Abstract
The greatest risk from live-attenuated vaccines is reversion to virulence. Particular concerns arise for RNA viruses, which exhibit high mutation frequencies. We examined the stability of 3 attenuation strategies for the alphavirus, Venezuelan equine encephalitis virus (VEEV): a traditional, point mutation-dependent attenuation approach exemplified by TC-83; a rationally designed, targeted-mutation approach represented by V3526; and a chimeric vaccine, SIN/TC/ZPC. Our findings suggest that the chimeric strain combines the initial attenuation of TC-83 with the greater phenotypic stability of V3526, highlighting the importance of the both initial attenuation and stability for live-attenuated vaccines.
Keywords: vaccine stability, RNA viruses, alphavirus, Venezuelan equine encephalitis virus
Introduction
Despite their dramatic impact on the reduction of infectious diseases, vaccines are viewed skeptically by some, and modern vaccines are subject to ever-tightening safety requirements. Many successful vaccines are attenuated strains that undergo limited replication in the vaccinee. These live-attenuated vaccines offer advantages over inactivated agents, subunit or virus-like particles that do not replicate in the host, including a typically low cost of manufacture and the induction of rapid and long-lived humoral and cell-mediated immunity after a single dose. Vaccines for polio, smallpox, and yellow fever are a few examples of highly successful, live-attenuated viral vaccines. However, these vaccines have a low but significant risk for reactogenicity and can sometimes produce life-threatening disease [1–5]. Because of their reactogenicity, current regulatory standards would probably prevent their licensure today.
Today, successful live-attenuated vaccines must carefully balance robust immunogenicity and safety. In many cases, the more immunogenic a vaccine, the more likely it will result in adverse effects. A major challenge to the generation of safe, live-attenuated vaccines to protect against RNA viral diseases is the inherent instability of the RNA genome as a result of the high error rate of RNA-dependent RNA polymerases [6]. In general, RNA viruses have mutation rates ranging from 10−3 to 10−5 substitutions per nucleotide copied [7–9]. This allows rapid adaptation and evolution when RNA viruses are subjected to changing selective pressures. These high mutation frequencies result in heterogenous mutant populations of viral genomes, even from clonal sources such as plaque harvests or cDNA [10]. This presents a major challenge for the generation of safe, live-attenuated vaccines. RNA viral vaccine genetic instability is underscored by studies of type 3 oral polio vaccinees (OPV), which commonly reveal the presence of virulent mutants [11–13]. It is therefore essential to evaluate the genomic stability of a new vaccine to ensure the genomic heterogeneity generated by replication does not impact the stable attenuation of the population.
Traditional approaches for generating live-attenuated RNA viral vaccines have relied principally on serial passage through cell cultures or animals. Examples include the yellow fever 17D, OPV, and the TC-83 Venezuelan equine encephalitis (VEE) vaccine. Genetic characterizations have revealed that attenuation of these vaccine strains results from only a few point mutations. Because of the inherent instability of the RNA genome, attenuating point mutations are likely to revert in vivo, or the virus may acquire a compensatory point mutation(s) that restores virulence (pseudoreversion). An example is TC-83, produced via 83 passages of the virulent Trinidad donkey strain (TrD) of VEEV in guinea pig heart cells (4). TC-83 attenuation is attributed to only two mutations: position three of the 5′UTR and a nonsynonymous mutation that changes amino acid 120 of the E2 glycoprotein. [14]. This small number of attenuating mutations may contribute to the high rates of reactogenicity seen in human vaccinees [15–17]. Attenuation of TC-83 has also been shown experimentally to be unstable; as few as three serial intracranial (i.c.) passages in infant mice result in reversion to a neurovirulent phenotype characteristic of the parent TrD strain [18, 19]. Of even more significance are rodent-virulent isolates made from human TC-83 vaccinees, indicating that reversion can occur in humans [20].
