Abstract
Both high platelet reactivity (HPR) and CYP2C19 genotyping have been proposed to stratify cardiovascular event risk and to personalize maintenance dual antiplatelet therapy (DAPT) in stented patients. However, how well CYP2C19 genotype correlates with HPR in patients on maintenance DAPT is less clear. We determined the association of CYP2C19 loss-of-function (*2) and gain-of- function (*17) allele status with platelet reactivity in 118 stented patients on DAPT ≥2 weeks and in 143 patients with stable coronary artery disease on aspirin therapy alone. Thirty-two percent and 36% carried at least one copy of *2 and *17 alleles, respectively. Neither allele was associated with platelet reactivity in patients on aspirin therapy alone. On DAPT, platelet aggregation was higher in those with *2 allele than non-carriers (p ≤0.01) but did not differ between those with the *17 allele and non-carriers. The prevalence of HPR using the 20uM ADP-induced aggregation cutpoint was 34% in the total population; 26% in *1/*1 homozygotes, 49% in those with the *2 allele and 20% in those with the *17 allele (p=0.006). Determination of diplotype status enhanced identification of HPR. However, platelet function on DAPT is highly variable within diplotype groups. Therefore, CYP2C19 genotype and HPR are imperfect correlates of each other. Since both predict CV events with similar risk ratios, CYP2C19 genotyping and HPR may provide complementary information to stratify risk and personalized DAPT in stented patients than either alone.
Keywords: cytochrome P450 2C19*2, cytochrome P450 2C19*17, platelets, clopidogrel, pharmacogenomics
Dual antiplatelet therapy with clopidogrel and aspirin (DAPT) is the cornerstone of pharmacologic treatment to prevent ischemic events following percutaneous coronary intervention (PCI) and acute coronary syndromes (ACS). High platelet reactivity (HPR) as measured by ex vivo platelet aggregation in response to adenosine diphosphate (ADP) during DAPT has been linked to post-PCI ischemic event occurrence in multiple reports (1). Cytochrome P450 2C19 (CYP2C19) is a drug metabolism enzyme that plays an important role in converting clopidogrel into its active metabolite (2). The enzyme is encoded by CYP2C19 gene located on chromosome 10. A common single nucleotide polymorphism (SNP) of CYP2C19 located in exon 5 (681G>A, rs4244285, designated *2) encodes for a cryptic splice variant resulting in a protein product with no enzyme activity (3). In several studies, the loss-of-function CYP2C19*2 allele was associated with decreased clopidogrel responsiveness as measured by ADP-induced ex vivo platelet aggregation and post-PCI ischemic risk (4–8). In contrast, the common CYP2C19*17 allele, resulting from a SNP (-806C>T, rs12248560) has been associated with increased expression and enzyme activity. However, its effect on clopidogrel response and the differential effects of *17 and *2 on platelet function during maintenance DAPT have been less studied (8). Moreover, the influence of genotype on platelet function in the absence of clopidogrel therapy is unknown.
Considering the advent of more potent P2Y12 inhibitors that do not require activation by CYP, the assessment of clopidogrel antiplatelet efficacy will become more important in deciding long term treatment choice (9). How CYP2C19 genotypes relate to high platelet reactivity (HPR) as measured by ex vivo platelet function testing during maintenance DAPT and the role of genetic analyses to identify the subset of PCI patients at increased risk for cardiovascular events is increasingly under investigation (10). Therefore, we sought to determine how well the CYP2C19 loss-of-function and gain-of- function alleles associate with platelet reactivity in general and also how well they identified patients with HPR during maintenance DAPT.
METHODS
Patients >18 years, who had established coronary artery disease (CAD) and were on aspirin (81 – 325 mg/day) therapy for a minimum of two weeks were studied (n = 261). Among these patients, 143 were consecutive stable outpatients on aspirin therapy alone (clopidogrel naïve). One hundred and eighteen consecutive patients had undergone prior coronary arterial stenting and were on aspirin and maintenance clopidogrel therapy for at least 2 weeks; of these, 84 were undergoing non-emergent diagnostic arteriography and 34 were stable outpatients. Patients with a bleeding diathesis or a history of gastrointestinal bleeding, hemorrhagic stroke, illicit drug or alcohol abuse, coagulopathy, platelet count <100,000/mm3, hematocrit <25%, creatinine >2 mg/dL, myocardial infarction within 48 hours, or non-hemorrhagic cerebrovascular accident within 3 months were excluded. The study was approved by the Institutional Review Board at Sinai Hospital of Baltimore and informed consent was obtained from each patient.
Platelet Aggregation
Blood samples were collected by venipuncture in vacutainer tubes (Becton-Dickinson®, Franklin Lakes, NJ) containing 3.8% trisodium citrate. The tubes were centrifuged at 120 g for 5 minutes to recover platelet rich plasma (PRP) and further centrifuged at 850 g for 10 minutes to recover platelet poor plasma (PPP). The PRP and PPP were stored at room temperature and used within two hours. Briefly, platelets were stimulated with ADP (5 µM and 20 µM) as previously described (10). Aggregation was assessed using a Chronolog Lumi-Aggregometer (Model 490-4D) with the AGGRO/LINK control software (Chronolog, Havertown, PA). Aggregation was expressed as the maximum percent change in light transmittance from baseline, using PPP as a reference.
