Abstract
Extracranial carotid aneurysms are a rare entity and carry an inherent risk of thromboembolic complications. Treatment options consist of endovascular and conventional surgical techniques. We describe the cases of 3 patients who were treated with an interposition graft for a large extracranial carotid aneurysm.
The patients had presented with an extracranial carotid aneurysm with a diameter of 30 to 43 mm. In all cases, the aneurysm was excluded by means of an interposition graft, without major perioperative complications. There was 1 case of temporary paresis of the facial nerve and another of temporary paresis of the vocal cord. After a mean follow-up period of 14 months, all patients were alive, and there were no neurologic deficits.
A retrospective analysis was performed of patients who had undergone conventional surgical treatment of extracranial carotid aneurysms. The patients' characteristics, symptoms, surgical interventions, complications, and deaths were all documented.
Carotid aneurysms can safely be excluded by interposition grafting, and this treatment should still be considered for most patients, although endovascular repair might provide a valid alternative.
Key words: Aneurysm/surgery; carotid artery diseases; carotid artery, common/surgery; carotid artery, internal/surgery; cranial nerve injuries/etiology; graft, interposition; stents; treatment outcome
Extracranial carotid aneurysms are an uncommon entity, comprising 0.4% to 4% of all peripheral aneurysms1,2; only 0.1% to 2% of all surgical carotid procedures are performed for aneurysms.3 Local pain and a pulsating mass in the neck are the most frequently described symptoms.1,4,5 Patients might also present with ischemic stroke, transient ischemic attack, amaurosis fugax, or cranial nerve compression. Most patients, however, remain asymptomatic. Carotid artery aneurysms are usually diagnosed by means of ultrasonographic scanning. Additional diagnostic testing—by computed tomographic angiography, magnetic resonance imaging, or angiography—can lead to more accurate information on the aneurysm's size and its relationship to surrounding structures.4 Most aneurysms in the carotid vasculature occur at the level of the common carotid artery, followed by that of the internal carotid artery. Aneurysms of the external carotid artery are extremely rare.6 Although most carotid artery aneurysms are caused by atherosclerosis, other common causes include trauma and infection. Less frequent causes are cystic medial necrosis, Marfan syndrome, Takayasu arteritis, and idiopathic medial arteriopathy.2
Indications for intervention arise chiefly from the risk of rupture and embolic sequelae, or from the presence of cranial nerve dysfunction.7–9 Treatment options consist of surgical exclusion with an interposition graft, ligation of the artery, and endovascular exclusion with a stent-graft. Between 2007 and 2008, we treated 3 carotid-aneurysm patients with interposition grafts, in 2 different hospitals. Results of this treatment are presented herein.
Case Reports
Patient 1
A 71-year-old man with a history of hypertension, type 2 diabetes mellitus, hypercholesterolemia, coronary artery disease, moderate aortic valve stenosis, and obesity presented with a thiamine deficiency attributable to alcohol abuse. Coincidentally, a carotid artery aneurysm was found. Computed tomographic angiography showed a saccular aneurysm of the left internal carotid artery with a maximal diameter of 36 mm (Fig. 1). The right carotid artery at the level of the bifurcation was modestly enlarged, at 14 mm.
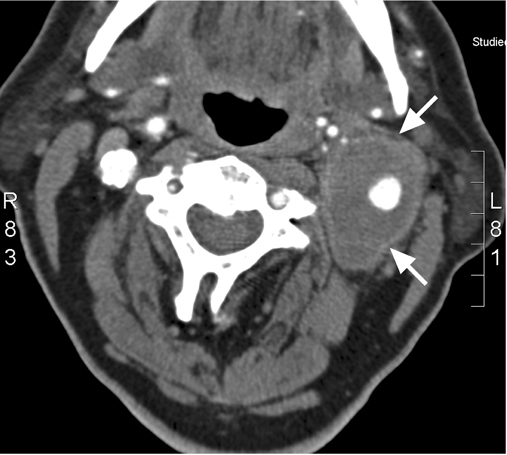
Fig. 1 Patient 1. Computed tomographic angiogram shows a left-sided saccular aneurysm of the internal carotid artery (arrows) in the axial plane.
