Abstract
We report results from an experimental study that tested the effectiveness of dissemination interventions to improve implementation of smoking cessation guidelines in maternal and child public health clinics. We additionally examine individual clinic results for contextual explanations not apparent from the experimental findings alone. Twelve clinics in Illinois were randomized to three dissemination strategies: (i) core dissemination (provision of the 2000 Public Health System Clinical Practice Guideline and a tested smoking cessation program, including program supplies and training), (ii) core dissemination and access to telephone counseling and (iii) core dissemination, telephone counseling access and outreach visits to clinics. Implementation outcomes were post-dissemination improvements over baseline in the percent of smokers reporting receipt/exposure to (i) provider advice, (ii) self-help booklet, (iii) videos, (iv) posters and (v) an adjunct intervention. Results showed significant increases in the percent of smokers receiving a booklet (overall) and an adjunct intervention (Groups 2 and 3). There were no increases in smoker-reported provider advice or videos and poster exposure. Examination of individual clinic findings showed that seven clinics accounted for all the experimental effectiveness. Smoker-reported provider advice to quit also increased in these clinics. Type of clinic and the absence of disruptive events distinguished clinics with and without effective dissemination outcomes.
Introduction
Smoking prevalence is high among low income, childbearing-age women, posing significant health risks for them and their children [1–3]. Improving smoking cessation intervention in the maternal and child health (MCH) clinics that predominantly serve these women is an important public health goal [4]. Guidelines for interventions in clinical practice are available [5–7] but have not achieved widespread application [8]. Dissemination studies aimed at improving guideline implementation have had mixed results [9–14]. More information is needed to develop effective dissemination strategies [15].
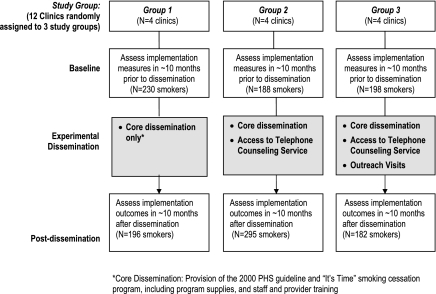
We report findings from a study that tested the effectiveness of three dissemination strategies to improve implementation of the 2000 Public Health System Clinical Practice Guideline (PHS Guideline) for smoking cessation intervention [6]. The goal was to improve implementation of the guideline's recommendations commonly known as the ‘5 As’. These are: ask and document smoking status for all patients, assess readiness to quit smoking, advise all smokers to quit, assist smokers in their quitting efforts and arrange for follow-up and/or adjunct interventions. Twelve MCH public health clinics in Illinois were randomized to three dissemination conditions: (i) core dissemination only (provision of the PHS Guideline and the previously tested ‘It's Time’ smoking cessation program [16, 17] including program supplies and training); (ii) core dissemination and access to free telephone counseling and (iii) core dissemination, access to telephone counseling and outreach visits. Study outcomes were post-dissemination improvement over baseline in six implementation variables that measured the percent of smokers reporting exposure to guideline-recommended interventions. The research hypotheses were:
i. Compared with the baseline, more smokers will report receiving smoking cessation interventions in the post-dissemination phase.
ii. The post-dissemination improvements will be greater in clinics with access to telephone counseling (Groups 2 and 3) than in clinics without such access.
iii. The post-dissemination improvements will further increase in clinics with outreach visits (Group 3).
In recent years, several authors have discussed the merits and limitations of experimental methods for ‘real world’ effectiveness studies [18–21]. These authors generally recommend paying greater attention to (i) the likelihood of non-homogeneous study samples and (ii) contextual factors that may influence study outcomes besides the experimental interventions. Our study addresses these issues in two ways. First, all experimental comparisons were adjusted for clustering of smokers within clinics and for four contextual variables (i.e. type of clinic, type of visit and smoker race and pregnancy status). Second, we examined the experimental results for individual clinics for explanatory patterns not readily apparent from the experimental findings alone. This descriptive examination considered whether groups of clinics with similar implementation outcomes were associated with clinic characteristics and clinic-unique secular events.
Background
Diffusion theories [22–24] and the published experience of other dissemination researchers [6, 12, 25, 26] indicate that four elements are essential for effective dissemination strategies. These are: (i) active involvement and ‘buy-in’ of key clinic decision makers, (ii) systemic protocols and tools to support routine smoker identification and intervention delivery, (iii) capacity building and (iv) feedback on performance. Also important is the role of influential intermediaries, defined as individuals or organizations that the intended program adopters perceive to be authoritative and knowledgeable about the issue addressed by the program [22]. Influential intermediaries are essential to lend ‘real world’ context to research-initiated dissemination efforts.