Genotyping for CYP2C19 [*2 (rs4244285), *3 (rs4986893) and *17 (rs12248560)] was performed using TaqManR® SNP genotyping assays (Applied Biosystems, Foster City, CA). CYP2C19*3 was present in only one Asian subject and this subject was excluded in subsequent analyses.
We postulated that CYP2C19*2 carriers (heterozygotes and homozygotes combined) will have at least 20% higher prevalence of HPR due to decreased antiplatelet effect of clopidogrel compared to non-carriers. Therefore, given the frequency of the *2 allele in the population, in order to determine a 20% absolute difference in the prevalence of HPR between these two groups, a sample size of 105 patients was required with an alpha value of 0.05 and power of 80% (SigmaStatR® 3.1 Software (Point Richmond, CA, USA).
Categorical variables are expressed as n (%) and continuous variables as mean ± SD. ANOVA, Student’s t-test or Mann-Whitney Rank Sum test were used for comparison of continuous variables after evaluation for normal distribution by the Kolmorgorov-Smirnov test (SigmaStatR® 3.1 Software; Point Richmond, CA, USA). Chi-square analysis was used for comparison of categorical variables between groups. A p-value of <0.05 was considered statistically significant.
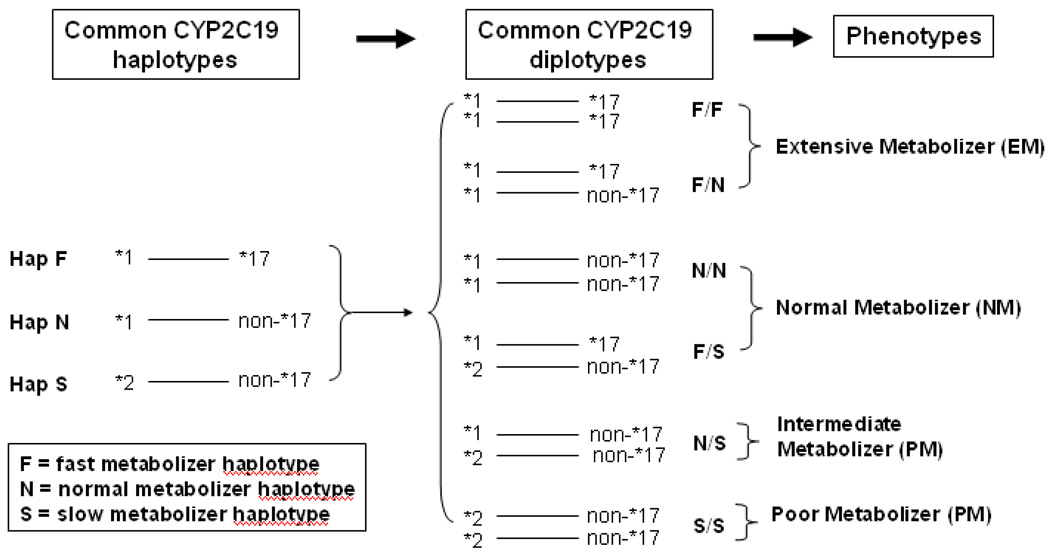
We examined the relationship between CYP2C19 genotypes and baseline and post-clopidogrel platelet aggregation, measured as percent aggregation and as a dichotomous variable (comparison of frequency of HPR). HPR was defined by specific cutoff values by receiver operating characteristic curve (ROC) analyses (5 uM ADP = 46%; 20 uM ADP = 59%) as previously described (10). First, we evaluated the relationship between CYP2C19 genotypes and HPR frequency treating the *2 and *17 variants as independent. Due to linkage disequilibrium between CYP2C19 *1 and *17 gain-of-function (fast metabolizer) variants, only three (of four possible) haplotypes exist (Figure 1). These three haplotypes result in six possible diplotypes. In a second analysis, we compared platelet function among the six diplotypes. We also classified subjects into extensive metabolizer (EM), normal metabolizer (NM), intermediate metabolizer (IM) and poor metabolizer (PM) groups, and compared platelet aggregation and HPR between these groups.
Figure 1.
Linkage disequilibrium and CYP2C19 haplotypes. Due to linkage disequilibrium between CYP2C19 *2 loss-of-function (slow metabolizer) and *17 gain-of-function (fast metabolizer) variants, only three (of four possible) haplotypes exist. These three haplotypes result in six diplotypes which define four main phenotypes, extensive metabolizers (EM), normal metabolizers (NM), intermediate metabolizers (IM) and poor metabolizers (PM).
The study was funded by Sinai Center for Thrombosis Research and a NIH grant (NIH U01 GM074518). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
RESULTS
Demographic characteristics of the population are shown in Table 1. Clopidogrel naïve patients were more often Caucasian and had higher systolic blood pressure and less often used beta-blockers than patients on clopidogrel maintenance therapy. The frequency of the CYP2C19 *2, and *17 alleles in the overall population were 0.17, and 0.20, respectively, and very similar among Caucasians and African Americans in our sample (Table 2). Genotype frequencies were in Hardy-Weinberg equilibrium. The *2 and *17 alleles were in linkage disequilibrium (D’ = 1; r2 = 0.04). Based on Chi-square analysis the p-values are -*2: p=0.24, *17: p=0.87. There were no differences in demographic variables between CYP2C19*2 genotype groups on clopidogrel maintenance therapy (Table 1).
Table 1.
