Abstract
Chronic Granulomatous Disease (CGD) and inflammatory bowel disease (IBD) have overlapping gastrointestinal manifestations. Serum antibodies to intestinal microbial antigens in IBD are thought to reflect a loss of tolerance in the setting of genetically encoded innate immune defects. CGD subjects studied here, with or without colitis, had considerably higher levels of ASCA IgA, ASCA IgG, anti-OmpC, anti-I2, and anti-CBir1, but absent to low pANCA, compared to IBD-predictive cutoffs. Higher antibody levels were not associated with a history of colitis. Except for higher ASCA IgG in subjects <18 years, antibody levels were not age-dependent. In comparison, 7 HIES subjects expressed negative to low antibody levels to all of these antigens; none had colitis. Our results suggest that markedly elevated levels of antimicrobial antibodies in CGD do not correlate with a history of colitis but may reflect a specific defect in innate immunity in the face of chronic antigenic stimulation.
Keywords: Chronic Granulomatous Disease, Hyper IgE Syndrome, Inflammatory Bowel Disease, serum antimicrobial antibodies, colitis, innate immunity
Introduction
Chronic granulomatous disease (CGD) is a primary immunodeficiency disorder related to defective microbial killing. CGD neutrophils have defective nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activity which results in an absent or decreased superoxide respiratory burst and the subsequent failure to clear bacterial and fungal infections[1]. Two-thirds of CGD patients have the X-linked form due to mutations in the gp91phox subunit of the NADPH oxidase complex[2; 3]; other mutations in the p47phox, p67phox, p22phox, and p40phox subunits account for the remainder of CGD patients who have autosomal recessive forms[3; 4; 5].
Patients with CGD are susceptible to frequent bacterial and fungal colonization and severe, invasive infections especially of the pulmonary and gastrointestinal (GI) tracts[1; 6]. Common causal organisms include Staphylococcus aureus, Burkholderia and Aspergillus species. In particular, it has been reported that a number of these patients have increased levels of IgG antibodies to Aspergillus species which are thought to correlate with the continual exposure via the high rate of apparent and inapparent Aspergillus infections[7].
In addition to serious infections and abnormal granuloma formation[8], CGD subjects may have concomitant autoimmune complications[9] and inflammation, particularly in the GI tract[10; 11; 12; 13; 14; 15; 16]. About half of CGD patients have been reported to have GI complications, occurring more frequently in conjunction with the X-linked form of the disease[15]. CGD subjects with colitis often present with signs and symptoms similar to those seen in Crohn’s disease (CD) and ulcerative colitis, the classical inflammatory bowel diseases (IBD). Subjects with either disease may suffer from abdominal pain, diarrhea, malabsorption, failure to thrive, and, in some cases, intestinal fistulae[1; 17]. However, in contrast to IBD, CGD-associated colitis may have distinctive histopathologic findings including more eosinophils, fewer neutrophils, and numerous lipid-laden macrophages[13; 14; 18]. These differences in histology and disease background have suggested alternate pathogenetic mechanisms for the GI inflammation in CGD[19].
Genome wide scans in large CD cohorts have identified several genes associated with the regulation of innate immune responses. Many of these (e.g. NOD2/CARD15, ATG16L1)[20; 21] are involved in pathways directing intracellular killing of invading microorganisms. Thus the presence of antimicrobial antibodies in this patient population may reflect defects in innate immunity rather than enhanced exposure. Antibodies to Saccharomyces cerevisiae (ASCA IgG and IgA), outer membrane porin of E. Coli (OmpC IgG), Pseudomonas fluorescens (anti-I2), flagellin (anti-CBir1), perinuclear antineutrophil antibody (pANCA)[22], and, most recently, anti-glycan antibodies which include anti-chitobioside IgA (ACCA), anti-laminaribioside IgG (ALCA), and anti-mannobioside IgG (AMCA)[23], in the sera of IBD patients have been proposed as biomarkers for IBD[24]. The prevailing theory for the production of these antibodies is that a selective loss of tolerance to microbial antigens results in local inflammation and disruption of the mucosal barrier. In turn, exposure to several microbial antigens ultimately leads to an exaggerated antibody response to these antigens in a genetically susceptible host [22; 25; 26; 27; 28]. This antibody panel is utilized commercially as a clinical screening tool for the diagnosis and management of IBD and as biomarkers distinguishing ulcerative colitis from CD. As colitis is common in CGD, the aim of this study was to assess the prevalence and level of antibodies indicating microbial sensitization in CGD in subjects with or without colitis.
We demonstrate here that nearly all CGD subjects, regardless of the presence or absence of GI tract inflammation, possessed high levels of serum antibodies to several antigens present on GI-tract associated microbes. The presence of these antibodies was not specific to a CGD genotype or gastrointestinal phenotype. We also examined the levels of these antibodies in Hyper IgE Syndrome (HIES) patients, who experience some overlapping chronic microbial infections and have an innate immune defect but rarely develop colitis or granulomas.
Methods
Sample Collection
Serum from previously banked samples or freshly drawn peripheral blood was obtained with written informed consent from CGD patients, with or without a known history of colitis, their family members if available, and HIES patients at the primary immunodeficiency clinic at the Mount Sinai Medical Center, New York, NY and at the National Institute of Allergy and Infectious Disease, NIH, Bethesda, MD. All CGD subjects had been diagnosed by impaired neutrophil oxidative burst[29], and some patients also had undergone genetic sequencing to determine specific mutations in the NADPH oxidase subunits. The presence or absence of colitis was assessed by clinical symptoms and, in some cases, confirmed by endoscopy, radiologic studies, colonoscopy and/or biopsy. Serum samples were drawn prior to bone marrow transplantation in 3 CGD subjects and prior to gene therapy in 1 CGD subject. These studies were approved by the Institutional Review Boards at Mount Sinai and the NIAID.
