Abstract
Alcoholism treatment often encourages involvement in Alcoholics Anonymous (AA). Little provision is made for women with social phobia (SP), who have been reported to have worse outcomes in twelve-step-facilitation (TSF) relative to cognitive behavioral therapy. This study examined whether SP moderated the effects of gender for these women in TSF. 133 SP alcoholics assigned to TSF (35 females and 98 males) in Project MATCH were compared to a non-SP control group. SP women drank earlier and more intensely than non-SP women and all males, had equivalent AA attendance and completion of Step 5, and were less likely to acquire a sponsor during TSF.
Keywords: Social anxiety, social phobia, alcoholism, alcohol dependence, alcoholics anonymous, AA Sponsor, twelve step treatment, gender, women, drinking outcome
Introduction
The twelve-step model is the prevailing therapeutic approach for treating substance abuse in the United States, and referral to Alcoholics Anonymous (AA) is common across different kinds of therapeutic approaches. As such, understanding the nature and magnitude of AA-related benefit has been assigned a high priority, especially within the context of the evidence-based movement. In general, prospective studies (e.g., Tonigan and Bogenschutz 2008; Moos and Moos 2006; Weiss, Griffin, and Gallop 2000) and meta-analytic reviews of the extant AA literature (e.g., Forcehimes and Tonigan 2008; Tonigan, Toscova, and Miller 1996) are in agreement that AA offers modest yet positive benefit for many problem drinkers. Additional findings converge suggesting that engagement in, and commitment to, AA is a stronger predictor of success than sheer frequency of AA meeting attendance (e.g., Montgomery, Miller, and Tonigan 1995; Weiss, Griffin, and Gallop 2000) and that social network support for abstinence found in AA explains, in part, AA benefit (e.g., Humphreys et al. 1999; Kaskutas, Bond, and Humphreys 2002; Longabaugh 1999).
About 1 in 5 alcohol dependent adults have co-occurring social phobia (SP) (Randall, Thomas, and Thevos 2001). However, it is not clear how, if at all, social phobia may interfere with the treatment approaches found to promote the highest yields of AA-related benefit. In essence, social phobia, also referred to as social anxiety disorder, is a fear of scrutiny in social situations. People either endure the anxiety or avoid situations where discomfort may be a problem (American Psychiatric Association 2000). Given that many of the documented predictors of AA-related benefit emanate from prescribed social interactions, it would appear that individuals with social phobia would derive less benefit from AA affiliation relative to those people without social phobia.
Book and colleagues recently reported results of a survey of 103 subjects enrolled in intensive outpatient treatment programs for addiction to alcohol or illicit drugs (Book et al. in press). Seventy-three of the subjects were women. They compared the 38 subjects (27 women) with high scores on a social anxiety rating scale to those with lower scores on their willingness to participate in addiction treatment activities. Individuals with social anxiety were significantly less willing to speak up in group therapy, talk to their therapist, attend a 12-step meeting, or ask for a sponsor. Although this primarily female group with social anxiety appeared to have significant barriers to effective treatment in a 12-step model, this study did not evaluate addiction treatment outcome.
Terra and colleagues (2006) examined the impact of having social phobia (SP) on both AA participation and alcohol treatment outcomes in a single group naturalistic study (Terra et al. 2006), and found mixed results. Specifically, they recruited 300 alcohol dependent individuals presenting for treatment in Brazil and then interviewed these study participants at 3 and 6-month follow-up. Twenty-four percent of the sample was diagnosed via the DSM-IV criteria as having mild, moderate, or severe SP (no difference in SP rates by gender). AA referral was made through physician advice and did not follow any systematic protocol. Overall, no differences in relapse rate and AA attendance at 3 and 6-month interviews was found between those with and without SP, although SP participants reported chairing AA meetings significantly less frequently at both interviews relative to non-SP participants. Further, SP participants reported that they did not feel as good after an AA meeting as did non-SP participants and the SP group also reported feeling significantly more shame about going to AA. Acknowledged by Terra et al., however, rates of AA attendance were extremely low in this study (e.g., 10 out of 64 of SP, and 42 out of 202 of non-SP), with statistical tests frequently based upon fewer than 5 adults endorsing a particular AA-related behavior.