Characteristics of Study Groups.
| Clopidogrel Naive (n=143) |
Clopidogrel Maintenance (n=118) |
p-value | Clopidogrel Maintenance CYP 2C19*2 Carriers (n=41) |
Clopidogrel Maintenance CYP 2C19 Non-carriers (n=77) |
p-value | |
|---|---|---|---|---|---|---|
| Age (years) | 65±11 | 63±11 | 0.13 | 63±11 | 64±11 | 0.64 |
| Gender n, (male %) | 52, (35) | 53, (45) | 0.05 | 14, (34) | 39, (51) | 0.05 |
| Caucasians n, (%) | 94, (63) | 59, (50) | 0.02 | 20, (49) | 41, (53) | 0.34 |
| African-Americans n, (%) | 49, (33) | 55, (47) | 0.11 | 19, (46) | 35, (45) | 0.46 |
| Body mass index (kg/m2) | 30±6 | 31±5 | 0.15 | 31±5 | 31±9 | 1.0 |
| Systolic Blood Pressure (mm Hg) | 142±21 | 135±18 | <0.01 | 135±18 | 136±21 | 0.80 |
| Diastolic Blood Pressure (mm Hg) | 73±13 | 72±15 | 0.55 | 72±15 | 72±15 | 1.0 |
| Medical History | ||||||
| History of Smoking n, (%) | 41, (27) | 23, (19) | 0.06 | 9, (22) | 14, (18) | 0.30 |
| Current Smokers n, (%) | 38, (25) | 18, (15) | 0.02 | 11, (27) | 17, (22) | 0.27 |
| Hypertension n, (%) | 116, (77) | 93, (79) | 0.35 | 33, (80) | 60, (77) | 0.35 |
| Hyperlipidemia n, (%) | 111, (74) | 85, (72) | 0.36 | 30, (73) | 55, (71) | 0.41 |
| Diabetes n, (%) | 55, (37) | 46, (39) | 0.37 | 20, (49) | 27, (35) | 0.10 |
| Myocardial infarction n, (%) | 42, (28) | 37, (31) | 0.30 | 14, (34) | 23, (30) | 0.33 |
| Coronary artery bypass graft n, (%) | 29, (19) | 29, (21) | 0.12 | 12, (29) | 17, (22) | 0.20 |
| Family CAD n, (%) | 60, (40) | 53, (45) | 0.21 | 21, (51) | 32, (42) | 0.18 |
| Baseline Medications | ||||||
| Beta-blocker n, (%) | 88, (59) | 85, (72) | 0.01 | 31, (76) | 54, (70) | 0.25 |
| ACE inhibitor n, (%) | 66, (44) | 60, (51) | 0.13 | 17, (41) | 43, (56) | 0.06 |
| Calcium blockers n, (%) | 30, (20) | 33, (28) | 0.07 | 15, (37) | 18, (23) | 0.05 |
| Lipid-lowering agent n, (%) | 109, (73) | 96, (81) | 0.06 | 36, (88) | 60, (78) | 0.09 |
| Diuretic n, (%) | 43, (29) | 26, (22) | 0.10 | 9, (22) | 17, (22) | 0.50 |
| Proton pump inhibitor n, (%) | 40, (27) | 22, (29) | 0.06 | 6, (15) | 16, (21) | 0.21 |
ACE= angiotensin converting enzyme; CAD= coronary artery disease
Table 2.
Allele, Genotype, Haplotype and Diplotype Frequencies of CYP2C19*2 and *17 Stratified by Ethnicity.
|
CYP2C19 Locus N, (%) |
Caucasian (n=155) |
African American (n=101) |
Asian-American (n=5) |
|---|---|---|---|
| Allele Frequencies | |||
| *2 | 53, (17) | 32, (15) | 2, (20) |
| *1 | 257, (83) | 170, (85) | 8, (80) |
| *17 | 66, (21) | 33, (17) | 2, (20) |
| non-*17 | 244, (79) | 169, (83) | 8, (80) |
| Genotype Frequencies | |||
| *17/*17 | 7 (5) | 2 (2) | |
| *1/*17 | 43 (28) | 27 (27) | 3 (60) |
| *1/*1 | 55 (35) | 42 (42) | |
| *2/*17 | 9 (6) | 3 (3) | |
| *1/*2 | 38 (25) | 24 (23) | 2 (20) |
| *2/*2 | 3 (2) | 3 (3) | |
| Metabolizer Frequencies | |||
| EM | 50, (32) | 29, (28) | 2, (40) |
| NM | 64, (41) | 45, (45) | 1, (25) |
| IM | 38, (25) | 24, (24) | 2, (40) |
| PM | 3, (2) | 3, (3) | 0 |
EM = extensive metabolizer (*17/*17 and *1/*17);
NM = normal metabolizer (*1/*1 and *1/*2);
IM = intermediate metabolizer (*1/*2)
PM = poor metabolizer (*2/*2).