Pathology
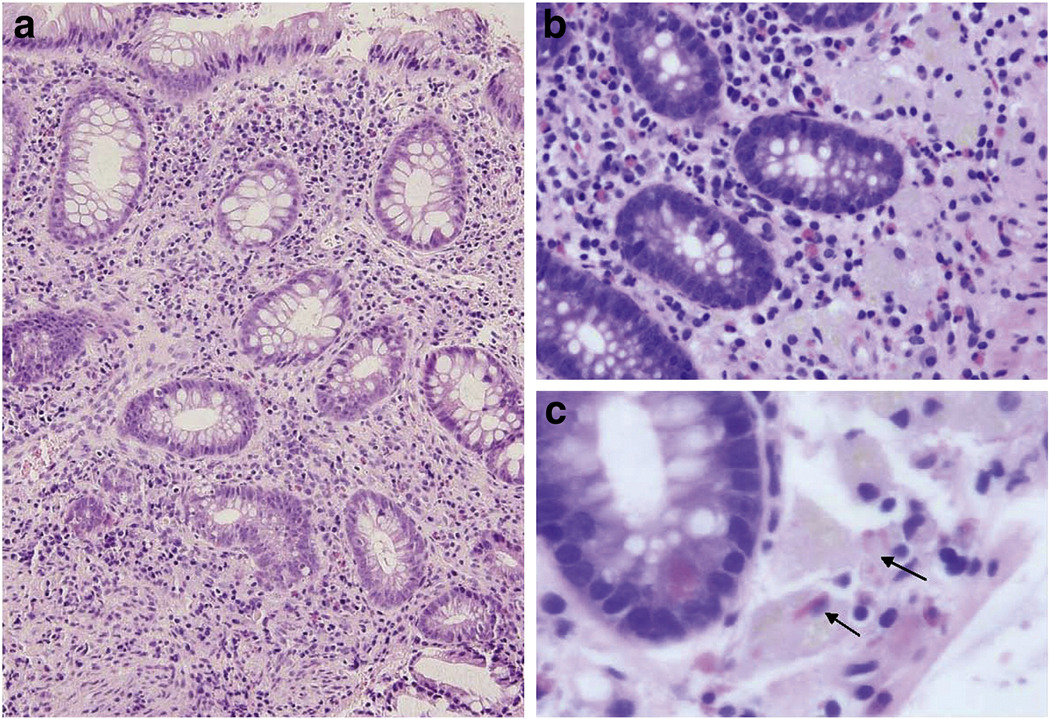
Biopsy findings on colonoscopy, if performed, were consistent with pathological features characteristic of CGD colitis, including a lack of neutrophils, increased eosinophils, eosinophilic cryptitis, and prominent pigment-laden histiocytes with cytoplasmic crystalline inclusions[14; 19] (Figure 1a–c).
Figure 1. Representative colonic biopsy from a CGD patient with colitis.
Section of colonic mucosa from a CGD patient with colitis demonstrating (a) architectural distortion, full-thickness lymphoplasmacytosis, and Paneth cell metaplasia (200×, H&E), (b) clusters of histiocytes with brown pigment in the lamina propria, paucity of neutrophils, and scattered eosinophils (400×, H&E), and (c) pink crystalline inclusions in pigmented histiocytes (arrows) (600×, H&E).
Serologic Testing
Serum antibody levels for ASCA IgG and IgA, OmpC IgG, anti- I2 IgG, anti-CBir1, and pANCA were determined for each subject by ELISA in a blinded fashion at the Cedars-Sinai Medical Center as previously described[25]. Antibody levels were expressed as ELISA units (EU/ml) and compared to the Cedars Sinai laboratory standards that were established based on analyses of immune reactivity in sera from subjects ages 18 years and older with and without well-characterized IBD[25; 30; 31; 32; 33; 34]. Antibody levels above the cutoff value predictive for proven IBD were considered positive.
Statistical Analysis
Wilcoxon signed rank test was used to compare median levels of each antibody with the positive cutoff values. Comparison of group differences in median antibody levels was evaluated by the non-parametric Mann-Whitney test. Statistical analyses were performed using GraphPad Prism 4.0 (La Jolla, CA). A p value < 0.05 was considered significant.
Results
Patients and GI disease
We obtained sera from a sample cohort of 59 CGD patients and 1 unaffected female relative of a CGD patient, representing CGD patients with and without colitis. The median age at testing was 20 years (range 3 to 62) with 47 males and 12 females (Table 1). Of the 40 CGD subjects with the gp91phox X-linked phenotype (66.7%), only 2 subjects expressed detectable gp91 protein; one additional female subject had ~5–12% Lyonization of her peripheral blood cells. The remaining 18 CGD subjects had either an autosomal recessive mutation in p47phox (28.8%) or p22 phox (1.7%). Of the subjects with X-linked CGD, 39.0% had a clinical history of colitis, the majority of which (93.8%) were confirmed by endoscopy and biopsy. Approximately one-third (33.3%) of the subjects with autosomal recessive CGD also had biopsy-confirmed colitis. Although the group contained 8 groups of siblings and one pair of cousins, not every relative with CGD was similarly affected by GI disease. Three CGD subjects died from complications due to infection, underlying disease, or medical treatment.
Table 1.
Clinical Features of CGD Subjects.
| Subject Number |
Age at Testing (Yr) |
Sex | Mutation | History of Colitis |
Other Clinical History |
|---|---|---|---|---|---|
| 1 | 3 | M | 91 | Yes | |
| 2 | 3 | M | 91 | ||
| 3 | 5 | M | 91 | ||
| 4 | 5 | M | 91 | ||
| 5 | 7 | M | 91 | Yes | sibling of #6, post-MUD HSCT |
| 6 | 8 | M | 91 | Yes | sibling of #5, post-MUD HSCT |
| 7 | 9 | M | 91 | died of fulminant T. inkin infection | |
| 8 | 9 | M | 91 | ||
| 9 | 10 | M | 91 | Yes | sibling of #10, rectal abscesses* |
| 10 | 14 | M | 91 | sibling of #10, rectal abscesses* | |
| 11 | 17 | M | 91 | Yes | cousin of #31 |
| 12 | 17 | M | 91 | ||
| 13 | 18 | M | 91 | Yes | |
| 14 | 19 | M | 91 | ||
| 15 | 19 | M | 91 | ||
| 16 | 20 | M | 91 | Yes | |
| 17 | 20 | M | 91 | Yes | sibling of #26 |
| 18 | 20 | M | 91 | Yes | disseminated CMV, received infliximab for colitis, died of colitis complications |
| 19 | 20 | M | 91 | Yes | |
| 20 | 21 | M | 91 | Yes | |
| 21 | 21 | M | 91 | ||
| 22 | 22 | M | 91 | Yes | |
| 23 | 22 | M | 91 | Yes | sibling of #27 |
| 24 | 22 | M | 91 | ||
| 25 | 24 | M | 91 | ||
| 26 | 24 | M | 91 | sibling of #17 | |
| 27 | 25 | M | 91 | Yes | sibling of #23 |
| 28 | 25 | M | 91 | ||
| 29 | 25 | M | 91 | ||
| 30 | 25 | F | 91 | Lyonized carrier (5–12% mutation-positive cells), discoid lupus | |
| 31 | 26 | M | 91 | cousin of #11 | |
| 32 | 28 | M | 91 | ||
| 33 | 29 | M | 91 | sibling of #35 | |
| 34 | 32 | M | 91 | received gene therapy | |
| 35 | 33 | M | 91 | sibling of #33* | |
| 36 | 34 | M | 91 | sibling of #38 | |
| 37 | 35 | M | 91 | died of renal failure and other transplant complications post-BMT | |
| 38 | 38 | M | 91 | sibling of #36 | |
