Abstract
Early onset pancreatic cancer (EOPC) constitutes less than 5% of all newly diagnosed cases of pancreatic cancer (PC). Although histopathological characteristics of EOPC have been described, no detailed reports on precursor lesions of EOPC are available. In the present study, we aimed to describe histopathological picture of extratumoral parenchyma in 23 cases of EOPCs (definition based on the threshold value of 45 years of age) with particular emphasis on two types of precursor lesions of PC: pancreatic intraepithelial neoplasia (PanIN) and intraductal papillary mucinous neoplasms (IPMNs). The types, grades, and densities of precursor lesions of PC were compared in patients with EOPCs, in young patients with neuroendocrine neoplasms (NENs), and in older (at the age of 46 or more) patients with PC. PanINs were found in 95.6% of cases of EOPCs. PanINs-3 were found in 39.1% of EOPC cases. Densities of all PanIN grades in EOPC cases were larger than in young patients with NENs. Density of PanINs-1A in EOPC cases was larger than in older patients with PC, but densities of PanINs of other grades were comparable. IPMN was found only in a single patient with EOPC but in 20% of older patients with PC. PanINs are the most prevalent precursor lesions of EOPC. IPMNs are rarely precursor lesions of EOPC. Relatively high density of low-grade PanINs-1 in extratumoral parenchyma of patients with EOPC may result from unknown multifocal genetic alterations in pancreatic tissue in patients with EOPCs.
Keywords: Pancreas, Pancreatic neoplasms, Pancreatic ductal carcinoma, Pancreatic ducts, Intraepithelial carcinoma
Introduction
Pancreatic cancer (PC) is one of the most frequent and most deadly abdominal cancers [1]. The mean age of patients diagnosed with PC of ductal origin (i.e., ductal adenocarcinoma) in the USA is 70.2 years (Surveillance, Epidemiology, and End Results database, 1988–2003) [2]. PC is a rare diagnosis in young patients. Early onset PC (EOPC, definition based on the threshold of 40, 45, or 50 years of age [3–9]) constitutes less than 5% of all newly diagnosed cases of PC [4, 6, 9]. Nowadays, it is clear that cancers in young patients need a specific management since they often differ in molecular, epidemiological, and therapeutic aspects from cancers in older population [10, 11]. Several groups of investigators studied the issue of EOPC [3, 4, 6–9, 12]. Inherited predisposition and smoking are believed to be the major EOPC risk factors [6]. Younger age of an individual patient at the PC onset may be a hallmark of so-called familial PC [13]. However, the mean age of patients with familial PC is less than 5 years younger than the mean age of patients with sporadic PC [13]. That is why only a small portion of patients with familial PC are diagnosed as EOPC [4]. Unfortunately, there are no sensitive nor specific clinical, histopathological, genomic, or proteomic features which could clearly distinguish EOPC from PC in older patients [3, 9].
Pancreatic intraepithelial neoplasia (PanIN) is a well-recognized and extensively studied precursor lesion of PC of ductal lineage [14–23]. PanINs may present as flat, micropapillary, or papillary noninvasive intraductal lesions, which usually develop within small pancreatic ducts (less than 5 mm [18–20] or less than 10 mm in diameter [15]). PanINs are divided into four categories based on grade of dysplasia (1A, 1B, 2, and 3) [15–18, 20, 21, 23]. Low-grade PanINs (PanINs-1A, PanINs-1B, PanINs-2) may be found in pancreata of 16–80% of individuals without any clinically detectable pancreatic disease. In contrast, PanINs-3 are very rarely seen in pancreata of individuals without PC [reviewed in Refs. 16, 17]. In a proportion of cases, PanINs (particularly low-grade ones) may be associated with obstruction of branch pancreatic ducts. This may lead to localized atrophy of pancreatic lobule [focal lobular atrophy (FLA)] drained by the affected duct and subsequent focal fibrosis of the pancreatic parenchyma [24]. Atrophy and fibrosis within areas of FLA are frequently associated with acinar–ductal metaplasia and formation of so-called tubular complexes. Tubular complexes may develop within atrophic lobules with or without associated PanIN within a draining duct. At the advanced stage of this process, mucinous metaplasia within ductules of tubular complexes may develop (mucinous tubular complexes) [25, 26]. It should be distinguished from PanIN (i.e., mucinous change within pre-existing duct) [27].
PanINs and FLAs are more frequent in older individuals, and therefore, they are believed to represent an age-related phenomenon [24, 28, 29]. However, PanIN–FLA complexes are particularly frequent in pancreata of individuals with a strong family history of PC [19, 26, 30]. This may be very useful for screening of persons with high risk of developing PC, since FLAs may be visualized by endoscopic ultrasonography [19, 26, 30–34].
Up to 20% of ductal PC (both sporadic and familial) are derived from other type of PC precursor lesions–intraductal papillary mucinous neoplasms (IPMNs) [19].
