Abstract
Background
The Dyspnea Management Questionnaire (DMQ) is a measure of the psychosocial and behavioral responses to dyspnea for adults with COPD. The research objectives were to evaluate the reliability and validity of an expanded DMQ item pool, as a preliminary step for developing a computer adaptive test.
Methods
The original 66 items of the DMQ were used for the analyses. The sample included 63 women and 44 men with COPD (n = 107) recruited from two urban medical centers. We used confirmatory factor analysis to test the factor structure of the DMQ and its underlying cognitive-behavioral theoretical base. The internal consistency and test-retest reliability, and breadth of coverage of the expanded DMQ item bank were also evaluated.
Results
Five distinct dyspnea domains were confirmed using 56 original items of the DMQ: dyspnea intensity, dyspnea anxiety, activity avoidance, activity self-efficacy, and strategy satisfaction. Overall, the breadth of items was excellent with a good match between sample scores and item difficulty. The DMQ-56 showed good internal consistency reliability (α = .85 to .96) and good preliminary test-retest reliability over a 3-week interval (ICC = .69 to .92).
Conclusions
The DMQ demonstrated acceptable levels of reliability and validity for measuring multidimensional dyspnea outcomes after medical, psychological, and behavioral interventions for adults with COPD.
Keywords: dyspnea, anxiety, chronic obstructive pulmonary disease, outcomes research, item response theory, cognitive-behavioral therapy
Introduction
Dyspnea is the perception and experience of labored, uncomfortable breathing, and may produce secondary physiological, emotional, cognitive, and behavioral responses.1 It is the primary symptom of COPD.1–6 Such responses to dyspnea significantly impact the functional status and health-related quality of life of adults with COPD.7–8,9–11 For example, adults with COPD experience loss of social life and social withdrawal and isolation, decreased participation in leisure activities, and decreased physical functioning related to their dyspnea.8,12 Because dyspnea is multifaceted and significantly impacts the functional status and health-related quality of life of adults with pulmonary disease, a biopsychosocial approach to dyspnea assessment and treatment is essential.1,10,13–15
Several therapeutic interventions are available that focus on decreasing the disabling psychological and behavioral responses to dyspnea. These interventions include: relaxation and breathing retraining, desensitization, monitored activity training, cognitive-behavioral treatment, and education in self-management strategies.1 The individual and long term impact and benefits of these interventions in improving dyspnea in adults with COPD are however largely unknown and have not been well established.1
Limitations of Existing COPD-Specific Dyspnea Instruments
Existing dyspnea scales are very limited in their scope and comprehensiveness. Most measure either dyspnea intensity with physical activities or dyspnea self-efficacy perceptions.16–21 Current COPD instruments do not comprehensively capture the psychological, social and behavioral impact of dyspnea. For example, the University of Cincinnati Dyspnea Questionnaire (UCDQ)17 uses a one-factor model to measure dyspnea severity with physical and speech activities. The Pulmonary Functional Status and Dyspnea Questionnaire Modified (PFSDQ-M)16 measures dyspnea intensity with activities and activity levels associated with dyspnea but no other dimensions of dyspnea, using a limited range of activities. Therefore, the full impact of dyspnea on social and community participation and psychological functioning is not captured by the PFSDQ-M. Also, the COPD Self-Efficacy Scale (CSES)20, which was developed to measure individuals’ level of confidence in managing dyspnea in different situations, was found to result in high rates of missing data associated with concerns about its content validity.22
The University of California, San Diego Shortness of Breath Questionnaire (UCSD SOBQ)18, a unidimensional scale, measures dyspnea severity with activities of daily living (21 items); emotional distress of dyspnea (1 item); dyspnea cognition (1 item); and participation limitation due to dyspnea (1 item). Single items of the SOBQ are inadequate from a psychometric perspective to adequately measure the dyspnea dimensions, emotional anxiety, cognition, and participation limitation.
The Breathing Problems Questionnaire (BPQ) for patients with chronic bronchitis consists of 2 subscales: functional problems and negative evaluations.23 However, all 6 items of the negative evaluations subscale cross-load with the problems subscale indicating that the BPQ-33 most likely consists of only one factor. The items related to negative evaluations are not specific to anxiety but also relate to other emotions. The content range of the BPQ short-form is also limited.24 The BPQ requires further psychometric testing, especially of its construct validity in addition to its internal consistency and test-retest reliability.
The three subscales of the St. George’s Respiratory Questionnaire (SGRQ)25 (symptoms, activity, and impacts) do not separate out dyspnea, but instead measure several COPD symptoms combined. Similarly, only the coping skills subscale of the Seattle Obstructive Lung Disease Questionnaire26 (SOLQ) specifically measures dyspnea; it combines a question about dyspnea self-efficacy with three questions about dyspnea anxiety. The other 3 subscales of the SOLQ (physical function, emotional function, and satisfaction with care) measure the impact of lung problems in general.
The Chronic Respiratory Disease Questionnaire (CRQ)21,27 consisting of 20 items measures emotional, physical, and behavioral responses to several COPD symptoms and not dyspnea specifically, reducing its sensitivity to measuring change in dyspnea. It has two versions, an interview-administered version and a self-reported version. The individualized, nonstandardized activities of the CRQ dyspnea subscale (of both versions) render it inappropriate for comparisons between groups of patients with COPD and, therefore, randomized clinical trials.28 The CRQ dyspnea subscale has also been shown to have low internal consistency reliability.29 The interview-administered version of the CRQ has high respondent burden, as it can take 30 minutes to initially administer via interview. While the self-reported version takes less time, approximately 10 minutes, to initially complete, the individualized activities of the dyspnea subscale need to be transcribed for repeat administrations, which increases its administration burden.
Dyspnea measures such as the baseline dyspnea index (BDI)30, transition dyspnea index (TDI) 30, and the British Medical Research Council (MRC)30 are categorical scales that are further limited in their scope and precision of measurement.31 The MRC measures magnitude of tasks that provoke dyspnea while the BDI and TDI measure functional impairment, magnitude of effort, and magnitude of task associated with dyspnea. The MRC was not designed to measure dyspnea change over time.