At first, treatment of the asymptomatic aneurysm was conservative, consequent to the patient's multiple comorbidities. Because of myocardial ischemia, a coronary artery stenosis was treated with angioplasty and stenting. During 8 months of follow-up, however, the carotid aneurysm expanded to 43 mm. Ultrasonographic scanning showed a mural thrombus within the aneurysm. Although the aneurysm remained asymptomatic in terms of embolic complications, we decided to exclude it by open surgery.
The procedure was performed with the patient under general anesthesia and monitored by electroencephalography (EEG) and transcranial Doppler (TCD) echocardiography. First, the mandible was subluxated and temporarily fixed, in order to expose the distal end of the aneurysm. Then, we dissected the internal carotid artery and identified the hypoglossal nerve. The aneurysm was opened after clamping, mural thrombus was removed, and the aneurysm was partly resected. The greater saphenous vein was used as an interposition graft. During the entire procedure, the EEG remained normal and no temporary shunt had to be used. Postoperatively, the patient was placed on a lifelong regimen of aspirin, taken daily. There were no postoperative complications, and on the 3rd day after surgery the patient was discharged from the hospital in good ambulatory condition. After a follow-up of 2 years and 4 months, the bypass was patent and there were no neurologic complications.
Patient 2
An 85-year-old man, a nonsmoker with an extensive cardiac history who had survived a ruptured abdominal aortic aneurysm 5 years earlier, presented with collapse, without focal neurologic deficits. Physical examination revealed a pulsatile mass on the left side of the neck with a palpable thrill and systolic bruit. Duplex ultrasonographic scanning and computed tomographic angiography (Fig. 2) confirmed the diagnosis of a saccular aneurysm of the common carotid artery (diameter, 38 mm), with signs of a penetrating atherosclerotic ulcer. The right carotid artery was normal.

Fig. 2 Patient 2. Computed tomographic angiogram shows a saccular aneurysm of the common carotid artery (arrows) in the coronal plane.
It was decided to perform an emergency surgical repair, because of the neurologic symptoms the night before. The procedure was performed with the patient under general anesthesia, without EEG or TCD monitoring. The aneurysm was exposed and opened after clamping. Cerebral flow was secured by using a temporary shunt throughout the operation. A ruptured atherosclerotic ulcer was found. The aneurysm was excluded by means of an 8-mm ePTFE interposition graft. Postoperatively, the patient resumed taking acenocoumarol, on a daily lifelong regimen. His postoperative course was complicated by a temporary bruising of the left vocal cord, which resolved within months. There were no neurologic sequelae. The patient was discharged from the hospital on the 4th postoperative day. At the 8-month follow-up appointment, the interposition graft was patent and there were no neurologic sequelae.
Patient 3
A 70-year-old woman, a nonsmoker, was being analyzed for thoracic pain caused by a Stanford type B dissection. She had a history of hypertension, hypercholesterolemia, and treatment for aneurysms of the abdominal aorta and left common iliac artery. During her physical examination, an aneurysm of the left internal carotid artery was found. Duplex ultrasonography and magnetic resonance imaging showed a saccular aneurysm of the left internal carotid artery with a diameter of 30 mm (Fig. 3). The right internal carotid artery was slightly enlarged, to a maximum diameter of 15 mm.
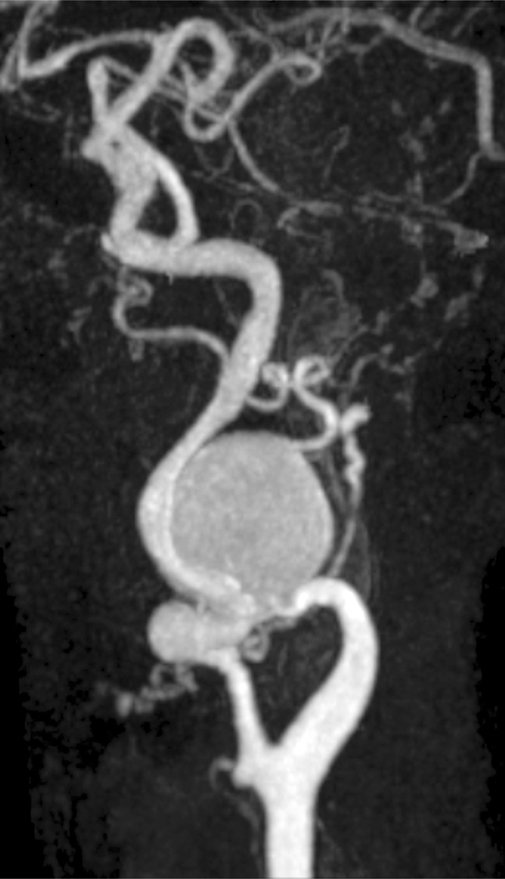
Fig. 3 Patient 3. Magnetic resonance image shows a saccular aneurysm of the left internal carotid artery in the coronal plane.
