Abstract
Regional differences between large cities and rural areas are observed in the Korean National Health and Nutrition Examination Survey (KNHANES). This present study was conducted to evaluate the effect of dietary factors on hypertension risk in Korean populations, especially residents of the Chungcheong province which was not in metropolitan area, using KNHANES III. A total of 544 adults aged ≥ 19 years were placed into either the normotensive or the hypertensive group. Subject characteristics, BMI, blood pressure, and nutrient intakes were compared between the two groups using a chi-square test and t-test. We estimated odds ratios (ORs) using multiple logistic regression, adjusted for energy intake and selected covariates. There were significant differences in age, education level, alcohol consumption, and BMI between the normotensive and hypertensive groups. We found decreased ORs for the medium versus lowest tertile of calcium intake (multivariate OR = 0.43, 95% CI: 0.21-0.88), for the highest versus lowest tertile of calcium intake (multivariate OR = 0.43, 95% CI: 0.20-0.90) with significant trends in risk (P = 0.040), and for the medium versus lowest tertile of potassium intake (multivariate OR = 0.43, 95% CI: 0.20-0.89). Subjects with the highest sodium/calcium ratio had a 2.10-fold greater risk of hypertension compared to the subject with the lowest, with significant trends in risk (P = 0.002). Adequate calcium and potassium intake should be encouraged and regional differences should be considered in making a healthy plan for hypertension management.
Keywords: Hypertension, sodium, potassium, calcium, Korean National Health and Nutrition Examination Survey
Introduction
Hypertension presents a significant public health burden due to increased cardiovascular disease, mortality, disability, and economic cost. It is becoming an increasingly common health problem worldwide because of increasing longevity and a higher prevalence of contributing factors, such as obesity, physical inactivity and an unhealthy diet [1,2]. Worldwide hypertension is estimated to cause 7.1 million premature deaths and 4.5% of the disease burden [3]. Mortality rate per 100,000 persons due to high blood pressure varies from country to country. It is reported that the mortality rate due to hypertension was 15.9 per 100,000 persons in the United States in 2000 and 4.5 in 2002 in Japan. The mortality rate due to high blood pressure in Korea increased slightly, from 10.6 to 11.0 per 100,000 persons, between 2002 and 2007 [4].
Currently, the prevalences of hypertension in many developing countries, particularly in urban areas, are as high as those seen in developed countries [5-8]. In contrast to previous studies in other developing countries, the prevalence of hypertension in Korean adults (≥ 30 yrs) decreased from 30% to 24.9% between 1998 and 2007 [9] and the trends of regional differences in prevalence of hypertension were observed in opposite direction; the prevalence of hypertension were 26.2% in metropolitan areas while 34.3% in small towns [10]. Indeed, hypertension rate in Chungcheong province, which is not in metropolitan area, increased from 22.1% in 2001 to 28.0% in 2005, while normotensive rate decreased from 47.7% in 2001 to 41.0% in 2005 [10].
Local traditional and seasonal variations in foods intake are common in Korea, due to environmental differences such as regional variations in climate and geographical characteristics. The prevalence of hypertension in rural areas may differ from metropolitan areas based on these variations. Based on the Korean Health and Nutrition Examination Survey (KNHANES) III report [10], healthy lifestyles, including healthy diet patterns, were observed more in urban areas than in rural areas. Sodium intake was relatively higher in rural areas than in urban areas (4,834 mg vs. 4,571 mg). Community nutritionists should consider these regional variations and characteristics when they plan hypertension management program for the community residents.
The target of this research area, Chungcheong province, is located in central area of South Korea, and includes the inland area, Chungcheongbuk-do and the west coast border, Chungcheongnam-do. The characteristics of local food culture in Chungcheong province is a mix between that of the inland and the west coast area. Particularly, people in this province have traditionally used a wide variety of salted foods, including abundant sea foods, which leads to high sodium intake and might eventually relate to high blood pressure and a risk of hypertension. Therefore, this study was executed to reveal the relationship of blood pressure to intakes of sodium, potassium, and calcium and to the sodium/calcium ratio and the sodium/potassium ratio in residents of Chungcheong province using KNHANES III data. It is hoped that this study can contribute to the creation of a guideline for the prevention and treatment of hypertension attuned to regional differences.