| 39 | 39 | M | 91 | Yes | |
| 40 | 42 | M | 91 | Yes | gp91protein + |
| 41 | 50 | M | 91 | several granulomas in esophagus and genitourinary tract, Hepatitis C+, gp91 protein +/− | |
| 42 | 62 | F | gp91 carrier | ||
| 43 | 6 | M | 47 | Candida esophagitis | |
| 44 | 15 | F | 47 | Yes | |
| 45 | 16 | F | 47 | ||
| 46 | 17 | F | 47 | Yes | received infliximab treatment |
| 47 | 17 | F | 47 | ||
| 48 | 17 | F | 47 | sibling of #50 and #51 | |
| 49 | 18 | F | 47 | Yes | |
| 50 | 18 | M | 47 | Yes | sibling of #48 and #51 |
| 51 | 20 | M | 47 | sibling of #48 and #50 | |
| 52 | 21 | M | 47 | ||
| 53 | 30 | F | 47 | sibling of #55 | |
| 54 | 33 | F | 47 | Yes | |
| 55 | 33 | M | 47 | sibling of #53 | |
| 56 | 38 | F | 47 | Yes | |
| 57 | 40 | M | 47 | ||
| 58 | 40 | F | 47 | ||
| 59 | 43 | M | 47 | ||
| 60 | 35 | F | 22 | * |
MUD HSCT, matched unrelated hematopoietic stem cell transplant; CMV, cytomegalovirus; BMT, bone marrow transplant
testing performed at two different time points
Antibody production to microbial antigens
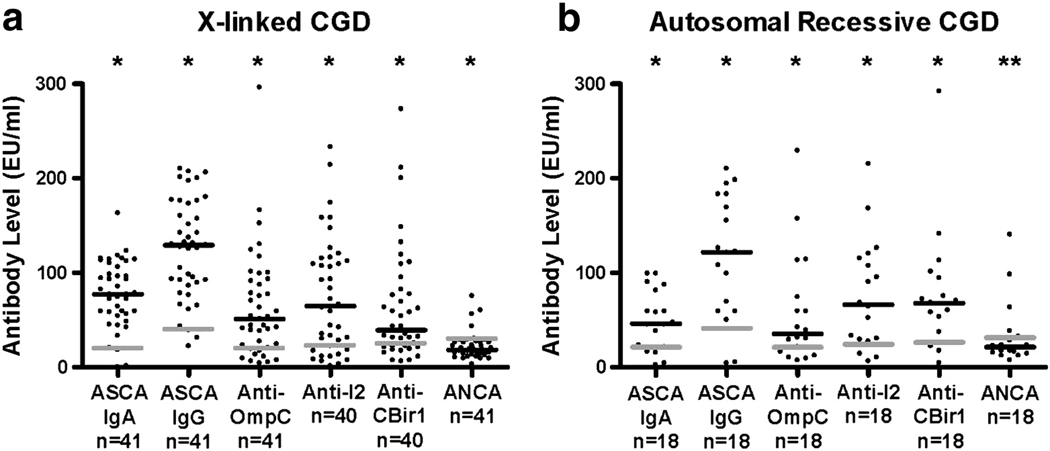
Nearly all CGD subjects (96.6%) expressed positive antibody levels above the established cutoff values used for the diagnosis of IBD to one or more microbial antigens. Irrespective of the genotype, the median antibody levels for ASCA IgA (72 EU/ml), ASCA IgG (126 EU/ml), anti-OmpC (44 EU/ml), anti-I2 (65 EU/ml), and anti-CBir1 (58 EU/ml) in the CGD subjects (Figure 2a and 2b) were markedly greater than the predictive cutoff values for IBD[25]. There was no significant difference in the median values of these antibodies between subjects who had colitis and those who did not, in either the X-linked or autosomal recessive CGD groups with the exception of a higher ASCA IgA in the autosomal recessive CGD group with colitis (Table 2a and 2b). The antibody levels were generally similar in both the X-linked and autosomal recessive CGD subjects. Few autosomal recessive CGD subjects had marginally higher levels of certain antibodies than the X-linked subjects but the differences were not significant (data not shown). The pANCA levels (median 19 EU/ml), on the other hand, were in the negative to low positive range in the majority of CGD subjects (81.7%) when compared to the IBD-predictive cutoff level. The CGD carrier subject had positive OmpC, I2, and pANCA antibody levels, but these were much lower than the affected subjects.
Figure 2. Serum antibody levels in X-linked (a) or autosomal recessive (b) CGD subjects.
Antimicrobial antibodies in serum samples were measured by ELISA. Median antibody titers are represented by the black lines. Antibody cutoff levels predictive for possible IBD are represented by the grey lines. *p<0.05, **p=0.2353
Table 2.
| a. Comparison of Antibody Levels in X-linked CGD Subjects With or Without Colitis. | |||
|---|---|---|---|
| Antibody (EU/ml)a | No colitisb (n=25) |
Colitisb (n=16) |
p value |
| ASCA IgA (20) | 77.0 (0.0–163.0) | 79.5 (20.0–123.0) | 0.6689 |
| ASCA IgG (40) | 127.0 (22.0–207.0) | 136.5 (65.0–210.0) | 0.3428 |
| Anti-OmpC (20) | 54.0 (4.0–152.0) | 40.5 (5.0–296.0) | 0.5746 |
| Anti-I2 (23) | 92.0 (1.0–233.0) | 42.0 (6.0–214.0) | 0.5859 |
| Anti-CBir1 (25) | 43.0 (6.0–273.0) | 32.0 (7.0–211.0) | 0.9777 |
| pANCA (30) | 17.0 (9.0–75.0) | 19.5 (3.0–43.0) | 0.7687 |
| 2b. Comparison of Antibody Levels in Autosomal Recessive CGD Subjects With or Without Colitis. | |||
|---|---|---|---|
| Antibody (EU/ml)a | No colitisb (n=12) |
Colitisb (n=6) |
p value |
| ASCA IgA (20) | 30.5 (2.0–99.0) | 73.0 (47.0–99.0) | 0.0217 |
| ASCA IgG (40) | 84.0 (4.0–198.0) | 140.5 (121.0–210.0) | 0.1466 |
| Anti-OmpC (20) | 30.5 (7.0–229.0) | 50.5 (12–157.0) | 0.3489 |
| Anti-I2 (23) | 71.0 (6.0–168.0) | 66.0 (14.0–215.0) | 0.7431 |
| Anti-CBir1 (25) | 63.5 (4.0–292.0) | 69.0 (37.0–75.0) | 0.9254 |
| pANCA (30) | 16.5 (7.0–63.0) | 30.5 (22.0–140.0) | 0.017 |
Positive cutoff reference value predictive for IBD
Median (range)
To account for possible differences in age-related antibody expression, the antibody levels of the CGD subjects were analyzed according to two age groups, <18 years (n=19) and ≥18 years (n= 40). Group assignments were based on the ages of the subjects used to establish the IBD cutoff levels. Although the median antibody levels in the 0–18 years were generally lower than the >18 years group (Table 3), most of the differences were not statistically significant. In four of the CGD subjects who were tested at two different time points, no differences in antibody levels were noted (subjects marked with * in Table 1).
Table 3.
