Abstract
Neonatal mortality is a major health problem in low and middle income countries and the rate of improvement of newborn survival is slow. This article is a review of the PhD thesis by Mats Målqvist, titled ‘Who can save the unseen – Studies on neonatal mortality in Quang Ninh province, Vietnam,’ from Uppsala University. The thesis aims to investigate structural barriers to newborn health improvements and determinants of neonatal death. The findings reveal a severe under-reporting of neonatal deaths in the official health statistics in Quang Ninh province in northern Vietnam. The neonatal mortality rate (NMR) found was four times higher than what was reported to the Ministry of Health. This underestimation of the problem inhibits adequate interventions and efforts to improve the survival of newborns and highlights the invisibility of this vulnerable group.
The findings of the thesis also point at an inequity in survival chances based on ethnicity of the mother. Newborns of ethnic minority mothers were at a twofold risk of dying within the first 4 weeks of life compared to their peers belonging to the hegemonic group of Kinh (OR 2.08, 95% CI: 1.39–3.10). This increased risk was independent of maternal education and household economic status. Neonatal mortality was also associated with home deliveries, non-attendance to antenatal care and distance to the health care facilities. However, ethnic minority mothers still had an increased risk of experiencing a neonatal death even if they attended antenatal care, delivered at, or lived close to a health facility. This example of ethnic inequity highlights the importance to target those most in need.
Keywords: neonatal mortality, inequity, ethnic minorities, care seeking, delivery care utilisation, under-reporting, Vietnam

Nearly four million newborns die during the first 4 weeks of life each year and world-wide neonatal mortality makes up 40% of the total child mortality (1, 2). With an annual number of births in the world reaching 130 million, this means that the overall neonatal mortality rate is about 30/1,000. This is a level that has gone basically unchanged for the past 50 years, despite minor improvements (3). However, recently there has been an increasing focus on the neonatal period among researchers and policy makers calling for action (4, 5), as well as some evidence of an accelerating improvement during the past few years (6). One reason for the stagnant development in neonatal survival might be found in global inequity. While Sweden and the rest of the industrialised sector maintain a neonatal mortality rate of 2–3/1,000, it is not uncommon that this rate reaches over 60/1,000 in the poorer segments of the world (6). Ninety-nine (99%) of all children who die during the first 4 weeks of life are doing so in the poorer parts of the world, especially in sub-Saharan Africa and South Asia (7).
In order for interventions that improve the chances for neonatal survival to be put into practice, demand and supply need to meet: there should be enough resources and knowledge among care providers, as well as adequate care-seeking behaviours, and a readiness and willingness to utilise the existing health system among families. To have skilled attendance at birth might avert a large proportion of all intrapartum-related neonatal deaths if good coverage is reached (8, 9). A person with knowledge about and experience of difficult situations and potential delivery complications is taken for granted (and is almost expected as the ‘norm’) in most high-income countries. Yet, in many places of the world this is not the norm and, globally, 65.7% of all pregnant women deliver without a skilled attendant (2008 estimate). In Asia, the skilled attendance rate is as low as 46.5% (10). In fact, the definition of skilled attendance at birth involves two components – both the presence of skilled health personnel as well as an ‘enabling environment,’ which means adequate supplies and equipment, possibilities for transport, and effective communications (10). The recognition of needing to strengthen these parts could also be expressed as understanding the importance of where a delivery takes place (11). Any complications that might arise during delivery, for mother or child, need immediate attention; and the time to intervene is short (9). Being at the right place at the time of delivery therefore considerably increases the chances of neonatal and maternal survival (12, 13). Previous results from our research group in Vietnam showed, for example, a strong link between home delivery rate (HDR) and NMR at district level (14).
Another important aspect of safe motherhood and delivery is care-seeking. Moreover, the decision to seek appropriate care at the time of delivery, as well as the road to ensuring a safe delivery is an important determinant of neonatal outcome. In a widely cited review article from 1994, Thaddeus and Maine present a conceptual framework of three delays in care-seeking (15). The first delay potentially occurs during the time it takes from onset of a condition requiring medical attention until the decision to seek care is taken. The second delay is the time it takes from once the decision to seek care is made until a health facility is reached. The third delay is the time it takes from arrival at a health facility until appropriate and adequate care is commenced. Thaddeus and Maine developed their conceptual framework for obstetric emergencies, but the same mechanisms are valid for preventive care-seeking for delivery, and Gabrysch and Campbell have expanded the framework to involve this aspect as well (16).
Vietnam is a country that for many years has shown relative good health statistics in relation to its overall economic status. Through sustained investments in primary health care, Vietnam has achieved great reductions in infant and child mortality rates (17). Officially, the NMR in Vietnam is 12/1,000 2004 (18). However, a study in Bavi district, a health surveillance site west of Hanoi, showed a persistent neonatal mortality rate over the last three decades of the last century (19) exhibiting the same trend as has been shown in many other countries around the world. The Bavi study not only showed a stagnant neonatal mortality, but also indicated that ethnicity was a major risk factor for neonatal death, whereas education and economic status was not. Ethnic minorities in Vietnam are living in more remote mountainous areas compared to the hegemonic ethnic group (Kinh), and there was a sharp social inequity arising from minority status (20).