Work by Thevos and colleagues (Thevos et al. 2000) suggests that the interaction between formal treatment, social phobia, and AA participation may be more complex than that reported by Terra et al (2006). In a post hoc analysis of the Project MATCH database, 261 subjects (188 males, 73 females) with alcohol dependence were randomized to either Twelve Step Facilitation (TSF) or Cognitive Behavioral Therapy (CBT), were permitted to attend AA during treatment, and were followed both during treatment and for 12 months after the completion of treatment. Consistent with Terra et al (2006), results showed that alcohol dependent individuals with social phobia fared equally well as those without social phobia in terms of alcohol quantity and frequency, and many of these subjects received 12-step focused treatment in Project MATCH and attended AA after treatment. Unlike Terra et al (2006), however, and in line with the findings of Book et al (in press), Thevos and colleagues also reported that social phobia and the gender of the alcoholic interacted such that females with social phobia fared less well when assigned to 12-step treatment relative to cognitive behavioral therapy. Males with and without social phobia fared equally well in both treatments.
This study aims to further investigate the reasons why female alcoholics with social phobia fared less well when assigned to 12-step therapy. Unresolved by Thevos et al., for example, was whether the poorer outcome for socially phobic female alcoholics assigned to TSF stemmed, in part, from their inability to meaningfully engage in AA after treatment, a time of high relapse rates. Cognizant of the social phobia and gender interaction, this study offers to map the trajectory of specific AA-related behaviors of four groups of alcoholics (female SP and non-SP, and male SP and non-SP), all of whom received TSF (Nowinski, Baker, and Carroll 1994).
Methods
Project MATCH was a large randomized clinical trial (N = 1,726) investigating the relative effectiveness of Motivational Enhancement Therapy (Miller et al. 1995), Cognitive Behavioral Therapy (Kadden et al. 1995), and Twelve Step Facilitation Therapy (TSF) (Nowinski, Baker, and Carroll 1994), with the specific objective of identifying what types of alcoholics fared better when assigned to a particular treatment. Alcoholics were recruited at 13 locations in the United States, which were divided according to whether they were presenting for outpatient (N = 952) or inpatient aftercare treatment (N = 774). Clients in both arms of the study received individualized and manual-guided therapy for 12 weeks, and in-person follow-up interviews were conducted in 3-month increments for 12 months after treatment. Reported elsewhere (Project MATCH Research Group 1997, 1998), the fidelity of the therapeutic protocols was good (Carroll et al. 1998), follow-up rates were excellent (Project MATCH Research Group 1997, 1998), and self-reported alcohol use was corroborated by collateral report and urine toxicology (Project MATCH Research Group 1997). This study sample focuses only on the 133 participants with social phobia and 133 matched control participants without social phobia who were randomly assigned to TSF.
Measures
The Alcoholics Anonymous Involvement tool (AAI) (Tonigan, Connors, and Miller 1996) has 13-items and yields a total score of overall AA involvement as well as program and fellowship scales. AA program behaviors include: (1) reading AA literature, (2) progress in working the 12 steps of AA, (3) having or being an AA sponsor, and (4) prayer and meditation. AA fellowship behaviors include: (1) AA meeting attendance, and (2) celebrating AA birthdays and AA social interactions. The AAI has demonstrated psychometric properties and strong convergence with other measures collecting information on the frequency of AA meeting attendance, (e.g., r = .70 between AAI and the Form 90 semi-structured interview). The Form 90 (Miller and Del Boca 1994) was used to measure day-by-day substance use. Primary drinking variables in Project MATCH included percent days alcohol abstinence (PDA) aggregated on a monthly basis and drinks per drinking day (DDD).