Antibody Levels by Age Group.
| Antibody (EU/ml)a | < 18 Yearsb (n=19) |
≥ 18 Yearsb (n=40) |
p value |
|---|---|---|---|
| ASCA IgA (20) | 59.0 (0.0–163.0) | 72.0 (4.0–115.0) | 0.5868 |
| ASCA IgG (40) | 93.0 (5.0–210.0) | 134.5 (4.0–210.0) | 0.0222 |
| Anti-OmpC (20) | 41.0 (4.0–229.0) | 52.0 (6.0–296.0) | 0.3723 |
| Anti-I2 (23) | 30.5 (1.0–214.0) | 90.0 (6.0–233.0) | 0.0785 |
| Anti-CBir1 (25) | 58.0 (6.0–292.0) | 60.0 (4.0–273.0) | 0.9802 |
| pANCA (30) | 20.0 (9.0–140.0) | 18.5 (3.0–75.0) | 0.9483 |
Positive cutoff reference value predictive for IBD
Median (range)
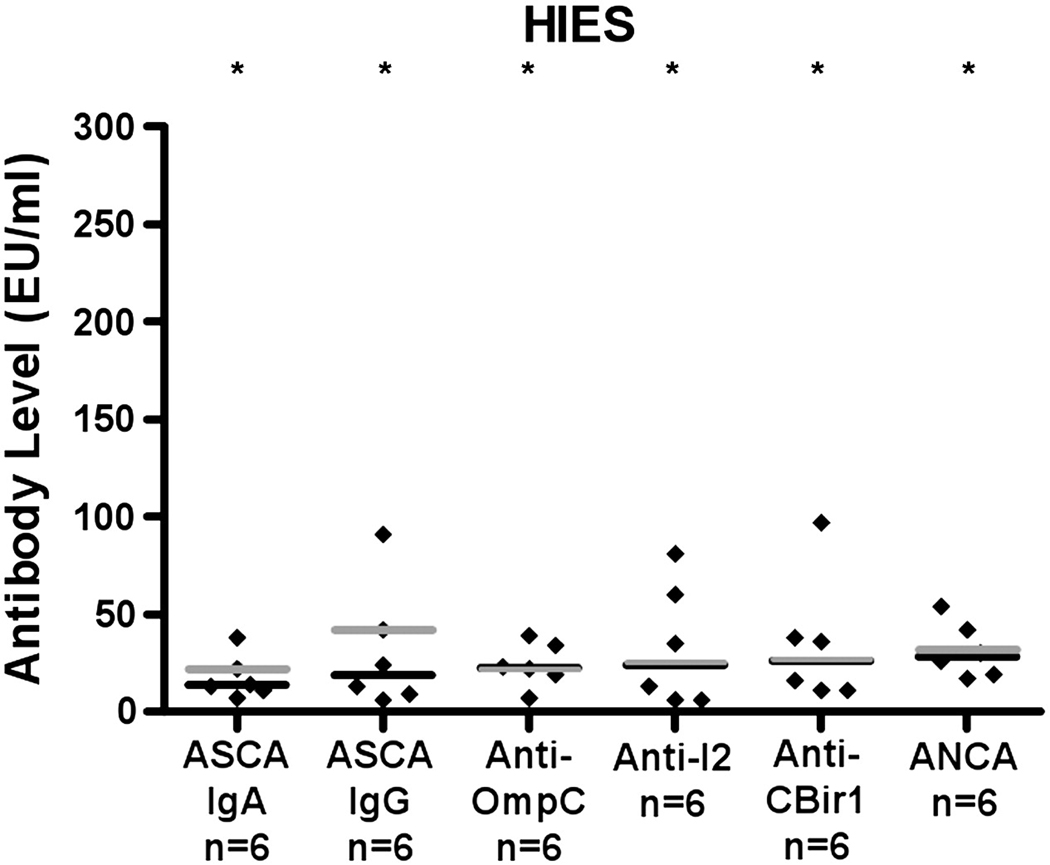
To determine whether elevated antimicrobial antibody levels were generic to defects in innate immunity, we also analyzed subjects with a clinical diagnosis of HIES for comparison. Although many of the HIES subjects (n=6), median age 25 years (range 11–45), had extensive histories of infections (Table 4), none of the HIES subjects had a clinical history of colitis. All the HIES subjects produced antibody to one or more of the antigens tested. However, unlike the CGD subjects, the median antibody levels were either negative or slightly positive in comparison to the positive predictive cutoffs (Figure 3).
Table 4.
Clinical Features of HIES Subjects.
| Subject Number |
Age at Testing (Yr) |
Sex | History of Colitis |
Other Clinical History |
|---|---|---|---|---|
| 1 | 11 | F | No | Candidal infections, neonatal rash, delayed dentition, atopic dermatitis, Hemophilus buttock abscess |
| 2 | 19 | F | No | Oral candidiasis, chronic diarrhea, cholecystectomy, pneumatoceles, recurrent pneumonias |
| 3 | 25 | M | No | Brain abscesses, craniosynostosis, lung abscesses, died of HIV |
| 4 | 25 | M | No | Aspergillus and staphylococcal infections, severe atopic dermatitis, end-stage lung disease, died of pulmonary hemorrhage |
| 5 | 41 | F | No | Candidal esophagitis, chronic mucocutaneous candidiasis, pneumococcal and staphylococcal pneumonia, Klebsiella lung abscess, died of pneumonia |
| 6 | 45 | M | No | Aspergillus infections, pulmonary hemorrhage, pneumatoceles |
Figure 3. Serum antibody levels in HIES subjects.
Antimicrobial antibodies in serum samples were measured by ELISA. Median antibody titers are represented by the black lines. Antibody cutoff levels predictive for possible IBD are represented by the grey lines. *p=NS
Discussion
IBD-like colitis has been described in several diseases of defective innate immunity including CGD, leukocyte adhesion deficiency, glycogen storage disease type 1b, Hermansky-Pudlak syndrome[10; 19; 35; 36; 37; 38; 39] and X-linked ectodermal dysplasia with immunodeficiency (EDID)[40; 41; 42] as well as in more complex heterogeneous immune defects such as common variable immunodeficiency (CVID)[43; 44]. Current hypotheses for the complex pathogenesis of GI inflammation include chronic infections, disruption of the normal mucosal immunologic barrier, and/or immune dysregulation. Neutrophil dysfunction has been implicated in the development of colitis[8; 38; 45; 46] because of likely impaired bacterial clearance and control of GI commensal microflora leading to bacterial overgrowth and subsequent antigen sensitization. Inappropriate degradation of pro-inflammatory cytokines within the macrophages of subjects with CD has also been correlated with reduced bacterial elimination[47].
