Abstract
Objectives. The aim of this study was to investigate: (i) the frequency and patterns of radiographic OA (ROA) in the thumb joints; and (ii) associations between thumb ROA and the clinical characteristics of thumb OA in older adults with hand pain or problems.
Methods. Participants were 592 community-dwelling older adults with hand pain or hand problems who attended a research clinic. Hand X-rays were taken and 32 joints were scored for the presence of ROA. The occurrence and pattern of ROA in the hand were examined. Univariable and multivariable associations of thumb pain and clinical assessments (nodes, deformity, enlargement, thenar muscle wasting, grind test, Kapandji index, Finkelstein’s test and thumb extension) with ROA were investigated.
Results. The first CMC and thumb IP joints were the hand joints most frequently affected with ROA. The thumb (thumb IP, first MCP, first CMC, trapezioscaphoid) was the most commonly affected joint group (n = 412). Isolated thumb ROA occurred more frequently than in any other isolated joint group. Multivariable analyses showed that older age, thumb pain, thenar muscle wasting and presence of nodes, deformity or enlargement best determined the presence of thumb ROA.
Conclusion. The first CMC and thumb IP joints were frequently affected with ROA. Prevalence estimates of ROA would be underestimated if these were not scored. One-third of the individuals with thumb ROA did not have involvement of the first CMC joint. The presence of thumb ROA was strongly associated with a combination of older age, thumb pain and clinical features of OA.
Keywords: Epidemiology, Osteoarthritis, Thumb, Radiography, Pain, Clinical features, Clinical assessment
Introduction
OA is a common joint problem affecting older adults in Western populations [1]. Individuals with hand OA report significant pain and disability in their everyday life and consider hand OA to be a serious condition [2]. It has been suggested that OA in the thumb joints may represent a different syndrome of OA in comparison with other hand joints due to different causal mechanisms [3–5]. Previous studies of the thumb have only focused on the joints at the base of thumb: the first CMC and the trapezioscaphoid (TS) joints [6]. However, the joints of the thumb (thumb IP, first MCP, first CMC and TS joints) have been found to group together [7]. There is a paucity of research examining ROA of the whole thumb and associations with clinical characteristics of thumb OA, particularly in community-dwelling older adults.
The objectives of this study were to: (i) describe the frequency and patterns of thumb ROA in a cross-sectional study of community-dwelling older adults with hand pain or hand problems; and (ii) investigate associations of thumb pain, clinical features and clinical assessment results with the presence of thumb ROA.
Methods
Study design and sample
The Clinical Assessment Study of the Hand (CAS-HA) is a prospective observational cohort study. All adults aged ≥50 years registered with two general practices in North Staffordshire were invited to take part in a postal survey. Respondents who indicated that they had experienced hand pain or hand problems in the past 12 months and consented to further contact were invited to attend a research clinic. This consisted of a clinical interview, physical examination, plain radiographs, anthropometric measurements and a brief self-complete questionnaire. Full details of the study design and methods have been previously reported [8]. The study was approved by the North Staffordshire Local Research Ethics Committee and all participants provided written informed consent (Project No. 1430).
Data collection
At the research clinics, participants were assessed by trained occupational therapists and physiotherapists. Thumbs were examined for the presence of deformity and enlargement in the thumb IPs, first MCP and the first CMC joints, nodes in the thumb IP joints and muscle wasting of the thenar eminence. The grind test was conducted to determine whether there was pain in the first CMC joint on movement of the joint under compression [9]. Finkelstein’s test was performed to examine whether pain was located in the dorsal aspect of the wrist [10]. The Kapandji test assessed participants’ ability to oppose the pulp of the thumb to the distal palmar crease [10]. Thumb extension was measured in degrees using a transparent 360° goniometer. Height and weight were measured at the clinic and used to calculate BMI. Reliability of the clinical features and tests has been established [11, 12].
In self-complete questionnaires, participants were asked to report whether they had experienced thumb pain during activity in the previous month, and to indicate on hand drawings the location of any aches or pains lasting a day or longer in the past month.
