indirect ophthalmoscope using a +20 D lens.
Refractive correction at near or full threshold perimetry (N-30 strategy) was performed if the VCDR was larger than 0.6 or the VCDR asymmetry was larger than 0.2 or IOP ≥ 21 mm Hg, using frequency doubling technology (FDT; Zeiss Humphery System, Dublin, CA, USA). These tests were considered reliable when fixation loss was less than 50 percent and the false-positive and false-negative error rates were under 50 percent. Abnormal examination results were defined as the presence of 2 or more points having a p < 5% on the pattern deviation plot [10-11]. All abnormalities were then confirmed using a subsequent test.
Diagnosis of glaucoma
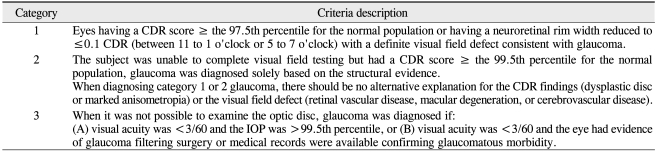
Glaucoma was diagnosed according to the criteria described by ISGEO (Table 1). In this study, a cup disc ratio (CDR) equal to or greater than the 97.5 percentile was roughly 0.6, and a CDR equal to or greater than the 99.5 percentile was roughly 0.9.
Table 1.
Diagnostic criteria for glaucoma by International Society of Geographical and Epidemiological Ophthalmology
CDR = cup disc ratio; IOP = intraocular pressure.
All participants were classified into the following groups: normal, POAG with low IOP (IOP ≤ 21 mmHg), POAG with high IOP (IOP > 21 mmHg), primary angle closure glaucoma (PACG), and secondary glaucoma.
POAG was defined as glaucoma associated with open angles. POAG with low IOP was defined as open angle glaucoma with an IOP of 21 mmHg or less while not taking medication for the treatment of glaucoma.
A diagnosis of PACG was assigned on the basis of these criteria as well as the use of gonioscopically occludable angles (invisible trabecular meshwork ≥270° without indentation or peripheral anterior synechiae).
Eyes with a history of significant ocular trauma, iridocyclitis, or the presence of new vessels on the iris or chamber angle or other ocular findings which may cause glaucomatous optic discs or visual field changes were classified as secondary glaucoma.
Data analysis
All information was maintained in accordance with the protection of the participants' privacy at Severance Hospital, Yonsei University College of Medicine. The prevalence of the different forms of glaucoma and their 95% confidence intervals were calculated using SAS ver. 9.1 (SAS Inc., Cary, NC, USA). The prevalence of glaucoma and 95% confidence interval (CI) were calculated individually for each age group.
Results
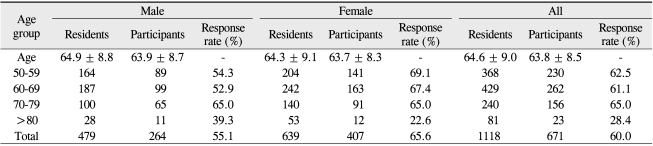
Among the identified potential participants older than 50 years, 1,118 were eligible to participate in this study. Of these, 671 (264 males and 407 females) participated in the examination, which is an overall response rate of 60.0%. Table 2 reports the age and sex distributions for the town's residents and the participants of this study. The sex ratio of participants was 1:1.54 (male:female). Female participation rates were greater in all age groups with the exception of the, group with an age of older than 80 years.
Table 2.
Response rates for this study according to age and sex
The female age group with the highest participation rate (69.1%) was the group aged 50 to 59 years. The male group with the highest participation rate (65.0%) was the group between 70 and 79 years old. The group over 80 years old had the lowest participation rate for both males and females.