Diagnosis of social phobia (SP) was assessed with the C-DIS, which mirrored criteria in the DSM-III-R for SP. The C-DIS is a computerized version of a structured clinical interview designed by the National Institute of Mental Health, the Diagnostic Interview Schedule (DIS) and has documented reliability and validity (Robins et al. 1989).
Results
A total of 582 alcoholics were assigned to Twelve Step Facilitation (TSF) in the outpatient (N = 335) and aftercare (N = 247) arms of the study, and 133 (23%) of these people were diagnosed by the C-DIS as having social phobia (SP). Table 1 provides selected characteristics of this comorbid sub-sample along with the characteristics of a matched sub-sample of alcoholics assigned to TSF who did not have social phobia (non-SP). Non-SP subjects were matched to SP subjects on age, gender, and treatment arm. Groups were relatively equivalent in regards to all other non-matched characteristics shown in Table 1. Importantly, no differences were found in alcohol use quantity and frequency as measured by baseline percentage abstinent days (PDA) or drinks per drinking day (DDD). Additionally, no proportional differences were found between those alcoholics with and without social phobia in baseline rates of marriage, living alone, and prior frequency and engagement in AA. Also of importance, any difference in outcome cannot be attributed to differences in the number of treatment sessions attended since both groups attended an average of about 8 of the 12 sessions.
Table 1.
Baseline Characteristics of Alcoholics with and without Social Phobia Assigned to Twelve Step Facilitation
| Non Social Phobia (n = 133) |
Social Phobia (n = 133) |
p | |
|---|---|---|---|
| Gender-% female (n) | 26% (35) | 26% (35) | .99 |
| Age (±SD) | 39.43 (10.71) | 39.22 (10.48) | .87 |
| Years Education (±SD) | 13.19 (2.14) | 12.86 (2.06) | .20 |
| % Never Married (n) | 24.1% (32) | 30.1% (40) | .44 |
| % Living Alone (n) | 21.1% (28) | 23.3% (31) | .38 |
| % Caucasian (n) | 74.4% (99) | 78.9% (105) | .60 |
| % with Health Insurance (n) | 43.6% (58) | 47.4% (63) | .14 |
| Percent Days Abstinent (±SD) | .30 (.32) | .30 (.30) | .50 |
| Drinks per Drinking Day (±SD) | 18.20 (11.19) | 17.76 (10.74) | .55 |
Treatment outcome
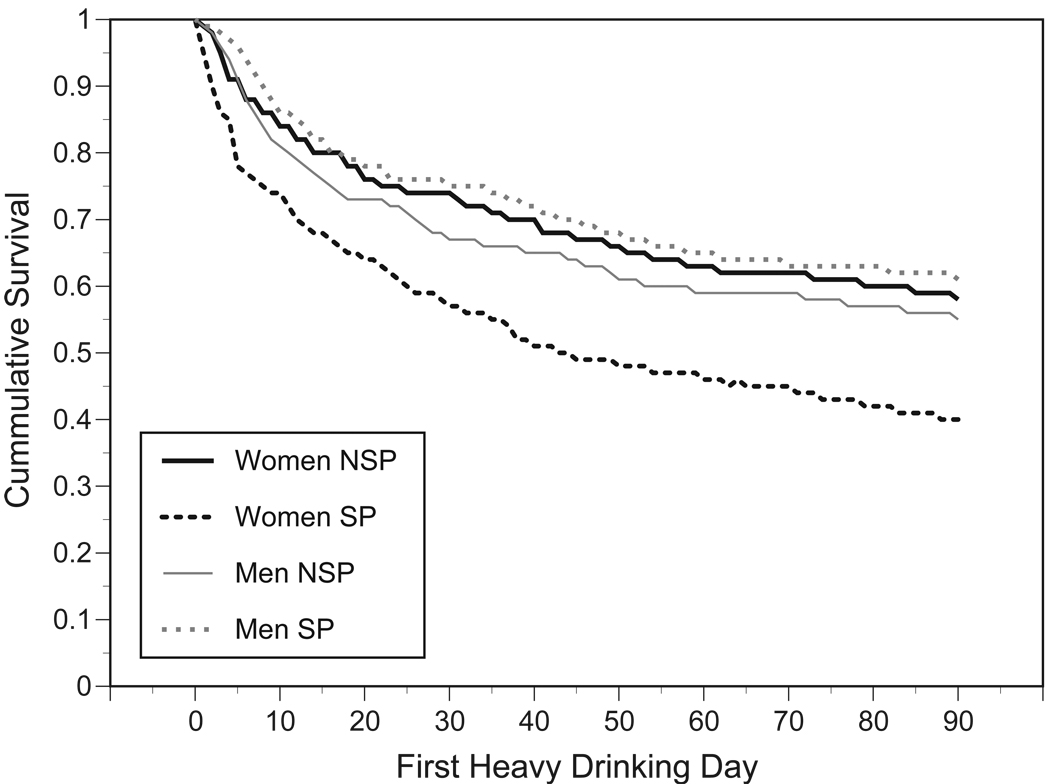