Radiographs
Posterior–anterior radiographs of the hands and wrists were taken according to a standardized protocol [8]. A single reader (M.M.) graded 16 joints in each hand: DIPs (n = 4), PIPs (n = 4), MCPs (n = 5), thumb IP, first CMC and TS joints for ROA using the Kellgren and Lawrence (K&L) grading system [13]. ROA for a joint was defined as the presence of K&L ≥ 2, and thumb ROA was defined as the presence of K&L ≥ 2 in one or more joints of the thumb (thumb IP, first MCP, first CMC and TS). Inter-observer reliability was found to be very good (unweighted mean κ 0.79, mean percentage agreement 95%).
Data analysis
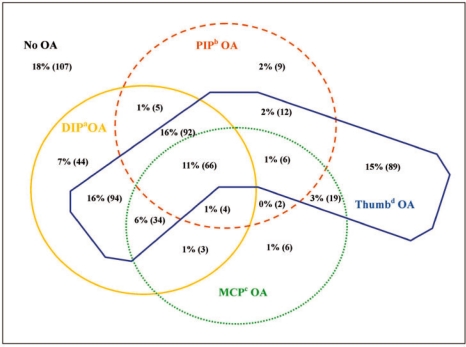
Statistical analysis was performed using SPSS (version 14.0 SPSS, Chicago, IL, USA) and Confidence Interval analysis (version 2.0.0 Statistics with Confidence, second edition, BMJ Books, 2000). The number and percentage of participants with ROA in each joint and joint group were calculated. Combinations of involvement of the thumb joints with other joint groups were examined using a Venn diagram.
Univariable analysis was carried out to determine the magnitude and statistical significance of associations of the presence of ROA in any thumb joint with variables of thumb pain, clinical features and clinical assessment results. Thumb extension was measured as a continuous variable but was dichotomized for analysis using the median value in both thumbs (≥40° and <40°). The analysis was repeated to compare those with and without ROA in the first CMC joint.
Multivariable logistic regression models were constructed using block-entered data: (i) demographic data (age, gender and BMI); (ii) thumb pain (during activity and as indicated on a hand diagram); (iii) clinical features (thenar muscle wasting, presence of nodes, enlargement or deformity in the thumb); and (iv) clinical assessments (grind test, Finkelstein’s test, Kapandji index and thumb extension). Only items with a significance of <0.1 were kept in the models. The amount of explained variance of the models was estimated by calculating Nagelkerke values and the discriminatory ability of the models was assessed by calculating the area under the receiver operating curves (AUCs).
Results
Following exclusion for inflammatory arthritis and absence of hand X-rays, 592 participants were included in the analyses (62% females, mean age 64 years, 90% right handed).
Pattern and occurrence of ROA
The first CMC and the thumb IP were the most frequently affected hand joints (45 and 33%, respectively). The joints of the thumb were the most commonly affected joint group: 70% (n = 412) of participants compared with 58, 33 and 24% for DIPs, PIPs and MCPs, respectively. Bilateral thumb involvement was present in 71% of the participants. There were 314 participants who had first CMC ROA, 61% of whom had bilateral involvement. The Venn diagram (Fig. 1) shows that isolated thumb ROA was more common than ROA in any other isolated joint group.
Fig. 1.
A Venn diagram demonstrating the frequency of ROA in different joint groups of the hand. OA = K&L≥2 in one or more joints in each joint group, aDIP = 2nd–5th DIP joints, bPIP = 2nd–5th PIP joints, cMCP = 2nd–5th MCP joints, dThumb = thumb IP, first MCP, first CMC and FS joints.
Associations with pain, clinical features and tests
Univariable analysis found statistically significant associations for thumb pain during activity, thumb pain as indicated on a hand diagram, the presence of nodes, deformity or enlargement, muscle wasting of the thenar eminence and a positive grind test with the presence of ROA in the right (Table 1) and the left thumb (data not shown). Associations were found to be equally strong when the presence of ROA was based on involvement of the right first CMC (Table 1) and left first CMC joints (data not shown). Therefore, multivariable analysis was only undertaken to examine the wider definition of ROA in any of the thumb joints.
Table 1.