In summary, we developed the multidimensional Dyspnea Management Questionnaire (DMQ) to overcome the deficiencies of existing instruments used in clinical and research settings for measuring treatment outcomes for patients with COPD.32 The DMQ addresses a need for a comprehensive dyspnea measure, that captures the physical, emotional (anxiety), behavioral, and cognitive aspects of dyspnea, in order to enhance our understanding of patients’ dyspnea experience and the effectiveness of treatments.
Previous research supported the reliability and validity of the DMQ in a sample of 85 participants (73 with physician-confirmed COPD and 12 with physician-confirmed asthma).30 The DMQ items were developed using qualitative interview data with patients with COPD, a comprehensive literature review, and individual semi-structured interviews with a sample of 4 adults with COPD who had participated in a pulmonary rehabilitation program and 8 interdisciplinary clinicians specializing in pulmonary medicine and rehabilitation to test the relevance and content validity of the items and subscales. Sixty-six items were rated by the12 experts to be relevant and to have content validity. The DMQ was reduced to 30 items, which were found to have high internal consistency (α = .87 to .96) and test-retest reliability over 2.5 weeks (ICC = .71 to .95). The results provided strong evidence for the concurrent validity of the dyspnea intensity, dyspnea anxiety, and activity avoidance subscales of the DMQ-30, while more testing was indicated for the activity self-efficacy and strategy satisfaction scales. The DMQ discriminated between COPD adults with different severities of lung disease. The DMQ’s factor structure and range of difficulty levels were not examined in previous work. Also, the previous research aimed to limit the number of DMQ items since the DMQ was initially designed to be administered using a fixed-format. In contrast, the current research was undertaken to begin to evaluate the psychometric properties of an expanded pool of items for the DMQ in preparation for constructing a computer adaptive test (CAT) version of the instrument, including its factor structure, internal consistency reliability, test retest reliability, and breadth using Item Response Theory (IRT) measurement techniques.33
Methods
Samples
Data on 107 subjects with pulmonary disease were derived from two sources: 73 adults with physician-confirmed pulmonary disease from our initial work32 supplemented by an additional 34 adults with physician-confirmed COPD referred for pulmonary rehabilitation at the Rusk Institute of Rehabilitation Medicine.
The Dyspnea Management Questionnaire
The DMQ consists of five conceptually-derived dyspnea dimensions: dyspnea intensity, dyspnea anxiety, activity avoidance, activity self-efficacy, and satisfaction with strategy use. Cognitive-behavioral theory underlies the DMQ including: the model of dyspnea7, the cognitive behavioral model of panic34, cognitive-perceptual model of somatic interpretation35, fear-avoidance model36, social learning theory of self-efficacy37, in addition to the theory of patient satisfaction38. The activity self-efficacy scale of the DMQ is based on the COPD self-efficacy scale.20 The DMQ uses a 7-point Likert response scale that ranges from 0 to 6 with higher scores representing better dyspnea-related function. For example, the activity avoidance scale of the DMQ ranges from (6) “never” to (0) “all the time”. To calculate each subscale score, raw values for items are summed and then divided by the number of items in the subscale to obtain a mean score. The DMQ was developed to be both a clinical and a research outcome scale to measure the effectiveness of multi-disciplinary treatments that aim to reduce the emotionally distressing and disabling responses to dyspnea and promote adaptive coping for adults with COPD.
Testing Procedures
Institutional review board approvals were obtained prior to commencing DMQ psychometric testing. Building on our previous sample32, we recruited an additional sample of 34 adults using mail survey procedures.39 Patients with a diagnosis of COPD and referred for pulmonary rehabilitation services at the pulmonary outpatient clinic in 2005 and 2006 were mailed a recruitment letter. People who consented via postcard were mailed the DMQ-66 and an informed consent form to complete and return. Respondents completed the DMQ-66 twice within a three week interval, in addition to two questions about their health stability.
Analysis
We first used a series of confirmatory factor analyses to analyze how well the data fit the theoretically derived factor structure hypothesized for the DMQ.40 This factor analysis method, based on the polychoric correlation matrix, was used because our data were not normally distributed. Since there is no universally accepted fit index, we used multiple goodness-of-fit indices including chi-square to degrees of freedom ratio41, Comparative Fit index (CFI)42, Tucker–Lewis Index (TLI)42 and Root Mean Square Error of Approximation (RMSEA) to check the model fit43. For the chi-square to degrees of freedom ratio, an index of less than 3 is generally acceptable43. CFI and TLI compare the model to a baseline null model; possible values range from 0 to 1; 0.95 or higher suggests an acceptable fit42. RMSEA assesses misfit per degree of freedom; values less than 0.08 suggest an acceptable fit, and values less than 0.05 suggest a very good fit.43
The remaining 56 items were used for all subsequent analyses. Rasch item response theory (IRT) analyses were used to estimate item difficulty parameters and compare them to person ability estimates for each subscale.44–45 Greater breadth of measurement and precision are achieved when item locations of a construct are spread across a respective continuum.46–47
To check the scale’s internal consistency, we calculated Cronbach’s alphas for each of the subscales. Test-retest reliability of the DMQ was assessed using intraclass correlation coefficients. For inclusion in test-retest reliability analyses, respondents needed to deny both hospitalization and a noticeable change in their health in the last month.
Results
Sample Characteristics
The sample consisted of 107 adults with COPD from two medical centers in New York City. A majority of adults were female (58.9%), married (42.1%), and Caucasian (73.8%); see Table 1. The mean age of participants was 75.1 years (SD = 8.6); 38.3% required supplemental oxygen use at home.
Table 1.