Clinic ‘buy-in’ was inherent to the study recruitment procedures and facilitated by the participation of the leadership of the Illinois Department of Human Services (IDHS) as an influential intermediary. IDHS provides ongoing leadership, regulatory oversight and funding to county health departments (CountyHDs) across the state. Moreover, prior to this study, IDHS had distributed portions of the ‘state tobacco settlement monies’ to all CountyHDs, expecting each in turn to implement a smoking control program of its choice. The study provided a tested smoking control plan for the CountyHDs that had not yet implemented one. Eligible clinics received samples of all program and study materials. A teleconference organized by the influential intermediary stressed the public health merits of implementing the PHS Guideline and promoted the It's Time program as appropriate for this purpose. The principal investigator followed up with a personal visit to each interested clinic.
The dissemination strategies (summarized in Fig. 1) addressed the other dissemination elements. All clinics received the It's Time program as a means to increase their capacity to deliver interventions to smokers. The program was designed for delivery to all women smokers in MCH services, regardless of readiness to quit or pregnancy status, and was shown to be effective in a previous trial [16, 17]. Intervention components for smokers included: (i) provider advice to quit, (ii) self-help booklet, (iii) smoker-provider agreement form to set a quit date or commit to take intermediate actions toward quitting, (iv) educational video and (v) motivational posters about quitting smoking. Support components included protocols for providers and office support staff, chart reminders and a chart stamp to facilitate intervention documentation. Provider training included feedback on baseline performance.
Fig. 1.
Study design.
The dissemination strategies in Group 2 and 3 further enhanced resources and feedback opportunities. Access to a telephone counseling service increased capacity to offer an adjunct intervention to smokers. Telephone counseling was shown to be an effective adjunct intervention in several studies [27, 28] including two studies with low-income populations [16, 29]. Additionally, service utilization required establishing daily office routines and staff involvement that have been shown to improve implementation of health maintenance procedures [30]. Such routines may be difficult to establish around provider advice to quit alone [31] but were necessary for processing the telephone counseling requests. Periodic summary reports from the service provided additional performance feedback. Outreach visits provided assistance and reinforcement during the program start-up period. Outreach visits (or ‘academic detailing’) have been associated with improved implementation of health maintenance practices [32]. The main feature of this approach is a repeated and personalized interface between the program disseminators and the intended program users [33].
Methods
Clinics
Eligible MCH clinics were located in the upper half of the state, were expected to see at least 100 smokers per year and did not have another specific smoking cessation program. IDHS identified 28 such clinics, including two main types. Twenty-three clinics [non-physician (MD) clinics] were each part of a separate CountyHD with few or no other direct patient services besides the MCH clinics. They were located in small or mid-size towns and had predominantly White patients. These clinics provided MCH services such as case management, prenatal visits, family planning, immunization and the WIC program but referred clients to outside physicians for medical care. Five other clinics (MD clinics) were located in a metropolitan area and had predominantly African American patients. These clinics provided physician care in addition to the above MCH services and were part of large health care centers with multiple other medical departments besides those involved in this study. Three were affiliated with outpatient services at three hospitals. Sixteen clinics agreed to participate but four of these were lost during the study (i.e. never ready to start, poor smoker accrual and the clinic closed). The 12 study clinics included nine non-MD and three MD clinics, two of which were hospital based. Within clinic type, participating and non-participating clinics did not differ overall on the above characteristics. Participating clinics received $1000 as reimbursement for research participation tasks.
Dissemination implementation
Core dissemination
All clinics received: (i) copies of the PHS Guideline and It's Time program implementation manual, (ii) 1-year supply of It's Time booklets and forms and (iii) staff and provider training. Training workshops were conducted after baseline completion. For Group 1 and 2 clinics, ‘train-the-trainer’ workshops were conducted at a central location (non-MD clinics) or on-site (MD clinics) and attended by one to three representatives from each clinic (supervisory-level nurses and/or health educators and one physician from each MD clinic). Workshops were conducted on-site at each of the Group 3 clinics and attended by all providers and support staff (except that participation from the MD clinic physicians was limited). The half-day workshops had the same content for all study groups.
Telephone counseling service
Besides the core dissemination, Groups 2 and 3 clinics received access to the telephone counseling service. The It's Time agreement forms for these clinics included a line for a smoker to accept the counseling. The 15-min counseling calls were modeled after Miller's motivational interviewing [34] and performed by trained counselors at the researchers’ facilities. Group 1 clinics received cards referring smokers to the state's telephone quitline number.
Outreach visits
Besides the core dissemination and telephone counseling access, Group 3 clinics received outreach visits from the principal investigator and/or study coordinator. Visits included: (i) one visit to help customize protocols in preparation for the training workshop, (ii) one visit at 1-month post-training to discuss program implementation experiences and (iii) additional visits and/or phone calls over the ensuing 2 months to address concerns and provide reinforcement. The on-site training workshop at each of these clinics was attended by all relevant clinic personnel.
Study design
Figure 1 shows the study design. Baseline data were collected over a 10-month period before the dissemination intervention. Post-dissemination data were collected over the ensuing 12 months. All clinics were expected to have some smoking cessation procedures already implemented at baseline. Therefore, the same implementation variables were measured in both study phases. Dissemination outcomes were the changes in implementation rates from baseline to post-dissemination. Changes in study Group 1 indicated the effect of the core dissemination alone. Changes in study Groups 2 and 3 indicated the effectiveness of the two enhanced dissemination strategies. Random assignment of clinics to study groups was stratified by type of clinic. The office for the protection of research subjects at the University of Illinois at Chicago (UIC) approved all study protocols (Protocol # 1999-0494). Participating clinics signed a study participation agreement. Participating smokers gave written consent to be called for a telephone interview.