Subjects and Methods
Study population
The data analyzed in the present study were obtained from KNHANES III, conducted by the Ministry for Health, Welfare and Family Affairs in Korea. KNHANES has been conducted every three years since 1998, and the raw data are released to the public for scientific use. KNHANES consists of a Health Interview Survey, a Health Behavior Survey, a Health Examination Survey, and a Nutrition Survey. The surveys are given to stratified multistage samples of the South Korean population from multiple geographic areas, ages, and sexes. Trained interviewers administered structured questionnaires in participants' homes to obtain information on sociodemographic characteristics, lifestyle, health, nutritional status, and the use of dietary supplements.
In total, 33,848 people responded to KNHANES III, but only 7,597 people participated in the Health Behavior Survey, the Health Examination Survey, and the Nutrition Survey. From this group, 544 adults aged 19 years or older in Chungcheong province were selected for the present study. Data from the Health Examination Survey were used to obtain information on smoking, alcohol intake, and physical activity. Intakes of energy, sodium, potassium, and calcium were obtained from the Nutrition Survey, while data on height, weight, body mass index (BMI), blood pressure [systolic blood pressure (SBP) and diastolic blood pressure (DBP)], and pulse rate were obtained from the Health Examination Survey.
Ascertainment of hypertension
Hypertension was identified in individuals who met at least 1 of 4 criteria from the KNHANES III data: self-reports of physician diagnosis of hypertension; self-reports of antihypertensive drug intake; SBP ≥ 140 mmHg; DBP ≥ 90 mmHg. Blood pressure measurements were taken three times in a stable state, and the average SBP and DBP measurements were used to determine hypertension.
Statistical analysis
As part of the standard KNHANES data collection protocol, 24-hour dietary recalls were elicited, and here were used to estimate intakes of energy, sodium, potassium, and calcium. General characteristics, nutrient intakes, and anthropometric data were compared across the normotensive and hypertensive group. In addition, sodium, potassium, and calcium intakes were calculated per 1,000 kcal of energy. Income groups were categorized according to average monthly income in 2005 in relation to the minimum cost of living. Low income was defined as an average monthly income that was, at most, 1.2 times the minimum cost of living; middle income was defined as an average monthly income that was 1.2 to 2.5 times the minimum cost of living; and high income was defined as an average monthly income that was more than 2.5 times the minimum cost of living. Subjects were also categorized based on their educational level, defined as middle school or less (9 years and below), high school (10-12 years), and college or more (13 years or more). Present smoking status was used to classify each subject as a "current smoker", "ex-smoker", or "non-smoker". Metabolic Equivalent of Task values (METs) were used to classify physical activity as low, middle, or high. METs are multiples of the resting metabolic rates and were calculated using the short form (version 2.0, April 2004) of the International Physical Activity Questionnaire; that is, low activity was 600 > MET-minutes/week, middle activity was 600 ≤ MET-minutes/week < 3,000, and high activity was 3,000 ≤ MET-minutes/week. Responses for the question regarding following the instructions of eating a healthy diet (reducing salt consumption) were classified as "take action", "try to practice", and "do not practice".
All analyses used survey weighting to account for the complex survey design that consisted of multistage, stratified, and clustered sampling. Probability sampling weights were used with strata and primary sampling units in the data analysis. Subject characteristics were compared between the normotensive and the hypertensive groups using a chi-square test. Mean values and standard errors for nutrient intakes were calculated and t-test was used to verify significance for each normotensive and hypertensive group. To determine the impact of risk factors on high blood pressure, weight, waist circumference, sodium, potassium, and calcium intake were each classified by tertile. We estimated odds ratios (ORs) using multiple logistic regression, adjusted for age (19-29, 30-49, 50-64, ≥ 65), sex, education (middle school or lower, high school, college or higher), BMI, alcohol drinking (drinker, non-drinker), and energy intake. All statistical analyses were performed using SURVEY procedure of SAS software (version 9.12, Cary, NC, USA) and DESCRIPT procedure of SUDDAN software (release 9.0, Research Triangle Institute, Research Triangle Park, NC, USA) applying a significance level of P < 0.05.