Demographic Background of Adults with COPD (N = 107)
| Variable | ||
|---|---|---|
| Mean Age (y) [SD] | 75.1 [8.6] | |
| Missing (%) | 6.5 | |
| Female (%) | 58.9 | |
| Time Since Diagnosis Made (y) [SD] | 4.4 [3.8] | |
| Race (%) | Caucasian | 73.8 |
| African American | 12.1 | |
| Asian | 2.8 | |
| Hispanic | 1.9 | |
| Other | 0.9 | |
| Missing | 8.4 | |
| Marital Status (%) | Married | 42.1 |
| Other | 53.3 | |
| Missing | 4.6 | |
| Oxygen Use at Home (%) | Yes | 38.3 |
| Missing | 4.7 | |
Construct Validity: Dyspnea Domains
Confirmatory factor analysis supported the five-factor conceptually-derived model for the DMQ: Dyspnea Intensity, Dyspnea Anxiety, Activity Avoidance, Activity Self-efficacy, and Strategy Satisfaction (see Tables 2 and 3). The first factor, dyspnea intensity, consisting of 12 items, is the amount of dyspnea experienced with performing self-care, mobility, home management, community, leisure, and social activities. Dyspnea anxiety, consisting of 16 items, is the magnitude of anxiety symptoms associated with shortness of breath. Activity avoidance, comprised of 15 items, is the extent to which anxiety symptoms, related to dyspnea, contribute to avoidance of daily activities. Activity self-efficacy, with 6 items, is an individual’s perceived confidence in being able to manage shortness of breath with activity participation. Strategy satisfaction, comprised of 7 items, is the individual’s evaluation of his or her mastery of dyspnea management strategies.
Table 2.
Overall Fit Indices for the Five Factor Model (N = 107)
| No | Model | No. Items | Chi-square (DF) | Ratio | P | CFI | TLI | RMSEA | Removed Items* |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 5-Factor | 66 | 133.37 (41) | 3.25 | 0.0000 | 0.820 | 0.873 | 0.146 | - |
| 2 | 5-Factor | 64 | 112.75 (47) | 2.40 | 0.0000 | 0.895 | 0.935 | 0.115 | IIA2, IIA6 |
| 3 | 5-Factor | 62 | 96.78 (46) | 2.10 | 0.0000 | 0.922 | 0.952 | 0.103 | IIA2, IIA6, V9, V11 |
| 4 | 5-factor | 56 | 78.15 (45) | 1.74 | 0.0016 | 0.953 | 0.973 | 0.084 | IIA2, IIA6, V9, V11, V6, V8, V7, IV2, V4, 3A3 |
| 5 | 5-factor | 56 | 57.67 (36) | 1.60 | 0.0124 | 0.969 | 0.978 | 0.076 | Same as model 4, but fixed the correlation in F1 and F5, F5 and F3 at 0 |
Notes.
based on modification indices; CFI = comparative fit index, TLI = Tucker–Lewis index, RMSEA = root mean square error of approximation
Table 3.
Factor Loadings and Standard Errors for Five-Factor Model (N = 107)
| Items | Estimation* | SE |
|---|---|---|
| Dyspnea Intensity: | ||
| DI1. Getting dressed | 0.850 | 0.036 |
| DI2. Showering or bathing | 0.862 | 0.036 |
| DI3. Reaching above your head | 0.842 | 0.041 |
| DI4. Bending down | 0.786 | 0.046 |
| DI5. Walking indoors for 40 feet | 0.891 | 0.031 |
| DI6. Walking outdoors for 2 blocks | 0.835 | 0.043 |
| DI7. Walking uphill for 1 block | 0.758 | 0.044 |
| DI8. Carrying a 5–7 pound shopping bag 40 feet | 0.814 | 0.042 |
| DI9. Climbing one flight of stairs | 0.824 | 0.038 |
| DI10. Talking with other people for half an hour while seated | 0.661 | 0.064 |
| DI11. Engaging in active leisure pursuits | 0.810 | 0.046 |
| DI12. Participating in social activities in your community | 0.884 | 0.039 |
| F2: Dyspnea Anxiety | ||
| DA1A. Nervous during breathing difficulty | 0.763 | 0.048 |
| DA2A. Worried in general about your shortness of breath | 0.800 | 0.042 |
| DA3A. Afraid when it was hard for you to breathe | 0.766 | 0.046 |
| DA4A. Panicked when you couldn’t breathe well | 0.776 | 0.048 |
| DA5A. Upset when you had to stop and rest due to shortness of breath | 0.745 | 0.047 |
| DA6A. Tense if you thought about prior episodes of shortness of breath | 0.774 | 0.05 |
| DA7A. You had little control over your shortness of breath | 0.679 | 0.059 |
| DAB1. Intense breathing discomfort | 0.776 | 0.049 |
| DAB2. Your shortness of breath being life-threatening | 0.822 | 0.047 |
| DAB3. Panicking during a future breathing attack | 0.913 | 0.035 |
| DAB4. Chest tightness | 0.792 | 0.054 |
| DAB5. Delay in your breathing returning to normal after activity | 0.707 | 0.057 |
| DAB6. Increased breathing effort with exercise | 0.625 | 0.063 |
| DAB7. Not surviving an episode of shortness of breath | 0.828 | 0.048 |
| DAB8. Loss of breathing control during routine daily activities | 0.825 | 0.044 |
| DAB9. Something terrible happening to you when short of breath | 0.826 | 0.045 |
| F3: Activity Avoidance | ||
| AA1A. Hold back from doing activities that you enjoy | 0.883 | 0.031 |
| AA2A. Stay at home more often than you wanted to | 0.887 | 0.031 |
| AA3A. Stay sitting for long periods of time | 0.748 | 0.046 |
| AA4A. Keep to yourself or avoid seeing other people | 0.681 | 0.057 |
| AA5A. Be less active than you would have liked to be | 0.814 | 0.04 |
| AAB1. Bending down | 0.779 | 0.049 |
| AAB2. Walking | 0.863 | 0.035 |
| AAB3. Physically exercising | 0.840 | 0.036 |
| AAB4. Climbing stairs | 0.797 | 0.045 |
| AAB5. Doing housework | 0.863 | 0.036 |
| AAB6. Shopping | 0.864 | 0.036 |
| AAB7. Participating in family activities | 0.880 | 0.035 |
| AAB8. Pursuing active leisure interests | 0.847 | 0.039 |
| AAB9. Social activities in your community | 0.856 | 0.038 |
| AAB10. Engaging in sexual activities | 0.655 | 0.064 |
| F4: Activity Self-Efficacy | 0.914 | 0.082 |
| SE1. Do light physical activity | 0.870 | 0.102 |
| SE2. Walk outdoors | 0.437 | 0.109 |
| SE3. Experience extreme cold or hot weather conditions | 0.749 | 0.074 |
| SE4. Experience stressful situations | 0.629 | 0.098 |
| SE5. Smell strong odors | 0.754 | 0.079 |
| SE6. Travel far from home | 0.914 | 0.082 |
| F5: Strategy Satisfaction | ||
| SS1. Use controlled breathing when feeling stressed | 0.942 | 0.047 |
| SS2. Use controlled breathing with daily activities | 0.842 | 0.045 |
| SS3. Use controlled breathing with exercise | 0.732 | 0.061 |
| SS4. Use relaxation techniques | 0.854 | 0.048 |
| SS5. Take medications correctly as prescribed | 0.642 | 0.073 |
| SS6. Keep good eating habits | 0.437 | 0.106 |
| SS7. Assert your needs | 0.555 | 0.082 |
all factor loadings: p<0.05
Analyses of modification indices resulted in 10 of the 66 items being removed from the model. Two items, confident that you could relieve your shortness of breath, calm even if your breathing took effort, were deleted due to poor item fit. In a 5-factor CFA, removing these two items from the 2nd factor improved the model fit (CFI = 0.895, TLI = 0.935, RMSEA = 0.115). Eight additional items were removed from the 3rd, 4th, and 5th factors based on the modification indices, further improving the model fit (Chi-square (DF) = 78.15 (45), CFI = 0.953, TLI = 0.973, RMSEA = 0.084). These items were respectively: avoid smoking, exercise regularly, lean forward to recover from exercise or activity, protect lungs, use devices that help you save energy, do moderate physical activity, use efficient movements, and keep strong emotions inside. Correlations between 3rd factor and 5th factor, 1st factor and 5th factor were not significant. Therefore, we fixed these three correlations at 0, which further improved the model fit (Chi-square (DF) = 57.67(35), CFI=0.969, TLI=0.978, RMSEA=0.076). Three of the DMQ factors, Dyspnea Intensity, Dyspnea Anxiety, and Activity Avoidance, were moderately to highly correlated (r = 0.69 to 0.80); see Table 4.