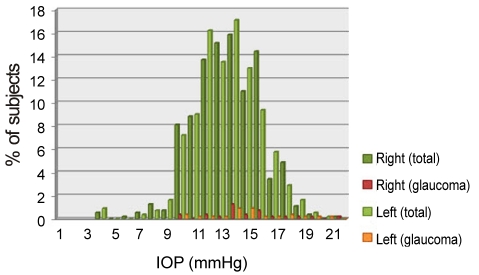
Fig. 1 shows the distribution of intraocular pressure for all participants and glaucoma patients. There were no differences between levels of the IOP in the right and left eyes or between the age groups. The mean IOP for the full sample was 13.5 ± 2.9 mmHg, and the IOP for the participants in the 99.5th percentile was 19 mmHg.
Fig. 1.
Distribution of intraocular pressure (IOP) (total no. of subjects = 671; no. of subjects with glaucoma = 23).
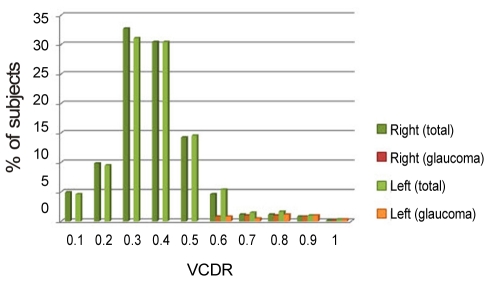
Fig. 2 shows the distribution of the vertical CDR for all participants and glaucoma patients. The 97.5th percentile and 99.5th percentile were 0.6 and 0.9, respectively; thus, these values were applied to the glaucoma diagnostic categories 1 and 2, respectively.
Fig. 2.
Distribution of vertical cup-to-disc ratio (VCDR) (total no. of subjects = 671; no. of subjects with glaucoma = 23).
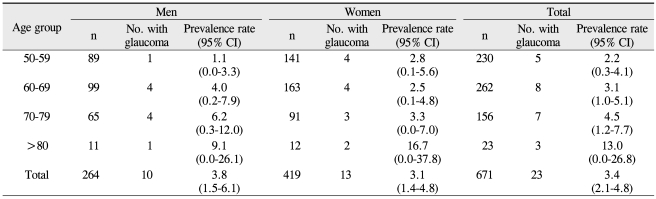
Table 3 reports the prevalence of glaucoma based on age and sex. As the age increased, there the prevalence of glaucoma also increased at the trend-level of significance. Additionally, there was no statistically significant difference in the prevalence of glaucoma for men and women.
Table 3.
Prevalence of glaucoma according to age and sex
CI = confidence interval.
23 of the participants received a diagnosis of glaucoma with of those 15 participants being placed in category 1 and 8 participants being placed in category 2. Therefore, the overall prevalence of glaucoma was determined to be 3.4%. The prevalence of glaucoma increased from 2.2% in the group aged 50 to 59 years to 3.1% in the group aged 60 to 69 years. The prevalence rate then increased to 4.5% for the group aged 70 to 79 years, and then, increased to 13.0% in the group aged 80 years and older. Among females, the prevalence rates of those participants in their 50's and 60's were similar, and then, the prevalence rates increased in association with each advancing decade of life.
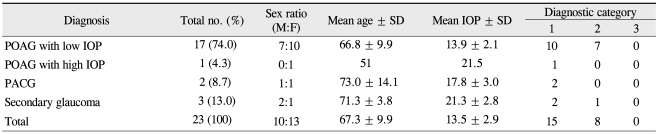
Table 4 reports the ratio of each type of glaucoma to the total of all the forms of glaucoma. Open angle glaucoma (OAG) was the most common form at 74.0% of the total, and the POAG with low IOP group included 94.4% of the total number of patients in the OAG group.
Table 4.
Prevalence of glaucoma according to mechanism
CI = confidence interval; POAG = primary open angle glaucoma; IOP = intraocular pressure; PACG = primary angle closure glaucoma.