Figure 1 displays a survival analysis that contrasted, in days, SP and non-SP relapse rates to heavy drinking by gender (defined as 4 standard drinks for females and 6 standard drinks for males). Indicative of the interaction reported by Thevos et al. (2000), rates of relapse to heavy drinking was relatively equivalent for males with and without SP (about 60% of both SP and non-SP males had not relapsed prior to the end of treatment). In contrast, by the end of treatment about 60% of the females without social phobia did not relapse to heavy drinking while only 40% of the females with social phobia had not relapsed, (X2 (3) = 12.05, p < .03). Why, then, given the similarity between SP and non-SP alcoholics on demographic, drinking, and therapy compliance measures, did females with SP fare so poorly in 12-step therapy?
Figure 1.
Days to First Heavy Drinking Day by Gender and Social Phobia Status: Time to Relapse Among 12-Step Therapy Clients
AA Attendance
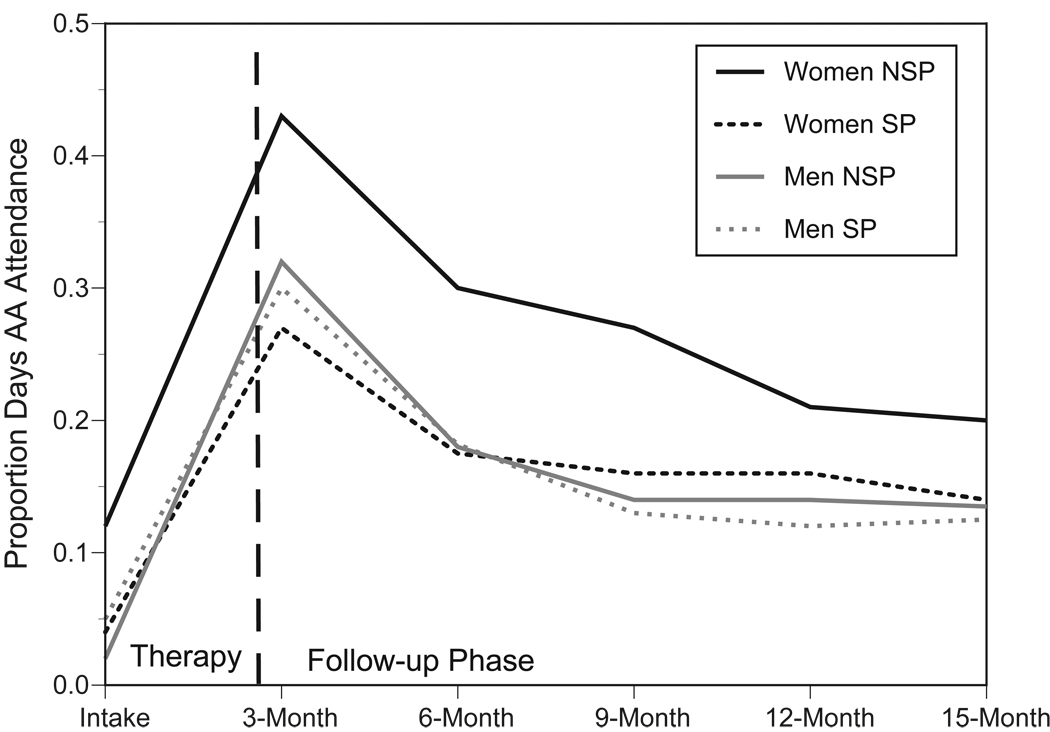
Figure 2 shows the mean rates of AA attendance for males and females with and without SP immediately before treatment through the 12-month follow-up. Repeated measure MANOVA with baseline values of proportion AA days used as a covariate, two between-subject factors (gender and SP status), and 1 within-subject factor (5 levels, proportion days AA attendance) indicated that rates of AA attendance did not differ by gender, F (1, 239) = 1.22, p < .27, SP status, F (1, 239) = 1.74, p < .19, or by the gender × SP status interaction, F (1, 239) = .36, p < .55. Overall, high rates of AA attendance were achieved between intake and end of 12-step treatment (3-month). AA attendance appeared to erode across the 12 months of follow-up, with the most rapid decay occurring the first three months after treatment ended (months 4–6). This pattern of AA attendance was unrelated to SP status, gender, or the interaction of gender × SP status.
Figure 2.
Proportion Days AA Attendance by Gender and Social Phobia Status: 12-Step Therapy and AA Attendance
Alcoholics Anonymous (AA) Engagement
Two core AA prescribed behaviors, ones that both emphasize and require intimate social interaction, behaviors expected to be difficult for socially phobic individuals, were tested, including the percentage of women with and without social phobia that reported having a sponsor as well as those reported having completed a 5th step (sharing of ones personal inventory, step 4, with another, generally a sponsor).
