Abstract
In cases of extropia with an exodeviation angle over 50 prism diopter (PD), a 3- or 4-muscle surgery is a rational option. But, in patients with sensory exotropia, there is usually a strong preference for a monocular procedure to avoid surgery on the single seeing eye. Thus, we confined surgery to visually poor eyes, and performed a medial rectus muscle resection with a mean of 10.3 mm (range, 9-11 mm) and a lateral rectus muscle recession with a mean of 12.8 mm (range, 10-14 mm) in 4 adult sensory exotropia patients who had a mean deviation of 82.3 PD (range, 75-90 PD). The mean postoperative angle of exodeviation was 2.0 PD (range, ortho-8 PD). The limitation on abduction was not disfiguring. Other expected disfigurements, such as narrowing of the palpebral fissure or enophthalmos, were not conspicuous. The mean follow-up period was 4.5 months (range, 3-7 months). In large-angle sensory exotropia, instead of additive surgery on the seeing eye, supermaximal medial rectus resection and lateral rectus recession only on the visually poor eye is a clinically feasible surgical option.
Keywords: Large sensory exotropia, Recession and resection, Supermaximal
Sensory exotropia is unilateral divergent misalignment of the eyes, resulting in loss of vision or longstanding poor vision in an eye. The angles are characteristically large, ranging from 30 to 100 prism diopters (PD) and increases gradually over time, as long as the cause of visual deficit remains active [1].
In exodeviation cases with an angle over 50 PD, most strabismic surgeons tend to chose three- or four-muscle surgery, instead of an excessive amount of recession or resections in fear of causing several disfigurements [2]. When more than a 6-mm medial rectus resection is performed, significant resistance to abduction, enophthalmos, and palpebral fissure narrowing can occur. A lateral rectus recession exceeding 7 mm to 8 mm is also said to reduce abduction significantly [3].
In 1973, Rayner and Jampolsky [4] published an article on managing large-angle amblyopic exotropia, in which they advocated the use of large medial rectus resection and maximum lateral rectus recession on the amblyopic eye, thus confining surgery only to the exotropic eye. They even assert that the supposed disadvantage of deficient abduction is converted into an advantage for the prevention of extropia recurrence. Of their 22 patients, 6 patients underwent medial rectus resections of more than 9 mm, while the amount of lateral rectus recession was 7 mm to 8 mm [4]. But they did not mention how disfiguring their results were, so we are unable to estimate the trade-offs between confining recession-resection surgery to one eye and bilateral 3- or 4-muscle surgery.
Here, we show our cosmetically acceptable results from 9 mm or greater medial rectus muscle resection and 10mm or greater lateral rectus muscle recession in large-angle sensory exotropia, as demonstrated by preoperative and postoperative photographs.
Case Reports
Three male patients and one female patient with sensory exotropia over 75 PD were included in this report. None of the patients had other causes of exotropia such as third nerve palsy, any restrictive cause, orbital wall fracture or previous ocular surgery. Their strabismic angles were measured by the Krimsky methods at 30 cm. All patients gave informed consent for unilateral recession and resection surgery. We carefully explained alternative approaches, namely bilateral surgery; and possible outcomes, especially enophthalmos, narrowing of the lid fissure and limitation on abduction. All operations were performed by one surgeon (JHC) under general anesthesia. Limbal incision was the choice for incision in all cases. Lateral rectus recession was performed first. The amount of recession was determined by the maximal possible exposure of the surgical field at the time of surgery. The amount of resection was planned roughly according to the results of Rayner and Jampolsky [4]. Adjustable sutures were placed on resected medial rectus muscle during surgery, but no adjustments were needed in any of the cases. Conjunctival recession was not performed. Digital photographs were taken preoperatively, at low resolution, and postoperatively, at high resolution, on the day of their last visit, except for case 1.
Although limited abduction and excessive adduction in the operated eye were noticeable in all four cases, it was only conspicuous in extreme horizontal gaze positions, as shown in our photographs. None of the patients complained of limitation of abduction, enophthalmos or narrowing of lid fissure, but they were aware of the injection and lump on the nasal conjunctiva in our relatively short follow-up period.
Case 1 was a 46-year-old man. His left sensory exotropia was due to corneal opacity. The strabismic angle was 80 PD in his left eye. A 10 mm left medial rectus muscle resection and 13mm left lateral rectus muscle recession was performed. At 3 months after surgery, there remained no horizontal deviation, but 10 PD left hypertropia (photographs were not taken).
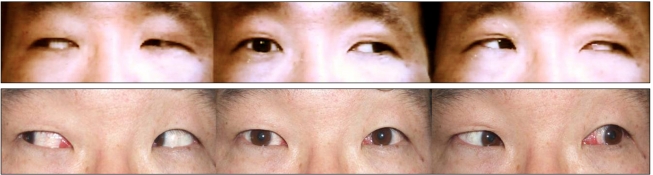
Case 2 was a 51-year-old female whose left vision was lost because of extensive macular degeneration. We measured 75 PD left exotropia preoperatively. Left medial rectus muscle resection 9 mm and left lateral rectus muscle recession 14 mm were performed and the eyes were straight at 5 months after surgery (Fig. 1).
Fig. 1.