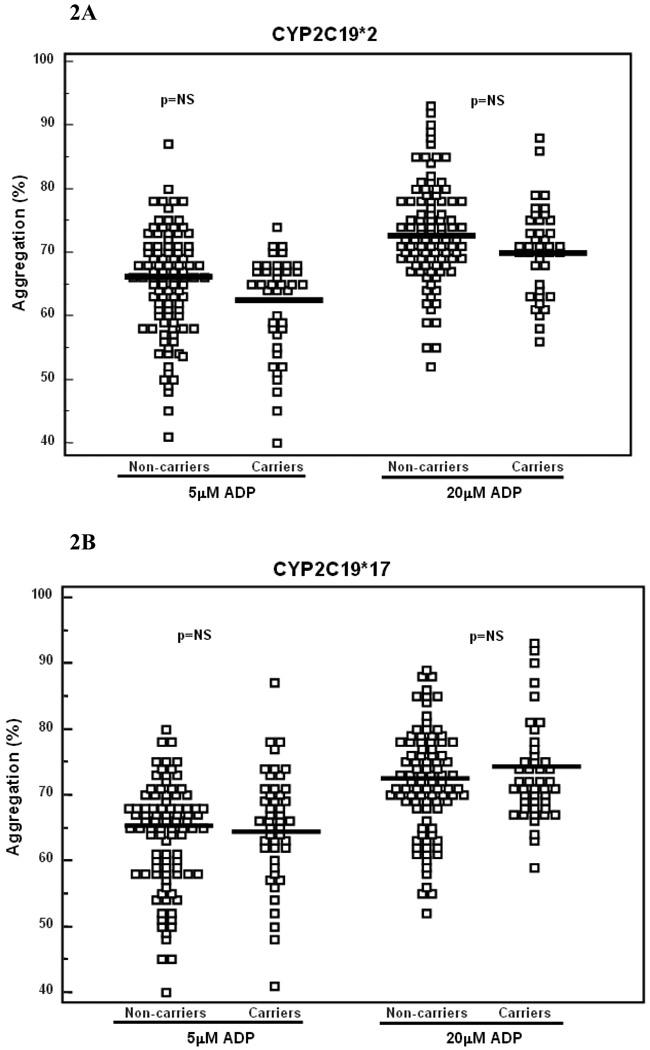
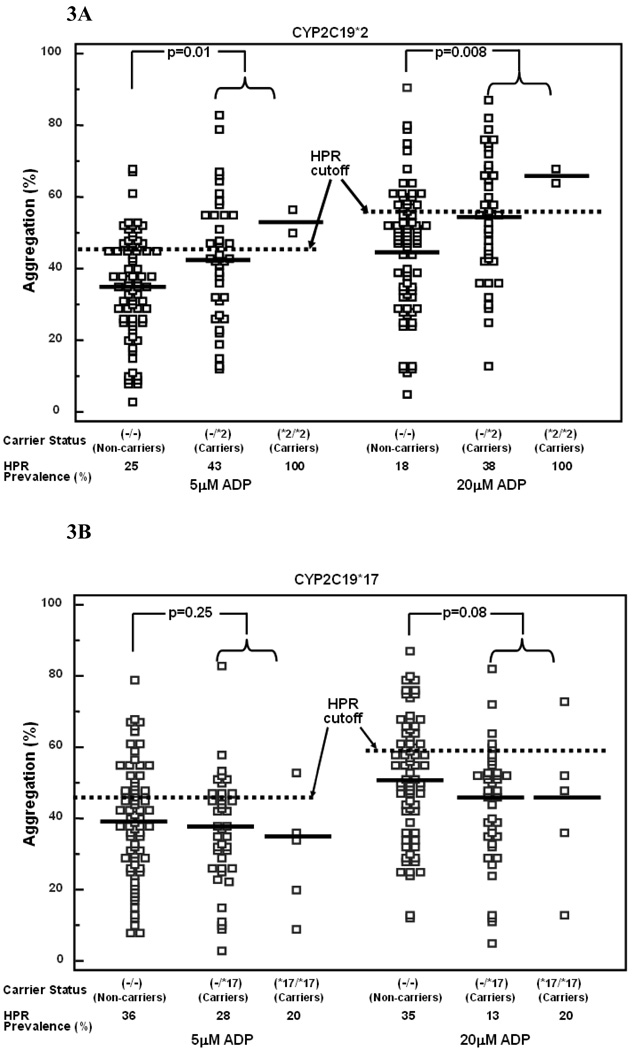
There was no significant relation of CYP2C19 *2 or *17 carrier status to platelet aggregation in patients treated with aspirin alone (Figure 2A and B). In patients on DAPT, platelet aggregation was higher in those carrying one or two copies of the *2 allele, compared to non-carriers (p= 0.01 and p=0.008 for 5 and 20 µM ADP-induced aggregation respectively, Figure 3A). By contrast, ADP-stimulated platelet aggregation did not differ between CYP2C19*17 carriers and non-carriers treated with DAPT (Figure 3B).
Figure 2.
A and B.
Platelet aggregation stimulated by 5 µM and 20 µM ADP in patients treated with aspirin therapy alone and relation to CYP2C19*2 (2A) and CYP2C19*17 (2B) genotypes. Carriers denote presence of one or two copies of the respective alleles. Thick lines indicate mean values.
Figure 3.
A and 3B.
Platelet aggregation stimulated by 5 µM and 20 µM ADP and prevalence of high platelet reactivity (HPR) in patients on clopidogrel maintenance therapy and relation to CYP2C19*2 (3A) and CYP2C19*17 (3B) genotypes. Thick lines indicate mean values and dotted lines indicate HPR cutoff levels. In multivariate analysis in which both the, presence of the *2 and *17 alleles were included, only the *2 allele was an independent predictor of HPR.
The overall prevalence of HPR in patients on DAPT was 23% and 34% assessed by 5 and 20 µM ADP-induced aggregation, respectively. The prevalence of HPR was greater in *2 carriers versus non-carriers (Table 3, Figure 3A). In *17 carriers using the 20 µM ADP-induced aggregation cutpoint the prevalence of HPR was lower than non-carriers (Table 3 and Figure 3B).