To overcome the instability and reactogenicity of TC-83, a new VEEV attenuation approach was developed for the V3526 vaccine. A full-length cDNA cloned derived from the Trinidad donkey (TrD) strain was modified to contain two independently attenuating mutations: 1) a deletion of the four amino acid furin cleavage recognition site between envelope proteins E3 and E2; and 2) a nonsynonymous mutation encoding a Phe-to-Ser residue change at position 253 (F253S) of the E1 envelope glycoprotein [21]. The latter mutation is required to rescue viability of the cleavage site mutant, so its reversion should be prevented as long as the E3–E2 cleavage site deletion cannot be restored. Thus, this attenuation design of V3526 should be inherently more stable than that of TC-83. Previous studies examining neurovirulence of this vaccine candidate indicated it does not gain virulence following five serial intracerebral (i.c.) passages in adult mice or five cell culture passages. Also, V3526 replicates poorly in adult mouse brains and causes less pathology when compared to TC-83 [20].
Another approach to alphavirus attenuation is to generate chimeric strains in which nonstructural genes and cis-acting RNA elements are derived from a relatively benign virus [e.g., Sindbis (SINV)], while the structural proteins are derived from the vaccine target virus. Multiple chimeric alphavirus vaccine candidates have been developed and shown to be safe, immunogenic, and protective in rodent models [22–25]. For one SIN/VEEV chimera, the capsid is derived from the TC-83 VEEV strain to enhance viral packaging and the remaining structural protein genes and cis-acting RNA elements are derived from enzootic VEEV strain ZPC738 (subtype ID) [26]. This strain, SIN/TC/ZPC (previously referred to as SIN/ZPC) is highly attenuated, immunogenic, protects against VEEV challenge, and generates no detectable viremia in mice or hamsters (Fig. 1)[27].
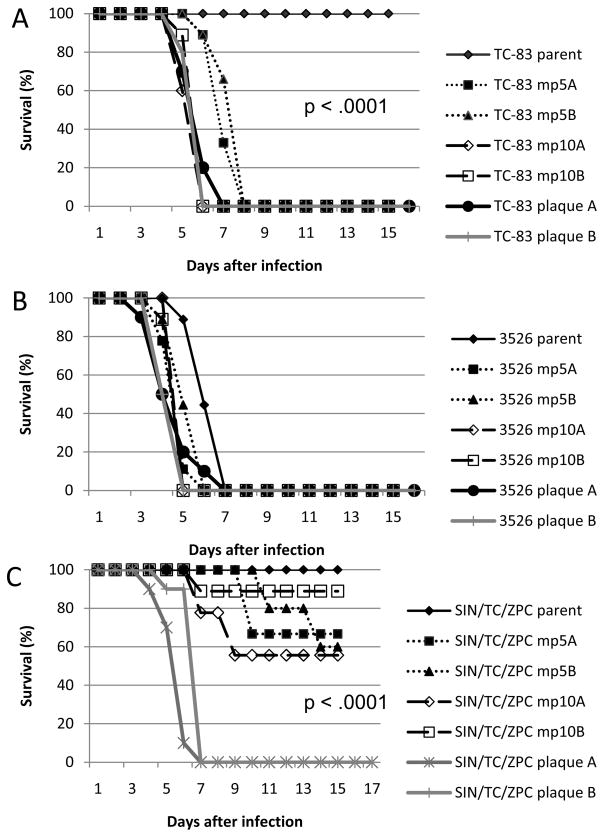
FIG 1.
Kaplan-Meier survival curves of consensus and plaque isolates from each attenuation approach. (A) TC-83; (B) V3526; (C) SIN/TC/ZPC.
In this study we tested the hypothesis that the traditional, point mutation-dependent attenuation approach exemplified by TC-83 is less stable than the attenuation strategies represented by V3526 and SIN/TC/ZPC. To assess attenuation stability, we selected for reversion to virulence and compared the phenotypic and genetic stability of each attenuation approach.