Smokers
The study population was all smokers seen in the clinics. As part of the reception process throughout both study phases (from March 2001 to July 2003), clinic staff asked all patients to complete the study accrual form. Patients themselves completed the form and dropped it in a sealed box to be forwarded to the researchers. The form assessed the patient's smoking status, demographics characteristics, pregnancy status and reason for the visit and asked for consent to be called for a telephone interview. Interviews were attempted 2 months later with all consenting female smokers 18–45 years old. The 20-min interview assessed exposure to smoking cessation interventions during the clinic visit and current smoking status. Professionally trained interviewers at the UIC Survey Research Laboratory performed all interviews. Respondents received a $ 10.00 coupon.
During the baseline phase, 4642 patients completed the form, 1439 (31%) were smokers and 971 (67% of smokers) consented to the study; of these, 616 (63%) completed the 2-month interview. During the post-dissemination phase, 6931 patients completed the form, 1872 (27%) were new smokers, 1252 (67%) gave consent and 671 (54%) completed the 2-month interview. Incomplete interviews were due primarily to inability to achieve telephone contact. Less than 5% refused. Of 1278 non-overlapping smokers from both study phases, 61% were White, 30% African American and 9% Hispanic and/or other races; 18% were pregnant and 51% were at the clinics for WIC services.
Variables
There was no smoking status assessment variable because all clinics already had a smoking status prompt in their computerized record system. Implementation variables in both study phases were the percent of smokers who reported: (i) receiving provider advice, (ii) receiving a self-help booklet and (iii) seeing posters or (iv) a video about quitting smoking (each coded no = 0 and yes = 1). A variable ‘total interventions’ was the sum of ‘yes’ responses to these four items (range 0–4). Referral of smokers to adjunct interventions, such as smoking cessation classes, could occur during both phases and was not precluded by acceptance of the telephone counseling in the post-dissemination phase. A variable adjunct intervention was coded ‘yes’ if the smoker reported receiving the telephone counseling or any other type of adjunct intervention. Two comparison variables were study phase (baseline versus post-dissemination) and study group (Group 1, 2 or 3). A clinic-level contextual variable was clinic type (MD clinics versus non-MD clinics). Smoker-level variables were visit type (WIC services versus all others), race (White versus all others) and pregnancy status (pregnant at the accrual visit versus not pregnant).
Two variables reflected secular events during the study period and were used in the examination of individual clinic findings. One variable was whether the clinic's contact person changed during the study. The second variable, disruptive events, summarized events observed through periodic research-related contacts with the clinics and in end-of-study debriefing with clinic key informants. Events included: (i) loss of funding and/or personnel, (ii) organizational restructuring due to a merge with another clinic (not a study clinic), (iii) large staff turnover, (iv) new administrator or director and (v) the clinic moved. The disruptive events variable was coded 1 if no event occurred, 2 if events occurred but were not deemed a major disruption by key informants and 3 if events were multiple and/or deemed disruptive.
Data analysis
To test Hypothesis 1, we compared the baseline and post-dissemination rates for each outcome variable, overall and within each study group. To test Hypotheses 2 and 3, we compared the size of the baseline/post-dissemination changes between study groups. Adjusted odds ratios (AOR) and adjusted average differences (AD) were estimated controlling for clustering of smokers within clinics, smoker pregnancy status and race and WIC visits. For the descriptive examination of individual clinic findings, we ranked clinics on their baseline/post-dissemination changes on the provider advice variable. We explored descriptively and through additional comparisons whether groups of clinics with similar ranking were associated with clinic characteristics and secular events. All statistical analyses were done with STATA.
Results
In the 12 clinics overall, compared with baseline, at post-dissemination there was an overall increase in smoker-reported receipt of a booklet (16–32%, AOR 3.1, P = 0.001) and an adjunct intervention (<1–10%, AOR 11.2, P = 0.001) and in mean total interventions (1.5–1.7, AD 0.24, P = 0.001) (data not shown in tables). Table I shows the implementation outcomes by study group. Smoker-reported receipt of a self-help booklet increased in Group 1 (6.5–37%) and Group 2 (8.5–28%) but not in Group 3 (34–32%). This inverse study group effect was significant (see rightmost column in Table I) but largely explained by the low baseline rates in Group 1 and 2. Smoker-reported adjunct interventions increased in Group 2 (1.1–9.5%) and in Group 3 (2–17%) but not in Group 1 (<1–3.6%). These between-group differences were not statistically significant (rightmost column). The lack of significance was partly explained by the highly skewed distribution of the adjunct intervention variable (i.e. several almost empty cells). The dissemination strategies had no effect on smoker-reported provider advice to quit or exposure to posters or videos about quitting.