Similar to IBD, macrophages stimulated with bacterial antigens in CGD secrete abnormally low levels of certain pro-inflammatory cytokines[48], which may be associated with ineffective clearance of specific microbial flora in the gut. Chronic exposure to a high bacterial load in the gut could possibly result in a heightened adaptive immune response to certain bacterial antigens, such as those seen with generalized hyperimmunization, despite potential differences in the integrity of the mucosal barrier. A similar phenomenon of hypersensitization to aspergillus antigens has been previously described in CGD and HIES patients who have had a history of severe aspergillus infection or allergic bronchopulmonary aspergillosis (ABPA)[7]. In IBD subjects, multiple antibodies to an increasing number of microbial antigens and higher antibody levels have been correlated to more small bowel complications[49], suggesting that amplified antibody responses to bacterial exposure may contribute to mucosal dysfunction. Similarly, mice with deficient Toll-like receptor (TLR) signaling or impaired phagocyte oxidative burst have impaired intestinal clearance of bacteria associated with higher levels of serum IgG specific for GI microbial flora than do control animals[50].
We found a high prevalence of serum antibodies for OmpC, CBir1Fla, ASCA, and I2 in CGD subjects. Although local inflammation and disruption of the GI mucosa would be expected to result in similar patterns of antibody sensitization in IBD and CGD, the antibody levels in this group of CGD subjects were significantly higher than those typically observed in patients with IBD[25]. The majority of CGD patients in this study, regardless of the presence or absence of colitis or underlying CGD genotype had high antibody levels suggesting that antibody production does not predict symptomatic colitis in CGD. In contrast, elevated pANCA, a marker that has been proposed to discriminate ulcerative colitis from CD, was only noted in three autosomal recessive CGD subjects possibly reflecting a higher extent of mucosal inflammation and thus increased bacterial sensitization. Otherwise, pANCA was not seen in nearly all the CGD patients, indicating that antibody production in the intestine is selective.
Defects in innate receptors, such as TLRs, NOD-like receptors (NLRs), and NOD receptors, have been proposed to contribute to the pathogenesis in IBD[28; 51; 52] and have been linked to the presence of particular antibodies. In healthy controls and unaffected relatives of CD patients, carriers for NOD2 variants had higher antibody levels than non-carriers[53]. Elevated anti-CBir1 and ASCA in association with specific NF-κB haplotypes in CD[54] and higher anti-OmpC in unaffected family members of CD patients, but not of ulcerative colitis[55], strongly indicate that the pattern of antibody expression is linked to distinct heritable genotypes associated with innate immune deficiency. Mutations in many of these innate immune receptors have not been identified in CGD, but the strongly positive antibody repertoire observed in our CGD subjects may reflect the primary genetic abnormality of CGD affecting the macrophages[48] or other components of innate immunity. While increasing absolute antibody level and cumulative antibody response have been correlated to more severe and/or complicated GI disease in CD, a similar analysis of antibody patterns in CGD subjects, who express very high levels of all the antibodies regardless of colitis, would likely not be prognostic or diagnostic for GI disease activity.
Although the median antibody levels were exceptionally high amongst CGD subjects, we found wide variability. CGD patients likely have variable degrees of subclinical GI inflammation resulting in subtle damage to the GI mucosa sufficient to permit abnormal mucosal permeability which allows antigen sensitization without clinical symptoms. Since only symptomatic CGD patients were biopsied, it is possible that microscopic examination of the intestinal mucosa in all subjects would show low grade inflammation and permeability. It is also possible that the specific antibody pattern in CGD may reflect a distinct ecology and concentration in the CGD intestinal tract as opposed to classical IBD subjects.
The autosomal dominant form of HIES has innate defects due to mutations in STAT3[56]. Like CGD, subjects with HIES have recurrent bacterial infections and increased sensitization to other mucosal antigens[7]. They typically present with cold staphylococcal abscesses, pneumatoceles, and elevated total IgE but infrequently with GI disease. The HIES subjects studied here had no known inflammatory GI disease and either no or low antibody levels to the GI antigens we examined. While chronic bacterial antigen stimulation might also occur in HIES, the lack of sensitization to gastrointestinal antigens could be a result of a different spectrum of resident microbes in this immune defect or a manifestation of the STAT3-mediated block in IL-21 signaling leading to blunted antibody production in HIES[57].
Age-dependent serum levels of these antibodies could also have influenced our analyses. Several prior studies compared antibody levels in children with the commonly utilized standards derived from patients ages 18 years and older[58; 59; 60; 61]. However, recent studies have reported that children with IBD tend to have lower antibody levels than adults with IBD[62; 63]. Therefore, the diagnostic value of these serum antibodies in the pediatric population is less apparent. According to these studies, most children with IBD would fall into the negative IBD-predictive category. To account for the possible evolution of the immune response with age, we assigned the subjects to groups according to age-matched limits. Although the older subjects tended to have higher antibody levels than the younger ones, the differences were not statistically significant, with the exception of ASCA IgG. Although we observed higher antibody levels in the older CGD subjects, this does not explain why some CGD patients develop colitis and others do not.
These antibodies did not correlate with overt colitis in CGD subjects. Therefore, the use of these serological tests in CGD patients has no predictive clinical value and may obscure the diagnosis of CGD if an IBD diagnosis is applied first. Therefore, application of these screening serological tests to detect IBD should be carefully done.
In conclusion, high levels of serum antimicrobial antibodies in CGD are common and not specifically associated with symptomatic inflammatory bowel disease. The presence of such antibodies in CD may likewise be associated with underlying defects in innate immunity. Factors such as excess exposure to microbial antigens, breakdown of mucosal immunity, hyperimmunization due to dysregulated adaptive immunity may further contribute to this exuberant adaptive response to microbial antigens. These serum antibody tests will not be universally helpful in predicting GI inflammation, but the presence of these antibodies may indicate underlying innate immune deficiency.
Acknowledgments
Declaration of All Sources of Funding:
Supported by the National Institutes of Health AI-101093, AI-467320, AI-48693 and National Institute of Allergy and Infectious Diseases Contract 03-22 (CCR), National Institutes of Health T32 AI007605-07 (JEY), and the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Abbreviations
- ABPA
allergic bronchopulmonary aspergillosis
- ACCA
anti-chitobioside IgA
- ALCA
anti-laminaribioside IgG
- AMCA
anti-mannobioside IgG
- ASCA
antibody to Saccharomyces cerevisiae
- CD
Crohn’s disease
- CGD
Chronic Granulomatous Disease
- EDID
ectodermal dysplasia with immunodeficiency
- ELISA
enzyme-linked immunosorbent assay
- GI
gastrointestinal
- HIES
Hyper IgE Syndrome
- IBD
inflammatory bowel disease
- NADPH
nicotinamide adenine dinucleotide phosphate
- NLR
NOD-like receptor
- OmpC
outer membrane porin of E. Coli
- pANCA
perinuclear antineutrophil antibody
- TLR
Toll-like receptor
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
C.C.R. has received research support from the National Institutes of Health/National Institute of Allergy and Infectious Diseases, has served on the medical advisory boards of Talecris Corporation and Baxter Therapeutics, and has received a research grant from Baxter Therapeutics.
S.T. is a founder and on the Board of Directors of Prometheus RxDx, Inc.
J.E.Y., S.S.R., G.U., C.L., H.L.M., S.M.H., W.Q., N.H., and L.M. have declared that they have no conflict of interest.