Results
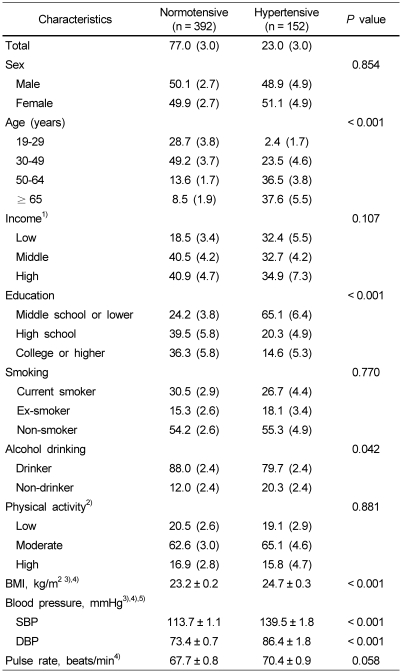
General characteristics of the participants in the normotensive and the hypertensive group are shown in Table 1. One hundred and fifty two people were classified as hypertensive subjects; the prevalence rate of hypertension was 23.0%. There was no sex difference between the normotensive and the hypertensive group: Men made up 50.1% in the normotensive group, and 49.9% of the hypertensive group. There was also no difference between the normotensive and the hypertensive group according to income, smoking, and physical activity. Persons aged 65 years or older and persons aged 50-64 years accounted for 37.6% and 36.5%, respectively, of the hypertensive subjects, significantly different from the percentages of normotensive subjects (P < 0.001). Persons who had achieved an education level of middle school or lower accounted for 65.1% in the hypertensive group, while persons in the same education level were 24.2% of the normotensive group. Alcohol drinkers accounted for 79.7% of the hypertensive group, which was significantly lower than in the normotensive group (88.0%, P = 0.042). The BMI of the hypertensive group was significantly higher than that of the normotensive group. The mean BMI in the hypertensive group was 24.7 kg/m2, significantly higher than that of the normotensive group (P < 0.001).
Table 1.
General characteristics of study subjects according to sex, age and other selected variables (Chungcheong province, KNHANES III) % (SE)
1)Low income: monthly income < minimum cost of living × 1.2
Middle income: minimum cost of living × 1.2 ≤ monthly income < minimum cost of living × 2.5
High income: monthly income ≥ minimum cost of living × 2.5
2)METs are multiples of the resting metabolic rates and calculated using the short form (version 2.0, April 2004) of the International Physical Activity Questionnaire (Low activity: 600 > MET-minutes/week, Moderate activity: 600 ≤ MET-minutes/week < 3000, and High activity: 3000 ≤ MET-minutes/week).
3)Significantly different at α = 0.05 by t-test.
4)Mean ± SE
5)SBP: systolic blood pressure, DBP: diastolic blood pressure
The mean SBP of the normotensive group was 113.7 mmHg, whereas that of the hypertensive group was 139.5 mmHg. In addition, mean DBP of the normotensive group was 73.4 mmHg. The mean DBP of the hypertensive group was 86.4 mmHg (P < 0.001). The mean pulse rate was 70.4 beats/min the hypertensive group, while that of normotensive group was 67.7 beats/min, without a significant difference (Table 1).
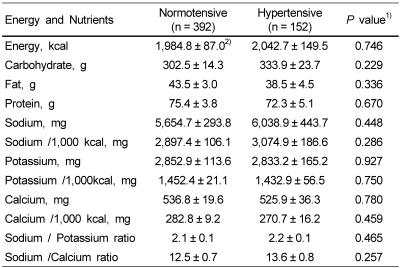
Energy and nutrient intakes of the normotensive and hypertensive subjects in Chungcheong province are shown in Table 2. No significant differences in energy and nutrient intake between the normotensive and hypertensive groups were observed. Also, the sodium/potassium ratio and sodium/calcium ratio of the hypertensive group did not differ from that of the normotensive group.