Aims
Neonatal mortality has long been a neglected problem in the world with stagnant development over the past decades. Previous studies within our research group have verified this limited development in Vietnam with persistent neonatal mortality despite major improvements in overall under-five survival. The Vietnamese setting is thus offering a model for the exploration of obstacles for improved neonatal survival. Such obstacles can be found in societal structures as well as in patterns of behaviour at an individual level. Stimulating development requires the acquisition of reliable data as well as a proper understanding of socio-economic and proximate determinants of neonatal death. The overall aim of the thesis was, therefore, to study and assess factors associated with neonatal mortality with special emphasis on structures within society and the health care system in Quang Ninh Province. Specific aims were to analyse the rate and sources of information on neonatal mortality and to identify and assess socio-economic and proximate determinants of neonatal mortality including care-seeking patterns, place of delivery, and distance to health facilities.
Conceptual framework
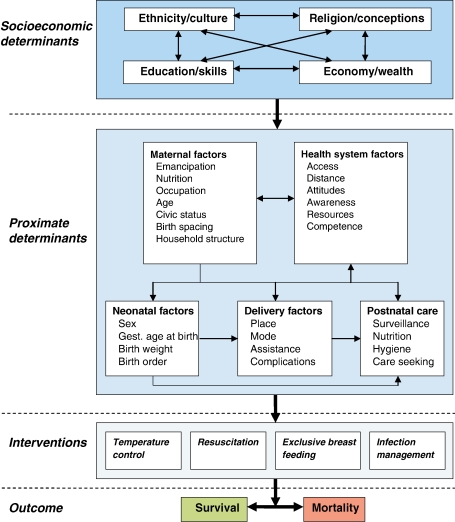
The conceptual framework here presented is adopted from Mosley and Chen, who in 1984 suggested an analytical framework for child health studies (21), which has since been widely used. Mosley and Chen tried to combine sociological and biological explanatory models into a single conceptual framework by sorting independent variables as either socio-economic (distal) determinants or proximate determinants, creating a hierarchy for analysis. Victora and colleagues further stress this hierarchical approach when they claim that a common mistake in epidemiological literature is to analyse distal and proximate factors as being at the same level, which results in a reduction or elimination of the former's effects (22). The model set up by Mosley and Chen has later been adapted to fit specific areas, for example HIV/AIDS (23), neonatal health (24), and maternal mortality (25), and the framework here presented is a further adaptation for the analysis of neonatal mortality risk factors (Fig. 1).
Fig. 1.
Conceptual framework for factors influencing neonatal mortality, adapted from Mosley and Chen (21).
The socio-economic determinants in the model are ethnicity/culture, religion/conceptions, education/skills, and economy/wealth. The arrows in the model suggest that all the socio-economic determinants are interrelated and affecting each other. For example, is the level of education affecting the amount of income, generating wealth, or sustaining poverty, while at the same time a high economic status increases the possibilities for a better education. Even in Vietnam, being a communist country, this is valid, especially with the transformation from planned to market economy and rapid economic development of recent years. The influence of maternal educational level on child health has been explored in many studies. In a seminal paper from studies on maternal mortality in Nigeria in 1979, Caldwell discusses the reason that well educated mothers have better health indicators as being due to their ability to better understand and use the health system, compared to their less educated peers (26). It would also be reasonable to assume that mothers with higher education are more prone to internalise and adopt new knowledge and behaviour for the benefit of themselves and their offspring. The impact of household economy on neonatal survival could be both direct – through payment capacity directly related to delivery or sickness – and indirect, by the manifestation of better nutritional status. In Vietnam, there are now user fees in the health care system, both official as well as unofficial (27). However, if a family is poor, it can obtain a certificate from the authorities stating their low economic capacity and thereby assuring them health care free of charge (at least when it comes to official fees). Religion and conceptions about life influence cultural pre-understanding as well as how to relate to wealth and education. Religious beliefs and customs also affect neonatal health and the chances for survival such as the Vietnamese tradition of not considering a newborn child fully human until it has reached 1 year of age (28). Another factor that could greatly influence the care and survival of newborns: the preference for sons, which is closely related to patrilinearity and patriarchal structures (29) and in the end affects the decision-making power of women. Vietnam for many years has had a two-child policy, and the desire to breed sons together with an increased spread of ultrasound has in recent years led to a sex ratio at birth well above normal variations (30).
The proximate determinants in the model are divided into five categories: maternal factors, health system factors, neonatal factors, delivery factors, and postnatal care. In most models, there is no hierarchy among the proximate determinants and it is not strictly in this model either. However, by putting maternal and health system factors above the other groups acknowledges the circumstance that these two have a significant impact not only on the outcome but also on the three other groups. Characteristics of the mother are of great importance when it comes to birth weight and even the sex of the newborn. The level of female emancipation may decide where the delivery takes place and who is assisting (31, 32). Further, characteristics of the health system, for example attitudes and availability, greatly influence delivery place (33) and the postnatal care (34, 35). Notable is that not all arrows between proximate determinants are two-way. The characteristics of postnatal care do not, for example, influence the neonatal factors, whereas the sex of the baby may have a considerable impact on the postnatal care. Maternal factors are not easily affected by the other groups but, of course, have a major influence on the choice of delivery place and the quality of postnatal care.
In the end, the difference between death and survival in the neonatal period is dependent upon what responses are given to the newborn's needs and to the threats to the neonates' health. Most of the interventions needed to save newborn lives are not complicated, costly, or high-tech but, instead, simple and straightforward with a potential of reducing mortality with up to two-thirds (8). With the addition of resources and the latest medical technology, it is possible to save almost all newborns, as statistics from Singapore exhibit, further emphasising the importance of actions taken or not taken (36). The interventions in the model are examples based on priorities made by WHO.
Methods
NeoKIP
The studies here presented are parts of a population-based cluster randomised study called NeoKIP (Neonatal Health – Knowledge Into Practice, ISRCTN44599712), initiated by Uppsala University in Sweden, the Ministry of Health in Vietnam and the Vietnam – Sweden hospital in Uong Bi, Vietnam. A baseline survey in the whole province was performed in 2006, registering all births and neonatal deaths occurring in 2005. The intervention of the NeoKIP study commenced in July 2008.
