Abstract
Context: Historically, successful surgical management of primary hyperparathyroidism has required bilateral exploration of the neck. By confirming complete removal of hypersecreting tissue, an intraoperative parathyroid hormone (IO-PTH) assay allows use of a more limited procedure.
Objective: Our objective was to evaluate the utility of IO-PTH assay used in 32 parathyroid explorations versus conventional bilateral exploration used before the advent of IO-PTH assays.
Methods: Minimally invasive parathyroidectomy (MIP) was used. Plasma samples were obtained at several intervals and were analyzed for IO-PTH by use of a rapid immunochemiluminescent assay (ICMA). Outcomes were assessed by univariate inferential testing, yielding one-tailed t-test results.
Results: The study group had a mean plasma IO-PTH level decrease of 87% at ten minutes after excision. All 32 patients who underwent MIP using IO-PTH monitoring had successful surgery. At last postoperative follow-up examination, all 32 patients were normocalcemic. There were statistically significant decreases in duration of surgery, length of hospital stay, and surgery cost.
Conclusions: IO-PTH levels predicted the postoperative outcome for all patients studied, can provide valuable information to surgeons, and can decrease the duration of surgery and hospital stay.
Introduction
Primary hyperparathyroidism (PHPT) has become a common disease, affecting an estimated 28 per 100,000 people each year in the United States.1 Increased recognition of PHPT—resulting from advances in screening tests—has produced a clinical profile of hyperparathyroidism characterized by mild hypercalcemia with absent or subtle symptoms. The number of parathyroidectomies performed for PHPT has also increased dramatically since 1996. In the surgical management of PHPT, intraoperative PTH (IO-PTH) assays have been shown to improve the success of parathyroid gland surgery.2–4 Minimally invasive parathyroidectomy (MIP) has replaced the traditional four-gland bilateral exploration as the procedure preferred by many institutions.1,5
Surgical treatment of PHPT is challenging and carries uncertainty concerning presence or absence of disease in a single gland, two glands, or several hyperplastic glands.6 Sestamibi scans2–4 can provide some information about locating adenomas, but they may not be sensitive enough to detect second adenomas or multigland hyperplasia. Historically, endocrine surgeons have performed bilateral exploration to ensure detection of the reported 5% to 30% incidence of second hyperplastic glands. The success of surgical treatment depends on successfully localizing abnormal glands. Difficulties associated with parathyroidectomy relate to variability in the number of parathyroid glands, different locations of normal and abnormal glands, and problems distinguishing normal from subtly diseased glands.7 Although 80% to 85% of parathyroid adenomas are found adjacent to the thyroid gland in its normal location, 15% to 20% are ectopic.8,9 The number of glands present may further complicate locating the adenoma. About 85% of individuals have four glands, 5% have five, and 10% have three glands identified.8,9 In some cases, patients have four normal glands in the neck as well as an abnormal fifth gland in the mediastinum.7–9 Approximately 9% of all patients with PHPT have parathyroid hyperplasia in which all four parathyroid glands are enlarged.10
Although 80% to 85% of parathyroid adenomas are found adjacent to the thyroid gland in its normal location, 15% to 20% are ectopic.8,9
IO-PTH assays have been used by many surgeons to detect decreases in plasma PTH levels after all hypersecreting tissue has been excised.11,12 We here describe our experience with a rapid intraoperative PTH immunochemiluminescent assay (ICMA) in patients undergoing exploration for parathyroid adenoma or multigland hyperplasia. The status of the IO-PTH assay has shifted from investigative to routine clinical tool;13 the test allows a more limited procedure by confirming complete removal of hypersecreting tissue.1 It also reduces the need for repeat surgeries5 and reduces the extent of neck exploration in patients with single-gland disease.