Table 2.
Energy and nutrient intakes of the normotensive and hypertensive subjects (Chungcheong province, KNHANES III)
1)Different between two groups at α = 0.05 by t-test
2)Mean ± SE
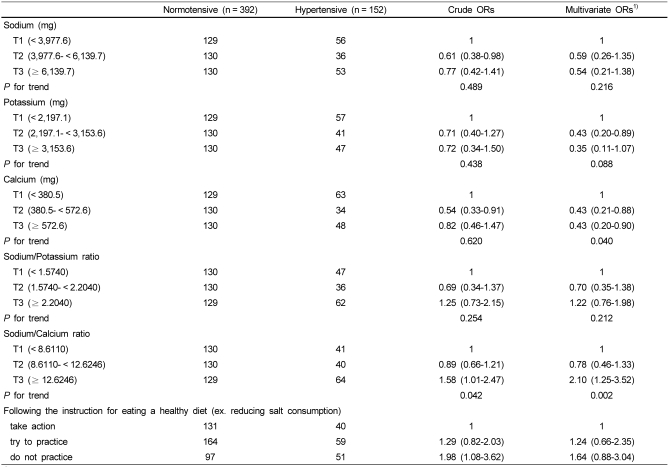
The results of logistic regression of hypertension prevalence among Korean adults by sodium, potassium, and calcium intake are shown in Table 3. Sodium intake did not show a relationship with the risk of hypertension, after adjusting for age, sex, education, BMI, alcohol drinking and energy intake. Potassium intake of T2 (2,197.1-3,153.6 mg) reduced hypertension risk by 57% compared to T1 (0- < 2,197.1 mg). A reduced risk for hypertension was most pronounced in the T2 (380.5- < 572.6 mg/day, multivariate OR = 0.43, 95% CI: 0.21-0.88) and T3 tertiles of calcium (≥ 572.6 mg/day, multivariate OR = 0.43, 95% CI: 0.20-0.90) with a significant trend in risk (P for trend = 0.040). Persons with a sodium/calcium ratio of over 12.62 had a significantly increased risk of hypertension by 110% with a significant trend in risk (multivariate OR = 2.10, 95% CI: 1.25-3.52, P for trend = 0.002). The response for following the instructions of eating a healthy diet was analyzed, and persons in the "do not practice" group had a 98% higher hypertension risk (crude OR = 1.98, 95% CI: 1.08-3.62) than those of the "take action" group (Table 3). However, multivariate ORs of the response did not differ significantly among three types of responses.
Table 3.
Odds ratios (ORs) and 95% confidence intervals (CIs) according to the intake of selected nutrients of the normotensive and hypertensive subjects (Chungcheong province, KNHANES III) ORs (95% CI)
1)Adjusted for age (19-29, 30-49, 50-64, ≥ 65), sex, education (middle school or lower, high school, college or higher), BMI, alcohol drinking (drinker, non-drinker) and energy intake.
Discussion
In the present study, we examined the effects of nutrients on blood pressure in the 19 year-old and older Korean population, especially in Chungcheong province using KNHANES III. There were significant differences in age, education level, alcohol drinking, and BMI between the normotensive and hypertensive group. Nutrient intake between normotensive and hypertensive group did not differ but raised the risk of hypertension; increased potassium and calcium intake reduced the risk of hypertension and increased sodium/calcium ratio raised 2.10 times more the risk of hypertension.