Univariable and multivariable associations between thumb pain, clinical assessments and the presence of ROA in the thumb (right hand)
| Univariable OR (95% CI) Chi-square significance |
Multivariable right thumba ROA |
|||||
|---|---|---|---|---|---|---|
| Outcome | Frequency, % | Right first CMC ROA | Right thumba ROA | βb | P-valuec | OR (95% CI) |
| Age group, years | ||||||
| 50–60 | 35.5 | Reference 1.0 | Reference 1.0 | |||
| 60–70 | 37.3 | 1.6 (1.1, 2.5) | 1.9 (1.3, 2.9) | 0.6 | 0.005 | 1.8 (1.2, 2.6) |
| ≤70 | 27.2 | 3.9 (2.5, 6.0) | 5.4 (3.4, 8.6) | 1.4 | < 0.001 | 4.1 (2.5, 6.7) |
| P < 0.001 | P < 0.001 | Dropped | ||||
| Gender | 61.8 | 1.4 (1.0, 1.9) | 1.5 (1.0, 2.0) | |||
| P = 0.077 | P = 0.030 | |||||
| BMI | ||||||
| <25 | 25.6 | Reference 1.0 | ||||
| 25.0–29.9 | 43.8 | 0.7 (0.5, 1.1) | 0.8 (0.6, 1.3) | Dropped | ||
| ≥30.0 | 30.6 | 0.8 (0.5, 1.3) | 1.1 (0.7, 1.7) | |||
| P = 0.360 | P = 0.354 | |||||
| Thumb pain during activity in the past month | 53.2 | 2.1 (1.5, 2.9) | 2.23 (1.6, 3.2) | 0.6 | 0.001 | 1.8 (1.3, 2.6) |
| P < 0.001 | P < 0.001 | |||||
| Thumb pain in the past month as indicated on a hand diagram | 51.5 | 1.5 (1.0, 2.1) | 1.4 (1.0, 2.0) | Dropped | ||
| P = 0.018 | P = 0.023 | |||||
| The presence of thenar muscle wasting | 20.8 | 3.0 (2.0, 4.6) | 3.1 (2.0, 5.0) | 0.6 | 0.016 | 1.9 (1.1, 3.1) |
| P < 0.001 | P < 0.001 | |||||
| The presence of nodes, deformity or enlargement | 72.6 | 2.2 (1.5, 3.3) | 3.1 (2.1, 4.5) | 0.7 | <0.001 | 2.1 (1.4, 3.1) |
| P < 0.001 | P < 0.001 | |||||
| A positive grind test | 12.2 | 1.8 (1.1, 2.9) | 1.7 (1.0, 2.9) | Dropped | ||
| P = 0.015 | P = 0.027 | |||||
| A positive Finkelstein’s test | 16.8 | 1.4 (0.9, 2.2) | 1.2 (0.8, 1.9) | Dropped | ||
| P = 0.092 | P = 0.213 | |||||
| Inability to achieve position 10 of the Kapandji index | 33.3 | 1.0 (0.7, 1.4) | 1.0 (0.7, 1.4) | Dropped | ||
| P = 0.511 | P = 0.535 | |||||
| Thumb extension <40 degrees | 55.3 | 1.3 (0.9, 1.8) | 1.2 (0.8, 1.6) | Dropped | ||
| P = 0.120 | P = 0.413 | |||||
aThumb ROA is defined as K&L grade ≥2 in any thumb joint (thumb IP, first MCP, first CMC and TS), bβ is parameter estimate, cP-value = significance level, missing data were <10.2%.
Multivariable regression analysis found that right thumb ROA was most strongly associated with a combination of older age; thumb pain during activity; thenar muscle wasting; and the presence of nodes, enlargement or deformity (Table 1). Gender, BMI and all four clinical assessments did not contribute significantly to the model. The amount of explained variance of the final model was 20% (Nagelkerke value = 0.203) and the AUC was 0.72 (95% CI 0.68, 0.76). The model obtained for the left thumb (data not shown) was identical to the model for right, except thumb pain as indicated on a hand diagram was included instead of thumb pain during activity. The amount of explained variance of the final model for the left thumb was 26% (Nagelkerke value = 0.261) and the AUC was 0.77 (95% CI 0.73, 0.81).
Discussion
In this study, we examined the occurrence and patterns of involvement of ROA in the joints of the thumb in a community-dwelling population of older adults, and investigated associations between thumb pain, positive results of the clinical assessment findings and the presence of thumb ROA.