Table 3.
Frequency of High Platelet Reactivity (HPR) in Patients on Clopidogrel Maintenance Therapy in Relation to CYP2C19 Genotype
| *2 Carriers (n=41) |
*2 Noncarriers (n=77) |
p-value | |
|---|---|---|---|
| HPR 5µM ADP | 46% | 25% | 0.015 |
| HPR 20µM ADP | 41% | 18% | 0.013 |
|
*17 Carriers (n=45) |
*17 Noncarriers (n=73) |
p-value | |
| HPR 5µM ADP | 27 % | 36% | 0.32 |
| HPR 20µM ADP | 14% | 35% | 0.016 |
Carriers denote one or two copies of the respective allele.
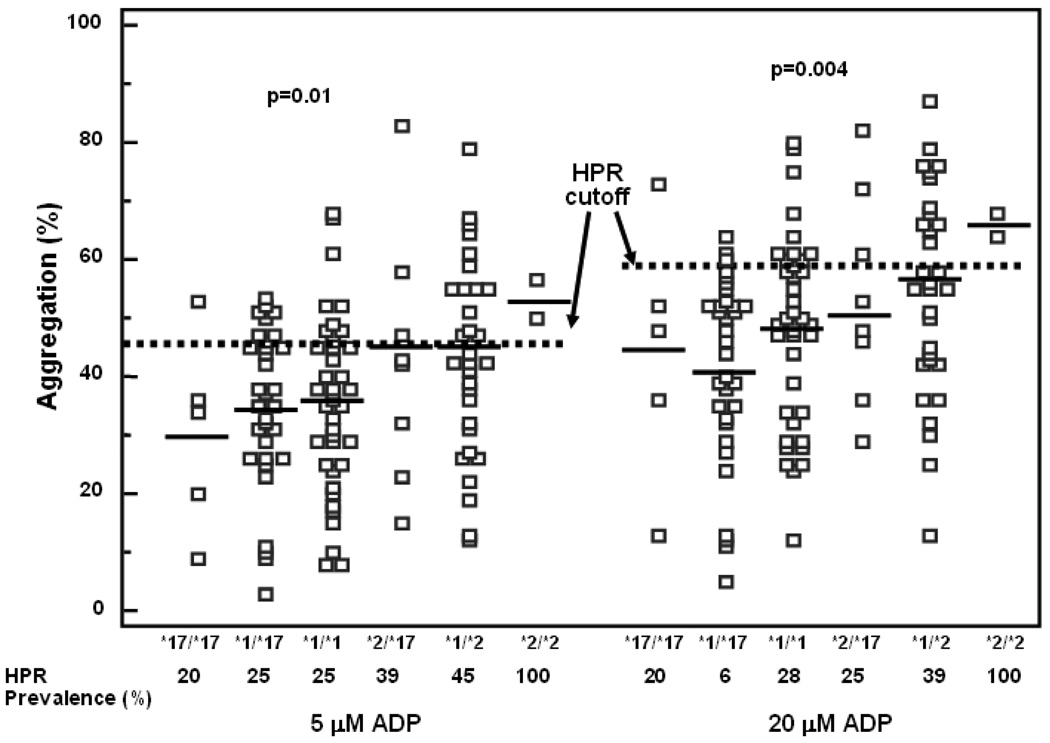
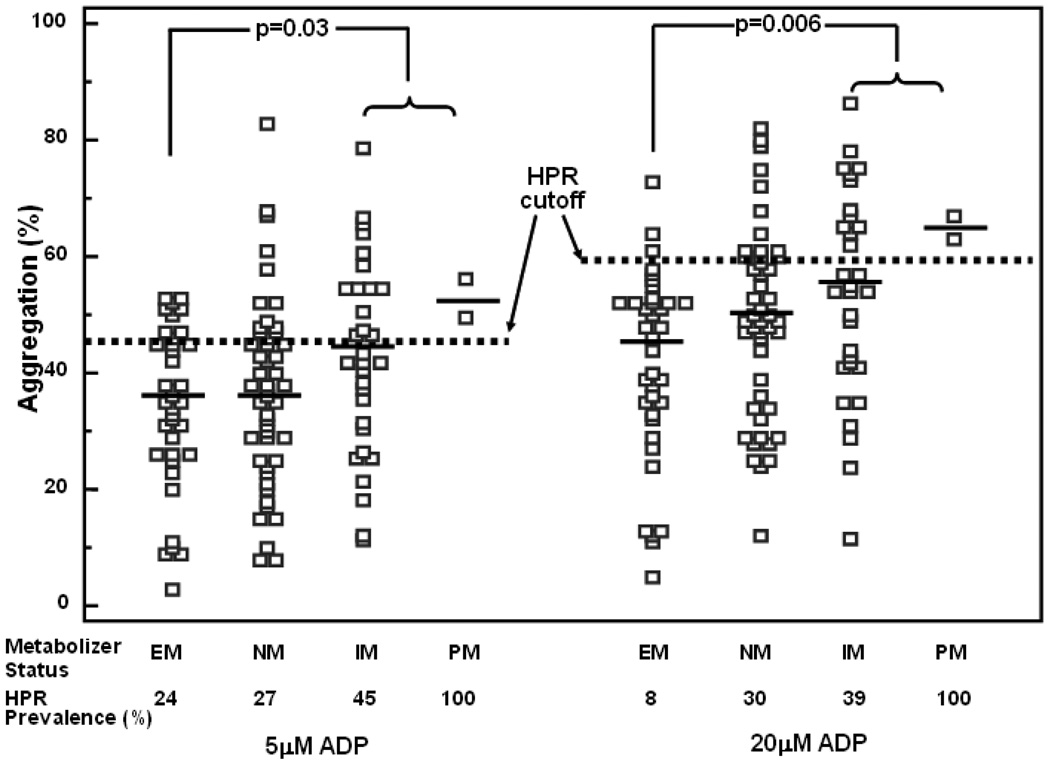
Since the *2 and *17 variants are in linkage disequilibrium, we next considered the six naturally occurring diplotypes. We found a gradient of response in which increasing doses of the *2 allele increased platelet reactivity and HPR and increasing doses of the *17 allele decreased platelet reactivity and HPR (p =0.01 and 0.004 for 5 and 20 uM ADP-induced platelet aggregation, respectively, Figure 4). Both patients homozygous for *2 had HPR by 5 and 20 uM ADP-induced aggregation. However, platelet function was highly variable in *17 homozygotes but only 1/5 patients had HPR (Figure 4). When patients were categorized by metabolizer status a similar pattern was observed (p=0.03 and p=0.06 between EM and PM for 5 and 20 uM ADP-induced platelet aggregation, respectively (Figure 5).