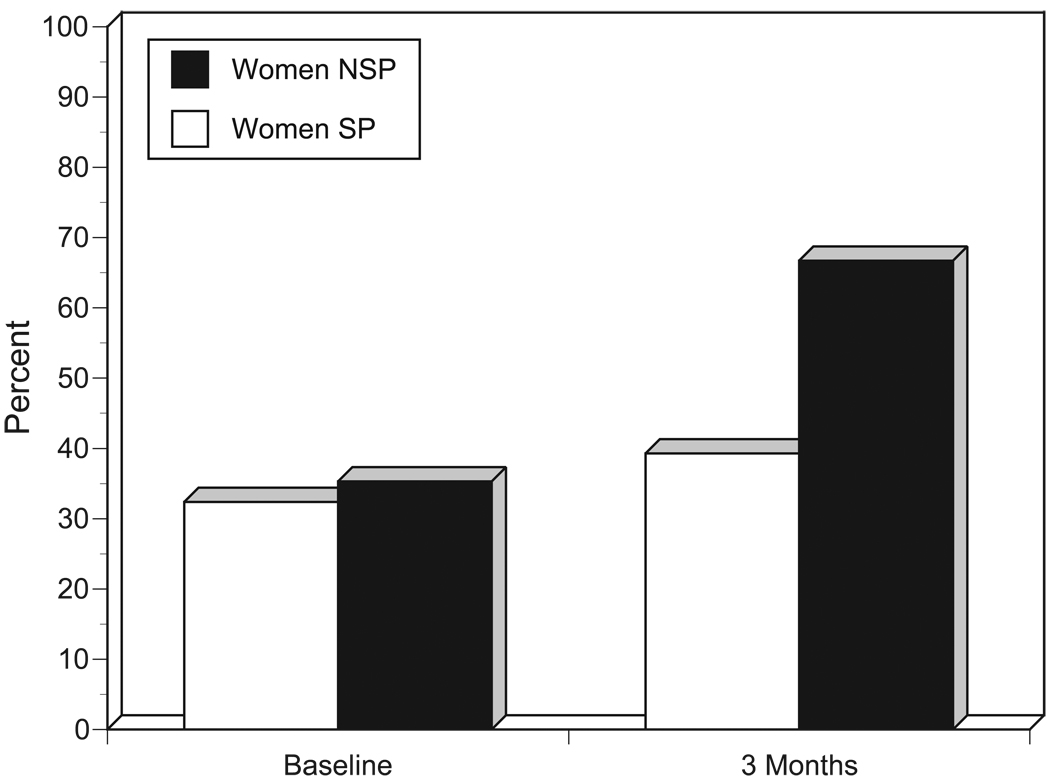
A total of 6 hierarchical logistic regressions were done, one for each follow-up (3, 9, and 12 month following end of treatment) for the two AA prescribed behaviors. Intake responses (yes/no dummy coded) were entered in step 1, step 2 entered the dummy coded variable indicating SP status, and the criterion measure was the follow-up yes/no response to having a sponsor or completion of step 5. No relationships between SP status and the completion of step 5 were found at any of the 3 follow-up periods nor was there any relationship between whether a woman had completed a 5th step in the past (intake, lifetime) and then reported repeating a 5th step at follow-up. However, consistent with prediction, women with SP were significantly less likely to acquire a sponsor by the 3-month follow-up relative to NSP women (Wald (1) = 5.23, p < 022). At 9-months, this same relationship was no longer significant, but was observed at the trend level, (Wald (1) = 1.87, p < .17), although the relationship was completely absent at the 12-month follow-up, (Wald (1) = 1.47, p < .23). Figure 3 shows the differences in the percentages of alcoholics with and without social phobia who obtained a sponsor. These percentages indicate that 12-step therapy was effective in facilitating the acquisition of a sponsor among women without SP who had never had a sponsor in the past. In contrast, the women with SP were less likely to acquire a sponsor during treatment.
Figure 3.
Percent of Alcoholics with and without Social Phobia having an AA Sponsor at Baseline and at 3-month Follow-up
Discussion
Alcohol dependency and social phobia are frequently co-occurring disorders and prior work suggested that 12-step therapy, the prevailing therapeutic model in the United States, may not be equally effective for alcoholic women with and without social phobia. This study investigated whether differential AA attendance or commitment to, and practice of, prescribed 12-step behaviors accounted for the relatively poor outcomes of socially phobic women assigned to 12-step therapy. Overall, the number of similarities in the ways that women practiced prescribed AA behaviors outweighed the differences between women with and without social phobia. As examples, during and after treatment, women with and without social phobia tended to report attending roughly the same number of AA meetings, and patterns of decay in AA attendance over 12 months was also similar regardless of social phobia status among women assigned to 12-step therapy. Likewise, there was no proportional difference in completing a 5th step between the two groups.