… the test allows a more limited procedure by confirming complete removal of hypersecreting tissue.1
Methods
The Kaiser Permanente Southern California Institutional Review Board approved this study. MIP using IO-PTH assays was performed for 32 patients at the Kaiser Permanente (KP) Fontana Medical Center, Fontana, California, between August 2003 and June 2006. Rapid IO-PTH assays were used primarily to determine whether all hyperfunctioning tissue had been removed.6 In one patient, the MIP was a repeat surgical exploration necessitated by a failed parathyroid surgery done at a non-KP medical center; one patient showed multigland hyperplasia and one exhibited secondary hyperparathyroidism.
We used the Immulite analyzer (Diagnostic Products Corporation, Los Angeles, CA), which employs a solidphase goat polyclonal anti-PTH and an alkaline phosphatase-labeled mobile-phase goat polyclonal anti-nPTH antibody. The standard PTH assay in the Immulite analyzer has a 60-minute incubation time, requires a serum sample, and has an analytic range of 5 to 5000 pg/mL.14 The testing method used in this study was a second-generation Immulite PTH assay: the Turbo Intact PTH assay, which shortens incubation time to 14 minutes and produces an analytic range of 10 to 2500 pg/mL. Our laboratory uses a rolling turbo cart with a StatSpin Express 2 primary tube centrifuge (StatSpin, Inc, Norwood, MA) and an uninterrupted power supply for point-of-surgery testing during MIP.14
To determine the assay's clinical utility, we performed univariate inferential testing for duration of surgery, duration of hospital stay, and surgery cost. We wanted to have at least a 95% likelihood of true decreases in these parameters. Our hypotheses were tested with a one-sample, one-tailed t-test.
Results
Figure 1 shows the percentage decrease in PTH levels for each of the 32 patients ten minutes after excision. Figure 2 shows the patients' t-test data.
Figure 1.
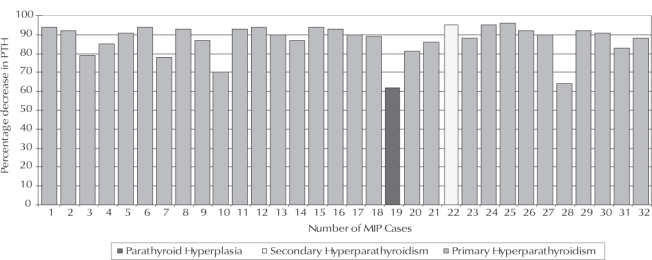
Percentage decrease in parathyroid hormone (PTH) levels for 32 patients who underwent minimally invasive parathyroidectomy (MIP).
Figure 2.
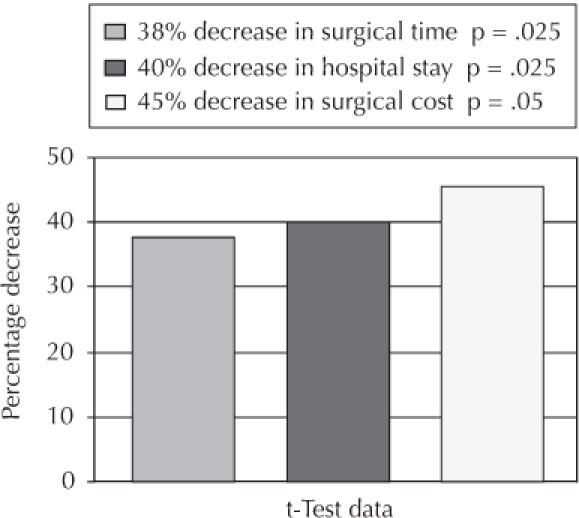
Data from t-test for 32 patients who underwent minimally invasive parathyroidectomy.
At our institution, historical mean duration of surgery needed to complete bilateral parathyroid explorations was 210 minutes. This mean reflected length of surgery per bilateral exploration done during the year before advent of MIP with IO-PTH assay.
Our mean time for MIP with IO-PTH assay was 119 minutes, a 43% decrease, with t = 2.111 (critical value for t.025,31 was 2.039). Thus, we estimate a 97.5% likelihood (p = .025) that the mean duration of surgery was decreased by 38% using MIP with IO-PTH assay, compared with the mean duration of surgery for bilateral exploration (Figure 2).