Methods
2.1 Viruses
Each of the three viruses used in this study was derived from a cDNA clone and transcribed RNA was electroporated into BHK cells to generate infectious virus. The TC-83 [28], SIN/TC/ZPC [27], and V3526 clones were described previously. The V3526 mutations were introduced into a V3000 clone of a VEEV TrD isolate that had previously been passed once in guinea pig brain and 14 times in embryonated eggs [21, 29].
2.2 Selection for virulence
We subjected each VEEV strain to 10 serial, i.c. inoculations in 6-day-old outbred NIH Swiss mice (Harlan Laboratories, Indianapolis, IN). For each passage, approximately 50 μl of a 6 log10 plaque forming unit (pfu)/ml stock of virus was inoculated into five mice per replicate. Two parallel replicate passage series (A and B) of each strain were performed to assess variation in the results and to detect convergent mutations that might indicate positive selection. Following ca. 48 h of incubation, after which the mice were euthanized, their brains were harvested, triturated, and titrated by plaque assay on Vero cells. Virus isolated from one brain sample from each replicate was used as the inoculum for the next passage. During the passage series, we observed that mice in both the V3526 and TC-83 series began dying less than 48 h after infection. Therefore, during later passages we harvested at earlier time points to retrieve brains prior to death. Following 10 passages, the brain isolates were plaqued on Vero cell monolayers to isolate clonal populations for further study. A single clonal population for each replicate was randomly selected and subjected to further analysis. While there was some plaque size variation observed in some replicates of passages 2–5 for V3526 and SIN/TC/ZPC, no major plaque phenotype differences were observed in p10 of any of the strains. Thus, the plaque clonal isolates were derived from average size plaques for each p10 replicate.
2.3 Phenotypic virulence
The virulence of the parental strains, consensus viruses isolated from passages 5 (p5) and 10 (p10), and plaque clonal isolates was evaluated by inoculating 6-day-old mice NIH Swiss mice subcutaneously (s.c.) with 50 μl of a 6 log10 pfu/ml stock and assessing survival over 14 days. Subcutaneous infection was selected because intracranial infection results in rapid death with little opportunity to observe increased virulence.
2.4 Genomic sequencing
To investigate potential determinants of increased virulence, the complete genomes of 5th and 10th passage populations as well as the p10 plaque clone isolate populations were analyzed. RNA was extracted using the QIAamp Viral RNA Mini kits (Qiagen, Valencia, CA) and amplified using the Titan One Tube RT-PCR kit (Roche, Germany). RT-PCR products were visualized on a 1% agarose gel and bands were gel extracted. Sequencing was performed using an ABI 3100 Genetic Analyzer (Applied Biosystems, Carlsbad, CA) and alignments and analysis were performed in Sequencher 4.9 (Ann Arbor, MI). The 5′ untranslated region (UTR) of each strain was amplified using the RLM-RACE kit (Ambion, Austin, TX).
Results
3.1 Virulence
As expected, each vaccine strain showed an overall increase in virulence following serial passages (Figure 1). The TC-83 parent caused no mortality over 14 days, but the p5 TC-83 replicates both caused 100% mortality by 8 days post-inoculation, and the p10 replicates caused 100% mortality by day 6 (Fig. 1A). TC-83 plaque isolates from replicates A and B caused 100% mortality by day 7 and 6, respectively (Fig. 1A). A log rank test on the survival curves indicated that this increase in TC-83 virulence was significant (p < .0001).
Strain V3526 exhibited the highest parental virulence (100% mortality by day 7), but passaging had little effect (100% mortality by days 6 and 5 for p5 and p10, respectively). Interestingly, the p10 plaque isolate from replicate A appeared to be no more virulent than the parental strain, (causing 100% mortality by day 7), whereas the replicate B plaque isolate was highly virulent, causing 100% mortality by day 5 (Fig. 1B). No changes in the virulence of any V3526 passages were significant.