Noteworthy, socially phobic women reported, in general, lower rates of acquiring an AA sponsor during therapy, and rates of getting an AA sponsor for the first time among this group were even lower. Given the documented value of sponsorship for achieving and sustaining abstinence (Sheeren 1988; Witbrodt and Kaskutas 2005) this apparent deficit for alcoholic socially phobic women may be an important factor accounting for relatively poor outcomes for this group. Study findings more clearly amplify the work of Terra et al (2006) that suggested that adults with SP might engage in AA in ways that are distinct from non-SP alcoholics. Specifically in severely underpowered analyses they suggested that some SP adults were less likely to assume roles of responsibility in AA and that they viewed the benefits of AA less favorably. Findings from this study parallel this interpretation, but do so from the perspective of a longer-term follow-up and a more rigorous prospective design.
Various clinical strategies to address a sponsorship deficit ought to be considered when SP women are offered 12-step therapy. First, therapeutic efforts to facilitate the acquisition of a sponsor ought to begin in the early phase of therapy for SP women. Typically, 12-step therapy begins with first promoting cognitive shifts that are consistent with AA ideology, (e.g., accepting powerlessness over alcohol, followed by more behaviorally anchored objectives) such as sponsorship. Work suggests, however, that few AA-related behaviors are initiated after treatment (Tonigan, Conners, and Miller 2003). Given the apparent difficulties faced by SP women in acquiring an AA sponsor, it seems prudent to allow sufficient therapeutic time to aid SP women in this endeavor. Second, and related, SP women may benefit from focused social skill training aimed at asking an AA member to become a sponsor. Here, training may include effective ways to get phone numbers, dealing with rejection, and understanding the nature of the sponsee-sponsor relationship.