Study setting
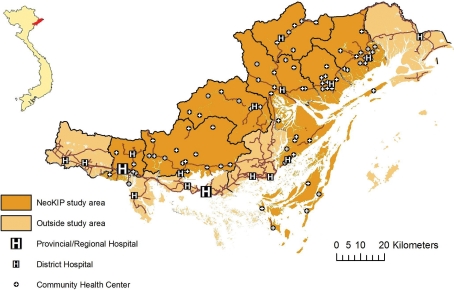
Quang Ninh province (QN) is situated in the north-east corner of Vietnam, sharing a border with China in the north. The province inhabits a little more than a million people and is currently undergoing rapid economic development. In Quang Ninh province, there are 10 different ethnic groups (Kinh, Dao, San Chi, San Diu, Tay, Hoa, Cao Lang, Thanh Y, Thanh Phan, and Chinee) with Kinh being the majority group constituting about 80% of the population (37). There are 14 districts in Quang Ninh province, of these, 8 districts had a neonatal mortality rate (NMR) higher than 15/1,000 2005 according to NeoKIP baseline results and were identified and chosen to constitute the study area (Fig. 2). In 2005 there were 17,519 births in the province, and the NMR was 16/1,000 (38).
Fig. 2.
Quang Ninh province in northern Vietnam.
The health care system in Quang Ninh province follows the national guidelines, with at least one community health centre (CHC) in each community and one district hospital (DH) in all district centres. In Ha Long City, the administrative centre of the province, there is a newly built provincial hospital with referral capacity, and in Uong Bi there is a regional hospital serving not only Quang Ninh but also the surrounding provinces. Women are free to go for antenatal care at any provider and there are many private ANC providers in the province, many of them specialised in ultrasound examinations. There are no private delivery care providers in QN.
Study designs, population, and sample size
We have analysed data from the NeoKIP baseline study, performed in early 2006, using a retrospective cross-sectional design registering all live births (n=17,519) and neonatal deaths (n=284) that occurred within the province during 2005. The neonatal mortality rates thus retrieved were compared to the official statistics reported to the MoH (38, 39).
Furthermore, data from the NeoKIP intervention database have been used, applying a case-referent design. All mothers within the NeoKIP study area who lost a newborn during the first month after delivery and during the time period from July 2008 to December 2009 (n=197) were approached for interview and 183 were available for interview. During interviews a semi-structured interview form was used. The same interview form was used to interview referent mothers randomly selected from the total population of live births.
Data collection
For the first two studies of the thesis (38, 39), data collection was mainly performed by compiling variables associated with deliveries and neonatal deaths. This information was derived from two major sources, health registers at all level of the health system and through group interviews with Village Health Workers. The WHO definitions of neonatal death and stillbirths were used by the NeoKIP data collectors to distinguish between death cases. Neonatal deaths were recorded by age, place of and assistance at delivery, place of death, birth weight, gestational age at birth, and gender. When a death case was found through any source, checking against the other sources on different levels was performed to verify each case.
For the two following studies of the thesis (40, 41), a team of data collectors recorded all live births in the eight districts constituting the NeoKIP study area on a monthly basis between July 2008 and December 2009 visiting health facilities and village health workers. All live births were entered into a database and once a month all new entries were grouped and assigned a number. By the use of a random number generator, 6% from each batch were selected as referents. With an estimated NMR of 20–25/1,000, a randomisation of 6% for referent interview assured a 2:1 ratio between referents and cases. Data collectors visited all sample mothers in their homes 8 to 10 weeks after delivery and conducted a semi-structured interview, gathering information about antenatal, delivery and postnatal care, as well as socio-economic factors.
GIS coordinates were collected by the use of handheld GPS devices (Garmin GPS 60 or Garmin GPS 60Cx). All governmental health facilities and homes of respondents were recorded and entered into the database. Geographic background information was obtained from VidaGIS, a Vietnamese-Danish commercial GIS provider.
From the results of interviews, an asset index was developed using principal component analysis in order to assess the economic status of respondents' household. This was done by an inventory of 15 different assets and household characteristics conducted in the homes of interviewees (motorbike, car, stereo, TV, DVD/VHS, refrigerator, washing machine, gas stove, electrical stove, electric fan, AC, glass windows, flush toilet, running water, and whether or not the household was connected to the power grid).
Ethical considerations
The research presented in this thesis was conducted within the NeoKIP study, which has been approved by the Ministry of Health in Vietnam (ref 3934/QD-BYT), the Provincial Health Bureau in QN, and the Research Ethics Committee at Uppsala University, Sweden (ref 2005:319). Informed oral consent was obtained from all respondents prior to interview.
Findings
Under-reporting of births and deaths
The official figures given by the Provincial Health Bureau of QN stated that 16,551 live births and 70 neonatal deaths had occurred in 2005, thus resulting in a neonatal mortality rate of 4/1,000. However, during the NeoKIP baseline, 17,519 live births and 284 neonatal deaths were registered to have occurred in Quang Ninh province in 2005. This resulted in a NMR of 16/1,000, thus four times higher than the official statistics. This substantial under-reporting was unevenly spread among the different districts of the province with a varying degree of discrepancy between official figures and NeoKIP baseline results.
Determinants of neonatal mortality
All neonatal deaths during 18 months (July 2008 to December 2009) in QN were registered as cases (n=197) and 6% of all live births during the same period were randomly chosen as referents (n=686). Mothers of 183 cases and 599 referents responded. Mean age of case mothers was 24.1 years and for referent mothers 25.4 years (p<.001).