Table 4.
Factor Correlations.
| F1 | F2 | F3 | F4 | |
|---|---|---|---|---|
| F1: Dyspnea Intensity | - | |||
| F2: Dyspnea Anxiety | 0.688** | - | ||
| F3: Activity Avoidance | 0.802** | 0.788** | - | |
| F4: Activity Self-Efficacy | 0.180** | 0.232** | 0.252** | - |
| F5: Strategy Satisfaction | 0* | 0.247** | 0* | 0.497** |
Fixed Parameter
p < 0.05
Item Calibrations
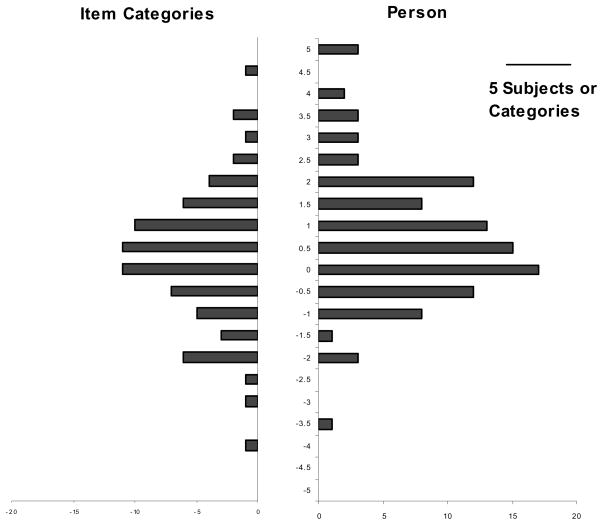
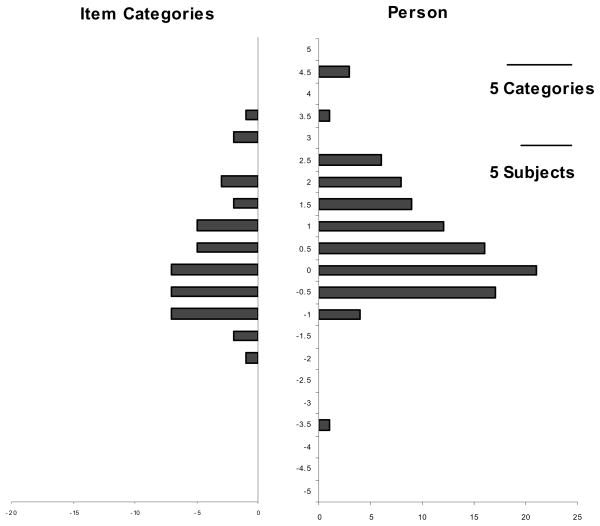
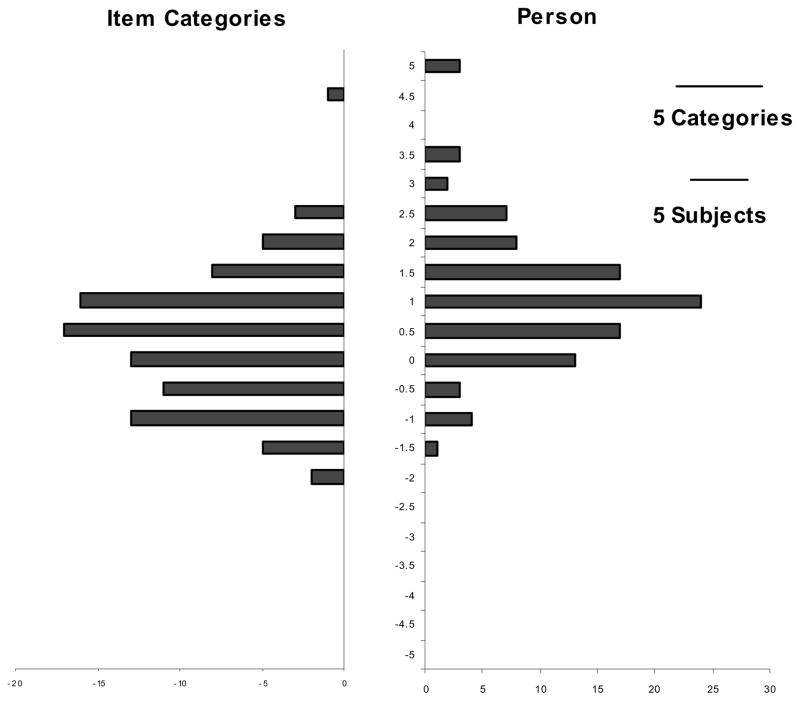
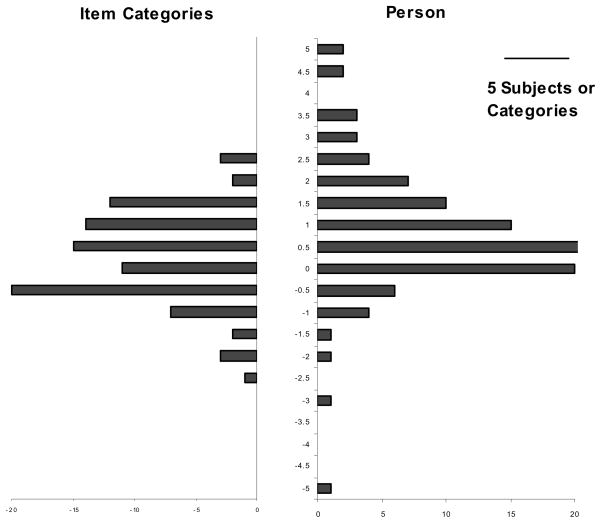
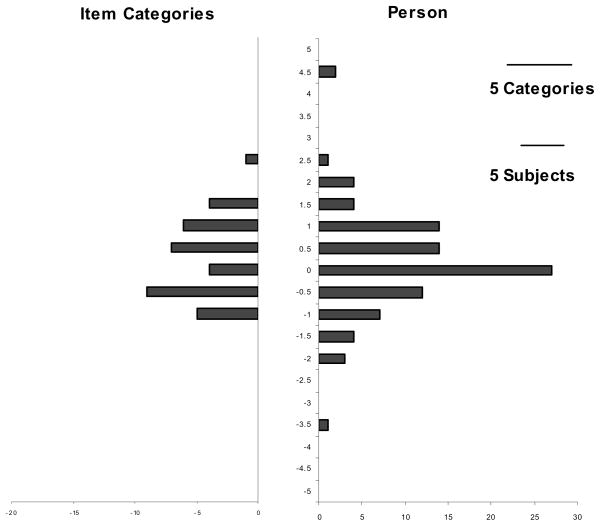
The breadths of the five DMQ subscales are shown as item-person histograms in Figures 1 to 5. They show the hierarchical distributions of estimated item difficulty and person ability with zero indicating the standardized mean or midpoint of difficulty of each subscale. Floor and ceiling effects were minimal. Floor effects ranged from 0 to 1% (n = 1) and ceiling effects were 0 to 2% (n = 2) for the five subscales.
Figure 1.
Item Person Map (Dyspnea Intensity)
Figure 5.
Item Person Map (Strategy Satisfaction)
Reliability
The Cronbach’s alphas for each of the DMQ subscales ranged from .85 to .96 (see Table 5). We estimated the test retest reliability of the DMQ over a mean interval of 3 weeks (21.5 days, SD = 10.97) using intraclass correlation coefficients (ICC). ICCs ranged between .69 and .92 for the five subscales (see Table 6).
Table 5.
Internal Consistency Reliability of the Five-Factor Model
| Scale | Cronbach’s Alpha | Number of items | Mean | Variance | N |
|---|---|---|---|---|---|
| Dyspnea Intensity | 0.95 | 12 | 3.53 | .71 | 103 |
| Dyspnea Anxiety | 0.95 | 16 | 4.20 | .31 | 99 |
| Activity Avoidance | 0.96 | 15 | 3.76 | .20 | 91 |
| Activity Self-Efficacy | 0.86 | 6 | 2.91 | .09 | 92 |
| Strategy Satisfaction | 0.85 | 7 | 3.76 | .31 | 92 |
Table 6.
Test-Retest Reliability of the DMQ over a 3.1 week interval (N =35)
| Dimension | ICC | N | p Values |
|---|---|---|---|
| Dyspnea Intensity | .91 | 33 | <.001 |
| Dyspnea Anxiety | .88 | 31 | <.001 |
| Activity Avoidance | .92 | 31 | <.001 |
| Activity Self-Efficacy | .83 | 32 | <.001 |
| Strategy Satisfaction | .69 | 32 | <.001 |
ICC: Intraclass Correlation Coefficient