Figure 4.
Platelet aggregation stimulated by 5 µM and 20 µM ADP and prevalence of high platelet reactivity (HPR) in patients on clopidogrel maintenance therapy and relation to CYP2C19*2 and *17 diplotype status. Thick lines indicate mean values and dotted lines indicate high platelet reactivity (HPR) cutoff levels.
Figure 5.
Platelet aggregation stimulated by 5 µM and 20 µM ADP and prevalence of high platelet reactivity (HPR) in patients on clopidogrel maintenance therapy and relation to metabolizer status. Thick lines indicate mean values and dotted lines indicate high platelet reactivity (HPR) cutoff levels.
EM = extensive metabolizer, NM = normal metabolizer, Intermediate metabolizer (IM), PM = poor metabolizer.
DISCUSSION
The present study demonstrates that CYP2C19*2 and *17 alleles are associated with platelet reactivity in patients on maintenance DAPT. We also observed an effect of both CYP2C19*2 and *17 alleles on the frequency of HPR and the effect of CYP2C19*2 was more pronounced. Most importantly, our data suggest that for the majority of patients (those who are not homozygous for either *2 or * 17), HPR cannot be excluded by genotyping in patients on maintenance DAPT.
The observed absence of a relation between pre-clopidogrel platelet function and CYP2C19 allele status suggests a true pharmacogenetic effect and is a critical observation in understanding the mechanism responsible for the reported effect of *2 carrier status on clinical outcomes in previous studies (4,5). It is only during clopidogrel therapy that *2 and *17 carrier status influences platelet function and the prevalence of HPR. Our findings with regard to CYP2C19 variants and clopidogrel response are largely consistent with studies of others where a lower antiplatelet responsiveness to clopidogrel in patients carrying the CYP2C19*2 allele was observed and extends findings to include the relation of pharmacodynamics to CYP2C19*17 genotype, diplotypes of *2 and *17 variants and metabolizer status, and the predictive value of these CYP2C19 variants on the prevalence of HPR in CAD patients on steady-state maintenance clopidogrel and aspirin therapy (4, 6,8, 11,12). Mega et al. demonstrated that CYP2C19*2 carriers had lower clopidogrel active metabolite levels and an absolute reduction in maximal aggregation that was 9% less than non-carriers treated with a 300 mg or a 600 mg followed by a 75 mg maintenance dose of clopidogrel (4). This study was performed in healthy volunteers; aspirin was not uniformly administered; and the relationship between CYP2C19*2 genotype and platelet aggregation in the absence of clopidogrel was not reported (4). Similar to our study, Trenk et al. reported no relation between CYP2C19*2 and pre-treatment residual platelet aggregation (6).
With regard to the gain of function CYP2C19*17 variant, the literature is more mixed. CYP2C19*17 had no influence on residual aggregation in PCI patients treated with 600mg clopidogrel in a study by Geisler et al (13). In a larger study, Sibbing et al demonstrated an association of the *17 allele (both homozygous and heterozygous carriers) with lower on-treatment platelet reactivity and higher bleeding events. However, since the *1 and *17 variants are in linkage disequilibrium, more individuals with the *17 variant would be expected to be lacking *2 variant, which may have accounted for this observed difference in platelet reactivity (14). In a subsequent study, the same authors studied the interaction between *2 and *17 on platelet reactivity measured by Multiplate analyzer in patients on chronic clopidogrel therapy. Similar to our study, a gradual increase in platelet reactivity from *17 carriers to *2 carriers was observed. Although this gradual increase in platelet reactivity across the various genotype combination was statistically significant, differences between non-carriers of the *2 variant with and without the *17 variant (to determine if the *17 variant had an independent effect on platelet reactivity) was not evaluated (15).