Table I.
Smokers’ reports of interventions by study phase and study group (Ns = 12 clinics, 1278 smokers)
| Group 1 |
Group 2 |
Group 3 |
Significance of between-group base-post differencea |
|||||||||
| Intervention item | Base | Post | AORb/ADc (95% CI) | Base | Post | AORb/ADc (95% CI) | Base | Post | AORb/ADc (95% CI) | Group 1 versus 2 | Group 2 versus 3 | Group 1 versus 3 |
| n = 230 | n = 194 | n = 188 | n = 295 | n = 189 | n = 182 | |||||||
| Poster (%) | 60.0 | 58.2 | 0.89 (0.60,1.33) | 62.8 | 66.4 | 1.02 (0.69,1.53) | 65.2 | 65.4 | 1.53 (0.95,2.47) | ns | * | ** |
| Video (%) | 8.7 | 10.8 | 1.54 (0.79,3.01) | 5.9 | 4.1 | 0.71 (0.30,1.69) | 7.1 | 4.9 | 0.67 (0.31,1.44) | ns | ns | ns |
| Provider advice (%) | 63.9 | 68.6 | 1.33 (0.87,2.02) | 52.1 | 54.2 | 1.11 (0.76,1.63) | 70.2 | 69.8 | 1.20 (0.73,1.96) | ns | ns | ns |
| Self-help booklet (%) | 6.5 | 37.1 | 8.96 (4.81,16.68)*** | 8.5 | 28.5 | 3.96 (2.19,7.17)*** | 33.8 | 32.4 | 1.44 (0.90,2.31) | (*) | (***) | (***) |
| Total interventions (mean) | 1.4 | 1.7 | 0.37 (0.18,0.55)***c | 1.3 | 1.5 | 0.22 (0.03, 0.40)*c | 1.8 | 1.7 | 0.18 (−0.01,0.39)c | ns | ns | ns |
| Adjunct counseling (%) | 0.9 | 3.6 | 4.71 (0.95,23.36) | 1.1 | 9.5 | 9.38 (2.28,38.61)** | 2.0 | 17.0 | 11.50 (3.79,34.83)*** | ns | ns | ns |
Significance tests of between-group differences in base-post changes are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnancy status and type of visit (WIC versus all others). bAOR (adjusted odds ratios) and cAD (adjusted average difference) are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnant status and type of visit (WIC visit versus all others). ‘ns’ or no asterisk = not significant at 0.05 level. *P < 0.05; **P < 0.01; ***P < 0.001. Asterisks in () are significant in opposite direction. All are one-directional.
Table II shows the association of clinic ranking on change in provider advice to quit (first column) with secular events and type of clinic. The five lowest ranking clinics included all clinics in which the contact person changed during the study and all clinics with Level 3 disruptive events. These clinics also had no improvements in any other implementation variable. The two lowest ranking clinics were the only non-MD clinics with post-dissemination decline in smoker-reported provider advice (from 79 to 37% and from 53 to 40%, respectively). The disruptive events in these non-MD clinics may have altered the size and nature of the patient or provider population, thus affecting their study phase comparability. We excluded these two clinics from further analysis. The next three lowest ranking clinics included all MD clinics regardless of whether they had disruptive events or not, suggesting that their low ranking was due to type of clinic rather than to specific events.
Table II.
Clinic ranking on baseline/post-dissemination change in percent of smokers reporting provider advice to quit, secular events and type of clinic
| Clinic rank: 1 = largest negative change, 12 = largest improvement | Percent change | Contact person changed | Disruptive events: 3 = very disruptive, 2 = somewhat disruptive, 1 = no events | Type of clinic | Study group |
| 1 | −42 | No | 3 | Non-MD | 1 |
| 2 | −13 | Yes | 3 | Non-MD | 2 |
| 3 | −6 | Yes | 3 | MD | 2 |
| 4 | −12 | No | 1 | MD | 1 |
| 5 | −6 | Yes | 2 | MD | 3 |
| 6 | +4 | No | 1 | Non-MD | 2 |
| 7 | +7 | No | 1 | Non-MD | 3 |
| 8 | +18 | No | 2 | Non-MD | 2 |
| 9 | +19 | No | 2 | Non-MD | 1 |
| 10 | +19 | No | 1 | Non-MD | 3 |
| 11 | +22 | No | 1 | Non-MD | 3 |
| 12 | +40 | No | 1 | Non-MD | 1 |
To test this descriptive observation, we compared all implementation outcomes by type of clinic in the remaining 10 clinics (i.e. excluding the two non-MD clinics whose disruptive events may have affected group comparability but including all MD clinics where outcomes were unaffected by disruptive events). As shown in Table III, in the three MD clinics, the dissemination strategies had no effect except for a small improvement in smoker-reported adjunct interventions. In the seven non-MD clinics without disruptions, there were significant increases in smoker-reported provider advice to quit (62–72%), self-help booklets (23–43%) and adjunct interventions (1.1–11.7%) and in mean total interventions (from 1.6 to 1.9).
Table III.