The response rate was 51% for re-administration of the DMQ. Some respondents (n = 12) were not asked to complete the DMQ twice because they did not consent to receive a follow-up survey; had fallen; died; completed the questionnaire with assistance (n = 1); or skipped sections of the questionnaire the first time. A sample of 35 adults with stable COPD was used. The sample was 65.7% female, 42.9% married, 94.3% Caucasian, and had a mean age of 75.7 years (SD = 7.26). Test retest participants differed significantly on use of supplemental oxygen, requiring less oxygen at home, compared to participants who did not respond twice (p = .02); all other demographics did not differ significantly between the two groups.
Discussion
We confirmed the five-factor structure of the DMQ with 56 items. The strengths of the DMQ are its comprehensive, multi-factor model structure of dyspnea and wide range of item difficulty levels. The dyspnea domains of anxiety, activity avoidance, and strategy satisfaction are not measured by any other dimensional dyspnea instrument for adults with COPD. The multifactorial model of the DMQ facilitates the study of dyspnea to determine which dimensions specifically improve after clinical interventions. The DMQ can help to, (1) improve dyspnea measurement in clinical and research settings for adults with COPD, (2) increase our understanding of how to improve dyspnea symptom management, and (3) facilitate the appropriate selection of patients for different dyspnea interventions. The DMQ is intended to be used as both a clinical and research outcome tool, to compare individual and group dyspnea scores, for adults with COPD in order to evaluate the effectiveness of clinical interventions, including adjunctive pulmonary rehabilitation therapies whose benefits are largely unknown48–49.
The appropriate selection of a dyspnea assessment to measure dyspnea change should be based on a match between the dimensions measured and the dimensions of dyspnea targeted by the treatment. If treatment specifically targets psychological and behavioral dimensions of dyspnea, then the DMQ is a good choice to evaluate the effectiveness of the medical, cognitive-behavioral, or rehabilitative treatment component. For example, if therapy is designed to (1) increase a person’s dyspnea tolerance, (2) limit the distress and disabling effects of dyspnea, and or (3) facilitate a healthy, active lifestyle and coping strategies, then the DMQ would be a good outcome instrument to use.