Several studies revealed that smoking was a factor that increased the risk of hypertension, whereas appropriate physical activities lowered blood pressure. Physical activity accounted for 5-14% of the population attributable risk percentage (PAR) in western populations - Finland, Italy, The Netherlands, UK, and USA [8,11-13]. However, there was no difference of smoking, and physical activities between the two groups in this study, which did not coincide with the figures in other studies. Also, there was no difference of income levels between the two groups. In contrast, there was a significant difference between the two groups with regard to education levels, alcohol drinking, and BMI. Persons with middle school or lower level accounted for 65.1% in the hypertensive group. Persons with normal blood pressure were highly educated, compared to those with hypertension. This tendency was also observed in other studies; persons with hypertension showed relatively lower education levels compared to the normotensive persons [11,14]. It is well known that increased BMI raises the risk of hypertension [13-17]. This study also demonstrated that higher BMI was related to higher risk of hypertension significantly. Overweight was an important risk factor, accounting for 11-25% PAR in the human population [7,8,12,18,19].
Logistic regression analysis was conducted in this study after grouping the tertiles of sodium, potassium and calcium intake, respectively. However, the results of the crude ORs and multivariate ORs did not differ significantly between sodium intake and risk of hypertension (P for trend = 0.489 and 0.216, respectively). High sodium intake accounted for 9-17% of PAR in western populations with national differences, and other epidemiological studies reported the association between sodium intake and hypertension [8]. The risk of hypertension was significantly elevated with increasing sodium intake in Guangxi Bai Ku Yao and Han populations in China (OR = 1.479, P = 0.002) [13]. Schroder et al. [16] reported that sodium intake increased DBP in the normotensive and non-medicated hypertensive subjects in a Mediterranean population. A recent study of NHANES III data also showed that subjects in the higher quartile of sodium intake were more likely to have a higher DBP [20]. This difference from other studies may be the result of limitations of national level cross-sectional data, although the data was adjusted for confounding factors. The variation in sodium intake was more than double the variation in calcium or potassium intake. KNHNAES III collected dietary data for one day. Furthermore, high sodium intake level may partially contribute to the discrepancy between this and other studies; the mean sodium intakes of both the hypertensive and the normotensive group in the present study was over 5,500 mg/day, which is 2.5 times higher than the recommended intake level for sodium [21].
Although sodium intake did not affect the risk of hypertension in the present study, salt intake was known to be related to sodium intake and associated with blood pressure [18,22]. Persons who responded as "do not practice" regarding following the instructions for eating a healthy diet had a 1.98 times (crude ORs, 95% CI: 1.08-3.62) higher risk of hypertension than those who were classified as "take action". Dietary management of hypertension may be more effective if the focus is on the overall nutritional profile and life style managements rather than single-nutrient intake as currently recommended for most patients.
Moderate potassium intakes (T2) reduced the risk of hypertension by 57% (OR = 0.43, 95% CI: 0.20-0.89, P for trend = 0.088), but there was no association between the sodium/potassium ratio and the risk of hypertension in this study. It is widely hypothesized that an appropriate potassium intake will lower hypertension risk. However, epidemiological evidence of the effect of potassium on blood pressure is inconsistent [12,16,23-25]. Geleijnse et al. [8] reported that low potassium intake substantially contributes to the prevalence of hypertension; they suggested that in five western countries the PAR of hypertension caused by low potassium intake was between 4% and 17%. This study also confirmed the inverse association between potassium intake and the risk of hypertension.
Metabolic and experimental studies have reported that calcium may play a role in the regulation of blood pressure. Significantly decreased OR was observed with the consumption over 380.5 mg/day of calcium in this study. Recently, we also examined the association of calcium intake and blood pressure and revealed that calcium intake was inversely associated with both SBP and DBP in the 30-49-year-old group, according to KNHANES III (data not shown), which coincided with the results of this study. Several epidemiological studies have reported that people who have a higher intake of calcium tend to have lower blood pressure. Dickinson et al. [26] conducted a meta-analysis and demonstrated that calcium supplementation is effective in lowering blood pressure and hypertension risk. They analyzed 13 randomized controlled trials and found that participants receiving calcium supplementation, when compared to controls, had a statistically significant reduction in SBP (mean difference: -2.5 mmHg, 95% CI: -4.5 mmHg to -0.6 mmHg) but not in DBP (mean difference: -0.8 mmHg, 95% CI: -2.1 mmHg to 0.4 mmHg). Another meta-analysis also combined 40 clinical trials and revealed that calcium supplementation (mean daily dose: 1,200 mg) reduced SBP by -1.86 mmHg and DBP by -0.99 mmHg [27]. A higher dietary calcium intake reduced the risk of hypertension in women over the age of 45 in the American Women's Health Study, and a calcium intake over 1,000 mg/day lowered the risk of hypertension (multivariate relative risk = 0.87) [28]. Also, the appropriate intake levels of sodium, along with a calcium intake of 800 mg or more, reduced the hypertension risk in normotensive or non-treated hypertensive populations, to that of treated hypertensive populations, respectively [16,24].