Mean length of hospital stay was also reduced by MIP, compared with the mean duration of hospital stay observed before advent of MIP with IO-PTH assay.3,15,16 Historically, the mean historical duration of hospital stay was 1.3 days.16,17 For patients undergoing MIP with IO-PTH assay at our institution, the mean duration was 0.65 days, a 54% decrease (t = 2.073 vs the critical t table value of 2.039). This yields an estimated 97.5% likelihood (p = .025) that, compared with hospital stay required after bilateral exploration, mean duration of hospital stay was decreased by 40% by using MIP (Figure 2).
Historically, the reported mean surgical cost of bilateral exploration in the US during our study period (August 2003 through June 2006) averaged $6865.16–18 This figure includes a surgical cost of $4135, as well as a 1.3-day hospital stay, costing $2730. The mean estimated cost for our 32 patients was $3194, 53.4% lower than the reported US average. The estimated t-test value for this comparison was 1.828 (vs 1.695 cited as the critical value in the t table, indicating a 95% likelihood [p = .05] that MIP reduced mean cost per surgery by 45%).
Collectively, the 32 patients had an 87% mean decrease in PTH level measured at ten minutes after excision. Calcium levels of all 32 patients remained normal at last postoperative follow-up examination, and none of the patients showed persistent or recurrent hyperparathyroidism at follow-up examination.
Discussion
Criteria for Predicting Cure
Chemical assays used for intraoperative determination of adequate resection rely on the specific, unique products produced by the parathyroid glands. Whereas standard PTH assays, with routine incubation times and temperatures, can require more than an hour, the rapid PTH assay generally has a higher incubation temperature, uses an agitation cycle, and has a shorter incubation time.19,20 First-generation PTH assays were radioimmunoassays, a methodology seldom used today because of lengthy turnaround time and poor diagnostic utility.12,21–23 Test methodology has greatly improved in the second- and third-generation assays, which include immunoradiometric assay (IRMA) and the more current ICMA method.
IRMAs and ICMAs use an excess of capture antibody specific for one end of the PTH molecule. The capture antibody is bound to a solid phase, commonly a bead. After blood specimen collection, serum or plasma is separated and an aliquot is added to the solid phase along with the capture antibody. The PTH in the specimen binds to the capture antibody during incubation. Next, the signal antibody is added because it recognizes an immunologic site (on the PTH molecule) distinct from the site recognized by the capture antibody. After unbound material is removed, the bound signal is measured. The signal output is directly proportional to the level of PTH present in the specimen.4,13
The IRMAs—considered-second generation assays—have disadvantages that are substantially overcome by ICMAs, the third-generation assays. The latter have a long shelf life (six months or longer), are technically easy to use, do not require radioactive safety precautions, and have high analytic accuracy. Portable ICMA automated formats are available so that monitoring can be done directly in the operating room. Carter and Howanitz14 calculated the cost of reagents for the Immulite turbo assay to be $100.00 per surgery. Our actual cost per surgery averaged $80.00.2
The IO-PTH concentration used to indicate a surgical cure relied on the half-life of the PTH molecule and on the postresection interval after which the specimen was drawn.
As our main criterion, we used a >50% drop in PTH measured at ten minutes after resection. When a patient's PTH level has decreased and been maintained at a level 50% below the baseline value (determined at commencement of surgery), the surgeon can be confident that production of PTH has ceased as a result of complete excision of all hypersecreting tissue.24 We routinely drew four samples for PTH assay: the preincision baseline sample, the postincision–preexcision (second) baseline sample, the sample drawn five minutes after excision, and the sample drawn ten minutes after excision. The second baseline sample was drawn to determine stability of the original baseline. The higher of the two baseline values was used as our working PTH baseline, from which we calculated the required ≥50% decrease in PTH level.24
… none of the patients showed persistent or recurrent hyperparathyroidism at follow-up examination.