Like TC-83, the SIN/TC/ZPC parental strain induced no mortality and remained the most attenuated after selection for increased neurovirulence, with 11–44% mortality rates for p5 and p10 isolates. Specifically, replicate p5A killed 33% of mice by day 10, whereas replicate p5B killed 40% by day 12. Even more pronounced, passage p10A produced 44% mortality by day 9, while p10B only produced 11% mortality by day 10. Both plaque isolates showed an increase in virulence compared to the populations from which they were derived, causing 100% mortality by day 7 (Fig. 1C). A log rank analysis indicated that the virulence changes exhibited by both passaged populations and plaque isolates were highly significant (p < .0001). Comparison of the plaque isolate replicates alone indicated a significant difference in virulence between the replicates (p <0.01).
3.2 Genetic stability
Full genome sequencing of each p10 strain was performed to correlate genetic changes with changes in virulence. As seen in Table 1, TC-83 consensus replicate A had an insertion in the 3′ UTR and a mutation in E1. TC-83 consensus replicate B had an amino acid change in nsP2, synonymous mutations in nsP2 and E1, and a deletion in the 3′ UTR. The plaque isolate from TC-83 replicate A had a nonsynonymous mutation in the E1 gene, while the replicate B plaque had a mutation at position 3 of the 5′UTR. Both p10 replicates of V3526 accumulated 4 nonsynonomous changes, all of which occurred in either the E2 or E1 genes. The sequence of V3526 plaque clonal replicate A had a previously unseen nonsynonymous mutation in the E1 gene, and clonal replicate B had an additional nonsynonymous nsP2 mutation at position 129. In both passage replicates, SIN/TC/ZPC had a consensus mutation at nucleotide 5 in the 5′ UTR, and replicate B had two adjacent mutations in the nsP3 gene. SIN/TC/ZPC plaque isolate A had two unique nucleotide changes at position 130 in the nsP1 gene and at position 32 of the nsP3 gene. Replicate B had a T45C mutation in the 5′UTR.
Table 1.
Sequencing findings for passage 10 consensus and plaque isolates of TC83, 3526, and SIN/TC/ZPC.
| Position | Nucleotide | Amino Acids | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| nr | AA | Parent | consensus 10A | consensus 10B | plaque 10A | plaque 10B | parent | consensus 10A | consensus 10B | plaque 10A | plaque 10B | |
| TC83 | 3 | 5′ UTR | A | A | A | A | G | - | - | - | - | - |
| 2929 | 438 (nsP2) | G | G | C | G | G | Gly | - | Ala | - | - | |
| 2930 | 438 (nsP2) | C | C | G | C | C | Gly | - | - | - | - | |
| 5578 | 516 (nsP3) | C | C | C | T | C | Thr | - | - | Ile | - | |
| 10900 | 304 (E1) | A | G | G | G | G | Glu | - | - | - | - | |
| 11404 | 3′UTR | - | - | - | T (insert) | T (insert) | - | - | - | - | - | |
| 11409 | 3′UTR | - | T (insert) | - | - | - | - | - | - | - | - | |
| 11414 | 3′UTR | T | T | T (deletion) | T | T | - | - | - | - | - | |
| 3526 | 44 | 5′UTR | - | - | - | - | A (deletion) | - | - | - | - | - |
| 2034 | 129 (nsP2) | G | G | G | G | A | Asp | - | - | - | Asn | |
| 7061 | 452 (nsP4) | G | G | G | G | A | Arg | - | - | - | - | |
| 8571 | 7 (E2) | A | C | A | C | A | Lys | Thr | - | Thr | - | |
| 9080 | 177 (E2) | A | A | C | A | C | Ser | - | Arg | - | Arg | |
| 9097 | 182 (E2) | C | A | C | A | C | Ser | Arg | - | Arg | - | |
| 10602 | 204 (E1) | C | C | C | T | C | Ser | - | - | Phe | - | |
| 10979 | 331 (E1) | C | C | C/T | C | C | His | - | Tyr | - | - | |
| SIN/TC/ZPC | 5 | 5′UTR | A | G | G | A | A | - | - | - | - | - |
| 45 | 5′UTR | T | T | T | T | C | - | - | - | - | - | |
| 448 | 130 (nsP1) | C | C | C | T | C | Ala | - | - | Val | - | |
| 4014 | 775 (nsP2) | C | C | C | C | A | Arg | - | - | - | - | |
| 4191 | 31 (nsP3) | G | G | G/C | G | G | Glu | - | Gln | - | - | |
| 4192 | 31 (nsP3) | A | A | C | A | A | Glu | - | Asp | - | - | |
| 31 (if both) | GAG | GAG | CCG | GAG | GAG | Glu | - | Pro | - | - | ||
| 4194 | 32 (nsP3) | A | A | A | C | A | Glu | - | - | Ala | - | |
Discussion