Smokers’ reports of interventions by study phase and type of clinic
| MD clinics (N = 3) |
Non-MD clinics (N = 7) |
Significance of between MD & non-MD base-post differencea | |||||
| Implementation items | Base | Post | AORb/ADc (95% CI) | Base | Post | AORb/ADc (95% CI) | |
| n = 176 | n = 145 | n = 372 | n = 426 | ||||
| Poster (%) | 48.9 | 49.7 | 0.95 (0.60,1.49) | 68.3 | 70.7 | 1.13 (0.83,1.53) | ns |
| Video (%) | 9.1 | 10.3 | 1.37 (0.60,3.13) | 5.9 | 4.9 | 0.82 (0.43,1.55) | ns |
| Provider advice (%) | 60.2 | 50.3 | 0.60 (0.38,0.96)* | 62.3 | 71.8 | 2.08 (1.48,2.94)*** | *** |
| Self-help booklet (%) | 4.5 | 10.3 | 2.29 (0.93,5.66) | 22.6 | 43.2 | 3.78 (2.63,5.44)*** | ns |
| Total interventions (mean) | 1.2 | 1.2 | −0.08 (−0.29,0.13)b | 1.6 | 1.9 | 0.29 (0.14,0.43)***c | *** |
| Adjunct counseling (%) | 1.7 | 6.9 | 4.02 (1.04,15.54)* | 1.1 | 11.7 | 10.91 (4.15,28.67)*** | ns |
Significance tests of between-group differences in base-post changes are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnant status and type of visit. bAOR (adjusted odds ratios) and cAD (adjusted average difference) are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnant status and type of visit. ‘ns’ or not indicated = not significant at 0.05 level. *P < 0.05; **P < 0.01; ***P < 0.001. Asterisks in () are significant in opposite direction. All are one-directional.
We next tested whether study group effects might be found in the seven non-MD clinics that apparently accounted for all dissemination effectiveness (Table IV). We found patterns similar to those described above for Table I (i.e. significant baseline/post-dissemination changes within study group, but either inverse or non-significant between-group differences). However, significant post-dissemination improvements now occurred also in Group 3 clinics, including an increase in smoker-reported advice to quit. The positive effect of the enhanced dissemination strategies on completion of an adjunct intervention was also more evident in these clinics. In study Group 3, smoker-reported completion increased from 2% at baseline to 25% at post-dissemination.
Table IV.
Smokers’ reports of interventions by study phase and study group (Ns = 7 non-MD clinics, 798 smokers)
| Group 1 |
Group 2 |
Group 3 |
Significance of between-group base-post differencea |
|||||||||
| Implementation items | Base | Post | AORb/ADc (95% CI) | Base | Post | AORb/ADc (95% CI) | Base | Post | AORb/ADc (95% CI) | Group 1 versus 2 | Group 2 versus 3 | Group 1 versus 3 |
| n = 107 | n = 99 | n = 111 | n = 230 | n = 154 | n = 97 | |||||||
| Poster (%) | 67.3 | 69.7 | 1.07 (0.58,1.96) | 65.8 | 68.3 | 1.07 (0.66,1.75) | 70.8 | 77.3 | 1.96 (1.02,3.77)* | ns | * | ** |
| Video (%) | 3.7 | 6.1 | 1.84 (0.49,6.98) | 4.5 | 4.3 | 0.92 (0.30,2.79) | 8.4 | 5.2 | 0.44 (0.14,1.41) | ns | ns | ns |
| Provider advice (%) | 58.9 | 85.9 | 4.61 (2.28,9.32)*** | 47.7 | 57.8 | 1.47 (0.93,2.33) | 75.3 | 90.7 | 2.75 (1.19,6.34)* | ns | ns | ns |
| Self-help booklet (%) | 8.4 | 56.6 | 16.09 (7.06,36.67)*** | 10.8 | 32.2 | 3.92 (2.01,7.65)*** | 40.9 | 55.7 | 1.83 (1.05,3.19)* | (*) | (***) | (***) |
| Total interventions (mean) | 1.4 | 2.2 | 0.76 (0.53,1.00)***c | 1.3 | 1.6 | 0.32 (0.09,0.54)**c | 2.0 | 2.3 | 0.34 (0.24, 0.58)**c | ns | ns | ns |
| Adjunct counseling (%) | 0.9 | 2.0 | 2.11 (0.18,24.29) | 0.9 | 10.4 | 11.51(1.95,68.07)** | 1.9 | 24.7 | 17.59(4.85,63.75)*** | ns | ns | ns |
Significance tests of between-group differences in base-post changes are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnancy status and type of visit. bAOR (adjusted odds ratios) and cAD (adjusted average difference) are adjusted for clustering of smokers within clinics, smoker race/ethnicity and pregnancy status and type of visit. ‘ns’ or not indicated = not significant at 0.05 level. *P < 0.05; **P < 0.01; ***P < 0.001. Asterisks in () are significant in opposite direction. All are one-directional.