Socio-economic determinants
Ethnic minority mothers constituted 38% of referent mothers (228/599) and 63% (130/183) of case mothers. This resulted in an elevated risk of neonatal mortality for ethnic minority mothers (COR 2.75, 95% CI: 1.94–3.91).
Maternal and paternal education co-varied and, hence, maternal education level was used alone. A larger proportion of case mothers had not completed primary school (less than 5 years) (29%) compared to referent mothers (18%). There were no differences in neonatal mortality risks between different levels of education once mothers had completed primary school. There was, however, an increased risk for mothers who had not attended school or done so less than five years, compared to mothers who at least had finished primary school (COR 2.60, 95% CI: 1.96–3.93).
Referent interviews were used to generate an asset index using primary component analysis. By applying the generated asset index, sample households were classified into five quintiles. Households were labelled as ‘poor’ when having an asset index score of less then the cut-off point of the 20th percentile among referent mothers. When dichotomising the wealth quintiles into poor and non-poor, there was a more than double risk for newborns of mothers from poor households compared to the non-poor to die within the first month after delivery (COR 2.21, 95% CI: 1.53–3.18).
When combining ethnicity, education, and economic status in a multivariate logistic regression model, an increased risk of neonatal mortality was shown for ethnic minority mothers and mothers with low education but could not be confirmed for mothers from poor households (Table 1).
Table 1.
Multivariate logistic regression model with maternal ethnicity, household economic status, and maternal education with adjusted odds ratios for neonatal mortality in Quang Ninh province, Vietnam
| Ref (n) | Cases (n) | OR | 95% CI | |
|---|---|---|---|---|
| Kinh | 370 | 67 | Ref | |
| Minority | 228 | 114 | 2.08† | 1.39–3.10 |
| Non-poor | 476 | 116 | Ref | |
| Poor | 122 | 65 | 1.28 | 0.84–1.94 |
| Primary school or higher | 492 | 116 | Ref | |
| No primary school | 106 | 65 | 1.65* | 1.08–2.53 |
p<.05,
p<.001.
Note: An asset score below the 20th percentile was considered poor. Primary school or higher completed representing ≥5 years of schooling.
Proximate determinants
In a first analysis of the proximate variables investigated, ANC attendance, delivery place, and distance to the closest health facility showed an association with neonatal mortality. Even if it has been previously noted in the literature, there was neither increased risk for young or old mothers in the material nor was parity associated with neonatal mortality. Family structure and marital status were investigated as well but showed no association with the outcome.
Mothers who had not attended any antenatal check-ups had a more than threefold risk of neonatal mortality (COR 3.45, 95% CI: 2.35–5.06) compared to mothers who had attended at least one ANC visit. Likewise, there was an increased risk for newborns to die before reaching 1 month of age if the mother delivered at home (COR 3.01, 95% CI: 2.02–4.49) compared to a health facility delivery.
The GIS coordinates for the homes of 597 referents and 181 cases were recorded. Straight-line distances from respondents' homes and all health facilities were calculated. Most mothers lived closest to a CHC. Distances to the closest health facility among different levels of the health system were divided into quintiles based on data from referents. The 40% living farthest away were labelled as being ‘remote’ compared to the rest that were labelled as ‘close.’ There was an increased risk of neonatal mortality for mothers living farthest away (COR 1.96 95% CI: 1.40–2.74) from any health facility.
When combining the variables that were associated with neonatal mortality (place of delivery, antenatal care attendance, and distance to health facilities) all three were still significant risk factors for neonatal mortality (Table 2). It can, however, be argued that these variables are all in the casual pathway of neonatal mortality and should thus not be combined in the same multivariate model. Nevertheless, by doing so and still maintaining the association to neonatal mortality hints to the individual impact of each variable. Furthermore, mothers who did not attend antenatal care and who also delivered at home were at an even higher risk of experiencing neonatal mortality (OR 4.79 95% CI: 2.98–7.71).
Table 2.
Multivariate logistic regression model with proximate determinant of neonatal mortality in NeoKIP study area in Quang Ninh province, Vietnam
| Ref (n) | Cases (n) | OR | 95% CI | |
|---|---|---|---|---|
| Health facility delivery | 519 | 125 | Ref | |
| Home delivery | 80 | 58 | 1.63 | 1.01–2.65 |
| ANC attendance | 507 | 113 | Ref | |
| No ANC attendance | 91 | 70 | 2.38 | 1.51–3.75 |
| Close to any health facility | 358 | 78 | Ref | |
| Remote from any health facility | 239 | 102 | 1.47 | 1.03–2.11 |
Combining distal and proximate determinants
We have thus far demonstrated the association of the distal socio-economic variables, ethnicity, and education and of three different proximate variables (place of delivery, antenatal care and distance to health facilities) to neonatal mortality. According to the conceptual framework earlier presented and the intention not to mix distal and proximal determinants in the analysis, stratification was used to investigate the influence of proximal determinants in each socio-economic subgroup. When stratifying by ethnicity, there were still associations between the proximate variables and neonatal mortality (Table 3). A similar pattern was seen when stratifying by education (data not shown).
Table 3.