In this study we evaluated the genetic and phenotypic stability of three attenuation methods for alphavirus vaccine development. We subjected each strain to selection for adaptation to virulence by sequentially passaging them through infant mouse brains. We observed significant increases in lethality of both TC-83 and SIN/TC/ZPC, and an increasing trend for virulence in V3526. However, while we observed an increase in virulence for each strain, only modest changes occurred in the consensus sequences. The lack of a clear correlation between genetic and phenotypic changes was surprising, but not unprecedented. Quasispecies analyses of multiple RNA viruses have shown that selection can act on viral populations as a whole rather than the individual representative genomes [30–32]. Similarly, virulence can be determined by the proportion of and interaction between attenuated and virulent genomes [33–36]. Therefore, the observed phenotype may not correlate with consensus mutations because the virulence determinants operate at a population level. This is exemplified by foot-and-mouth disease (FMDV) and mumps viruses, in which significant changes in virulence are not reflected in the observed genetic heterogeneity [37, 38]. Similar findings have been demonstrated previously for other arboviruses [39–41].
By examining plaque clones from each passage replicate we were able to identify some virulent variants that differed from the consensus sequence. The plaque isolate from TC-83 replicate B had a mutation in the 5′UTR that is known to be one of two sites responsible for attenuation of this strain [14]. However, this mutation did not appear to afford the variant full wild-type virulence, as the parental Trinidad Donkey strain caused 100% lethality within three days when inoculated subcutaenously into infant mice (data not shown). We also observed a higher virulence of plaque clonal isolates of both replicates of SIN/TC/ZPC, as compared to the uncloned populations, without any genetic change in regions known to be important for virulence. These clonal isolates may represent subpopulations of genomes that are masked, and suggest that more intensive viral population analysis may reveal details about the range and frequency of individual variants. As discussed above, RNA virus populations are expected to exhibit genetic instability as a result of their error-prone polymerases.
While all three attenuation methods showed some evidence of instability, the only direct genetic reversion was observed for TC-83, which is known to revert to virulence in both animal models and human vaccinees [18–20]. While V3526 had the least overall change in virulence, it showed the greatest genomic instability with 8 total mutations, 6 of which were nonsynonymous. SIN/TC/ZPC had a high degree of initial attenuation and strong genomic stability in the VEEV-derived structural protein genes, with consensus mutations observed only in the nonstructural SINV-derived genome regions. Plaque clones exhibited higher virulence than either of the passaged populations or the parental strain, suggesting that these clonal isolates are examples of variants masked by more attenuated variants in the population. It is not surprising to observe a subpopulation of variants differing in virulence within an RNA viral population [34, 37]. However, we were encouraged to observe that, even when subjected to strong serial selective pressures, higher virulence variants did not emerge as consensus sequences within the SIN/TC/ZPC populations. While this level of stability is clearly enhanced over that of TC-83, it remains to be determined if it is acceptable for vaccine development. As greater scrutiny is placed on vaccine safety, further characterization of the quasispecies found within vaccine products may become common, and next generation deep sequencing may play a greater role in characterization of master seeds. Our results underscore the current gap between characterizing genomic variants within an RNA virus population and understanding and ultimately predicting their effect on virulence. This topic clearly deserves further attention.