The mean intraocular pressure for the normal population was 13.4 ± 2.5 mmHg, and it was 13.9 ± 2.1 mmHg for patients with POAG with low IOP. In this study, there was only one person with POAG with high IOP. This participant had an IOP of 22 and 21 mmHg. Intraocular pressure according to the type of glaucoma is summarized in Table 5.
Table 5.
Mechanisms and characteristics associated with glaucoma
IOP = intraocular pressure; POAG = primary open angle glaucoma; PAGC = primary angle closure glaucoma.
Discussion
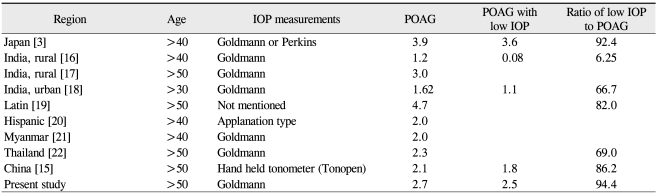
This is the first population-based epidemiological report regarding the prevalence of glaucoma in Korea. The glaucoma prevalence was determined to be 3.4% of the population aged 50 years and older, which is similar to the prevalence reported in other East Asian countries [12-15]. The prevalence of POAG with low IOP in the study outlined by Tajimi was 92.4%, and this prevalence was 94.4% in this study [3]. This result differs from results based on Chinese, Indonesia, and Mongolian data, which described a higher prevalence rate of POAG with high IOP [12-15]. The similar ethnic and cultural backgrounds of Korea and Japan may contribute to the similarities in prevalence of glaucoma in the two countries (Table 6) [3,13-20].
Table 6.
Prevalence of primary open angle glaucoma (POAG) and POAG with low intraocular pressure (IOP)
Data are presented as percentage.
The average IOP for all participants in this study was 13.5 ± 2.9 mmHg, which is lower than that observed in most other surveys (12.5 to 18.7 mmHg). Therefore, the low mean IOP likely plays a role in the higher prevalence of POAG with low IOP observed in this study. However, the low average IOP in the POAG participants and the high prevalence of POAG with low IOP, do not necessarily mean that the IOP value was not related to POAG.
The prevalence of PACG has been reported to range from 0.6% to 1.4% in other Asian countries [12-13,16,23-25]. The prevalence of angle closure glaucoma (0.46%) was significantly lower than that observed in other East Asian or Japanese studies. However, this may be attributable to the examination methods. The results of this stuy may have been underestimated as only the Van Herick method was used in the screening of ACG, and this screening only included the cases which met criteria for ISGEO.
Although there have been several reports on the prevalence and composition of glaucoma in Korea [4-8], many of these reports have been hospital or health center-based studies. In a hospital-based study, the overall incidence of glaucoma was determined to be 4.7% of new patients visiting the ophthalmology outpatient clinic, and POAG with high IOP was determined to be the most common form of glaucoma, accounting for 37.7% of all cases of glaucoma [5]. In contrast, recent studies by Lee et al. [7] and Choe and Hong [8] found that normal-tension glaucoma (POAG with low IOP) was the most common type of glaucoma in Korean popykatuibs, based on the results of two health center studies. According to these studies, the prevalence rates of all types of glaucoma were 2.67% [7] and 2.04% [8], with OAG with low IOP comprising 2.04% [7] and 1.71% [8], respectively.
The prevalence of glaucoma is known to increase with age, and this was also shown in the data of this study. The average age of the participants in this study was 64.1 years, while the average age of the population over 50 years old in South Korea was 62.6 years at the end of 1998 [26]. The older average age of the residents in this rural area, compared with those in urban areas and the entire nation, may have increased the prevalence of glaucoma observed in the present study.
The overall response rate in this study was 60.0%. Individuals aged 80 years or more showed an especially low participation rate (26.4%), which may reflect the limited mobility and poorer physical health observed in this population.