Rare reports on histopathological characteristics of EOPCs are available [3, 9]. In contrast, we are not aware of any detailed reports on precursor lesions of EOPC. Therefore, in the present study, we aimed to provide a histopathological description of extratumoral pancreatic parenchyma (EPP) in patients with EOPCs. We particularly emphasized morphological types of EOPC precursor lesions and their density in EPP.
Materials and methods
The study was performed in concordance with the Helsinki Declaration.
Study design and selection of cases
We reviewed retrospectively all cases of pancreatic resections received and diagnosed in our institution between January 1985 and December 2010. In all cases, available clinical data, gross pathology reports, as well as microscopic slides, were reexamined by two of the authors (LL and JP). Histopathological diagnoses were based on the criteria published in the U.S. Armed Forces Institute of Pathology Fascicle [35] and the recent World Health Organization reference book [36]. A minority (less than 10%) of cases were not available for rereview, and these cases were excluded from the study.
The main study group (EOPC cases)
The main study group included patients with pancreatic ductal adenocarcinoma diagnosed at the age of 45 and younger between 1985 and 2010. These patients were diagnosed as EOPCs. The age cut-off value we implemented here (45 years) was selected based on the largest so far study of patients with EOPC performed by Dr. Duffy and associates at Memorial Sloan Kettering Cancer Center, New York [4]. Patients with neoplasms of non-ductal origin [e.g., acinar cell carcinomas, neuroendocrine neoplasms (NENs), solid pseudopapillary neoplasms] were carefully excluded from the main study group. Cases of invasive carcinomas associated with mucinous cystic neoplasms were also excluded since their pathogenesis, demographic characteristics, and clinical presentation differ in significant extent from those of PCs [35, 36].
Control groups
For comparative purposes, we distinguished two control groups.
Control group 1 included cases of primary pancreatic NENs diagnosed in patients at the age of 45 or less between 1985 and 2010. That control group was established since it is highly probable that the prevalence of PC precursor lesions in patients with NENs represent their “baseline” prevalence in the general population. It was showed previously that the prevalence of PC precursor lesions in patients with NENs is primarily related to the patients’ age and/or presence of chronic pancreatitis [37, 38]. Moreover, there is no convincing evidence that NENs are related pathogenetically to PanINs/IPMNs [35].
Control group 2 included patients with pancreatic ductal adenocarcinoma diagnosed at the age of 46 or older in 2009 and 2010. That control group was established since we aimed to examine whether types and density of PC precursor lesions in patients with EOPC differ from PC precursor lesions in older patients. This could potentially indicate that PCs in younger and older patients differ in some aspects of their pathogenesis.
Data collection and histopathological examination
All available slides of cases of EOPCs and control groups were examined for the presence of EPP. Since in the present study we aimed to describe the characteristics of PC precursor lesions, we selected a subgroups of cases of EOPCs, NENs in young patients, and PCs in older patients in which at least 2 cm2 of EPP was found. In some specimens, smaller portions of EPP were available for review. In those cases, EPP was frequently localized in a very close proximity to the tumor border, and it showed usually changes compatible with mass-related atrophy and/or inflammation.
The main lesions which EPP was searched for were PanINs and IPMNs [15, 16]. In cases when the particular precursor lesion was less than 0.5 cm in diameter, it was classified as PanIN. When it was larger than 0.5 cm but smaller than 1 cm, it was called “incipient IPMN.” Larger lesions were named as IPMNs. These diagnostic categories were based on the previous study [19]. The grade of dysplasia within PanINs was assessed using internationally accepted criteria [18]. In cases of IPMNs/incipient IPMNs, grade of dysplasia (low grade, moderate grade, or high grade) as well as histopathological variant (gastric foveolar, intestinal, pancreatobiliary, oncocytic) was described [35, 39]. PanINs-3 and incipient IPMNs with high-grade dysplasia were classified as high-grade PC precursor lesions [19]. Reactive atypical epithelium, transitional/squamous cell metaplasia, as well as cancerization of ducts, were taken into account in differential diagnosis of PanINs/IPMNs and carefully excluded before establishing the PanINs/IPMNs diagnosis, based on previously proposed criteria [17, 18]. In particular, abrupt transition from highly dysplastic epithelium to the “normal” epithelium, continuity of dysplastic intraductal foci with invasive carcinoma, as well as flat rather than (micro) papillary configuration of the lesion, were considered as hallmarks of secondary colonization of pre-existing ducts by invasive carcinoma rather than the presence of primary non-invasive high-grade lesion, PanIN-3 [17, 18].
EPP was also searched for foci of FLA related to PanINs [24]. Acinar cell atrophy, islet aggregation, tubular complexes, small intralobular retention cysts, fatty change, as well intralobular fibrosis, are frequently seen in FLAs [19, 24–26, 28, 30, 40–42]. Additionally, a subcategory of FLA associated with mucinous tubular complexes was separately distinguished.
