Abstract
We report a rare case of optic nerve atrophy with severe disc cupping resulting from methanol poisoning. A 30-year-old man presented to the hospital complaining of decreased visual acuity in both eyes a day after drinking alcohol containing methanol. His initial visual acuity allowed for only visualizing hand motion and not corrected in either eye. Initial intraocular pressure was within normal limits in both eyes. Initial fundus examination showed optic disc swelling in both eyes. Four years later, he visited our hospital for an eye evaluation. Visual acuity in both eyes still only allowed for visualizing hand motion. No nystagmus was observed in either eye during the optokinetic nystagmus test, and no waves were found in a visual evoked potential test. No specific change was noted on brain magnetic resonance imaging. On fundus examination, there was disc pallor in both eyes and disc cupping with a high cup/disc (C/D) ratio above 0.9 in the left eye. C/D ratio of the right eye was 0.5. Methanol poisoning may induce glaucomatous disc cupping in the late stage as well as optic atrophy. One possible mechanism of disc cupping is ganglion cell loss due to acute demyelination of the retrobulbar optic nerve. This report is the first photographic evidence of methanol induced optic disc cupping in Korea.
Keywords: Disc cupping, Methanol, Optic atrophy
It is well known that the ingestion of a small amount of methanol can cause visual disturbance and loss of vision in a few hours [1-3]. The mechanism of the visual disturbance is a degenerative change in the optic nerves and a secondary change in the ganglion cell, rather than the production of formic acid, which develops when methanol is metabolized by the retina, inducing direct tissue intoxication to the retina and the optic nerve. After acute methanol poisoning, initially there is an optic neuritis-like change, congestion or swelling of the optic disc, and then optic nerve atrophy with pale discs may develop rapidly or gradually [4-6]. Severe disc cupping, which is found in the last stage of glaucoma, will occur if optic nerve atrophy becomes severe [7]. The mechanism of optic nerve atrophy is unknown, but it is suspected to be caused by progressive demyelination of nerve fibers [8-10]. There are some reports of optic nerve atrophy after methanol poisoning. However, a case of optic nerve atrophy with glaucomatous severe disc cupping has never been reported in Korea [11,12]. We report on one case of optic nerve atrophy with severe disc cupping after methanol poisoning.
Case Report
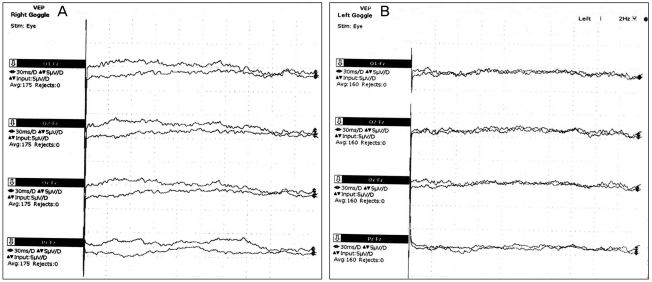
A 30-year-old male visited our hospital for evaluation of both eyes. Four years ago, he experienced visual deterioration after drinking a 20% alcoholic beverage (soju) contaminated with methanol. One day after a single shot of this alcoholic beverage, visual symptoms began to occur, and he presented to a university hospital the next day. His initial visual acuity in both eyes only allowed for visualization of hand motion, and no light reflex was observed. Initial intraocular pressure was 18 mmHg by Goldmann applanation tonometry in both eyes. Depth of the anterior chamber was deep, and all quadrants of angle were opened by gonioscopy in both eyes. There were no signs of uveitis on slit lamp exam. Cup/disc (C/D) ratio of both eyes was about 0.5. There were no specific fundus findings except for edema of both optic discs (Fig. 1). Laboratory studies showed metabolic acidosis and mildly elevated methanol levels in his serum. He had no significant past medical history and no other physical symptoms besides visual deterioration. He had no home medications, including eye drops. After initial conservative treatment, he was lost to follow up. On presentation to our hospital 4 years later, he wanted an evaluation of both eyes. His visual acuity still only allowed for visualization of hand motion in both eyes and was not corrected. No nystagmus was found in either eye on the optokinetic nystagmus test. The intraocular pressure was 15 mmHg by Goldmann applanation tonometry in both eyes. He had not taken any other antiglaucomatous eye drops during the follow-up loss period. The pupils were dilated to approximately 4 mm, and direct light reflex was barely visible in either eye. No new vessels of the iris were observed on slit-lamp examination. Angles were open and no new vessels were observed on the iris or angles by gonioscopic exam in either eye. From red free photographs, diffuse retinal nerve fiber layer defects were observed in both eyes (Fig. 2A and 2B). On fundus exam, optic discs were pale in both eyes, and C/D ratio of the right eye was 0.5. C/D ratio of the left eye was higher than 0.9, which appeared as glaucomatous disc cupping (Fig. 2C and 2D). Filling of fluorescein in the optic disc did not appear in either eye on fluorescein angiography. The thickness of the retinal nerve fiber layer (RNFL) by optical coherence tomography (OCT) was 43.55 µm in the right eye, 43.57 µm in the left eye, which was less than 1% in normal distribution of all sectors around the optic disc (Fig. 3). The left eye was bigger than the right with respect to the cup area, C/D area ratio, horizontal C/D ratio, and vertical C/D ratio in OCT (Fig. 4). To rule out other reasons for the optic atrophy, brain magnetic resonance imaging (MRI) and visual evoked potentials (VEP) were performed. No special signals from the brain MRI were noted, and N75, P100, and N145 wave forms were not observed from VEP (Fig. 5).