The patient underwent operation within 1 week, under EEG monitoring. A temporary shunt was used during the procedure. The aneurysm was exposed and the facial, accessory, and hypoglossal nerves were all identified. There was no mural thrombus. The aneurysm was excluded by means of a greater saphenous vein interposition graft. Postoperatively, the patient continued taking aspirin. As a sequela of the operation, there was a temporary paresis of the facial nerve that resolved within 3 months. She was discharged from the hospital on the 4th postoperative day.
Two months afterwards, a stent-graft was implanted in the descending aorta for a post-dissection false aneurysm. Because there was a clinical suspicion of connective-tissue disease, due to the patient's unusually long fingers and toes, genetic analysis was performed. Neither Marfan syndrome nor Ehlers-Danlos syndrome type 4 could be proved. After a follow-up period of 18 months, the interposition graft was patent and there were no neurologic sequelae.
Discussion
In the present article, we have shown that carotid artery aneurysms can be safely excluded with interposition grafts. In our 3 patients, there were no perioperative strokes or other major neurologic complications. However, an instance of temporary paresis of the facial nerve and an instance of temporary paresis of the vocal cord occurred, in 2 different patients. These results are in accord with observations in earlier reports3,10 of surgical exclusion of carotid artery aneurysms. In a series of 67 surgically treated carotid aneurysms, El-Sabrout and Cooley3 reported a rate of 9% for death or major stroke and a rate of 6% for cranial nerve injury. During a follow-up period of approximately 6 years, 28% of the patients died, due mainly to cardiac causes. In 2009, Attigah and colleagues10 published their long-term results of surgical therapy of extracranial carotid artery aneurysms in 57 patients. The perioperative stroke rate was 2%, and 6% experienced a transient ischemic attack. Permanent and transient cranial nerve injury occurred in 6% and 20% of all patients, respectively. After follow-up periods of 5, 10, 15, and 20 years, the actuarial survival rates were 90%, 77%, 65%, and 57%; and the ipsilateral stroke-free rates were 96%, 96%, 93%, and 87%, respectively.
Endovascular repair of carotid aneurysms has been described as a quick and less invasive alternative that causes fewer nerve injuries.8,9 Endovascular repair can especially benefit high-risk patients: that is, those with severe comorbidity or with a “hostile neck” unsuitable for surgery. However, the main concern associated with endovascular procedures in the carotid artery—the risk of embolic complications—remains. Because there are few reports on endovascular treatment of carotid aneurysms, the actual risk of stroke is still unknown. There have been 2 case reports of successful endovascular exclusion in patients with hostile necks after radiation treatment.9,11 These cases have short follow-up periods but certainly suggest that endovascular treatment is a useful alternative in cases that are unsuitable for surgery. There are also several reports of successful endovascular exclusion of traumatic carotid pseudoaneurysms.12,13 Patel and colleagues13 have stated that most patients with saccular aneurysms might be candidates for endovascular treatment. In a multicenter study, Radak and co-investigators7 found that 51% of all carotid aneurysms are saccular. Zhou and associates8 retrospectively compared 2 cohorts of patients with carotid aneurysm. Patients in the first group had undergone operative repair in the first 10-year period, and patients in the second group had undergone either surgical correction (30%) or endovascular exclusion (70%) in the second 10-year period. Zhou concluded that treatment of extracranial carotid artery aneurysms had largely evolved from operative to endovascular intervention. Benefits of endovascular treatment included shorter convalescent times and less cranial nerve injury. Unfortunately, the authors did not describe the causes or the morphologic types of the treated aneurysms.