In conclusion, we found that calcium and potassium intake were associated with prevalence of hypertension in Chungcheong province, respectively. Adequate calcium and potassium intake should be encouraged and regional differences should be considered in making a healthy plan for hypertension management.
Footnotes
This work was supported by the National Cancer Center (0731060 & 0910221).
References
- 1.Singh RB, Suh IL, Singh VP, Chaithiraphan S, Laothavorn P, Sy RG, Babilonia NA, Rahman AR, Sheikh S, Tomlinson B, Sarraf-Zadigan N. Hypertension and stroke in Asia: prevalence, control and strategies in developing countries for prevention. J Hum Hypertens. 2000;14:749–763. doi: 10.1038/sj.jhh.1001057. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 3.Whitworth JA World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Death cause statistical data. KOSIS [Internet] 2009. [cited 2009 6 May]. Available from: www.kosis.kr/OLAP/Analysis/stat_olap.
- 5.Khor GL. Cardiovascular epidemiology in the Asia-Pacific region. Asia Pac J Clin Nutr. 2001;10:76–80. doi: 10.1111/j.1440-6047.2001.00230.x. [DOI] [PubMed] [Google Scholar]
- 6.Vorster HH. The emergence of cardiovascular disease during urbanisation of Africans. Public Health Nutr. 2002;5:239–243. doi: 10.1079/phn2001299. [DOI] [PubMed] [Google Scholar]
- 7.Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, Woodward M, Li X, Chalmers J, Gao R, Kong L, Yang X China NNHS Steering Committee; China NNHS Working Group. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 8.Geleijnse JM, Kok FJ, Grobbee DE. Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. Eur J Public Health. 2004;14:235–239. doi: 10.1093/eurpub/14.3.235. [DOI] [PubMed] [Google Scholar]
- 9.Han HR, Kim KB, Kang J, Jeong S, Kim EY, Kim MT. Knowledge, beliefs, and behaviors about hypertension control among middle-aged Korean Americans with hypertension. J Community Health. 2007;32:324–342. doi: 10.1007/s10900-007-9051-y. [DOI] [PubMed] [Google Scholar]
- 10.Korean Ministry of Health and Welfare. The Korean National Health and Nutrition Examination Survey - KNHANES III(2005) 2006. [Google Scholar]
- 11.Stamler J, Elliott P, Appel L, Chan Q, Buzzard M, Dennis B, Dyer AR, Elmer P, Greenland P, Jones D, Kesteloot H, Kuller L, Labarthe D, Liu K, Moag-Stahlberg A, Nichaman M, Okayama A, Okuda N, Robertson C, Rodriguez B, Stevens M, Ueshima H, Horn LV, Zhou B. Higher blood pressure in middle-aged American adults with less education-role of multiple dietary factors: the INTERMAP study. J Hum Hypertens. 2003;17:655–775. doi: 10.1038/sj.jhh.1001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sugiyama T, Xie D, Graham-Maar RC, Inoue K, Kobayashi Y, Stettler N. Dietary and lifestyle factors associated with blood pressure among U.S. adolescents. J Adolesc Health. 2007;40:166–172. doi: 10.1016/j.jadohealth.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Ruixing Y, Shangling P, Shuquan L, Dezhai Y, Weixiong L, Qiming F, Yuming C, Yaoheng H, Yijiang Z, Qinchen L. Comparison of hypertension and its risk factors between the Guangxi Bai Ku Yao and Han populations. Blood Press. 2008;17:306–316. doi: 10.1080/08037050802589593. [DOI] [PubMed] [Google Scholar]