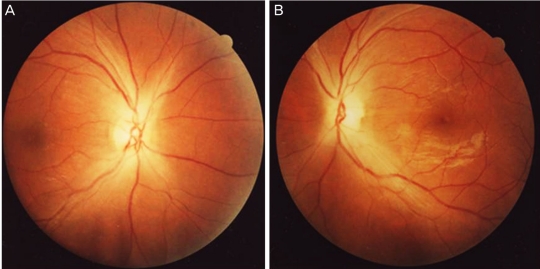
Fig. 1.
A 30-year-old man complained of visual disturbance in both eyes one day after drinking methanol. The fundus photographs demonstrate optic disc edema with blurred disc margins at the initial visit. (A) Right eye, (B) left eye.
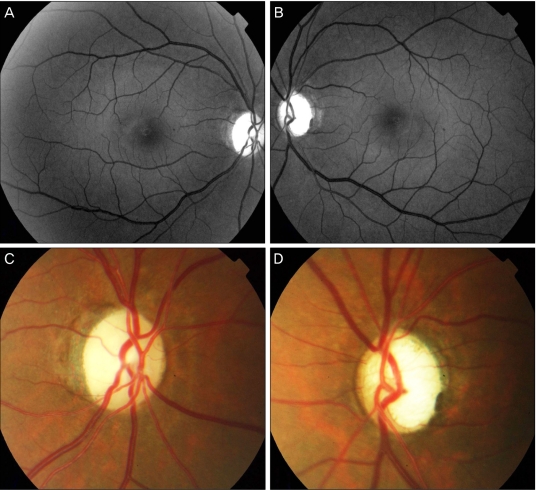
Fig. 2.
The patient presented to our hospital four years after the initial visit for methanol intoxication. (A,B) Red free photographs of both eyes. Red free photographs demonstrate diffuse defects of retinal nerve fiber layers in both eyes. (C) Disc photograph of the right eye, which shows optic nerve atrophy. (D) Disc photograph of the left eye which shows severe disc cupping.
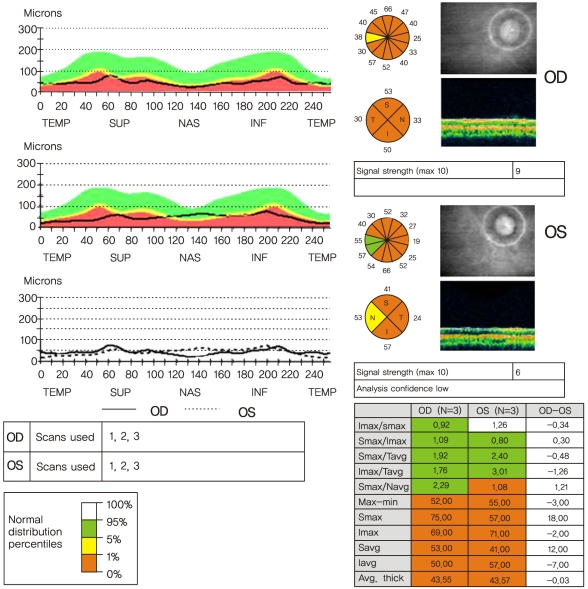
Fig. 3.