Conclusion
At present, the indications for intervention in patients with extracranial carotid aneurysms have not been completely brought to light. In the event of symptoms, an intervention is clearly indicated. To date, the risk of complications of an asymptomatic aneurysm and its relation to issues like aneurysmal diameter and plaque instability have not been studied. The choice between endovascular repair and conventional surgery can depend on various factors, including the type of aneurysm, comorbidities, symptoms, and the experience and preference of the surgeon. The relatively low incidence of these lesions makes it difficult to obtain sufficient experience with endovascular procedures for carotid aneurysm. However, growing proficiency with carotid stenting for stenotic lesions might provide adequate interventional skills.
In summary, we have shown that interposition grafting of large atherosclerotic carotid aneurysms can be safe, but that there is a risk of cranial nerve injury. There were no strokes or major neurologic complications in our 3 patients. Controlled comparative studies of endovascular treatment are a challenge for the future; however, the low incidence of lesions will complicate the design of such studies.
References
- 1.Quigley F, Matalanis G, Doolan L. Aneurysm surgery. In: Faris I, Buxton B, editors. Practice of surgery. London: Churchill Livingstone; 1995. p. 258–63.
- 2.Goldstone J. Aneurysms of the extracranial carotid artery. In: Rutherford RB, editor. Vascular surgery. 6th ed. Philadelphia: Elsevier Saunders; 2005. p. 2052–64.
- 3.El-Sabrout R, Cooley DA. Extracranial carotid artery aneurysms: Texas Heart Institute experience. J Vasc Surg 2000;31 (4):702–12. [DOI] [PubMed]
- 4.Knight GC, Hallman GL, Reul GJ, Ott DA, Cooley DA. Surgical management of extracranial carotid artery aneurysms: report of 17 cases. Tex Heart Inst J 1988;15(2):91–7. [PMC free article] [PubMed]
- 5.Stehbens WE. Aneurysms. In: Vascular pathology, aneurysm. Stehbens WE, Lie JT, editors. London: Chapman & Hall Medical; 1995. p. 369.
- 6.Rosset E, Albertini JM, Magnan PE, Ede B, Mathieu JP, Branchereau A. Surgical treatment of extracranial internal carotid artery aneurysms. In: Branchereau A, Jacobs M, editors. New trends and developments in carotid artery disease. Armonk (NY): Futura Publishing Company, Inc.; 1998. p. 169–81.
- 7.Radak D, Davidovic L, Vukobratov V, Ilijevski N, Kostic D, Maksimovic Z, et al. Carotid artery aneurysms: Serbian multicentric study. Ann Vasc Surg 2007;21(1):23–9. [DOI] [PubMed]
- 8.Zhou W, Lin PH, Bush RL, Peden E, Guerrero MA, Terramani T, et al. Carotid artery aneurysm: evolution of management over two decades. J Vasc Surg 2006;43(3):493–7. [DOI] [PubMed]
- 9.Bellosta R, Sesana M, Baglini R, Luzzani L, Talarico M, Sarcina A. Endovascular treatment of a symptomatic carotid artery aneurysm with a stent graft. Vasc Endovascular Surg 2008; 42(3):276–8. [DOI] [PubMed]
- 10.Attigah N, Kulkens S, Zausig N, Hansmann J, Ringleb P, Hakimi M, et al. Surgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year period. Eur J Vasc Endovasc Surg 2009;37(2):127–33. [DOI] [PubMed]
- 11.Mukherjee D, Roffi M, Yadav JS. Endovascular treatment of carotid artery aneurysms with stent grafts. J Invasive Cardiol 2002;14(5):269–72. [PubMed]
- 12.Simionato F, Righi C, Melissano G, Rolli A, Chiesa R, Scotti G. Stent-graft treatment of a common carotid artery pseudoaneurysm. J Endovasc Ther 2000;7(2):136–40. [DOI] [PubMed]
- 13.Patel JV, Rossbach MM, Cleveland TJ, Gaines PA, Beard JD. Endovascular stent-graft repair of traumatic carotid artery pseudoaneurysm. Clin Radiol 2002;57(4):308–11. [DOI] [PubMed]