Discussion
Experimental results
The study dissemination strategies aimed at improving clinic provision of the smoking cessation interventions recommended by the PHS Guideline. Consistent with Hypothesis 1, results showed positive effects of providing the clinics with resources for assisting and referring smokers. Compared with baseline, more smokers in the post-dissemination phase received a self-help booklet and completed an adjunct intervention. These effects were significant in the experimental design with all 12-study clinics and even stronger in the seven clinics that accounted for all dissemination effectiveness. These findings are consistent with a physician survey in which performance of all the ‘5 As’ of the PHS Guideline was associated with availability of at least one material resource for smokers and one counseling resource for smoker referral [35].
Contrary to Hypothesis 1, there was no dissemination effect on smoker-reported provider advice to quit. This finding could be explained by an already fairly high baseline implementation rate (62% overall). This rate compares favorably to baseline or control findings in other studies. For example, the percent of smokers reporting provider advice to quit was as low as 19 and 38% in community-based medical centers in two studies [13, 36] and around 45 or 59% in private physician practices in two other studies [12, 37]. However, provider advice to quit increased in the seven non-MD clinics without disruptions despite high baseline rates.
Comparisons of our findings with those of other dissemination studies provide little additional insights. In a study that disseminated the PHS Guideline to primary care physician practices, Katz et al. [13] found a positive effect on assistance to smokers but not on provider advice. Three other studies found a positive effect on provider advice to quit [9, 10, 12]. As was the case for our dissemination strategies, all these studies included dissemination elements that addressed clinic ‘buy-in’, office support components, capacity building and performance feedback. It is unclear whether the different results could be due to different versions or intensity of these dissemination elements, different study settings and smoker populations or different study methods.
Study Hypotheses 2 and 3 assumed that the enhanced dissemination strategies would be more effective in improving all implementation outcomes than the core dissemination alone. Except for adjunct interventions, these hypotheses were not supported. Instead, larger post-dissemination increases in the self-help booklet and mean total interventions variables were associated with lower baseline implementation rates. Perhaps the dissemination strategies were most effective in the clinics that needed them most.
The enhanced dissemination strategies did have the expected positive effect on smoker-reported adjunct interventions. This finding has important practice implications and merits attention despite the lack of statistically significant between-group differences. Completion of an adjunct intervention is recommended to improve the limited benefits that can be expected from minimal provider intervention alone [6]. Completion of any adjunct intervention was almost nil at baseline in all clinics, did not improve at post-dissemination in Group 1, but increased up to one in four smokers at post-dissemination in the clinics with access to the proactive telephone counseling service. Noticeably, almost all of the smoker-reported adjunct interventions were completion of that telephone counseling. Our findings also show that providing smokers with only Quit Line information (study Group 1) did not increase the chances that they would receive adjunct counseling, whereas a linkage of clinic patients with an external proactive counseling service was feasible and more effective in reaching smokers. Since utilization doubled in the clinics with outreach visits, special efforts may however be necessary to promote clinic acceptance of such a linkage.
Examination of individual clinic findings
Two other findings emerged from the examination of individual clinics outcomes. First, the examination suggested that the overall experimental results may have been unduly depressed by two non-MD clinics with negative implementation outcomes. Unique secular events at these clinics may have undermined either the integrity of the research design and/or the program implementation. In both clinics, considerably fewer smokers received provider advice at post-dissemination than at baseline. It is more plausible to attribute this change to the disruptive events than to a strong negative dissemination effect that would be unique to these two clinics only.
Second, excluding the two above clinics from further analysis clarified that dissemination effectiveness varied by type of clinic. The dissemination strategies had no effect in the MD clinics, apparently due to these clinics’ characteristics (described earlier) rather than to specific disruptive events during the study. In particular, the MD clinics were part of large health care facilities with multiple other medical services and complex bureaucratic organizations. This organizational context may have hampered the implementation of new department-specific procedures. Additionally, only the MD clinics provided physician care. Physicians at these clinics may have perceived the smoking cessation program and joint staff training as aimed primarily at nursing staff. Different dissemination approaches or different smoking cessation programs may be needed in this type of medical settings.
In contrast, the dissemination strategies resulted in substantial guideline implementation improvements in the seven non-MD clinics with no disruptive events. As described earlier, these clinics were smaller and more self-contained than the MD clinics. Moreover, in these clinics, the key individuals involved in the initial study participation decisions appeared to be more directly involved in day-to-day clinic operations than those in the MD clinics. Finally, this type of non-MD public health MCH clinic has traditionally emphasized preventive care and patient education. The study dissemination strategies may be a promising approach to improve implementation of the PHS smoking cessation guideline in these clinics.
Study strengths and limitations
Strengths
The study addressed the public health priority of improving smoking cessation interventions in clinics serving low-income women. The clinic sample included multiple clinics representing two common types of MCH public health settings. Dissemination outcomes were measured on all available smokers and reflected non-research assisted routine clinic performance over an almost 2-year period. The experimental design was complemented by consideration of contextual variables and clinic-unique secular events.