Although there were moderate to high correlations between three of the DMQ factors, extensive model fitting was completed and the best model fit was achieved with a solution that revealed five distinct and interpretable domains. All confirmatory factor analysis fit indices met acceptable standards using 56 items of the DMQ.
In developing the current version of the DMQ, 10 items were removed (from the initial pool of 66 DMQ items) following factor analyses. Most of these items came from factor five, strategy satisfaction. The specific coping strategies of using efficient movements and forward leaning postures, assistive devices, avoiding environmental lung irritants and smoking, and exercising regularly were removed. Less diversity in coping strategies is measured by the strategy satisfaction scale as a result. The item, “do moderate physical activity” did not fit the activity self-efficacy scale. This may indicate that the examples given for this item, carrying grocery bags or climbing 1 flight of stairs, need to be measured separately for improved construct validity.
The DMQ-56 improves on the breadth of measurement compared to the DMQ-30. For example, many more physical and social activities are included in the dyspnea intensity and activity avoidance scales, including “getting dressed”, “reaching above your head”, “bending down”, “talking with other people”, and “sexual activities”. The larger item pool for the dyspnea anxiety scale includes more items representing hypervigilance and catastrophic interpretation responses to dyspnea, including thoughts about lack of control and death and dying. The activity self-efficacy scale includes more items about managing dyspnea in different environmental contexts.
IRT techniques provided support for the breadth of measurement across different ranges of ability levels for each factor of the DMQ. Overall, IRT analyses showed excellent breadth of the DMQ for the five subscales and a good match of item difficulty compared to sample distributions. There was a very good match for the dyspnea intensity subscale between items and abilities. For dyspnea anxiety, while the match was good, item locations were skewed toward the lower end of the logit scale compared to subjects’ abilities. For the activity avoidance subscale, item difficulty matched person ability except for a few people functioning at the highest (most difficult) level of the continuum. For the activity self-efficacy and strategy satisfaction subscales, items matched sample distributions well except at the very lowest functional proficiency of the scales. Further testing is needed with diverse samples of patients with COPD to confirm that the IRT item calibrations can be generalized to the larger population of adults with COPD.
The results also provided support for the internal consistency and test-retest reliability over a 3-week interval of the DMQ. The results of the test-retest reliability analyses are preliminary given the response rate for retesting and since results cannot be generalized to patients who require higher levels of supplemental oxygen. Further test-retest reliability testing is needed to confirm the results in a more heterogeneous sample with respect to ethnicity and supplemental oxygen use. A 3 week interval may also have been too long for test-retest reliability since 17 individuals (31.5%) reported a change in health in this time period.
The newly expanded 56 items of the DMQ also provide the foundation for developing a computer adaptive test (CAT)50 version of this instrument. In preparation for using computer adaptive testing, we were interested to evaluate the reliability and validity of a larger DMQ item pool. CAT applications require a large set of items in any one outcome domain, items that consistently scale along a dimension of low to high proficiency. CAT and item response theory (IRT)51–52 techniques are currently being applied to the development of a new generation of function and disability assessment instruments52–53 and we believe may be ideally suited for dyspnea assessment.
We believe our sample for field testing the DMQ items was a reasonably representative sample of adults with COPD for which the DMQ was intended. Our patient sample had a verified diagnosis of COPD and was obtained from two medical centers. The DMQ is intended for both clinical and research use with adults with COPD. It can be employed to compare individual patient’s and groups of patients’ dyspnea scores before and after clinical interventions such as pulmonary medicine, pulmonary rehabilitation, cognitive-behavioral therapy, controlled breathing training, exercise therapy, psychological support, desensitization, relaxation therapy, and interdisciplinary self-management education in order to ascertain their effectiveness.
A limitation of this study was the small sample size. MacCallum et al.54–56, however, provided evidence that a stable, valid factor solution with close approximation to the major common factors can be achieved with smaller sample sizes. They contended that the effect of sampling error is minimal if unique loadings or variances are consistently low. MacCallum et al.’s research refutes traditional rules of thumb about sample size in factor analysis. Nonetheless, we need to interpret the confirmatory factor analysis findings with some caution given their preliminary nature.
Our study findings may have selection bias resulting from low initial responses to mailed recruitment letters. We were however unable to estimate whether responders differed from non-responders because medical data on non-responders was not available to the researchers. The results of our study, using a sample of patients from two New York City medical centers, may not generalize to the larger U.S. population of adults with COPD. Therefore, further psychometric testing of the DMQ using samples from other parts of the U.S. would be useful.
Conclusions
The DMQ-56 improves on the conceptual clarity and measurement breadth of the DMQ-30. The results of this study provide preliminary empirical evidence of five distinct dimensions of dyspnea represented by 56 items of the DMQ, capturing a wide continuum of functional abilities and satisfaction levels. The expanded DMQ-56 meets a need to comprehensively measure the cognitive, emotional, sensory, and behavioral components of dyspnea for adults with COPD. It uses dimensional scaling and IRT analyses to measure the distinct dyspnea domains of dyspnea intensity, dyspnea anxiety, activity avoidance, activity self-efficacy, and strategy satisfaction. The 56-item DMQ demonstrated good psychometric properties including internal consistency and test retest reliability and construct validity. The results support using the DMQ to measure change in dyspnea functioning following clinical interventions for adults with COPD.
The analyses undertaken and results from this study were important preparatory steps for future work to build dyspnea item banks and apply computer adaptive testing methods for dyspnea outcome measurement in adults with COPD. The study results provide a beginning foundation on which to develop a CAT version of the DMQ that has the potential to further improve the instrument’s feasibility of administration, breadth of measurement, and sensitivity to clinically meaningful change in dyspnea-related outcomes. Future work planned on the DMQ will also include evaluating its responsiveness to change following therapeutic pulmonary interventions.
Figure 2.
Item Person Map (Dyspnea Anxiety)
Figure 3.
Item Person Map (Activity Avoidance)
Figure 4.
Item Person Map (Activity Self-Efficacy)
Acknowledgments
This research was funded by the National Institute on Disability and Rehabilitation Research, U.S. Department of Education (H133F040015) and subsequently by the National Heart, Lung, and Blood Institute (1R21HL091237-01).