There are several methodological limitations associated with this study. In particular, random sampling was not performed and the participation rate was relatively low, about 60.0%. Additionally, visual field testing was not performed on all subjects as the glaucoma grading scheme required an enlarged VCDR for individuals to be classified as having glaucoma. This streamlined the logistics of examining the cohort. However, it is possible that some participants experiencing subtle optic nerve changes may have been missed due to visual fields which would not have been examined in these individuals. The estimate of the prevalence of glaucoma, therefore, may be somewhat biased. Furthermore, visual field measurements were performed using a full threshold of N-30 of the frequency doubling test rather than Humphrey visual field analyzer. The FDT perimetry was used instead of the Humphrey visual field because the FDT perimetry can be performed easily in a few minutes with a screening method, and the device is portable and relatively inexpensive. There are many other epidemiologic studies using only the FDT, which have reported that the results of the FDT were almost identical to that of the Humphery exam [27,28].
Despite the limitations, this is the first population-based epidemiological study in a rural area of South Korea, reporting that POAG with low IOP is the most common form of glaucoma. These results imply that there are unique characteristics of glaucoma in Korea and Japan and that specific race-based factors may contribute to the pathogenesis of glaucoma.
In conclusion, the prevalence of glaucoma in the rural Korean area was 3.4% and the prevalence of POAG with low IOP was 2.8%, which was similar to that observed in Japanese studies. The prevalence of PACG in Korea was relatively lower than those of other Asian countries. A large-scale epidemiologic study, the Nam-il study, is being conducted in Korea, which will allow for validation of this study and its findings.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudnicka AR, Mt-Isa S, Owen CG, et al. Variations in primary open-angle glaucoma prevalence by age, gender, and race: a Bayesian meta-analysis. Invest Ophthalmol Vis Sci. 2006;47:4254–4261. doi: 10.1167/iovs.06-0299. [DOI] [PubMed] [Google Scholar]
- 3.Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111:1641–1648. doi: 10.1016/j.ophtha.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 4.Hong C, Joo JH, Shin KH, Song KY. Clinical study of Korean glaucomatous patients. Korean J Ophthalmol. 1987;1:41–46. doi: 10.3341/kjo.1987.1.1.41. [DOI] [PubMed] [Google Scholar]
- 5.Shin SG, Ahn JH, Rho SH. A clinical analysis on 456 cases of glaucoma among outpatients during 5 years. J Korean Ophthalmol Soc. 1987;28:1021–1026. [Google Scholar]
- 6.Lee CK, Cho YJ, Hong YJ. Distribution of glaucoma outpatients. J Korean Ophthalmol Soc. 1995;36:1020–1027. [Google Scholar]
- 7.Lee JB, Cho YS, Choe YJ, Hong YJ. The prevalence of glanucoma in Korean adults. J Korean Ophthalmol Soc. 1993;34:65–69. [Google Scholar]
- 8.Choe YJ, Hong YJ. The prevalence of glaucoma in Korean careermen. J Korean Ophthalmol Soc. 1993;34:153–158. [Google Scholar]
- 9.Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–242. doi: 10.1136/bjo.86.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medeiros FA, Sample PA, Weinreb RN. Frequency doubling technology perimetry abnormalities as predictors of glaucomatous visual field loss. Am J Ophthalmol. 2004;137:863–871. doi: 10.1016/j.ajo.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Fogagnolo P, Mazzolani F, Rossetti L, Orzalesi N. Detecting glaucoma with frequency-doubling technology perimetry: a comparison between N-30 and C-20 screening programs. J Glaucoma. 2005;14:485–491. doi: 10.1097/01.ijg.0000184833.85912.2a. [DOI] [PubMed] [Google Scholar]