Photographs of 51 year-old woman (patient 2) with 75 prism diopter left exotropia before surgery due to macular degeneration of the left eye (upper). Left medial rectus 9 mm resection and left lateral rectus 14 mm recession were performed. No postoperative deviation was detected at 5 months after surgery (lower).
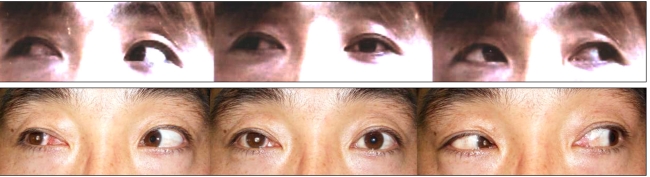
Case 3 was a 33-year-old man with left exotropia of 90 PD. He had optic atrophy in his left eye from previous head trauma. We performed 11 mm resection of the left medial rectus muscle and 14 mm recession of the left lateral rectus muscle. At 7 months after surgery, his alignment was nearly straight (Fig. 2).
Fig. 2.
Photographs of 33 year-old man (patient 3) with 90 prism diopter left exotropia before surgery due to optic atrophy of the left eye (upper). Left medial rectus resection of 11 mm and left lateral rectus recession of 14 mm were performed. Postoperative deviation was nearly straight at 7 months after surgery (lower).
Case 4 was 29 year-old man. A traumatic cataract resulted in vision loss of his right eye. He had 80 PD right exotropia. After performing 11 mm right medial rectus resection and 10 mm right lateral rectus recession, his exodeviation decreased to 8 PD at 3 months after surgery (Fig. 3).
Fig. 3.
Photographs of 29 year-old man (patient 4) with 80 prism diopter right exotropia before surgery due to traumatic cataract on right eye (upper). Right medial rectus resection of 11 mm and right lateral rectus recession of 10 mm were performed. Postoperative deviation was 8 prism diopter right exotropia at 3 months after surgery (lower).
Discussion
When sensory exotropia is present, combined recession-resection operation only on the eye with visual loss is preferred. But, if the deviation angle is too large to be corrected by conventional two-muscle surgery, the surgeon faces a challenge of choosing between additional one- or two-muscle surgery on the seeing eye or doing extra large amount of surgery on the visually poor eye alone leaving the seeing eye intact.
Partitioning the surgical dose over 3 or 4 muscles is a rational option in cases of large exotropia with equal vision in both eyes. If the surgeon plans on unilateral surgery, limitation on abduction will ensue and will cause diplopia in the field of gaze limitation. However, since there is no fusional potential in these patients, Rayner and Jampolsky stress that the surgical procedure should be a 'mechanical' operation, using large resection of the medial rectus as a stay suture to mechanically prevent an exotropic recurrence, while recession of the lateral rectus and conjunctiva releases the restrictive forces. Indeed, they reported 2 cases during a 15-year follow-up with stable results for 22 patients [4]. But even though long stability of alignment is a significant benefit of the surgical procedure, if the overall disfigurements, most probably caused by limited abduction, outweigh the benefit, the surgeon will certainly have to reconsider the procedure. Thus, prior to the surgery, we discussed this possibility with the patients in detail and they all chose unilateral extra large recession-resection, in order to spare their only seeing eye from potential surgical risks.
In contrast to our expectations, as shown in postoperative photographs, the disfigurements were not severe. Limitation on abduction and excessive adduction were certainly noticeable, but only in extreme horizontal gaze positions. Other expected disfigurements, such as narrowing of the palpebral fissure or enophthalmos, were not prominent.
The explanation for such a result is merely speculative in this small number of patients, but, we assume that the long-standing large exotropic position of the eye caused eventual stretching and elongation of the medial rectus. Thus, an extra large resection probably does not cause the usual restriction on abduction that is seen in muscles of relatively normal length.
There is another suggested method that consists of conventional maximum horizontal rectus recession-resection plus weakening of both obliques of the poorly seeing eye, releasing additional sites of contracture. This might circumvent the problem of limited abduction, however, as mentioned in the article, postoperative hypertropia of the deviated eye is the principal disadvantage and the results were 10 PD exotropia and hypertropia of 5 PD at best in their 8 subjects [5]. In conclusion, in large-angle (greater than 75 PD) sensory exotropia, supermaximal medial rectus resection and lateral rectus recession only on the visually poor eye can be a clinically feasible surgical option.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kraft SP. Selected exotropia entities and principles of management. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: principles and surgical techniques. Philadelphia: W. B. Saunders; 1999. pp. 193–199. [Google Scholar]
- 2.Santiago AP, Ing MR, Kushner BJ, Rosenbaum AL. Intermittent exotropia. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: principles and surgical techniques. Philadelphia: W. B. Saunders; 1999. pp. 163–173. [Google Scholar]
- 3.Parks MM, Parker JE. Atlas of strabismus surgery. Philadelphia: Harper & Row; 1983. pp. 6–23. [Google Scholar]
- 4.Rayner JW, Jampolsky A. Management of adult patients with large angle amblyopic exotropia. Ann Ophthalmol. 1973;5:95–99. [PubMed] [Google Scholar]
- 5.Raab EL. Unilateral four-muscle surgery for large-angle exotropia. Ophthalmology. 1979;86:1441–1450. doi: 10.1016/s0161-6420(79)35377-5. [DOI] [PubMed] [Google Scholar]