Odds Ratios (OR) for neonatal mortality risks related to delivery place, ANC attendance, and distance to health facility, divided by ethnic belonging
| OR | 95% CI | OR | 95% CI | ||
|---|---|---|---|---|---|
| Ethnicity | Distance to closest health facility | ||||
| Kinh | Close | Ref | |||
| Remote | 1.31 | 0.75–2.27 | |||
| Minority | Close | 2.12 | 1.27–3.54 | Ref | |
| Remote | 3.46 | 2.24–5.35 | 1.61 | 0.99–2.62 | |
| Ethnicity | ANC visit | ||||
| Kinh | Yes | Ref | |||
| No | 1.14 | 0.45–2.87 | |||
| Minority | Yes | 1.73 | 1.14–2.62 | Ref | |
| No | 5.52 | 3.45–8.82 | 3.20 | 1.97–5.20 | |
| Ethnicity | Place of delivery | ||||
| Kinh | Health facility | Ref | |||
| Home | 0.91 | 0.11–7.68 | |||
| Minority | Health facility | 2.05 | 1.37–3.07 | Ref | |
| Home | 4.20 | 2.67–6.59 | 2.05 | 1.28–3.26 | |
Discussion
The results from the four studies presented in this article highlight different structural obstacles for improved neonatal survival in Quang Ninh province, Vietnam. A faulty data reporting system hides the magnitude of the problem and obstructs evaluation of interventions made. Group differences based on ethnicity with ethnic minority mothers at a marked increased risk of neonatal mortality are grounded in societal structures and may be difficult to fully understand and target.
Consequences of under-reporting
The first structural obstacle on the road to better neonatal survival is the lack of valid statistics (42). This is not an isolated problem for Vietnam but has been described from many places and settings (28, 43–48). In the Vietnamese setting, there seems to be various reasons why births and neonatal deaths are under-reported. These range from a poor understanding among health staff regarding the rationale and importance for adequate statistics to systematic errors within the health care system. Utmost, however, the responsibility is put on the family when it comes to registering births and deaths and there are multiple reasons why the family is not always interested in reporting such events. Further, a living newborn who has died before it has been registered as a birth might not be reported as a death. Even if there has been a relaxation in the Vietnamese family planning laws that are now advocating a ‘small family size’ policy, the norm of one to two children may be a cause for the third and subsequent children to go unreported (49). If, instead, the reporting of births and deaths was fully the responsibility of the health system, our results indicate that the level of accuracy would increase considerably.
The problem with under-reporting neonatal deaths may have severe consequences. At national and provincial levels, the low neonatal mortality rates will be misleading for policy and decision-makers and health plans will not be able to target those most in need. At the local level, the faulty statistics will preserve status quo by keeping the problem invisible. Families and local health staff will not perceive the neonatal period as a time of enhanced risk for the newborn and will not see the need to take the necessary precautions to improve delivery or postnatal care.
Under-reporting is not only a matter of withheld interventions and lack of investments but it is also a matter of human rights. According to the UN Convention on the Rights of the Child, to be registered at birth is a right for every child as an acknowledgement of humanhood (50). To be visible in the statistics is to be part of society. Registering neonatal deaths in a systematic and honest way will further strengthen the position of all neonates by confirming their value as human beings. The enforcement of human rights is thereby an important part in the effort to improve neonatal survival (51).
Ethnic minorities at risk
Ethnic minorities in Quang Ninh province are at a higher risk of experiencing neonatal mortality than the majority group of Kinh. This increased risk is independent of the minority mother's education or the economic status of the household she lives in. Ethnic minorities in Vietnam are known to be marginalised, living in remote and mountainous areas (37, 52, 53). It has also been shown that the ethnic minorities have benefited less from the economic development in recent years than the Kinh group, thus leaving them even more disadvantaged (52, 54). Despite these economic and educational disadvantages, there seems to be more to ethnicity that explains the heightened risk of neonatal mortality. The proximate determinants health care utilisation prior to and at delivery seems to be a plausible explanation for the discrepancy in survival between the majority and minority groups since ethnic minority mothers are more likely not to attend ANC and to deliver at home – which are well known and in the material presented here – as proven risk factors of neonatal death. However, even if the minority mother attends ANC or delivers at a health facility, they are at a higher risk of losing their newborn in the first month. Therefore, a higher home delivery rate and less ANC are parts of the explanation (but do not represent the whole explanation). The remoteness of ethnic minority residences is often brought up as a reason for the disadvantages of minorities. It has, however, been argued that the development of a widening economic gap between the minority and majority is not only attributed to the remoteness of minority settlements but is due to a combination of many social factors (55). Study results support this argument. When analysing the distance from mothers' homes to the closest health facility, remoteness is still associated with neonatal mortality regardless of ethnic belonging (41).
What is demonstrated here is an example of horizontal inequity as described and defined by Stewart (56). Most often inequalities in society, whether in politics, economy, or health, are measured from an individual or household perspective. This vertical inequality, measured over a range of individuals or households, omits the group dimension and the existence of inequalities between different culturally defined groups. Ethnicity, which is often defined as having a common history, language, or tradition, may be a joining factor for such a group. Even if there might be large inequalities within the group, the difference between one culturally defined group relative to another may be a powerful preserver of status quo as well as a structural determinant that serves to explain differences in, for example, health outcomes. The universal human need to belong, by identification and affiliation with different groupings, inevitably leads to exclusion as a function to set and keep boundaries. This mechanism can be both internal within the group and external by people and groupings from outside. In this case of neonatal mortality and health care utilisation, the internal forces of ethnicity might cause the preservation of harmful traditions in newborn care. For example, there might be a certain cultural tenet within an ethnic grouping that forbids certain foods and nutritional intake during pregnancy or there might be complete sets of traditions that relate to childbirth. In Vietnam, the beliefs in traditional medicine are strong (37, 57), which could cause delay in seeking appropriate medical care. External forces of group belonging could, in this context, be any negative attitudes of health staff, discrimination against ethnic minority mothers (since ethnic minority markers might result in different treatment), as well as adverse attitudes in contacts with the health system. This is shown in the findings as an elevated risk for minority mothers even if delivering at a health facility. Finally, there are combinations and interactions of internal and external factors where, for example, the choice of delivery place might be influenced not only by the mother's perceptions of how she is going to be received at a health facility (internal), but also by her previous experiences of staff attitudes and reception (external). Regardless of what the exact and true mechanisms are – which would be within the research field of a social anthropologist – the understanding of the concept ‘horizontal inequality’ will anyway be useful when trying to comprehend and explain the adverse health effects of ethnic minority belonging in this setting.