Our results suggest that SIN/TC/ZPC combines the initially high degree of attenuation exhibited by TC-83 with the greater phenotypic stability of V3526, and thus is highly promising as a relatively stably attenuated vaccine candidate. Both the chimeric SIN/TC/ZPC and the V3526 attenuation methods have clear advantages to historical methods of serial cell culture passage represented by TC-83. However, additional studies are needed to evaluate the significance of the clonal variants within vaccine populations that vary in virulence, and to determine whether those variants have potential consequences for vaccine safety. Finally, our study highlights the need for the development of a standardized method and guidelines for evaluating acceptable RNA viral vaccine stability.
Acknowledgments
We thank Wenli Kang, Rubing Chen, and Mathilde Guerbois for technical assistance, and Nancy Davis, Robert Johnston, and Richard Kinney for providing cDNA clones for the V3526 and TC-83 vaccine strains. JLK was supported by a McLaughlin Endowment fellowship. SMV was supported by the NIH training grant T32 AI007536. This work was supported by a grant from the National Institute of Allergy and Infectious Disease (NIAID) through the Western Regional Center of Excellence for Biodefense and Emerging Infectious Disease Research, National Institutes of Health (NIH) grant U54 AIO57156.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Minor P. Vaccine-derived poliovirus (VDPV): Impact on poliomyelitis eradication. Vaccine. 2009 May 5;27(20):2649–52. doi: 10.1016/j.vaccine.2009.02.071. [DOI] [PubMed] [Google Scholar]
- 2.Kew OM, Sutter RW, de Gourville EM, Dowdle WR, Pallansch MA. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu Rev Microbiol. 2005;59:587–635. doi: 10.1146/annurev.micro.58.030603.123625. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs BL, Langland JO, Kibler KV, Denzler KL, White SD, Holechek SA, et al. Vaccinia virus vaccines: past, present and future. Antiviral Res. 2009 Oct;84(1):1–13. doi: 10.1016/j.antiviral.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrett AD, Teuwen DE. Yellow fever vaccine - how does it work and why do rare cases of serious adverse events take place? Curr Opin Immunol. 2009 Jun;21(3):308–13. doi: 10.1016/j.coi.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Belongia EA, Naleway AL. Smallpox vaccine: the good, the bad, and the ugly. Clin Med Res. 2003 Apr;1(2):87–92. doi: 10.3121/cmr.1.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holland J, Spindler K, Horodyski F, Grabau E, Nichol S, VandePol S. Rapid evolution of RNA genomes. Science. 1982 Mar 26;215(4540):1577–85. doi: 10.1126/science.7041255. [DOI] [PubMed] [Google Scholar]
- 7.Domingo E, Holland JJ. RNA virus mutations and fitness for survival. Annu Rev Microbiol. 1997;51:151–78. doi: 10.1146/annurev.micro.51.1.151. [DOI] [PubMed] [Google Scholar]
- 8.Drake JW. Rates of spontaneous mutation among RNA viruses. Proc Natl Acad Sci U S A. 1993 May 1;90(9):4171–5. doi: 10.1073/pnas.90.9.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drake JW, Holland JJ. Mutation rates among RNA viruses. Proc Natl Acad Sci U S A. 1999 Nov 23;96(24):13910–3. doi: 10.1073/pnas.96.24.13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinhauer DA, Holland JJ. Rapid evolution of RNA viruses. Annu Rev Microbiol. 1987;41:409–33. doi: 10.1146/annurev.mi.41.100187.002205. [DOI] [PubMed] [Google Scholar]