Supported in part by grant H133F040015 from the National Institute on Disability and Rehabilitation Research, and subsequently by grant R21HL091237-01 from the National Heart, Lung, and Blood Institute/National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Thoracic Society. Dyspnea: mechanisms, assessment, and management: a consensus statement. Am J Respir Crit Care Med. 1999;159:321–340. doi: 10.1164/ajrccm.159.1.ats898. [DOI] [PubMed] [Google Scholar]
- 2.Breslin EH. Breathing retraining in chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 1995;15:25–33. doi: 10.1097/00008483-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Lareau SC, Breslin EH, Meek PM. Functional status instruments: outcome measure in the evaluation of patients with chronic obstructive pulmonary disease. Heart Lung. 1996;25:212–224. doi: 10.1016/s0147-9563(96)80032-x. [DOI] [PubMed] [Google Scholar]
- 4.O’Donnell DE, McGuire M, Samis L, Webb KA. The impact of exercise reconditioning on breathlessness in severe chronic airflow limitation. Am J Respir Crit Care Med. 1995;152:2005–2013. doi: 10.1164/ajrccm.152.6.8520769. [DOI] [PubMed] [Google Scholar]
- 5.Sassi-Dambron DE, Eakin EG, Ries AL, Kaplan RM. Treatment of dyspnea in COPD: a controlled clinical trial of dyspnea management strategies. Chest. 1995;107:724–729. doi: 10.1378/chest.107.3.724. [DOI] [PubMed] [Google Scholar]
- 6.Meek PM. Measurement of dyspnea in chronic obstructive pulmonary disease: what is the tool telling you? Chron Respir Dis. 2004;1:29–37. doi: 10.1191/1479972304cd008ra. [DOI] [PubMed] [Google Scholar]
- 7.Carrieri-Kohlman V, Douglas MK, Gormley JM, Stulbarg MS. Desensitization and guided mastery: treatment approaches for the management of dyspnea. Heart Lung. 1993;22:226–234. [PubMed] [Google Scholar]
- 8.Hu J, Meek P. Health-related quality of life in individuals with chronic obstructive pulmonary disease. Heart Lung. 2005;34:415–422. doi: 10.1016/j.hrtlng.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Morgan MDL, Singh SJ, Hyland ME. The relationship between physical activity and quality of life in chronic lung disease. Eur Respir Rev. 1997;7:57–59. [Google Scholar]
- 10.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA. 1995;273:59–65. [PubMed] [Google Scholar]
- 11.Moody L, McCormick K, Williams A. Disease and symptom severity, functional status, and quality of life in chronic bronchitis and emphysema. Journal of Behavioral Medicine. 1990;13:297–306. doi: 10.1007/BF00846836. [DOI] [PubMed] [Google Scholar]
- 12.McCathie HCF, Spence SH, Tate RL. Adjustment to chronic obstructive pulmonary disease: the importance of psychological factors. Eur Respir J. 2002;19:47–53. doi: 10.1183/09031936.02.00240702. [DOI] [PubMed] [Google Scholar]
- 13.Carrieri-Kohlman V, Gormley JM, Douglas MK, Paul SM, Stulbarg MS. Differentiation between dyspnea and its affective components. Western Journal of Nursing Research. 1996;18:626–633. doi: 10.1177/019394599601800602. [DOI] [PubMed] [Google Scholar]
- 14.Smoller JW, Pollack MH, Otto MW, Rosenbaum JF, Kradin RL. Panic anxiety, dyspnea, and respiratory disease: theoretical and clinical considerations. Am J Respir & Crit Care Med. 1996;154:6–17. doi: 10.1164/ajrccm.154.1.8680700. [DOI] [PubMed] [Google Scholar]
- 15.Gift AG. Therapies for dyspnea relief. Holistic Nurs Pract. 1993;7:57–63. [PubMed] [Google Scholar]
- 16.Lareau SC, Meek PM, Roos PJ. Development and testing of the modified version of the pulmonary functional status and dyspnea questionnaire (PFSDQ-M) Heart Lung. 1998;27:159–168. doi: 10.1016/s0147-9563(98)90003-6. [DOI] [PubMed] [Google Scholar]
- 17.Hodgev V, Kostianev S, Marinov B. University of Cincinnati Dyspnea questionnaire for evaluation of dyspnoea during physical and speech activities in patients with chronic obstructive pulmonary disease: a validation analysis. Clin Physiol Funct Imaging. 2003;23:269–274. doi: 10.1046/j.1475-097x.2003.00506.x. [DOI] [PubMed] [Google Scholar]
- 18.Eakin EG, Resnikoff PM, Prewitt LM, Ries AL, Kaplan RM. Validation of a new dyspnea measure: the UCSD shortness of breath questionnaire. Chest. 1998;113:619–624. doi: 10.1378/chest.113.3.619. [DOI] [PubMed] [Google Scholar]
- 19.Lee L, Friesen M, Lambert IR. Evaluation of dyspnea during physical and speech activities in patients with pulmonary diseases. Chest. 1998;113:625–632. doi: 10.1378/chest.113.3.625. [DOI] [PubMed] [Google Scholar]
- 20.Wigal JK, Creer TL, Kotses H. The COPD self-efficacy scale. Chest. 1991;99:1193–1196. doi: 10.1378/chest.99.5.1193. [DOI] [PubMed] [Google Scholar]
- 21.Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773–778. doi: 10.1136/thx.42.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Migliore Norweg A, Whiteson J, Malgady R, Mola A, Rey M. The effectiveness of different combinations of pulmonary rehabilitation program components: A randomized controlled trial. CHEST. 2005;128:663–672. doi: 10.1378/chest.128.2.663. [DOI] [PubMed] [Google Scholar]
- 23.Hyland ME, Bott J, Singh S, Kenyon CA. Domains, constructs and the development of the breathing problems questionnaire. Qual Life Res. 1994;3:245–256. doi: 10.1007/BF00434898. [DOI] [PubMed] [Google Scholar]
- 24.Haave E, Hyland ME, Engvik H. Physical and emotional aspects of self-reported health status: a two-factor model of the short-form Breathing Problems Questionnaire. Chron Respir Dis. 2005;2:21–26. doi: 10.1191/1479972305cd057oa. [DOI] [PubMed] [Google Scholar]