Comparison with the Literature
Many studies have now demonstrated the clinical utility of IO-PTH testing,6 which has proven highly effective for predicting the success of MIP done for primary hyperparathyroidism. All of our 32 patients had successful surgery, and there were statistically significant decreases in duration of surgery, duration of hospital stay, and surgery cost. Of course, continued follow-up is needed.25
Udelsman's review of 656 cases15 showed that among patients having conventional bilateral explorations without IO-PTH assays, nearly 18% required repeat surgery. Thus, by extrapolation we might have expected a need to reoperate in about six of our 32 patients. Experienced surgeons can appreciate the promise this technique offers for eliminating the risk of missing hypersecreting tissue.
Future investigations for IO-PTH assays might include evaluating their role in guiding surgeons performing parathyroid surgery in patients with secondary hyperparathyroidism, surgeons performing bilateral exploration in patients with ectopic second adenomas, and surgeons performing parathyroid tissue autotransplant when surgical hypoparathyroidism might be a risk.
All of our 32 patients had successful surgery, and there were statistically significant decreases in duration of surgery, duration of hospital stay, and surgery cost.
Acknowledgments
Katharine O'Moore-Klopf of KOK Edit provided editorial assistance.
References
- Bilezikian JP, Silverberg SJ. Clinical spectrum of primary hyperparathyroidism. Rev Endocr Metab Disord. 2000 Nov;1(4):237–45. doi: 10.1023/a:1026508829397. [DOI] [PubMed] [Google Scholar]
- Thompson GB, Grant CS, Perrier ND, et al. Reoperative parathyroid surgery in the era of sestamibi scanning and intraoperative parathyroid hormone monitoring. Arch Surg. 1999 Jul;134(7):699–704. doi: 10.1001/archsurg.134.7.699. discussion 704–5. [DOI] [PubMed] [Google Scholar]
- Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery. 1999 Dec;126(6):1016–21. doi: 10.1067/msy.2099.101433. discussion 1021–2. [DOI] [PubMed] [Google Scholar]
- Wians FH. Intraoperative parathyroid hormone testing: a revolution in point-of-surgery testing on the horizon? Am Clin Lab. 2000 Jul;19(6):21–2. [Google Scholar]
- Udelsman R. Is unilateral neck exploration for parathyroid adenoma appropriate? Adv Surg. 2000;34:319–29. [PubMed] [Google Scholar]
- Garner SC, Leight GS., Jr. Initial experience with intraoperative PTH determinations in the surgical management of 130 consecutive cases of primary hyperparathyroidism. Surgery. 1999 Dec;126(6):1132–7. doi: 10.1067/msy.2099.101429. discussion 1137–8. [DOI] [PubMed] [Google Scholar]
- Gulec SA, Omer U. The intellectual and scientific basis of parathyroid surgery. Turkish Journal of Medical Sciences [serial on the Internet] 2004;34(2):81–4. [cited 2005 Sep 6] Available from: http://mistug.tetm.tubitak.gov.tr/~bdyim/toc.php3?dergi=sag&yilsayi=2004/2. [Google Scholar]
- Wang C. The anatomic basis of parathyroid surgery. Ann Surg. 1976 Mar;183(3):271–5. doi: 10.1097/00000658-197603000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson NW, Eckhauser FE, Harness JK. The anatomy of primary hyperparathyroidism. Surgery. 1982 Nov;92(5):814–21. [PubMed] [Google Scholar]
- Denham DW, Norman J. Cost-effectiveness of preoperative sestamibi scan for primary hyperparathyroidism is dependent solely on the surgeon's choice of operative technique. J Am Coll Surg. 1998 Mar;186(3):293–305. doi: 10.1016/s1072-7515(98)00016-7. [DOI] [PubMed] [Google Scholar]