Result of retinal nerve fiber layer (RNFL) thickness in optical coherence tomography. RNFL thinkness of both eyes is under one percentile of normal distribution in nearly all sectors. This exam was performed four years after methanol intoxicaion. TEMP=temporal; SUP=superior; NAS=nasal; INF=inferior; Imax=inferior maximum; Smax=superior maximum; Tavg=temporal average; Navg=nasal average; Max-Min = the difference value between maximum and minimum thickness; Savg=superior average; Iavg=inferior average.
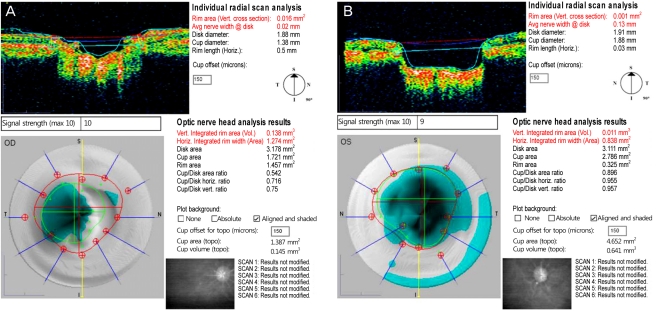
Fig. 4.
Vertical radial scans of optical coherence tomography (OCT) in both optic nerve heads. The cup area, cup/disc area and cup disc ratio of the left eye are larger than those of the right eye in OCT. This exam was performed four years after methanol intoxicaion. (A) Right eye, (B) left eye.
Fig. 5.
Visual evoked potentials (VEP) both eyes. Note that waves of N75, P100 and N145 do not appear in either eye. This exam was performed four years after methanol intoxicaion. (A) Right eye, (B) left eye.
In summary, the patient's intraocular pressures in both eyes were within normal limits on initial and follow up examination. There was no structural problem of the eyeball, including angle closure or new vessels of the anterior segment that could lead to glaucoma. The patient did not have any ophthalmological diseases such as uveitis, retinal vein occlusion, or diabetic retinopathy that could increase intraocular pressure. The C/D ratio of the right eye had been unchanged for four years. If his left eye had glaucoma, the C/D ratio of the right eye may have increased because normal tension or open angle glaucoma usually occurs bilaterally. Based on these findings, we concluded that methanol poisoning could have led to glaucomatous disc cupping in the patient's left eye.
Discussion
Methanol is an organic solvent that is poisonous when ingested. It can cause poisoning by contact with the skin or exposure to respiratory organs. Methanol poisoning causes depression of the central nervous system, metabolic acidosis, and retina/optic nerve cell damage. It causes visual loss and may result in death. Symptoms appear about 12 to 24 hours after exposure. In the early period, there is disc edema and congestion from accumulation of axonal material. Two months after exposure, optic nerve atrophy may appear. Like ethanol, methanol is metabolized by alcohol dehydrogenase. Formaldehyde is produced as a product of dissolution, which converts to formic acid and causes necrosis of retinal ganglionic cells and the optic nerve [13,14].
The formic acid controls cytochrome oxidase and interferes with ATP production from mitochondria, so it causes histologic hypoxia, which induces axonal cell death [15]. Secondarily, the retinal ganglionic cell is destroyed by the degeneration of the axonal region by formic acid. It interferes with transfer of cell signals, causing visual loss by damaging myelin selectively in the retrobulbar area [7,9,10].
The optic nerve atrophy suggests loss of ganglionic cells, which is a secondary change caused by the degenerative demyelination of the retrobulbar optic nerve rather than direct damage to axonal cells of the optic nerve. Although the actual incidence is unknown, optic nerve atrophy from methanol poisoning is relatively common, but cases with disc cupping are rare. The mechanism of disc cupping in methanol poisoning is not yet clear, and unlike optic nerve atrophy from progressive demyelination, this case had rapid demyelination of the retrobulbar optic nerve [7,8]. It is unknown whether the reason for asymmetry of the disc cupping between eyes in our case was related to a difference in the extensive ganglion cell loss due to acute demyelination of the retrobulbar optic nerve. Different mechanisms of optic nerve damage may have occurred because the RNFL thickness of both eyes decreased similarly, though the C/D ratios were different. RNFL loss with normal cup/disc ratios could appear in other optic neuropathies such as traumatic optic neuropathy [16]. The right eye may even progress to severe disc cupping like the left over a long period of time. In addition, it was difficult to completely rule out the possibility that the damage in one eye was a result of glaucoma. Further investigation and long term follow-up are required better understand asymmetric disc cupping after methanol poisoning.