- 11.Chumakov KM, Powers LB, Noonan KE, Roninson IB, Levenbook IS. Correlation between amount of virus with altered nucleotide sequence and the monkey test for acceptability of oral poliovirus vaccine. Proc Natl Acad Sci U S A. 1991 Jan 1;88(1):199–203. doi: 10.1073/pnas.88.1.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evans DM, Dunn G, Minor PD, Schild GC, Cann AJ, Stanway G, et al. Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 poliovaccine genome. Nature. 1985 Apr 11–17;314(6011):548–50. doi: 10.1038/314548a0. [DOI] [PubMed] [Google Scholar]
- 13.Westrop GD, Wareham KA, Evans DM, Dunn G, Minor PD, Magrath DI, et al. Genetic basis of attenuation of the Sabin type 3 oral poliovirus vaccine. J Virol. 1989 Mar;63(3):1338–44. doi: 10.1128/jvi.63.3.1338-1344.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kinney RM, Chang GJ, Tsuchiya KR, Sneider JM, Roehrig JT, Woodward TM, et al. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J Virol. 1993 Mar;67(3):1269–77. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996 Mar;14(4):337–43. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- 16.Alevizatos AC, McKinney RW, Feigin RD. Live, attenuated Venezuelan equine encephalomyelitis virus vaccine. I. Clinical effects in man. Am J Trop Med Hyg. 1967 Nov;16(6):762–8. [PubMed] [Google Scholar]
- 17.McKinney RW. Venezuelan equine encephalitis. Pan American Health Organization. 1972;243:369–76. [Google Scholar]
- 18.Berge TO, Bankds IS, Tigertt WD. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea pig heart cells. Am J Hyg. 1961;73:209–18. [Google Scholar]
- 19.McKinney RW, Berge TO, Sawyer WD, Tigertt WD, Crozier D. Use of an Attenuated Strain of Venezuelan Equine Encephalomyelitis Virus for Immunization in Man. Am J Trop Med Hyg. 1963 Jul;12:597–603. doi: 10.4269/ajtmh.1963.12.597. [DOI] [PubMed] [Google Scholar]
- 20.Ludwig GV, Turell MJ, Vogel P, Kondig JP, Kell WK, Smith JF, et al. Comparative neurovirulence of attenuated and non-attenuated strains of Venezuelan equine encephalitis virus in mice. Am J Trop Med Hyg. 2001 Jan-Feb;64(1–2):49–55. doi: 10.4269/ajtmh.2001.64.49. [DOI] [PubMed] [Google Scholar]
- 21.Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, et al. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995 Sep 10;212(1):102–10. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- 22.Atasheva S, Wang E, Adams AP, Plante KS, Ni S, Taylor K, et al. Chimeric alphavirus vaccine candidates protect mice from intranasal challenge with western equine encephalitis virus. Vaccine. 2009 Jul 9;27(32):4309–19. doi: 10.1016/j.vaccine.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. Recombinant sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J Virol. 2003 Sep;77(17):9278–86. doi: 10.1128/JVI.77.17.9278-9286.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, et al. Chimeric Sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine. 2007 Oct 23;25(43):7573–81. doi: 10.1016/j.vaccine.2007.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang E, Volkova E, Adams AP, Forrester N, Xiao SY, Frolov I, et al. Chimeric alphavirus vaccine candidates for chikungunya. Vaccine. 2008 Sep 15;26(39):5030–9. doi: 10.1016/j.vaccine.2008.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frolova E, Frolov I, Schlesinger S. Packaging signals in alphaviruses. J Virol. 1997 Jan;71(1):248–58. doi: 10.1128/jvi.71.1.248-258.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, et al. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J Virol. 2006 Mar;80(6):2784–96. doi: 10.1128/JVI.80.6.2784-2796.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kinney RM, Johnson BJ, Welch JB, Tsuchiya KR, Trent DW. The full-length nucleotide sequences of the virulent Trinidad donkey strain of Venezuelan equine encephalitis virus and its attenuated vaccine derivative, strain TC-83. Virology. 1989 May;170(1):19–30. doi: 10.1016/0042-6822(89)90347-4. [DOI] [PubMed] [Google Scholar]