Limitations
Practical considerations prevented a control group for the core dissemination strategy. In the clustered analysis, its baseline phase served as its own control for each clinic. Implementation improvements were associated with utilization of specific study-provided resources. However, we cannot rule out that extraneous factors may have affected the study results.
The implementation variables were based on smoker reports collected 8 weeks after the clinic visit. Smoker reports and similar time lags are generally accepted implementation measures and were used in most dissemination studies cited in this paper. Implementation measures based on chart reviews would have risked measuring improved intervention documentation (a dissemination effect) rather than improved delivery. Smoker attrition was high for both study consent in the clinics and telephone survey completion as is likely in special population studies [38]. Smoker attrition was unrelated to program participation, which was to be offered to all smokers as a regular clinic service. However, attrition analysis (not shown) indicated that smokers in the study were more likely to be White and more educated than those lost to the study. The generalizability of the study findings may be limited if these smoker characteristics also influence intervention delivery by providers.
Conclusions
To obtain population-level benefits, the smoking cessation interventions recommended in the PHS Guideline must achieve widespread implementation across a variety of health care delivery systems. Our study findings showed that such implementation can be improved in MCH clinics by: (i) disseminating the PHS Guideline in conjunction with a tested smoking cessation program, (ii) providing the training and resources necessary to implement the program and (iii) linking smokers in the clinics with a centralized proactive telephone counseling service. However, the effectiveness of these dissemination strategies appears to depend on type of clinic and on the absence of extraneous distractions.
Funding
Agency for Health Care Research and Quality (1RO1 HS10544-01A1); National Cancer Institute (2P50CA106743).
Conflict of interest statement
None declared.
Acknowledgments
The authors are thankful to the officers of the IDHS who provided assistance and advice in the implementation of this study. The authors thank the administrators, health care providers and office staff at the participating countyHD clinics for their kind study cooperation.
References
- 1.Centers for Disease Control and Prevention. Cigarette smoking among adults: United States 2006. MMWR Morb Mortal Wkly Rep. 2007;56:1157–61. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Women and Smoking: a Report of the Surgeon General. Rockville, MD: Public Health Service, Office of the Surgeon General; 2001. [Google Scholar]
- 3.U.S. Department of Health and Human Services. The Health Consequences of Smoking; A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health; 2004. [Google Scholar]
- 4.U.S. Department of Health and Human Services. Healthy People 2010. 2nd edn. Washington, D.C: U.S. Government Printing Office; 2000. [Google Scholar]
- 5.Fiore MC, Bailey WC, Cohen SH, et al. Smoking Cessation. Clinical Practice Guideline No. 18. Rockville, MD: Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research AHCPR Publication No. 96-0692. 1996. [Google Scholar]
- 6.Fiore MC, Bailey C, Cohen SH, et al. Treating Tobacco Use and Dependence. Clinical Practice Guideline. Rockville, MD: Department of Health and Human Services. (US), Public Health Service; 2000. [Google Scholar]
- 7.Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 8.Thorndike AN, Regan S, Rigotti NA. The treatment of smoking by U.S. Physicians during ambulatory visits: 1994-2003. Am J Public Health. 2007;97:1878–83. doi: 10.2105/AJPH.2006.092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews JO, Tingen MS, Waller JL, et al. Provider feedback improves adherence with AHCPR smoking cessation guideline. Prev Med. 2001;33:415–21. doi: 10.1006/pmed.2001.0907. [DOI] [PubMed] [Google Scholar]
- 10.Fisher E, Musick J, Scott C, et al. Improving clinic and neighborhood-based smoking cessation services within federally qualified health centers serving low-income, minority neighborhoods. Nicotine Tob Res. 2005;7(Suppl. 1):S45–56. doi: 10.1080/14622200500078105. [DOI] [PubMed] [Google Scholar]
- 11.Joseph AM, Adrian NJ, Larry AC, et al. Results of a randomized controlled trial of intervention to implement smoking guidelines in Veteran Affairs medical centers: increased use of medications without cessation benefits. Med Care. 2004;42:1100–10. doi: 10.1097/00005650-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Hollis JF, Bills R, Whitelock E, et al. (2000). Implementing tobacco interventions in the real world of managed care. Tob Control. 2000;9:18–i24. doi: 10.1136/tc.9.suppl_1.i18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz DA, Muehlenbruch DR, Brown RB, et al. Effectiveness of implementing the agency for healthcare research and quality smoking cessation clinical practice guideline: a randomized, controlled trial. J Natl Cancer Inst. 2004;96:594–603. doi: 10.1093/jnci/djh103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ward MM, Doebbeling BN, Vaughn TE, et al. Effectiveness of a nationally implemented smoking cessation guideline on provider and patient practices. Prev Med. 2003;36:265–71. doi: 10.1016/s0091-7435(02)00046-4. [DOI] [PubMed] [Google Scholar]