We also observed an effect of CYP2C19*2 and *17 alleles on the frequency of HPR when each was considered separately. This is particularly important since HPR is a known predictor of poorer cardiovascular outcomes (16). Hochholzer et al demonstrated that CYP2C19*2 carrier status was an independent predictor of insufficient antiplatelet response to clopidogrel, but platelet function was measured within 1 day after 600 mg loading dose of clopidogrel in the vast majority of patients (17). Overall, our findings are consistent with Hochholzer that genotyping does not completely discriminate HPR. Significantly higher platelet aggregation values measured by multiplate analyzer in CYP2C19*2 carriers and significantly lower platelet aggregation values in CYP2C19*17 carriers were observed compared to homozygous wild-type carriers in patients on chronic DAPT treated with stenting in a recent study by Sibbing et al. In contrast to the present study, both *2 and *17 alleles were identified as independent predictors for platelet reactivity in patients treated with chronic clopidogrel therapy (17).
Despite the clear effect of CYP2C19*2 on platelet aggregation and HPR in clopidogrel-treated patients in the present study, the predictive value to detect HPR in our study was modest. The sensitivity of CYP2C19*2 to detect HPR was only 50–56%; measurement of these alleles alone would miss many patients with HPR. Therefore, CYP2C19 genotyping alone cannot serve as a reliable surrogate for HPR determined by conventional aggregometry.
The moderate sensitivity of CYP2C19 genotyping in detecting HPR is consistent with the multiple non-genetic influences on clopidogrel metabolism and inherent variability in platelet reactivity (9,16). Furthermore, our previously published heritability and genome-wide association analyses show that the CYP2C19 locus accounts for approximately 12% of the variation in platelet response to clopidogrel and that there are likely to exist other yet-to-be identified genetic determinants of clopidogrel response (7). Discovery of additional genes and their variants that influence clopidogrel response may increase predictive value of genetic testing. Finally based on current and previous data, we believe that genotyping alone can not be served as a surrogate marker for HPR and estimations of both genotyping and HPR as complimentary tools may be more efficient to estimate the ischemic risk in patients treated DAPT (16,18).
The sample size of our study was not adequate to assess the effect of CYP2C19*2 or *17 homozygocity on platelet reactivity or HPR. In addition, HPR is also an imperfect predictor of recurrent cardiovascular events and assessment of cardiovascular outcomes were not possible in our study. Thus we could not assess the efficacy of CYP2C19 genotypes and HPR in predicting cardiovascular events. In this study we have included only light transmittance aggregometry to assess platelet function and the pattern of genetic influence on clopidogrel antiplatelet effect might have been different with whole blood assays such as VerifyNow, VASP or Multiplate analyzer.
The present study demonstrated that determination of diplotype status enhanced identification of HPR in patients on maintenance DAPT. However, platelet function on DAPT is highly variable within diplotype groups except *2 homozygotes. Thus our data suggest that for the majority of patients (those who are not homozygous for CYP2C19*2), genotype fails to identify a large proportion of patients on maintenance DAPT with HPR. Since both HPR and CYP2C19 genotype are imperfect correlates of each other and both are predictors of poorer cardiovascular outcomes, the two together may provide complementary information to stratify cardiovascular event risk in patients on DAPT than either alone. Larger and longer-term prospective studies that also include cardiovascular event outcomes will be necessary to optimize predictive algorithms that may include genetic and/or platelet function testing, and their use to individualize P2Y12 inhibitor therapy.
Table 4.
HPR Status Based on 5uM and 20 uM ADP-Induced Platelet Aggregation in CYP2C19*2 and CYP2C19*17 Carriers and Non-Carriers.
| 5uM ADP-induced Aggregation | 20uM ADP-induced Aggregation | |||
|---|---|---|---|---|
| HPR Positive n=27 |
HPR Negative n=91 |
HPR Negative n=40 |
HPR Negative n=78 |
|
|
CYP2C19*2 Carriers n=41 |
N=15 | N=26 | N=20 | N=21 |
|
CYP2C19*2 Non-Carriers n=77 |
N=12 | N=65 | N=20 | N=57 |
|
CYP2C19*17 Carriers n=45 |
N=8 | N=37 | N=9 | N=36 |
|
CYP2C19*17 Non-Carriers n=73 |
N=19 | N=54 | N=31 | N=42 |
Acknowledgments
Grant Support:
Dr. Paul A Gurbel has received research grants and honoraria from Schering Plough, Haemoscope, Astra Zeneca, Medtronic, Lilly/Daiichi Sankyo, Sanofi-Aventis, Boston-Scientific and Bayer Healthcare, Portola Pharmaceuticals, Pozen. This work was supported by grants from the Sinai Hospital of Baltimore (PAG), and NIH U01 GM074518 (ARS).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures
The remaining authors report no conflicts.