- 14.Mellen PB, Gao SK, Vitolins MZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988-1994 and 1999-2004. Arch Intern Med. 2008;168:308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 15.Lin SJ, Lee KT, Lin KC, Cheng KH, Tsai WC, Sheu SH, Wu MT, Lee CH, Lai WT. Prevalence of prehypertension and associated risk factors in a rural Taiwanese adult population. Int J Cardiol. 2010;144:269–273. doi: 10.1016/j.ijcard.2009.01.045. [DOI] [PubMed] [Google Scholar]
- 16.Schröder H, Schmelz E, Marrugat J. Relationship between diet and blood pressure in a representative Mediterranean population. Eur J Nutr. 2002;41:161–167. doi: 10.1007/s00394-002-0372-4. [DOI] [PubMed] [Google Scholar]
- 17.Yadav S, Boddula R, Genitta G, Bhatia V, Bansal B, Kongara S, Julka S, Kumar A, Singh HK, Ramesh V, Bhatia E. Prevalence & risk factors of pre-hypertension & hypertension in an affluent north Indian population. Indian J Med Res. 2008;128:712–720. [PubMed] [Google Scholar]
- 18.Ikeda N, Gakidou E, Hasegawa T, Murray CJ. Understanding the decline of mean systolic blood pressure in Japan: an analysis of pooled data from the National Nutrition Survey, 1986-2002. Bull World Health Organ. 2008;86:978–988. doi: 10.2471/BLT.07.050195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drøyvold WB, Midthjell K, Nilsen TI, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes (Lond) 2005;29:650–655. doi: 10.1038/sj.ijo.0802944. [DOI] [PubMed] [Google Scholar]
- 20.Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III) J Gen Intern Med. 2008;23:1297–1302. doi: 10.1007/s11606-008-0645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Korean Nutrition Society. Dietary reference intakes for Koreans 2005. The Korean Nutrition Society; [Google Scholar]
- 22.He FJ, Marrero NM, Macgregor GA. Salt and blood pressure in children and adolescents. J Hum Hypertens. 2008;22:4–11. doi: 10.1038/sj.jhh.1002268. [DOI] [PubMed] [Google Scholar]
- 23.Dickinson HO, Nicolson DJ, Campbell F, Beyer FR, Mason J. Potassium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev. 2006;3:CD004641. doi: 10.1002/14651858.CD004641.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Gao SK, Fitzpatrick AL, Psaty B, Jiang R, Post W, Cutler J, Maciejewski ML. Suboptimal nutritional intake for hypertension control in 4 ethnic groups. Arch Intern Med. 2009;169:702–707. doi: 10.1001/archinternmed.2009.17. [DOI] [PubMed] [Google Scholar]
- 25.Townsend MS, Fulgoni VL, 3rd, Stern JS, Adu-Afarwuah S, McCarron DA. Low mineral intake is associated with high systolic blood pressure in the Third and Fourth National Health and Nutrition Examination Surveys: could we all be right? Am J Hypertens. 2005;18:261–269. doi: 10.1016/j.amjhyper.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 26.Dickinson HO, Nicolson DJ, Cook JV, Campbell F, Beyer FR, Ford GA, Mason J. Calcium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev. 2006;19:CD004639. doi: 10.1002/14651858.CD004639.pub2. [DOI] [PubMed] [Google Scholar]
- 27.van Mierlo LA, Arends LR, Streppel MT, Zeegers MP, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to calcium supplementation: a meta-analysis of randomized controlled trials. J Hum Hypertens. 2006;20:571–580. doi: 10.1038/sj.jhh.1002038. [DOI] [PubMed] [Google Scholar]
- 28.Wang L, Manson JE, Buring JE, Lee IM, Sesso HD. Dietary intake of dairy products, calcium, and vitamin D and the risk of hypertension in middle-aged and older women. Hypertension. 2008;51:1073–1079. doi: 10.1161/HYPERTENSIONAHA.107.107821. [DOI] [PubMed] [Google Scholar]