A high frequency of ROA was seen in the first CMC joint, which is consistent with the previous findings [14–16], but the frequent involvement of the thumb IP joint has only been described in a few studies [17, 18]. The lack of information about the involvement of this joint is partly due to its inconsistent inclusion and classification in studies of hand ROA [6]. When the thumb joints (thumb IP, first MCP, first CMC and TS) were assessed collectively they were found to be the most frequently affected joint group followed by the DIPs. This is inconsistent with previous research undertaken in a Dutch population where the DIP joints, including the thumb IP, were more frequently affected than the base of the thumb [16]. However, when data from our study were reanalysed using the same classification as the Dutch study, the same patterns were found. This indicates that the classification of the thumb IP joint can make substantial differences when examining the frequency of involvement in different joint groups within the hand.
Similar associations for thumb pain, thenar muscle wasting, and the presence of nodes, deformity or enlargement were found when defining thumb ROA as involvement of the first CMC joint, as when analysing involvement of any thumb joint. This could suggest that nothing is gained by including the other joints of the thumb. However, the group of participants with any thumb joint affected with ROA included an additional 98 participants who did not have first CMC involvement. If only the first CMC joints were examined, these individuals would not have been identified as having thumb ROA, even though they experienced similar levels of pain and disability.
Multivariable analysis found that the combination of age, thumb pain, muscle wasting, and the presence of nodes, deformity or enlargement best determined the presence of thumb ROA. None of the clinical assessments contributed to these models. Although a univariable association was found between thumb ROA and a positive grind test, in combination with other factors this test was not significantly associated with the presence of ROA. The frequency of a positive grind test in this sample was low. It has been suggested that this test may not be positive in milder cases, and therefore when combined with other clinical features of OA the grind test could add little information to the models [19].
Good discrimination between individuals with or without thumb ROA was found for the multivariable models. This study has shown that in combination, age, thumb pain, thenar muscle wasting, and the presence of nodes, deformity and enlargement are able to identify most individuals with thumb ROA. This could be useful in large population studies where radiography is not feasible. However, performance of these models could potentially be further improved, as several important items, such as severity of thumb pain and pain on palpation were not included in our study. Palpation of the first CMC joint may also indicate the presence of crepitus in the joint capsule, another clinical sign of OA [20].
Few studies have examined the thumb as a complex and the CAS-HA study provided a rich source of self-report, radiographic, physical examination and clinical assessment data to investigate associations of clinical signs and symptoms with the presence of thumb ROA. One limitation is that missing data may have led to bias as data were mainly missing from participants who were unable to adopt the starting position or complete a test due to the presence of pain. However, for each test the amount of missing data was small (<3.6%). For the multivariable analysis, a complete case approach was taken, which meant that up to 10.2% of participants with any missing data were not included in these analyses. Finally, these findings need further testing in other populations to test their external validity.
In summary, this research has shown that the thumb IP and first CMC joints were frequently affected with ROA. Estimates of prevalence of thumb ROA may be underestimated if the thumb IP joints are not scored. ROA of both the left and right thumbs were most strongly associated with a combination of older age, thumb pain, thenar muscle wasting and the presence of nodes, deformity and enlargement. This model should be tested in other populations and future studies could improve on this model by including additional relevant features and clinical assessments.
Acknowledgements
The authors would like to acknowledge the contributions of Prof. Peter Croft, Prof. Elaine Hay, Dr George Peat, Dr Laurence Wood, Dr Elaine Thomas, June Handy, Charlotte Clements, Catherine Tyson, Prof. Chris Buckland-Wright and Prof. Iain McCall for aspects of the conception and design of the study and the acquisition of data. Dr Jacqueline Saklatvala, Carole Jackson, Julia Myatt, Janet Wisher, Sandra Yates, Krystina Wallbank and Jean Bamford from the Department of Radiography, Haywood Hospital have contributed specifically to the acquisition of radiographic data. The authors would also like to thank the administrative and health informatics staff at the Arthritis Research UK Primary Care Centre, Keele University, and the staff and patients of the participating general practices.