REFERENCES
- 1.Gurbel PA, Tantry US. Selecting optimal antiplatelet therapy based on platelet function monitoring in patients with coronary artery disease. Curr Treat Options Cardiovasc Med. 2009;11:22–322. doi: 10.1007/s11936-009-0003-y. [DOI] [PubMed] [Google Scholar]
- 2.Kazui M, Nishiya Y, Ishizuka T, Hagihara K, Farid NA, Okazaki O, Ikeda T, Kurihara A. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos. 2010;38:92–99. doi: 10.1124/dmd.109.029132. [DOI] [PubMed] [Google Scholar]
- 3.de Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA. The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem. 1994;269:15419–15422. [PubMed] [Google Scholar]
- 4.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 5.Sibbing D, Stegherr J, Latz W, Koch W, Mehilli J, Dörrler K, Morath T, Schömig A, Kastrati A, von Beckerath N. Cytochrome P450 2C19 loss-of-function polymorphism and stent thrombosis following percutaneous coronary intervention. Eur Heart J. 2009;30:916–922. doi: 10.1093/eurheartj/ehp041. [DOI] [PubMed] [Google Scholar]
- 6.Trenk D, Hochholzer W, Fromm MF, Chialda LE, Pahl A, Valina CM, Stratz C, Schmiebusch P, Bestehorn HP, Büttner HJ, Neumann FJ. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008;51:1925–1934. doi: 10.1016/j.jacc.2007.12.056. [DOI] [PubMed] [Google Scholar]
- 7.Shuldiner AR, O’Connell, Bliden KP, Gandhi A, Ryan K, Horenstein RB, Damcott CM, Pakyz R, Gibson Q, Pollin TI, Post W, Parsa A, Mitchell BD, Faraday N, Herzog W, Tantry US, Gurbel PA. Cytochrome p450 2C19 genityoe is a major determinant of the anti-platelet effect and clinical efficacy of clopidogrel therapy. JAMA. 2009;302:849–857. doi: 10.1001/jama.2009.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gladding P, Webster M, Zeng I, Farrell H, Stewart J, Ruygrok P, Ormiston J, El-Jack S, Armstrong G, Kay P, Scott D, Gunes A, Dahl ML. The pharmacogenetics and pharmacodynamics of clopidogrel response: an analysis from the PRINC (Plavix Response in Coronary Intervention) trial. JACC Cardiovasc Interv. 2008;1:620–627. doi: 10.1016/j.jcin.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Gurbel PA, Antonino MJ, Tantry US. Recent developments in clopidogrel pharmacology and their relation to clinical outcomes. Expert Opin Drug Metab Toxicol. 2009;5:989–1004. doi: 10.1517/17425250903107772. [DOI] [PubMed] [Google Scholar]
- 10.Gurbel PA, Antonino MJ, Bliden KP, Dichiara J, Suarez TA, Singla A, Tantry US. Platelet reactivity to adenosine diphosphate and long-term ischemic event occurrence following percutaneous coronary intervention: a potential antiplatelet therapeutic target. Platelets. 2008;19:595–604. doi: 10.1080/09537100802351065. [DOI] [PubMed] [Google Scholar]
- 11.Fontana P, Hulot JS, De Moerloose P, Gaussem P. Influence of CYP2C19 and CYP3A4 gene polymorphisms on clopidogrel responsiveness in healthy subjects. J Thromb Haemost. 2007;10:2153–2155. doi: 10.1111/j.1538-7836.2007.02722.x. [DOI] [PubMed] [Google Scholar]
- 12.Frere C, Cuisset T, Morange PE, Quilici J, Camoin-Jau L, Saut N, Faille D, Lambert M, Juhan-Vague I, Bonnet JL, Alessi MC. Effect of cytochrome p450 polymorphisms ACCEPTED MANUSCRIPT on platelet reactivity after treatment with clopidogrel in acute coronary syndrome. Am J Cardiol. 2008;101:1088–1093. doi: 10.1016/j.amjcard.2007.11.065. [DOI] [PubMed] [Google Scholar]
- 13.Geisler T, Schaeffeler E, Dippon J, Winter S, Buse V, Bischofs C, Zuern C, Moerike K, Gawaz M, Schwab M. CYP2C19 and nongenetic factors predict poor responsiveness to clopidogrel loading dose after coronary stent implantation. Pharmacogenomics. 2008;9:1251–1259. doi: 10.2217/14622416.9.9.1251. [DOI] [PubMed] [Google Scholar]
- 14.Sibbing D, Koch W, Gebhard D, Schuster T, Braun S, Stegherr J, Morath T, Schomig A, von Beckerath N, Kastrati A. Cytochrome 2C19*17 allelic variant,platelet aggregation, bleeding events, and stent thrombosis in clopidogrel-treated patients with coronary stent placement. Circulation. 2010;121:512–518. doi: 10.1161/CIRCULATIONAHA.109.885194. [DOI] [PubMed] [Google Scholar]
- 15.Sibbing D, Gebhard D, Koch W, Braun S, Stegherr J, Morath T, von Beckerath N, Mehilli J, Schömig A, Schuster T, Kastrati A. Isolated and interactive impact of common CYP2C19 genetic variants on the antiplatelet effect of chronic clopidogrel therapy. J Thromb Haemost. 2010 May 21; doi: 10.1111/j.1538-7836.2010.03921.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Bonello L, Tantry US, Marcucci R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to ADP. J Am Coll Cardiol. 2010 doi: 10.1016/j.jacc.2010.04.047. In press. [DOI] [PubMed] [Google Scholar]
- 17.Hochholzer W, Trenk D, Fromm MF, Valina CM, Stratz C, Bestehorn HP, Büuttner HJ, Neumann FJ. Impact of cytochrome P450 2C19 loss-of-function polymorphism and of major demographic characteristics on residual platelet function after loading and maintenance treatment with clopidogrel in patients undergoing elective coronary stent placement. J Am Coll Cardiol. 2010;55:2427–2434. doi: 10.1016/j.jacc.2010.02.031. [DOI] [PubMed] [Google Scholar]
- 18.Gurbel PA, Tantry US, Shuldiner AR, Kereiakes DJ. Genotyping One Piece of the Puzzle to Personalize Antiplatelet Therapy. J Am Coll Cardiol. 2010;56:112–116. doi: 10.1016/j.jacc.2010.04.008. [DOI] [PubMed] [Google Scholar]