- Kao PC, Van Heerden JA, Taylor RL. Intraoperative monitoring of parathyroid procedures by a 15-minute parathyroid hormone immunochemiluminometric assay. Mayo Clinic Proc. 1994 Jun;69(6):532–7. doi: 10.1016/s0025-6196(12)62243-5. [DOI] [PubMed] [Google Scholar]
- John MR, Goodman WG, Gao P, Cantor TL, Salusky IB, Juppner H. A novel immunoradiometric assay detects full-length human PTH but not amino-terminally truncated fragments: implications for PTH measurement in renal failure. J Clin Endocrinol Metab. 1999 Nov;84(11):4287–90. doi: 10.1210/jcem.84.11.6236. [DOI] [PubMed] [Google Scholar]
- Chen H, Zeiger MA, Gordon TA, Udelsman R. Parathyroidectomy in Maryland: effects of an endocrine center. Surgery. 1996 Dec;120(6):948–52. doi: 10.1016/s0039-6060(96)80039-0. discussion 952–3. [DOI] [PubMed] [Google Scholar]
- Carter AB, Howanitz PJ. Intraoperative testing for parathyroid hormone a comprehensive review of the use of the assay and the relevant literature. Arch Pathol Lab Med. 2003 Nov;127(11):1424–42. doi: 10.5858/2003-127-1424-ITFPHA. [DOI] [PubMed] [Google Scholar]
- Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002 May;235(5):665–70. doi: 10.1097/00000658-200205000-00008. discussion 670–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solucient, L.L.C. Length of stay by operation, Western region. Baltimore (MD): Solucient, L.L.C.; 2004. [Google Scholar]
- Yeh T. Combined status and trends report. Kaiser Permanente Medical Care Program—California Division, Southern California Region, Fontana Medical Center. Nov 2003–Nov 2004. [monograph on the Intranet]. [cited 2006 Jan 19]. Available from: http://kpnet.kp.org/california/finance/fin_south/reports/nov/Combined_StatusTrends_1003.xls.
- Kaiser Permanente. Non member fee schedule for Kaiser Permanente—NCR. April 15, 2004.
- Madira W, Robertson GS, London NJ, Iqbal SJ, Bell PR, Veitch PS. Comparison of “intraoperative” parathormone measurement with frozen section during parathyroid surgery. Ann R Coll Surg Engl. 1993 Jan;75(1):26–9. [PMC free article] [PubMed] [Google Scholar]
- Dackiw AP, Sussman JJ, Fritsche HA, Jr, et al. Relative contributions of technetium Tc99m sestamibi scintigraphy, intraoperative gamma probe detection, and the rapid parathyroid hormone assay to the surgical management of hyperparathyroidism. Arch Surg. 2000 May;135(5):550–5. doi: 10.1001/archsurg.135.5.550. discussion 555–7. [DOI] [PubMed] [Google Scholar]
- Brown RC, Aston JP, Weeks I, Woodhead JS. Circulating intact parathyroid hormone measured by a two-site immunochemiluminometric assay. J Clin Endocrinol Metab. 1987 Sep;65(3):407–14. doi: 10.1210/jcem-65-3-407. [DOI] [PubMed] [Google Scholar]
- Mallette LE, Coscia AM. Rapid radioimmunoassay for parathyroid hormone: its use in hypercalcemic crisis. South Med J. 1984 Mar;77(3):323–6. doi: 10.1097/00007611-198403000-00014. [DOI] [PubMed] [Google Scholar]
- Hsu FS, Clark OH, Serata TY, Nissenson RA. Rapid localization of parathyroid tumors by selective venous catheterization and parathyroid hormone bioassay. Surgery. 1983 Dec;94(6):873–6. [PubMed] [Google Scholar]
- Sokoll LJ, Wians FH, Jr, Remaley AT. Rapid intraoperative immunoassay of parathyroid hormone and other hormones: a new paradigm for point-of-care testing. Clin Chem. 2004 Jul;50(7):1126–35. doi: 10.1373/clinchem.2003.030817. Epub 2004 Apr 29. [DOI] [PubMed] [Google Scholar]
- Nordenstrom E, Westerdahl J, Bergenfelz A. Long-term follow-up of patients with elevated PTH levels following successful exploration for primary hyperparathyroidism. World J Surg. 2004 Jun;28(6):570–5. doi: 10.1007/s00268-004-7124-y. [DOI] [PubMed] [Google Scholar]