- 29.Davis NL, Willis LV, Smith JF, Johnston RE. In vitro synthesis of infectious venezuelan equine encephalitis virus RNA from a cDNA clone: analysis of a viable deletion mutant. Virology. 1989 Jul;171(1):189–204. doi: 10.1016/0042-6822(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 30.Eigen M. Viral quasispecies. Sci Am. 1993 Jul;269(1):42–9. doi: 10.1038/scientificamerican0793-42. [DOI] [PubMed] [Google Scholar]
- 31.Martinez MA, Carrillo C, Gonzalez-Candelas F, Moya A, Domingo E, Sobrino F. Fitness alteration of foot-and-mouth disease virus mutants: measurement of adaptability of viral quasispecies. J Virol. 1991 Jul;65(7):3954–7. doi: 10.1128/jvi.65.7.3954-3957.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruiz-Jarabo CM, Arias A, Baranowski E, Escarmis C, Domingo E. Memory in viral quasispecies. J Virol. 2000 Apr;74(8):3543–7. doi: 10.1128/jvi.74.8.3543-3547.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Codoner FM, Daros JA, Sole RV, Elena SF. The fittest versus the flattest: experimental confirmation of the quasispecies effect with subviral pathogens. PLoS Pathog. 2006 Dec;2(12):e136. doi: 10.1371/journal.ppat.0020136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de la Torre JC, Holland JJ. RNA virus quasispecies populations can suppress vastly superior mutant progeny. J Virol. 1990 Dec;64(12):6278–81. doi: 10.1128/jvi.64.12.6278-6281.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfeiffer JK, Kirkegaard K. Increased fidelity reduces poliovirus fitness and virulence under selective pressure in mice. PLoS Pathog. 2005 Oct;1(2):e11. doi: 10.1371/journal.ppat.0010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vignuzzi M, Stone JK, Arnold JJ, Cameron CE, Andino R. Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature. 2006 Jan 19;439(7074):344–8. doi: 10.1038/nature04388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanz-Ramos M, Diaz-San Segundo F, Escarmis C, Domingo E, Sevilla N. Hidden virulence determinants in a viral quasispecies in vivo. J Virol. 2008 Nov;82(21):10465–76. doi: 10.1128/JVI.00825-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sauder CJ, Vandenburgh KM, Iskow RC, Malik T, Carbone KM, Rubin SA. Changes in mumps virus neurovirulence phenotype associated with quasispecies heterogeneity. Virology. 2006 Jun 20;350(1):48–57. doi: 10.1016/j.virol.2006.01.035. [DOI] [PubMed] [Google Scholar]
- 39.Ciota AT, Ngo KA, Lovelace AO, Payne AF, Zhou Y, Shi PY, et al. Role of the mutant spectrum in adaptation and replication of West Nile virus. J Gen Virol. 2007 Mar;88(Pt 3):865–74. doi: 10.1099/vir.0.82606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Novella IS, Ebendick-Corpus BE. Molecular basis of fitness loss and fitness recovery in vesicular stomatitis virus. J Mol Biol. 2004 Oct 1;342(5):1423–30. doi: 10.1016/j.jmb.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 41.Coffey LL, Vasilakis N, Brault AC, Powers AM, Tripet F, Weaver SC. Arbovirus evolution in vivo is constrained by host alternation. Proc Natl Acad Sci U S A. 2008 May 13;105(19):6970–5. doi: 10.1073/pnas.0712130105. [DOI] [PMC free article] [PubMed] [Google Scholar]