Methodological considerations
One of the major concerns when gathering data has been to identify all neonatal cases. As was stated, there is a substantial under-reporting of neonatal deaths in official statistics. The reasons for this are many but some of the reasons pose problems, even if a separate data collection system is setup beside the official system. The lack of consistency and coordination of registers at different health facilities made it difficult to compare cases. Additionally, in Vietnam, there is a widespread attitude about the importance of showing good statistics, locally referred to as the ‘achievement disease.’ This also offers a strong force within the Communist and Confucian systems, where it is not allowed to criticise superiors and where goals are expected to be met. Many of the neonatal deaths occurring are due to poor competence and mishandling of health staff and instead of requesting more training and resources the problem is hidden in order to avoid disgrace. Such ‘achievement disease’ is sometimes so institutionalised that community health staff can be given directives from higher levels to tamper the reports. To deal with this issue, a case-referent study design was applied in order to get all information directly from the mothers since the official registers could not be trusted. However, the problem with identifying neonatal deaths remained and only through the use of a number of different sources (village health workers, admission registers, birth registers, mortality records, etc.) could an acceptable level of completeness be reached.
When registering a perinatal health event, one of the problems is that of defining a neonatal death. Since such a large proportion of neonatal deaths occur intrapartum, it might sometimes be difficult to distinguish between a neonatal death and a stillbirth (13), and many early neonatal deaths are misclassified as stillbirths (58). It has also been shown that neonatal deaths occurring in the first hours after birth or in small babies are less likely than other neonatal deaths to be reported (28, 59, 60). A neonate must, by definition, be alive after birth before dying to be classified as a neonatal death event even if life is just for a very short time. If the birth assistant is not receptive at the time of delivery, deciding whether or not the baby was a live birth or a stillbirth can be difficult.
Conclusion: who can save the unseen?
The neonatal period has long been neglected in global health, resulting in a persistent neonatal mortality despite considerable improvements of overall child survival in the recent decades (61). Fatalism and misconceptions have stalled development, and the width of the problem has not been visible in international statistics. The findings from Quang Ninh province reveal the invisibility of neonatal mortality in official statistics. Reasons for this under-reporting are diverse, but a common trait is the low importance the issue receives at all levels: families are told to forget and go on with their lives and that it is unavoidable that newborns die and health staff members are afraid to be accused of maltreatment or poor achievement and therefore omit reporting neonatal deaths. The consequences of this under-reporting are severe, ranging from lack of investments at the global level to neglect of the issue all the way down to the individual level.
It is not only in the registers and statistics that neonatal mortality is invisible. It is also a matter of marginalisation and hierarchical structures. In a patriarchal society where sons are regarded higher than daughters, women's health is not a priority. Childbirth and the postnatal period fall into the category of gender inequity, resulting in an association between the social position of women in society and child health and survival (62). In the same way, the poor, the less well educated, and the ethnic minorities are discriminated against and marginalised with inequities in health as the result. The Vietnamese government has put considerable emphasis on reducing economic disparities over the years and has seemingly managed well. However, at the time of data collection, there remained a large inequity based on ethnicity that is reflected in the material presented in this thesis. The causes of such inequity are complex involving higher home delivery rates and less ANC attendance among ethnic minorities. Many home deliveries are unknown to health care officials, and skilled attendance at birth can therefore not be promoted or provided. But the sources of ethnic inequity can also be found among the attitudes and level of discrimination within the health system causing difficulties in communication and a reluctance to seek care. In a rapidly changing society like Vietnam, a steep economic development causes the gaps between different segments to widen. Therefore, it is even more important to identify and acknowledge groups at highest risk – here found to be ethnic minorities – and to target them with interventions for improved neonatal survival.
Conflict of interest and funding
The author has no conflict of interest. The project has been financially supported by Sida/SAREC.