References
- 1.Holland SM. Chronic Granulomatous Disease. Clin Rev Allergy Immunol. 2009 doi: 10.1007/s12016-009-8136-z. [DOI] [PubMed] [Google Scholar]
- 2.Malech HL, Hickstein DD. Genetics, biology and clinical management of myeloid cell primary immune deficiencies: chronic granulomatous disease and leukocyte adhesion deficiency. Curr Opin Hematol. 2007;14:29–36. doi: 10.1097/00062752-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Yu G, Hong DK, Dionis KY, Rae J, Heyworth PG, Curnutte JT, Lewis DB. Focus on FOCIS: the continuing diagnostic challenge of autosomal recessive chronic granulomatous disease. Clin Immunol. 2008;128:117–126. doi: 10.1016/j.clim.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Jones LB, McGrogan P, Flood TJ, Gennery AR, Morton L, Thrasher A, Goldblatt D, Parker L, Cant AJ. Special article: chronic granulomatous disease in the United Kingdom and Ireland: a comprehensive national patient-based registry. Clin Exp Immunol. 2008;152:211–218. doi: 10.1111/j.1365-2249.2008.03644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matute JD, Arias AA, Wright NA, Wrobel I, Waterhouse CC, Li XJ, Marchal CC, Stull ND, Lewis DB, Steele M, Kellner JD, Yu W, Meroueh SO, Nauseef WM, Dinauer MC. A new genetic subgroup of chronic granulomatous disease with autosomal recessive mutations in p40 phox and selective defects in neutrophil NADPH oxidase activity. Blood. 2009;114:3309–3315. doi: 10.1182/blood-2009-07-231498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winkelstein JA, Marino MC, Johnston RB, Jr, Boyle J, Curnutte J, Gallin JI, Malech HL, Holland SM, Ochs H, Quie P, Buckley RH, Foster CB, Chanock SJ, Dickler H. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine (Baltimore) 2000;79:155–169. doi: 10.1097/00005792-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Eppinger TM, Greenberger PA, White DA, Brown AE, Cunningham-Rundles C. Sensitization to Aspergillus species in the congenital neutrophil disorders chronic granulomatous disease and hyper-IgE syndrome. J Allergy Clin Immunol. 1999;104:1265–1272. doi: 10.1016/s0091-6749(99)70023-0. [DOI] [PubMed] [Google Scholar]
- 8.Schappi MG, Jaquet V, Belli DC, Krause KH. Hyperinflammation in chronic granulomatous disease and anti-inflammatory role of the phagocyte NADPH oxidase. Semin Immunopathol. 2008;30:255–271. doi: 10.1007/s00281-008-0119-2. [DOI] [PubMed] [Google Scholar]
- 9.De Ravin SS, Naumann N, Cowen EW, Friend J, Hilligoss D, Marquesen M, Balow JE, Barron KS, Turner ML, Gallin JI, Malech HL. Chronic granulomatous disease as a risk factor for autoimmune disease. J Allergy Clin Immunol. 2008;122:1097–1103. doi: 10.1016/j.jaci.2008.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arimura Y, Goto A, Yamashita K, Endo T, Ikeda H, Tanaka K, Tsutsumi H, Shinomura Y, Imai K. Intractable colitis associated with chronic granulomatous disease. J Med Microbiol. 2006;55:1587–1590. doi: 10.1099/jmm.0.46722-0. [DOI] [PubMed] [Google Scholar]
- 11.Barton LL, Moussa SL, Villar RG, Hulett RL. Gastrointestinal complications of chronic granulomatous disease: case report and literature review. Clin Pediatr (Phila) 1998;37:231–236. doi: 10.1177/000992289803700403. [DOI] [PubMed] [Google Scholar]
- 12.Hoare S, Walsh JE, Eastham E, Abinun MA, Cant AJ. Abnormal technetium labelled white cell scan in the colitis of chronic granulomatous disease. Arch Dis Child. 1997;77:50–51. doi: 10.1136/adc.77.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang JS, Noack D, Rae J, Ellis BA, Newbury R, Pong AL, Lavine JE, Curnutte JT, Bastian J. Chronic granulomatous disease caused by a deficiency in p47(phox) mimicking Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:690–695. doi: 10.1016/s1542-3565(04)00292-7. [DOI] [PubMed] [Google Scholar]
- 14.Levine S, Smith VV, Malone M, Sebire NJ. Histopathological features of chronic granulomatous disease (CGD) in childhood. Histopathology. 2005;47:508–516. doi: 10.1111/j.1365-2559.2005.02258.x. [DOI] [PubMed] [Google Scholar]
- 15.Marciano BE, Rosenzweig SD, Kleiner DE, Anderson VL, Darnell DN, Anaya-O'Brien S, Hilligoss DM, Malech HL, Gallin JI, Holland SM. Gastrointestinal involvement in chronic granulomatous disease. Pediatrics. 2004;114:462–468. doi: 10.1542/peds.114.2.462. [DOI] [PubMed] [Google Scholar]
- 16.Schappi MG, Smith VV, Goldblatt D, Lindley KJ, Milla PJ. Colitis in chronic granulomatous disease. Arch Dis Child. 2001;84:147–151. doi: 10.1136/adc.84.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gopal L, Forbes J, Uzel G, Holland SM, Heller T. Gastrointestinal fistulae in chronic granulomatous disease. Am J Gastroenterol. 2009;104:2112–2113. doi: 10.1038/ajg.2009.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marks DJ, Miyagi K, Rahman FZ, Novelli M, Bloom SL, Segal AW. Inflammatory bowel disease in CGD reproduces the clinicopathological features of Crohn's disease. Am J Gastroenterol. 2009;104:117–124. doi: 10.1038/ajg.2008.72. [DOI] [PubMed] [Google Scholar]
- 19.Schappi MG, Klein NJ, Lindley KJ, Rampling D, Smith VV, Goldblatt D, Milla PJ. The nature of colitis in chronic granulomatous disease. J Pediatr Gastroenterol Nutr. 2003;36:623–631. doi: 10.1097/00005176-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Hugot JP, Cho JH. Update on genetics of inflammatory bowel disease. Curr Opin Gastroenterol. 2002;18:410–415. doi: 10.1097/00001574-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Rioux JD, Xavier RJ, Taylor KD, Silverberg MS, Goyette P, Huett A, Green T, Kuballa P, Barmada MM, Datta LW, Shugart YY, Griffiths AM, Targan SR, Ippoliti AF, Bernard EJ, Mei L, Nicolae DL, Regueiro M, Schumm LP, Steinhart AH, Rotter JI, Duerr RH, Cho JH, Daly MJ, Brant SR. Genome-wide association study identifies new susceptibility loci for Crohn disease and implicates autophagy in disease pathogenesis. Nat Genet. 2007;39:596–604. doi: 10.1038/ng2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beaven SW, Abreu MT. Biomarkers in inflammatory bowel disease. Curr Opin Gastroenterol. 2004;20:318–327. doi: 10.1097/00001574-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Dotan N, Altstock RT, Schwarz M, Dukler A. Anti-glycan antibodies as biomarkers for diagnosis and prognosis. Lupus. 2006;15:442–450. doi: 10.1191/0961203306lu2331oa. [DOI] [PubMed] [Google Scholar]