The present study has some limitations. Despite the large sample in Project MATCH, some of the sites were predominately male and the sample of women is small, as is the sub-sample of women with social phobia. In addition, the diagnosis of social phobia was made with a computerized survey, the C-DIS, which has been demonstrated to over diagnose Axis I diagnoses relative to the Structured Clinical Interview for Diagnosis (SCID), which is considered the gold standard (Ross et al. 1995). Further, although it is not altogether clear from these analyses whether these finding are based on a gender by social phobia interaction, as compared to main effect for social phobia within the female group, future studies could further clarify this. Additionally, this study was retrospective in nature, using an existing database, rather than a prospective design, and as such suffers from the same limitations as the parent study, Project MATCH (e.g. excluding most other drug dependence and homeless individuals), which may limit its generalizability.
In sum, findings suggest that the study of social phobia and AA engagement is complex. Efforts to identify only the main effects of social phobia on drinking outcomes and AA attendance are likely to miss critical nuances that will result in making erroneous conclusions. This study, for example, did report that SP by itself was largely unrelated to how frequently one attended AA or how one became engaged in AA. The consideration of alcoholic gender, however, showed that female alcoholics with SP fared significantly worse in 12-step therapy and that this outcome may be related to the failure to acquire an AA sponsor.
Acknowledgements
This work was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (K02 AA00326 to Dr. Tonigan), (K23 AA014430 to Dr. Book); (P50 AA010761 to Dr. C. Randall); (K24 AA013314 to Dr. C. Randall), (K01 AA015137-12 to Dr. Pagano).
The authors would like to thank Ms. Nancy White, and Mr. Adam G. Mace for their enthusiastic assistance with this project.
Contributor Information
J. Scott Tonigan, Department of Psychology, University of New Mexico, Albuquerque
Sarah W. Book, Charleston Alcohol Research Center, Medical University of South Carolina, Charleston, SC
Maria E. Pagano, Case Western Reserve School of Medicine, Department of Psychiatry, Division of Child Psychiatry, Cleveland, OH
Patrick K. Randall, Charleston Alcohol Research Center, Medical University of South Carolina, Charleston, SC
Joshua P. Smith, Charleston Alcohol Research Center, Medical University of South Carolina, Charleston, SC
Carrie L. Randall, Charleston Alcohol Research Center, Medical University of South Carolina, Charleston, SC
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revision: DSM-IV-TR. 4th-TR ed. Washington, DC: 2000. [Google Scholar]
- Book SW, Thomas SE, Dempsey JP, Randall PK, Randall CL. Social anxiety impacts willingness to participate in addiction treatment. Addictive Behaviors. doi: 10.1016/j.addbeh.2008.12.011. in press. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Kadden RR, Longabaugh RL, Rounsaville BJ, Wirtz PW, Zweben A. Internal validity of Project MATCH treatments: Discriminability and integrity. Journal of Consulting & Clinical Psychology. 1998;66(2):290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- Forcehimes A, Tonigan JS. Self-efficacy to remain abstinent and substance abuse: A Meta-Analysis. Alcoholism Treatment Quarterly. 2008;26(4):480. [Google Scholar]
- Humphreys K, Mankowski ES, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Annals of Behavioral Medicine. 1999;21(1):54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- Kadden RC, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Litt M, Hester R. Cognitive Behavioral Coping Skills Therapy Manual. In: Mattson ME, editor. Project Match Monograph Series. Vol. 3. Rockville: US Department of Health and Human Services; 1995. [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R. Matching alcohol treatment to patient social support and the effects of participation in Alcoholics Anonymous. Medicine & Health, Rhode Island. 1999;82(4):122. [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol Supplement. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual. In: Mattson ME, editor. Project Match Monograph Series. Vol. 2. Rockville: US Department of Health and Human Services; 1995. [Google Scholar]