Funding: This work was supported by a Programme Grant awarded by the Medical Research Council, UK (Grant Code: G9900220) and by support for science funding secured by North Staffordshire Primary Care Research Consortium for National Health Service support costs. K.D. was supported by a grant from Arthritis Research UK. Funding to pay the Open Access publication charges for this article was provided by Arthritis Research UK Primary Care Centre.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Creamer P, Hochberg MC. Osteoarthritis. Lancet. 1997;350:503–8. doi: 10.1016/S0140-6736(97)07226-7. [DOI] [PubMed] [Google Scholar]
- 2.Dziedzic K, Thomas E, Hill S, et al. The impact of musculoskeletal hand problems in older adults: findings from the North Staffordshire Osteoarthritis Project (NorStOP) Rheumatology. 2007;46:963–7. doi: 10.1093/rheumatology/kem005. [DOI] [PubMed] [Google Scholar]
- 3.O’Brien WM, Clemett AR, Acheson RM. Symptoms and patterns of osteoarthrosis in the hand in the New Haven survey of joint disease. In: Bennett PH, Wood PHN, editors. Population studies of the rheumatic diseases. Amsterdam: Excerpta Medical Foundation; 1968. pp. 398–405. [Google Scholar]
- 4.Haara MM, Heliovaara M, Kroger H, et al. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg. 2004;86:1452–7. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Chaisson CE, Zhang Y, Sharma L, Kannel W, Felson DT. Grip strength and the risk of developing radiographic hand osteoarthritis: results from the Framingham Study. Arthritis Rheum. 1999;42:33–8. doi: 10.1002/1529-0131(199901)42:1<33::AID-ANR4>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 6.Marshall M, Dziedzic KS, van der Windt DA, Hay EM. A systematic search and narrative review of radiographic definitions of hand osteoarthritis in population-based studies. Osteoarthr Cartil. 2008;16:219–26. doi: 10.1016/j.joca.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Marshall M, van der WD, Nicholls E, et al. Radiographic hand osteoarthritis: patterns and associations with hand pain and function in a community-dwelling sample. Osteoarthr Cartil. 2009;17:1440–7. doi: 10.1016/j.joca.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Myers H, Nicholls E, Handy J, et al. The Clinical Assessment Study of the Hand (CAS-HA): a prospective study of musculoskeletal hand problems in the general population. BMC Musculoskelet Disord. 2007;8:85. doi: 10.1186/1471-2474-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aulicino P. Clinical Examination of the Hand. In: Hunter J, Mackin E, Callahan A, editors. Rehabilitation of the hand: surgery and therapy. 4th edition. St Louis: Mosby; 1995. pp. 53–75. [Google Scholar]
- 10.Simpson CS. Hand assessment a clinical guide for therapists. Salisbury: APS Publishing. 2002:162–6. [Google Scholar]
- 11.Myers HL. Hand problems and hand function: a clinical epidemiological study in community-dwelling older adults. PhD thesis. Keele University. 2008 [Google Scholar]
- 12.Myers H, Dziedzic K, Thomas E, et al. Classifying hand OA in a population of older people: a reliability study (Abstract) Rheumatology. 2005;44(Suppl. 1):i14. [Google Scholar]
- 13.Lawrence JS. Osteo-arthrosis. In: Lawrence JS, editor. Rheumatism in populations. London: William Heinemann Medical Books; 1977. pp. 98–155. [Google Scholar]
- 14.Lawrence JS, Molyneux MK, Dingwall-Fordyce I. Rheumatism in foundry workers. Br J Ind Med. 1966;23:42–52. doi: 10.1136/oem.23.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egger P, Cooper C, Hart DJ, et al. Patterns of joint involvement in osteoarthritis of the hand: the Chingford Study. J Rheumatol. 1995;22:1509–13. [PubMed] [Google Scholar]
- 16.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, et al. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study) Ann Rheum Dis. 2005;64:682–7. doi: 10.1136/ard.2004.023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neame R, Doherty M. Osteoarthritis update. Clin Med. 2005;5:207–10. doi: 10.7861/clinmedicine.5-3-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toba N, Sakai A, Aoyagi K, et al. Prevalence and involvement patterns of radiographic hand osteoarthritis in Japanese women: the Hizen-Oshima study. J Bone Miner Metab. 2006;24:344–8. doi: 10.1007/s00774-006-0693-0. [DOI] [PubMed] [Google Scholar]
- 19.Glickel SZ. Clinical assessment of the thumb trapeziometacarpal joint. Hand Clinics. 2001;17:185–95. [PubMed] [Google Scholar]
- 20.Doherty M, Doherty J. Clinical examination in rheumatology. London: Wolfe Publishing; 1992. 46 pp. [Google Scholar]