- 12.Foster PJ, Baasanhu J, Alsbirk PH, et al. Glaucoma in Mongolia. A population-based survey in Hövsgöl province, northern Mongolia. Arch Ophthalmol. 1996;114:1235–1241. doi: 10.1001/archopht.1996.01100140435011. [DOI] [PubMed] [Google Scholar]
- 13.Foster PJ, Oen FT, Machin D, et al. The prevalence of glaucoma in Chinese residents of Singapore: a cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol. 2000;118:1105–1111. doi: 10.1001/archopht.118.8.1105. [DOI] [PubMed] [Google Scholar]
- 14.Congdon NG, Quigley HA, Hung PT, et al. Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmol Scand. 1996;74:113–119. doi: 10.1111/j.1600-0420.1996.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 15.He M, Foster PJ, Ge J, et al. Prevalence and clinical characteristics of glaucoma in adult Chinese: a population-based study in Liwan District, Guangzhou. Invest Ophthalmol Vis Sci. 2006;47:2782–2788. doi: 10.1167/iovs.06-0051. [DOI] [PubMed] [Google Scholar]
- 16.Ramakrishnan R, Nirmalan PK, Krishnadas R, et al. Glaucoma in a rural population of southern India: the Aravind comprehensive eye survey. Ophthalmology. 2003;110:1484–1490. doi: 10.1016/S0161-6420(03)00564-5. [DOI] [PubMed] [Google Scholar]
- 17.Raychaudhuri A, Lahiri SK, Bandyopadhyay M, et al. A population based survey of the prevalence and types of glaucoma in rural West Bengal: the West Bengal Glaucoma Study. Br J Ophthalmol. 2005;89:1559–1564. doi: 10.1136/bjo.2005.074948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dandona L, Dandona R, Srinivas M, et al. Open-angle glaucoma in an urban population in southern India: the Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1702–1709. doi: 10.1016/s0161-6420(00)00275-x. [DOI] [PubMed] [Google Scholar]
- 19.Varma R, Ying-Lai M, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1439–1448. doi: 10.1016/j.ophtha.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Quigley HA, West SK, Rodriguez J, et al. The prevalence of glaucoma in a population-based study of Hispanic subjects: Proyecto VER. Arch Ophthalmol. 2001;119:1819–1826. doi: 10.1001/archopht.119.12.1819. [DOI] [PubMed] [Google Scholar]
- 21.Casson RJ, Newland HS, Muecke J, et al. Prevalence of glaucoma in rural Myanmar: the Meiktila Eye Study. Br J Ophthalmol. 2007;91:710–714. doi: 10.1136/bjo.2006.107573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bourne RR, Sukudom P, Foster PJ, et al. Prevalence of glaucoma in Thailand: a population based survey in Rom Klao District, Bangkok. Br J Ophthalmol. 2003;87:1069–1074. doi: 10.1136/bjo.87.9.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamamoto T, Iwase A, Araie M, et al. The Tajimi Study report 2: prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology. 2005;112:1661–1669. doi: 10.1016/j.ophtha.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Dandona L, Dandona R, Mandal P, et al. Angle-closure glaucoma in an urban population in southern India. The Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1710–1716. doi: 10.1016/s0161-6420(00)00274-8. [DOI] [PubMed] [Google Scholar]
- 25.Vijaya L, George R, Arvind H, et al. Prevalence of angle-closure disease in a rural southern Indian population. Arch Ophthalmol. 2006;124:403–409. doi: 10.1001/archopht.124.3.403. [DOI] [PubMed] [Google Scholar]
- 26.Korean National Statistical Office Population Census Data. Available from http://kosis.kr/abroad/abroad_01List.jsp.
- 27.Anderson AJ, Johnson CA. Frequency-doubling technology perimetry and optical defocus. Invest Ophthalmol Vis Sci. 2003;44:4147–4152. doi: 10.1167/iovs.02-1076. [DOI] [PubMed] [Google Scholar]
- 28.Iwase A, Tomidokoro A, Araie M, et al. Performance of frequency-doubling technology perimetry in a population-based prevalence survey of glaucoma: the Tajimi study. Ophthalmology. 2007;114:27–32. doi: 10.1016/j.ophtha.2006.06.041. [DOI] [PubMed] [Google Scholar]