- 24.Targan SR, Karp LC. Inflammatory bowel disease diagnosis, evaluation and classification: state-of-the art approach. Curr Opin Gastroenterol. 2007;23:390–394. doi: 10.1097/MOG.0b013e3281722271. [DOI] [PubMed] [Google Scholar]
- 25.Landers CJ, Cohavy O, Misra R, Yang H, Lin YC, Braun J, Targan SR. Selected loss of tolerance evidenced by Crohn's disease-associated immune responses to auto- and microbial antigens. Gastroenterology. 2002;123:689–699. doi: 10.1053/gast.2002.35379. [DOI] [PubMed] [Google Scholar]
- 26.Reumaux D, Sendid B, Poulain D, Duthilleul P, Dewit O, Colombel JF. Serological markers in inflammatory bowel diseases. Best Pract Res Clin Gastroenterol. 2003;17:19–35. doi: 10.1053/bega.2002.0347. [DOI] [PubMed] [Google Scholar]
- 27.Targan SR, Karp LC. Defects in mucosal immunity leading to ulcerative colitis. Immunol Rev. 2005;206:296–305. doi: 10.1111/j.0105-2896.2005.00286.x. [DOI] [PubMed] [Google Scholar]
- 28.Wehkamp J, Stange EF. A new look at Crohn's disease: breakdown of the mucosal antibacterial defense. Ann N Y Acad Sci. 2006;1072:321–331. doi: 10.1196/annals.1326.030. [DOI] [PubMed] [Google Scholar]
- 29.Vowells SJ, Sekhsaria S, Malech HL, Shalit M, Fleisher TA. Flow cytometric analysis of the granulocyte respiratory burst: a comparison study of fluorescent probes. J Immunol Methods. 1995;178:89–97. doi: 10.1016/0022-1759(94)00247-t. [DOI] [PubMed] [Google Scholar]
- 30.Cohavy O, Bruckner D, Gordon LK, Misra R, Wei B, Eggena ME, Targan SR, Braun J. Colonic bacteria express an ulcerative colitis pANCA-related protein epitope. Infect Immun. 2000;68:1542–1548. doi: 10.1128/iai.68.3.1542-1548.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lodes MJ, Cong Y, Elson CO, Mohamath R, Landers CJ, Targan SR, Fort M, Hershberg RM. Bacterial flagellin is a dominant antigen in Crohn disease. J Clin Invest. 2004;113:1296–1306. doi: 10.1172/JCI20295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saxon A, Shanahan F, Landers C, Ganz T, Targan S. A distinct subset of antineutrophil cytoplasmic antibodies is associated with inflammatory bowel disease. J Allergy Clin Immunol. 1990;86:202–210. doi: 10.1016/s0091-6749(05)80067-3. [DOI] [PubMed] [Google Scholar]
- 33.Sendid B, Colombel JF, Jacquinot PM, Faille C, Fruit J, Cortot A, Lucidarme D, Camus D, Poulain D. Specific antibody response to oligomannosidic epitopes in Crohn's disease. Clin Diagn Lab Immunol. 1996;3:219–226. doi: 10.1128/cdli.3.2.219-226.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sutton CL, Kim J, Yamane A, Dalwadi H, Wei B, Landers C, Targan SR, Braun J. Identification of a novel bacterial sequence associated with Crohn's disease. Gastroenterology. 2000;119:23–31. doi: 10.1053/gast.2000.8519. [DOI] [PubMed] [Google Scholar]
- 35.D'Agata ID, Paradis K, Chad Z, Bonny Y, Seidman E. Leucocyte adhesion deficiency presenting as a chronic ileocolitis. Gut. 1996;39:605–608. doi: 10.1136/gut.39.4.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanderson IR, Bisset WM, Milla PJ, Leonard JV. Chronic inflammatory bowel disease in glycogen storage disease type 1B. J Inherit Metab Dis. 1991;14:771–776. doi: 10.1007/BF01799948. [DOI] [PubMed] [Google Scholar]
- 37.Yamaguchi T, Ihara K, Matsumoto T, Tsutsumi Y, Nomura A, Ohga S, Hara T. Inflammatory bowel disease-like colitis in glycogen storage disease type 1b. Inflamm Bowel Dis. 2001;7:128–132. doi: 10.1097/00054725-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Hussain N, Quezado M, Huizing M, Geho D, White JG, Gahl W, Mannon P. Intestinal disease in Hermansky-Pudlak syndrome: occurrence of colitis and relation to genotype. Clin Gastroenterol Hepatol. 2006;4:73–80. doi: 10.1016/s1542-3565(05)00858-x. [DOI] [PubMed] [Google Scholar]
- 39.Seger RA. Modern management of chronic granulomatous disease. Br J Haematol. 2008;140:255–266. doi: 10.1111/j.1365-2141.2007.06880.x. [DOI] [PubMed] [Google Scholar]
- 40.Nenci A, Becker C, Wullaert A, Gareus R, van Loo G, Danese S, Huth M, Nikolaev A, Neufert C, Madison B, Gumucio D, Neurath MF, Pasparakis M. Epithelial NEMO links innate immunity to chronic intestinal inflammation. Nature. 2007;446:557–561. doi: 10.1038/nature05698. [DOI] [PubMed] [Google Scholar]
- 41.Pai SY, Levy O, Jabara HH, Glickman JN, Stoler-Barak L, Sachs J, Nurko S, Orange JS, Geha RS. Allogeneic transplantation successfully corrects immune defects, but not susceptibility to colitis, in a patient with nuclear factor-kappaB essential modulator deficiency. J Allergy Clin Immunol. 2008;122:1113–1118. doi: 10.1016/j.jaci.2008.08.026. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Permaul P, Narla A, Hornick JL, Pai SY. Allogeneic hematopoietic stem cell transplantation for X-linked ectodermal dysplasia and immunodeficiency: case report and review of outcomes. Immunol Res. 2009;44:89–98. doi: 10.1007/s12026-008-8085-2. [DOI] [PubMed] [Google Scholar]
- 43.Agarwal S, Mayer L. Gastrointestinal manifestations in primary immune disorders. Inflamm Bowel Dis. 2009 doi: 10.1002/ibd.21040. [DOI] [PubMed] [Google Scholar]
- 44.Daniels JA, Lederman HM, Maitra A, Montgomery EA. Gastrointestinal tract pathology in patients with common variable immunodeficiency (CVID): a clinicopathologic study and review. Am J Surg Pathol. 2007;31:1800–1812. doi: 10.1097/PAS.0b013e3180cab60c. [DOI] [PubMed] [Google Scholar]
- 45.Couper R, Kapelushnik J, Griffiths AM. Neutrophil dysfunction in glycogen storage disease Ib: association with Crohn's-like colitis. Gastroenterology. 1991;100:549–554. doi: 10.1016/0016-5085(91)90229-e. [DOI] [PubMed] [Google Scholar]