- Montgomery HA, Miller WR, Tonigan JS. Does Alcoholics Anonymous involvement predict treatment outcome? Journal of Substance Abuse Treatment. 1995;12(4):241–246. doi: 10.1016/0740-5472(95)00018-z. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Participation in treatment and Alcoholics Anonymous: A 16-year follow-up of initially untreated individuals. Journal of Clinical Psychology. 2006;62(6):735–750. doi: 10.1002/jclp.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve Step Facilitation Therapy Manual. In: Mattson ME, editor. Project Match Monograph Series. Vol. 1. Rockville: US Department of Health and Human Services; 1994. [Google Scholar]
- Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Treatment main effects and matching effects on drinking during treatment. Project MATCH Research Group. Journal of Studies on Alcohol. 1998;59(6):631–639. doi: 10.15288/jsa.1998.59.631. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism: Clinical and Experimental Research. 2001;25(2):210–220. [PubMed] [Google Scholar]
- Robins L, Helzer J, Cottler L, Goldbring E. NIMH Diagnostic Interview Schedule: Version III Revised (DIS-III-R) St. Louis, MO: Washington University; 1989. [Google Scholar]
- Ross HE, Swinson R, Doumani S, Larkin EJ. Diagnosing comorbidity in substance abusers: A comparison of the test-retest reliability of two interviews. American Journal of Drug & Alcohol Abuse. 1995;21(2):167–185. doi: 10.3109/00952999509002686. [DOI] [PubMed] [Google Scholar]
- Sheeren M. The relationship between relapse and involvement in alcoholics anonymous. Journal of Studies on Alcohol & Drugs. 1988;49(1):104–106. doi: 10.15288/jsa.1988.49.104. [DOI] [PubMed] [Google Scholar]
- Terra MB, Barros HMT, Stein AT, Figueira I, Jorge MR, Palermo LH, Athayde LD, Goncalves MS, Spanemberg L, Possa MA, Filho L Daruy, Da Silveira DX. Social anxiety disorder in 300 patients hospitalized for alcoholism in Brazil: High prevalence and undertreatment. Comprehensive Psychiatry. 2006;47(6):463–467. doi: 10.1016/j.comppsych.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Thevos AK, Roberts JS, Thomas SE, Randall CL. Cognitive behavioral therapy delays relapse in female socially phobic alcoholics. Addictive Behaviors. 2000;25(3):333–345. doi: 10.1016/s0306-4603(99)00067-2. [DOI] [PubMed] [Google Scholar]
- Tonigan J, Connors GJ, Miller WR. Alcoholics Anonymous Involvement (AAI) scale: Reliability and norms. Psychology of Addictive Behaviors. 1996;10(2):75–80. [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: Sample and study characteristics moderate findings. Journal of Studies on Alcohol & Drugs. 1996;57(1):65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- Tonigan J Scott, Conners GJ, Miller WR. Participation and involvement in alcoholics anonymous. In: Babor TF, Del Boca FK, editors. Treatment Matching in Alcoholism. Cambridge: Cambridge University Press; 2003. [Google Scholar]
- Tonigan JS, Bogenschutz MP. Utilization of formal treatment and AA: Relative contributions to early abstinence. Alcoholism: Clinical & Experimental Research: Supplement. 2008;32(6):695. [Google Scholar]
- Weiss RD, Griffin ML, Gallop R. Self-help group attendance and participation among cocaine-dependent patients. Drug & Alcohol Dependence. 2000;60:169–177. doi: 10.1016/s0376-8716(99)00154-4. [DOI] [PubMed] [Google Scholar]
- Witbrodt J, Kaskutas LA. Does diagnosis matter? Differential effects of 12-Step participation and social networks on abstinence. American Journal of Drug & Alcohol Abuse. 2005;31(4):685–707. doi: 10.1081/ada-68486. [DOI] [PubMed] [Google Scholar]