References
- 1.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Kerber K, Enweronu-Laryea C, Massee Bateman O. Newborn survival in low resource settings – are we delivering? BJOG. 2009;116:49–59. doi: 10.1111/j.1471-0528.2009.02328.x. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad OB, Lopez AD, Inoue M. The decline in child mortality: a reappraisal. Bull World Health Organ. 2000;78:1175–91. [PMC free article] [PubMed] [Google Scholar]
- 4.Martines J, Paul VK, Bhutta ZA, Koblinsky M, Soucat A, Walker N, et al. Neonatal survival: a call for action. Lancet. 2005;365:1189–97. doi: 10.1016/S0140-6736(05)71882-1. [DOI] [PubMed] [Google Scholar]
- 5.Lawn JE, Cousens SN, Darmstadt GL, Bhutta ZA, Martines J, Paul V, et al. 1 year after The Lancet Neonatal Survival Series – was the call for action heard? Lancet. 2006;367:1541–7. doi: 10.1016/S0140-6736(06)68587-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 7.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 8.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–88. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 9.Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynaecol Obstet. 2009;107:S5–18. doi: 10.1016/j.ijgo.2009.07.016. S19. [DOI] [PubMed] [Google Scholar]
- 10.Adegoke AA, van den Broek N. Skilled birth attendance – lessons learnt. BJOG. 2009;116:33–40. doi: 10.1111/j.1471-0528.2009.02336.x. [DOI] [PubMed] [Google Scholar]
- 11.Lawn JE, Kinney M, Lee AC, Chopra M, Donnay F, Paul VK, et al. Reducing intrapartum-related deaths and disability: can the health system deliver? Int J Gynaecol Obstet. 2009;107:S40–42. doi: 10.1016/j.ijgo.2009.07.021. S123–140. [DOI] [PubMed] [Google Scholar]
- 12.Wall SN, Lee AC, Niermeyer S, English M, Keenan WJ, Carlo W, et al. Neonatal resuscitation in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynaecol Obstet. 2009;107:S3–4. doi: 10.1016/j.ijgo.2009.07.013. S47–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. 2005;83:409–17. [PMC free article] [PubMed] [Google Scholar]
- 14.Nga NT, Malqvist M, Eriksson L, Hoa DP, Johansson A, Wallin L. Perinatal services and outcomes in Quang Ninh province, Vietnam. Acta Paediatr. 2010:99. doi: 10.1111/j.1651-2227.2010.01866.x. [DOI] [PubMed] [Google Scholar]
- 15.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 16.Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bryant J. Communism, poverty and demographic change in North Vietnam. Population and Development Review. 1998;24:235–69. [Google Scholar]
- 18.UNICEF. New York: Unicef; 2009. The state of the world's children 2009. [Google Scholar]
- 19.Hoa DP, Nga NT, Malqvist M, Persson LA. Persistent neonatal mortality despite improved under-five survival: a retrospective cohort study in northern Vietnam. Acta Paediatr. 2008;97:166–70. doi: 10.1111/j.1651-2227.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- 20.World Bank. Vietnam development report 2004: poverty. Hanoi, Vietnam: World Bank; 2004. [Google Scholar]
- 21.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. Population and Development Review. 1984;10:25–45. [PMC free article] [PubMed] [Google Scholar]
- 22.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26:224–7. doi: 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- 23.Boerma JT, Weir SS. Integrating demographic and epidemiological approaches to research on HIV/AIDS: the proximate-determinants framework. J Infect Dis. 2005;191:S61–7. doi: 10.1086/425282. [DOI] [PubMed] [Google Scholar]
- 24.Titaley CR, Dibley MJ, Agho K, Roberts CL, Hall J. Determinants of neonatal mortality in Indonesia. BMC Public Health. 2008;8:232. doi: 10.1186/1471-2458-8-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCarthy J, Maine D. A framework for analyzing the determinants of maternal mortality. Stud Fam Plann. 1992;23:23–33. [PubMed] [Google Scholar]
- 26.Caldwell J. Education as a factor in mortality decline: an examination of Nigerian data. Population Studies. 1979:395–413. [Google Scholar]
- 27.Dao HT, Waters H, Le QV. User fees and health service utilization in Vietnam: how to protect the poor? Public Health. 2008;122:1068–78. doi: 10.1016/j.puhe.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Huy TQ, Long NH, Hoa DP, Byass P, Ericksson B. Validity and completeness of death reporting and registration in a rural district of Vietnam. Scand J Public Health Suppl. 2003;62:12–8. doi: 10.1080/14034950310015059. [DOI] [PubMed] [Google Scholar]
- 29.Gammeltoft T. Richmond, Surrey [England]: Curzon Press; 1999. Women's bodies, women's worries: health and family planning in a Vietnamese rural community. [Google Scholar]
- 30.Guilmoto CZ, Hoang X, Van TN. Recent increase in sex ratio at birth in Viet Nam. PLoS One. 2009;4:e4624. doi: 10.1371/journal.pone.0004624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fotso JC, Ezeh AC, Essendi H. Maternal health in resource-poor urban settings: how does women's autonomy influence the utilization of obstetric care services? Reprod Health. 2009;6:9. doi: 10.1186/1742-4755-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Furuta M, Salway S. Women's position within the household as a determinant of maternal health care use in Nepal. Int Fam Plan Perspect. 2006;32:17–27. doi: 10.1363/3201706. [DOI] [PubMed] [Google Scholar]
- 33.Kruk ME, Paczkowski M, Mbaruku G, de Pinho H, Galea S. Women's preferences for place of delivery in rural Tanzania: a population-based discrete choice experiment. Am J Public Health. 2009;99:1666–72. doi: 10.2105/AJPH.2008.146209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waiswa P, Kemigisa M, Kiguli J, Naikoba S, Pariyo GW, Peterson S. Acceptability of evidence-based neonatal care practices in rural Uganda – implications for programming. BMC Pregnancy Childbirth. 2008;8:21. doi: 10.1186/1471-2393-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bazzano AN, Kirkwood BR, Tawiah-Agyemang C, Owusu-Agyei S, Adongo PB. Beyond symptom recognition: care-seeking for ill newborns in rural Ghana. Trop Med Int Health. 2008;13:123–8. doi: 10.1111/j.1365-3156.2007.01981.x. [DOI] [PubMed] [Google Scholar]