- 46.Uzel G, Kleiner DE, Kuhns DB, Holland SM. Dysfunctional LAD-1 neutrophils and colitis. Gastroenterology. 2001;121:958–964. doi: 10.1053/gast.2001.28022. [DOI] [PubMed] [Google Scholar]
- 47.Smith AM, Rahman FZ, Hayee B, Graham SJ, Marks DJ, Sewell GW, Palmer CD, Wilde J, Foxwell BM, Gloger IS, Sweeting T, Marsh M, Walker AP, Bloom SL, Segal AW. Disordered macrophage cytokine secretion underlies impaired acute inflammation and bacterial clearance in Crohn's disease. J Exp Med. 2009;206:1883–1897. doi: 10.1084/jem.20091233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rahman FZ, Hayee B, Chee R, Segal AW, Smith AM. Impaired macrophage function following bacterial stimulation in chronic granulomatous disease. Immunology. 2009;128:253–259. doi: 10.1111/j.1365-2567.2009.03112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mow WS, Vasiliauskas EA, Lin YC, Fleshner PR, Papadakis KA, Taylor KD, Landers CJ, Abreu-Martin MT, Rotter JI, Yang H, Targan SR. Association of antibody responses to microbial antigens and complications of small bowel Crohn's disease. Gastroenterology. 2004;126:414–424. doi: 10.1053/j.gastro.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 50.Slack E, Hapfelmeier S, Stecher B, Velykoredko Y, Stoel M, Lawson MA, Geuking MB, Beutler B, Tedder TF, Hardt WD, Bercik P, Verdu EF, McCoy KD, Macpherson AJ. Innate and adaptive immunity cooperate flexibly to maintain host-microbiota mutualism. Science. 2009;325:617–620. doi: 10.1126/science.1172747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Henckaerts L, Pierik M, Joossens M, Ferrante M, Rutgeerts P, Vermeire S. Mutations in pattern recognition receptor genes modulate seroreactivity to microbial antigens in patients with inflammatory bowel disease. Gut. 2007;56:1536–1542. doi: 10.1136/gut.2007.125468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dann SM, Eckmann L. Innate immune defenses in the intestinal tract. Curr Opin Gastroenterol. 2007;23:115–120. doi: 10.1097/MOG.0b013e32803cadf4. [DOI] [PubMed] [Google Scholar]
- 53.Devlin SM, Yang H, Ippoliti A, Taylor KD, Landers CJ, Su X, Abreu MT, Papadakis KA, Vasiliauskas EA, Melmed GY, Fleshner PR, Mei L, Rotter JI, Targan SR. NOD2 variants and antibody response to microbial antigens in Crohn's disease patients and their unaffected relatives. Gastroenterology. 2007;132:576–586. doi: 10.1053/j.gastro.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 54.Takedatsu H, Taylor KD, Mei L, McGovern DP, Landers CJ, Gonsky R, Cong Y, Vasiliauskas EA, Ippoliti A, Elson CO, Rotter JI, Targan SR. Linkage of Crohn's disease-related serological phenotypes: NFKB1 haplotypes are associated with anti-CBir1 and ASCA, and show reduced NF-kappaB activation. Gut. 2009;58:60–67. doi: 10.1136/gut.2008.156422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mei L, Targan SR, Landers CJ, Dutridge D, Ippoliti A, Vasiliauskas EA, Papadakis KA, Fleshner PR, Rotter JI, Yang H. Familial expression of anti-Escherichia coli outer membrane porin C in relatives of patients with Crohn's disease. Gastroenterology. 2006;130:1078–1085. doi: 10.1053/j.gastro.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Brodsky N, Freeman AF, Demidowich A, Davis J, Turner ML, Anderson VL, Darnell DN, Welch PA, Kuhns DB, Frucht DM, Malech HL, Gallin JI, Kobayashi SD, Whitney AR, Voyich JM, Musser JM, Woellner C, Schaffer AA, Puck JM, Grimbacher B. STAT3 mutations in the hyper-IgE syndrome. N Engl J Med. 2007;357:1608–1619. doi: 10.1056/NEJMoa073687. [DOI] [PubMed] [Google Scholar]
- 57.Avery DT, Deenick EK, Ma CS, Suryani S, Simpson N, Chew GY, Chan TD, Palendira U, Bustamante J, Boisson-Dupuis S, Choo S, Bleasel KE, Peake J, King C, French MA, Engelhard D, Al-Hajjar S, Al-Muhsen S, Magdorf K, Roesler J, Arkwright PD, Hissaria P, Riminton DS, Wong M, Brink R, Fulcher DA, Casanova JL, Cook MC, Tangye SG. B cell-intrinsic signaling through IL-21 receptor and STAT3 is required for establishing long-lived antibody responses in humans. J Exp Med. 207:155–171. doi: 10.1084/jem.20091706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cannioto Z, Berti I, Martelossi S, Bruno I, Giurici N, Crovella S, Ventura A. IBD and IBD mimicking enterocolitis in children younger than 2 years of age. Eur J Pediatr. 2009;168:149–155. doi: 10.1007/s00431-008-0721-2. [DOI] [PubMed] [Google Scholar]
- 59.Desir B, Amre DK, Lu SE, Ohman-Strickland P, Dubinsky M, Fisher R, Seidman EG. Utility of serum antibodies in determining clinical course in pediatric Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:139–146. doi: 10.1016/s1542-3565(03)00321-5. [DOI] [PubMed] [Google Scholar]
- 60.Dubinsky M. Special issues in pediatric inflammatory bowel disease. World J Gastroenterol. 2008;14:413–420. doi: 10.3748/wjg.14.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoffenberg EJ, Fidanza S, Sauaia A. Serologic testing for inflammatory bowel disease. J Pediatr. 1999;134:447–452. doi: 10.1016/s0022-3476(99)70202-7. [DOI] [PubMed] [Google Scholar]
- 62.Zholudev A, Zurakowski D, Young W, Leichtner A, Bousvaros A. Serologic testing with ANCA, ASCA, and anti-OmpC in children and young adults with Crohn's disease and ulcerative colitis: diagnostic value and correlation with disease phenotype. Am J Gastroenterol. 2004;99:2235–2241. doi: 10.1111/j.1572-0241.2004.40369.x. [DOI] [PubMed] [Google Scholar]
- 63.Markowitz J, Kugathasan S, Dubinsky M, Mei L, Crandall W, Leleiko N, Oliva-Hemker M, Rosh J, Evans J, Mack D, Otley A, Pfefferkorn M, Bahar R, Vasiliauskas E, Wahbeh G, Silber G, Quiros JA, Wrobel I, Nebel J, Landers C, Picornell Y, Targan S, Lerer T, Hyams J. Age of diagnosis influences serologic responses in children with Crohn's disease: A possible clue to etiology? Inflamm Bowel Dis. 2008 doi: 10.1002/ibd.20831. [DOI] [PMC free article] [PubMed] [Google Scholar]