- 25.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145:1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 26.Tu SP, McDonell MB, Spertus JA, Steele BG, Fihn SD. A new self-administered questionnaire to monitor health-related quality of life in patients with COPD. Ambulatory Care Quality Improvement Project (ACQUIP) Investigators. Chest. 1997;112:614–622. doi: 10.1378/chest.112.3.614. [DOI] [PubMed] [Google Scholar]
- 27.Williams J, Singh S, Sewell L, Guyatt GH, Morgan MD. Development of a self-reported chronic respiratory questionnaire (CRQ-SR) Thorax. 2001;56:954–959. doi: 10.1136/thorax.56.12.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guell R, Casan P, Sangenis M, Morante F, Belda J, Guyatt GH. Quality of life in patients with chronic respiratory disease: the Spanish version of the Chronic Respiratory Questionnaire (CRQ) Eur Respir J. 1998;11:55–60. doi: 10.1183/09031936.98.11010055. [DOI] [PubMed] [Google Scholar]
- 29.Wijkstra PJ, TenVergert EM, Van Altena R, Otten V, Postma D, Kraan J, Koëter GH. Reliability and validity of the chronic respiratory questionnaire (CRQ) Thorax. 1994;49:465–467. doi: 10.1136/thx.49.5.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea: contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984;85:751–758. doi: 10.1378/chest.85.6.751. [DOI] [PubMed] [Google Scholar]
- 31.Jette AM, Norweg A, Haley SM. Achieving meaningful quantification of ICF domains. Disability & Rehabilitation. 2008;30(12):963–969. doi: 10.1080/09638280701800426. [DOI] [PubMed] [Google Scholar]
- 32.Migliore Norweg A, Whiteson J, Demetis S, Rey M. A new functional status outcome measure of dyspnea and anxiety for adults with lung disease: the dyspnea management questionnaire (DMQ-30) J Cardiopulm Rehabil. 2006;26:395–404. doi: 10.1097/00008483-200611000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Jette AM, Haley SM. Contemporary measurement techniques for rehabilitation outcome assessment. J Rehabil Med. 2005;37:339–345. doi: 10.1080/16501970500302793. [DOI] [PubMed] [Google Scholar]
- 34.Moore MC, Zebb BJ. The catastrophic misinterpretation of physiological distress. Behavior Research and Therapy. 1999;37:1105–1118. doi: 10.1016/s0005-7967(98)00197-1. [DOI] [PubMed] [Google Scholar]
- 35.Cioffi D. Beyond attentional strategies: cognitive-perceptual model of somatic interpretation. Psychol Bull. 1991;109:25–41. doi: 10.1037/0033-2909.109.1.25. [DOI] [PubMed] [Google Scholar]
- 36.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 38.Linder-Pelz S. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16:577–582. doi: 10.1016/0277-9536(82)90311-2. [DOI] [PubMed] [Google Scholar]
- 39.Salant P, Dillman DA. How to conduct your own survey. New York: John Wiley & Sons, Inc; 1994. [Google Scholar]
- 40.Muthen BO, Muthen LK. Mplus: Statistical analysis with latent variables. Los Angeles: Statmodel; 2001. [Google Scholar]
- 41.Kline RB. Principles and practices of structural equation modeling. New York: Guilford; 1998. [Google Scholar]
- 42.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 43.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Thousand Oaks, CA: 1993. pp. 136–162. [Google Scholar]
- 44.Fischer G, Molenaar I. Rasch models: Foundations, recent developments, and applications. Berlin: Springer-Verlag; 1995. [Google Scholar]
- 45.Andrich D. Rasch models for measurement. Beverly Hills, CA: Sage Publications; 1998. [Google Scholar]
- 46.McHorney CA. Health status assessment methods for adults: accomplishments and future challenges. Annu Rev Public Health. 1999;20:309–335. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]
- 47.Siebens H, Andreas PL, Pengsheng N, Coster WJ, Haley SM. Measuring physical function in patients with complex medical and postsurgical conditions: a computer adaptive approach. Am J Phys Med Rehabil. 2005;84:741–748. doi: 10.1097/01.phm.0000186274.08468.35. [DOI] [PubMed] [Google Scholar]
- 48.Devine and Pearcy. Devine C, Pearcy J. Meta-analysis of the effects of psychoeducational care in adults with chronic obstructive pulmonary disease. Patient Education and Counseling 1996. 1996;29:167–178. doi: 10.1016/0738-3991(96)00862-2. [DOI] [PubMed] [Google Scholar]
- 49.Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2006;(4) doi: 10.1002/14651858.CD003793.pub2. Art. No.: CD003793. [DOI] [PubMed] [Google Scholar]
- 50.Ware J, Bjorner J, Kosinski M. Practical implications of item response theory and computerized adaptive testing. Med Care. 2000;38(Suppl 2):73–82. [PubMed] [Google Scholar]
- 51.McHorney C, Cohen A. Equating health status measures with item response theory. Med Care. 2000;38(9, Suppl 2):43–59. doi: 10.1097/00005650-200009002-00008. [DOI] [PubMed] [Google Scholar]
- 52.Hambleton R. Emergence of item response modeling in instrument development and data analysis. Med Care. 2000;38(9 Supplement 2):60–65. doi: 10.1097/00005650-200009002-00009. [DOI] [PubMed] [Google Scholar]
- 53.Fries JF, Bruce B, Cella D. The promise of PROMIS: using item response theory to improve assessment of patient-reported outcomes. Clin Exp Rheumatol. 2005;39:S53–7. [PubMed] [Google Scholar]
- 54.MacCallum RC, Tucker LR. Representing sources of error in the common-factor model: implications for theory and practice. Psychol Bull. 1991;109:502–511. [Google Scholar]
- 55.MacCallum RC, Widaman KF, Preacher KJ, Hong S. Sample size in factor analysis: the role of model error. Mult Behav Res. 2001;36:611–637. doi: 10.1207/S15327906MBR3604_06. [DOI] [PubMed] [Google Scholar]
- 56.MacCallum RC. Working with imperfect models. Mult Behav Res. 2003;38:113–139. doi: 10.1207/S15327906MBR3801_5. [DOI] [PubMed] [Google Scholar]