- 15.Ellis P, Robinson P, Ciliska D, et al. A systematic review of studies evaluating diffusion and dissemination of selected cancer control interventions. Health Psychol. 2005;24:488–500. doi: 10.1037/0278-6133.24.5.488. [DOI] [PubMed] [Google Scholar]
- 16.Manfredi C, Crittenden K, Cho YI, et al. The effect of a structured smoking cessation program independent of exposure to existing interventions. Am J Public Health. 2000;90:751–6. doi: 10.2105/ajph.90.5.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manfredi C, Fleming S. Program evaluation in public health practice: a collaboration between the Chicago Department of Public Health and the University of Illinois at Chicago. In: Sullivan M, Kelly J, editors. Collaborative Research: University and Community Partnership. Washington, D.C: American Public Health Association; 2001. pp. 129–48. [Google Scholar]
- 18.Glasgow RE. Critical measurement issues in translational research. Res Soc Work Pract. 2009;19:560–8. [Google Scholar]
- 19.Glasgow RE, Magid DJ, Beck A, et al. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care. 2005;43:551–7. doi: 10.1097/01.mlr.0000163645.41407.09. [DOI] [PubMed] [Google Scholar]
- 20.Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: dissemination research and research dissemination: how can we close the gap? Health Psychol. 2005;5:443–6. doi: 10.1037/0278-6133.24.5.443. [DOI] [PubMed] [Google Scholar]
- 21.Tunis SR, Stryer DB, Clancey CM. Practical clinical trials. Increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–32. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 22.Rogers EM. Diffusion of innovation. 5th edn. New York, NY: Free Press; 2003. [Google Scholar]
- 23.Orlandi MA, Landers C, Weston R, et al. Diffusion of health promotion innovations. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education. Theory, Research and Practice. San Francisco, CA: Jossey-Bass Inc.; 1990. pp. 288–313. [Google Scholar]
- 24.Sonnad SS. Organizational tactics for the successful assimilation of medical practice guidelines. Health Care Manage Rev. 1998;23:30–7. doi: 10.1097/00004010-199802330-00004. [DOI] [PubMed] [Google Scholar]
- 25.Curry SJ. Organizational interventions to encourage guideline implementation. Chest. 2000;118:40S–8S. doi: 10.1378/chest.118.2_suppl.40s. [DOI] [PubMed] [Google Scholar]
- 26.Stone TT, Longo DR, Phillips RL, et al. Health care system and insurer support for smoking cessation guideline implementation. J Health Care Finance. 2002;29:78–86. [PubMed] [Google Scholar]
- 27.Ossip-Klein D, McIntosh S. Quitlines in North America: evidence base and applications. Am J Med Sci. 2003;326:201–5. doi: 10.1097/00000441-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Zhu SH, Anderson CM, Tedeschi GJ, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347:1087–93. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- 29.Wadland WC, Soffelmayr B, Ives K. Enhancing smoking cessation of low-income smokers in managed care. J Fam Pract. 2001;50:138–44. [PubMed] [Google Scholar]
- 30.Hollis JF, Vogt TM, Stevens V, et al. National Cancer Institute, Smoking and Tobacco Control. Monograph 5: Tobacco and the Clinician: Interventions for Medical and Dental Practice. U.S. Department of Health and Human Services, National Institute of Health, National Cancer Institute, Bethesda, MD: N.I.H. Publication No. 94-3693; 1994. The Tobacco Reduction and Cancer Control (TRACC) Program: team approaches to counseling in medical and dental settings; pp. 143–85. [Google Scholar]
- 31.Manfredi C, LeHew CW. Why implementation processes vary across the 5 A's of the smoking cessation guideline: administrators’ perspectives. Nicotine Tob Res. 2008;10:1597–607. doi: 10.1080/14622200802410006. [DOI] [PubMed] [Google Scholar]
- 32.O'Brien T, Oxman AD, Davis DA, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;4:CD000409. doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soumerai SB, Avorn J. Principles of Educational Outreach (‘Academic Detailing’) to improve clinical decision making. JAMA. 1990;263:549–56. [PubMed] [Google Scholar]
- 34.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: The Guilford Press; 1991. [Google Scholar]
- 35.Hartman KE, Wechter ME, Payne P, et al. Best practice smoking cessation intervention and resource needs of prenatal care providers. Obstet Gynecol. 2007;110:765–70. doi: 10.1097/01.AOG.0000280572.18234.96. [DOI] [PubMed] [Google Scholar]
- 36.DePue JD, Goldstein MG, Schilling A, et al. Dissemination of the AHCPR clinical practice guideline in community health centers. Tob Control. 2002;11:329–35. doi: 10.1136/tc.11.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldstein MG, Niaura R, Willey C, et al. An academic detailing intervention to disseminate physician-delivered smoking cessation counseling: smoking cessation outcomes of the Physician Counseling Smokers Project. Prev Med. 2000;36:185–96. doi: 10.1016/s0091-7435(02)00018-x. [DOI] [PubMed] [Google Scholar]
- 38.Crosby RA, Salazar LF, DiClemente R, et al. Balancing rigor against the inherent limitations of investigating hard-to-reach populations. Health Educ Res. 2010;25:1–5. doi: 10.1093/her/cyp062. [DOI] [PubMed] [Google Scholar]