This is the first reported case of optic nerve atrophy with severe disc cupping after methanol poisoning in Korea. Glaucomatous optic disc cupping can appear in other optic neuropathic diseases, and additional studies on the mechanism of disc cupping are needed to investigate this further.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Jacobsen D, McMartin KE. Methanol and ethylene glycol poisonings. Mechanism of toxicity, clinical course, diagnosis and treatment. Med Toxicol. 1986;1:309–334. doi: 10.1007/BF03259846. [DOI] [PubMed] [Google Scholar]
- 2.Benton CD, Jr, Calhoun EP., Jr The ocular effects of methyl alcohol poisoning: report of a catastrophe involving 320 persons. Am J Ophthalmol. 1953;36:1677–1685. doi: 10.1016/0002-9394(53)90002-6. [DOI] [PubMed] [Google Scholar]
- 3.Becker CE. Methanol poisoning. J Emerg Med. 1983;1:51–58. doi: 10.1016/0736-4679(83)90009-4. [DOI] [PubMed] [Google Scholar]
- 4.Fink WH. The ocular pathology of methyl alcohol poisoning. Trans Am Ophthalmol Soc. 1942;40:439–498. [PMC free article] [PubMed] [Google Scholar]
- 5.Baumbach GL, Cancilla PA, Martin-Amat G, et al. Methyl alcohol poisoning. IV. Alterations of the morphological findings of the retina and optic nerve. Arch Ophthalmol. 1977;95:1859–1865. doi: 10.1001/archopht.1977.04450100161023. [DOI] [PubMed] [Google Scholar]
- 6.Roe O. The ganglion cells of the retina in cases of methanol poisoning in human beings and experimental animals. Acta Ophthalmol (Copenh) 1948;26:169–182. [PubMed] [Google Scholar]
- 7.Sharma M, Volpe NJ, Dreyer EB. Methanol-induced optic nerve cupping. Arch Ophthalmol. 1999;117:286. doi: 10.1001/archopht.117.2.286. [DOI] [PubMed] [Google Scholar]
- 8.Stelmach MZ, O'Day J. Partly reversible visual failure with methanol toxicity. Aust N Z J Ophthalmol. 1992;20:57–64. doi: 10.1111/j.1442-9071.1992.tb00705.x. [DOI] [PubMed] [Google Scholar]
- 9.Lindenberg R, Walsh FB, Sacks JG. Neuropathology of vision: an atlas. Philadelphia: Lea and Febiger; 1973. p. 118. [Google Scholar]
- 10.Sharpe JA, Hostovsky M, Bilbao JM, Rewcastle NB. Methanol optic neuropathy: a histopathological study. Neurology. 1982;32:1093–1100. doi: 10.1212/wnl.32.10.1093. [DOI] [PubMed] [Google Scholar]
- 11.Bang JS, Yang HS, Rho SS, Chang YH. A case of toxic amblyopia caused by methanol intoxication. J Korean Ophthalmol Soc. 2007;48:1731–1735. [Google Scholar]
- 12.Kong SM, Hwang BK, Lee HK. 2 Cases of toxic amblyopia caused by acute methanol poisoning. J Korean Ophthalmol Soc. 1982;23:259–263. [Google Scholar]
- 13.Hayreh MS, Hayreh SS, Baumbach GL, et al. Methyl alcohol poisoning III. Ocular toxicity. Arch Ophthalmol. 1977;95:1851–1858. doi: 10.1001/archopht.1977.04450100153022. [DOI] [PubMed] [Google Scholar]
- 14.Rang HP, Dale MM, Ritter JM. Pharmacology. 4th ed. Edinburgh: Churchill Livingstone; 1999. pp. 628–629. [Google Scholar]
- 15.Liesivuori J, Savolainen H. Methanol and formic acid toxicity: biochemical mechanisms. Pharmacol Toxicol. 1991;69:157–163. doi: 10.1111/j.1600-0773.1991.tb01290.x. [DOI] [PubMed] [Google Scholar]
- 16.Medeiros FA, Susanna R., Jr Retinal nerve fiber layer loss after traumatic optic neuropathy detected by scanning laser polarimetry. Arch Ophthalmol. 2001;119:920–921. doi: 10.1001/archopht.119.6.920. [DOI] [PubMed] [Google Scholar]