- 36.WHO. Geneva: World Health Organization; 2006. Neonatal and perinatal mortality: country, regional and global estimates. [Google Scholar]
- 37.WHO. Hanoi: Technical Series No. 1. Geneva: World Health Organization; 2003. Health and ethnic minorities in Viet Nam. [Google Scholar]
- 38.Malqvist M, Eriksson L, Nga NT, Fagerland LI, Hoa DP, Wallin L, et al. Unreported births and deaths, a severe obstacle for improved neonatal survival in low-income countries; a population based study. BMC Int Health Hum Rights. 2008;8:4. doi: 10.1186/1472-698X-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malqvist M, Nga NT, Eriksson L, Wallin L, Ewald U, Persson LA. Delivery care utilisation and care-seeking in the neonatal period: a population-based study in Vietnam. Ann Trop Paediatr. 2008;28:191–8. doi: 10.1179/146532808X335633. [DOI] [PubMed] [Google Scholar]
- 40.Malqvist M, Nga NT, Eriksson L, Wallin L, Persson LA. Ethnic inequity in neonatal survival: a case-referent study in northern Vietnam. Acta Paediatrica. 2010 Oct 19; doi: 10.1111/j.1651-2227.2010.02065.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 41.Malqvist M, Sohel N, Do T, Eriksson L, Persson LA. Distance decay in delivery care utilisation associated with neonatal mortality. A case referent study in northern Vietnam. BMC Public Health. 2010;10:762. doi: 10.1186/1471-2458-10-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shibuya K, Scheele S, Boerma T. Health statistics: time to get serious. Bull World Health Organ. 2005;83:722. [PMC free article] [PubMed] [Google Scholar]
- 43.Nannan N, Bradshaw D, Mazur R, Maphumulo S. What is the infant mortality rate in South Africa? The need for improved data. S Afr Med J. 1998;88:1583–87. [PubMed] [Google Scholar]
- 44.Ndong I, Gloyd S, Gale J. An evaluation of vital registers as sources of data for infant mortality rates in Cameroon. Int J Epidemiol. 1994;23:536–39. doi: 10.1093/ije/23.3.536. [DOI] [PubMed] [Google Scholar]
- 45.Chen LM, Sun CA, Wu DM, Shen MH, Lee WC. Underregistration of neonatal deaths: an empirical study of the accuracy of infantile vital statistics in Taiwan. J Epidemiol Community Health. 1998;52:289–92. doi: 10.1136/jech.52.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mercer A, Uddin N, Huq NL, Haseen F, Khan MH, Larson CP. Validating neonatal mortality and use of NGO reproductive health outreach services in rural Bangladesh. Stud Fam Plann. 2006;37:111–22. doi: 10.1111/j.1728-4465.2006.00090.x. [DOI] [PubMed] [Google Scholar]
- 47.McCaw-Binns AM, Fox K, Foster-Williams KE, Ashley DE, Irons B. Registration of births, stillbirths and infant deaths in Jamaica. Int J Epidemiol. 1996;25:807–13. doi: 10.1093/ije/25.4.807. [DOI] [PubMed] [Google Scholar]
- 48.Bang A, Reddy MH, Deshmukh MD. Child mortality in Maharashtra. Economic and Political Weekly. 2002;49:4947–65. [Google Scholar]
- 49.Pham BN, Hall W, Hill PS, Rao C. Analysis of socio-political and health practices influencing sex ratio at birth in Viet Nam. Reprod Health Matters. 2008;16:176–84. doi: 10.1016/S0968-8080(08)32412-4. [DOI] [PubMed] [Google Scholar]
- 50.UNICEF. Florence, Italy: Unicef Innocenti Research Centre; 2002. International Child Development Centre. Birth registration right from the start. [Google Scholar]
- 51.UN Millennium Project 2005. New York: Task Force on Child Health and Maternal Health; 2005. Who's got the power? Transforming health systems for women and children. [Google Scholar]
- 52.Van de Walle D, Gunewardena D. Sources of ethnic inequality in Viet Nam. Journal of Development Economics. 2001;65:177–207. [Google Scholar]
- 53.Teerawichitchainan B, Phillips JF. Ethnic differentials in parental health seeking for childhood illness in Vietnam. Soc Sci Med. 2008;66:1118–30. doi: 10.1016/j.socscimed.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 54.Baulch B, Truong K, Haughton D, Haughton J. Ethnic minority development in Vietnam: a socio-economic perspective. In: Glewwe P, Agrawal N, Dollar D, editors. Economic growth, poverty and household welfare in Vietnam. Washington DC: World Bank; 2004. [Google Scholar]
- 55.Swinkels R, Turk C. Hanoi, Vietnam: World Bank; 2004. Poverty and remote areas: evidence from new data and questions for the future. [Google Scholar]
- 56.Stewart F. Working Paper Series no 81. Queen Elisabeth House: University of Oxford; 2002. Horizontal inequalities: a neglected dimension of development. [Google Scholar]
- 57.WHO. Geneva: World Health Organization; 2001. Legal status of traditional medicine and complementary/alternative medicine: a worldwide review. [Google Scholar]
- 58.Conde-Agudelo A, Belizan JM, Diaz-Rossello JL. Epidemiology of fetal death in Latin America. Acta Obstet Gynecol Scand. 2000;79:371–8. [PubMed] [Google Scholar]
- 59.Lumbiganon P, Panamonta M, Laopaiboon M, Pothinam S, Patithat N. Why are Thai official perinatal and infant mortality rates so low? Int J Epidemiol. 1990;19:997–1000. doi: 10.1093/ije/19.4.997. [DOI] [PubMed] [Google Scholar]
- 60.McCarthy BJ, Terry J, Rochat RW, Quave S, Tyler CW., Jr The underregistration of neonatal deaths: Georgia 1974–77. Am J Public Health. 1980;70:977–82. doi: 10.2105/ajph.70.9.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.WHO. Geneva: World Health Organization; 2005. World health report 2005 – make every mother and child count: report of the Director-General. [Google Scholar]
- 62.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]