EPP areas were additionally studied for other lesions of ductal origin (squamous cell metaplasia, goblet cell metaplasia, oncocytic metaplasia, mucinous nonneoplastic cysts), acinar origin (acinar cell nodules), endocrine origin (endocrine-ductular/ductuloinsular lesions, NENs), and centroacinar/intercalated origin (squamoid cysts, centroacinar cell hyperplasia, microscopic serous cystic, or solid neoplasms) [27, 35, 42, 43]. Intensity of fibrosis was described semiquantitatively as mild, moderate, or marked. Moreover, histopathological features suggestive of acute pancreatitis were documented if present [44].
Data analysis and statistics
In each case, duct profiles containing PC precursor lesions were counted. The EPP surface was measured directly on microscopical slides with the area rounded up to nearest 0.25 cm2. The densities of PC precursor lesions were calculated as a number of lesions per square centimeter of EPP (PanIN-1A density, PanIN-1B density, PanIN-2 density, PanIN-3 density, overall PanIN density, low-grade incipient IPMN density, moderate-grade incipient IPMN density, high-grade incipient IPMN density, overall incipient IPMN density, overall PC precursor density, overall high-grade PC precursor density) [19]. PanINs and IPMNs visualized in the main pancreatic duct were documented but not included in the above counts.
Additionally, in each case, the proportion of PanINs associated with FLAs among all PanIN lesions (FLA to PanIN rate) and the proportion of PanINs associated with FLAs with mucinous tubular complexes among all PanIN lesions (rate of mucinous tubular complexes to PanINs) were calculated.
Medians of densities of PC precursor lesions, FLA-related rates, and patients’ age were compared between the main study group and control groups using Mann–Whitney U tests. Proportions were compared between study groups using Fisher’s exact tests. The statistical relationship between patients’ age and PanINs’ densities was assessed using the Spearman’s rank correlation coefficient. All statistical tests were two-tailed. Significance was set up at p ≤ 0.05.
Results
Basic clinical and histopathological characteristics of EOPCs and control cases
We selected only these resected cases of EOPCs, NENs in young patients, and PCs in older patients, in which adequate EPP area (at least 2 cm2) could be examined. Therefore, the study included 23 out of 26 EOPC cases, 13 out of 22 NEN cases in young patients (the two additional enucleated tumors not taken into account), and 41 out of 44 PCs in older patients.
Two cases of PCs in older patients were then excluded since they were associated with intraductal tubulopapillary neoplasms [36]. At the moment, it is not clear whether intraductal tubulopapillary neoplasms represent a morphological variant of IPMNs or rather separate intraductal pancreatic lesions of separate origin and/or differentiation.
Basic clinical and histopathological characteristics of cases included in the present study were presented in Table 1. A single EOPC case was diagnosed as familial PC—the two first-degree relatives of that patient were affected with PC. Another EOPC patient had a family history of a single case of PC. Another EOPC patient had a family history of multiple cancers of different types and locations. There was no family history of PC in young patients with NENs. Two patients with PC older than 45 years had a first-degree relative with PC. Another two patients with PCs at the age above 45 years had a family history of several PC cases, but no case was diagnosed in first-degree relatives. No family history of three patients with PC at the age above 45 years was available. None of the patients or their family kindred in the main study group and in the control groups was diagnosed with hereditary syndromes associated in an increased risk of developing PC.
Table 1.
Basic clinical and histopathological characteristics of patients with EOPCs and patients in control groups 1–2
| Variable | Main study group: EOPCs (n = 23) | Control group 1: NENs of the pancreas in young patients (n = 13) | Control group 2: Ductal pancreatic adenocarcinomas in older patients (n = 39) |
|---|---|---|---|
| Gender (male/female) | 13:10 | 7:6 | 23:16 |
| Age (median, interquartile range) | 42.0 (40.0–44.0)a | 36.0 (35.0–44.0)a | 60.0 (55.0–66.0) |
| Localization (head/body/tail/more than 1 segment/not known) | 18:0:2:3:0 | 5:1:6:0:1 | 37:0:1:1:0 |
| Tumor characteristics | 21 cases of conventional ductal adenocarcinoma, a single case of undifferentiated carcinoma, a single case of invasive carcinoma associated with IPMN (colloid carcinoma) | 12 cases of neuroendocrine tumors G1/G2, a single case of (poorly differentiated) neuroendocrine carcinoma | 30 cases of conventional ductal adenocarcinoma, a single case of undifferentiated carcinoma, eight cases of invasive carcinoma associated with IPMN (six of tubular differentiation and two of colloid differentiation) |
EOPC Early onset pancreatic cancer; NEN neuroendocrine neoplasm; IPMN intraductal papillary mucinous neoplasm
aMedian age of patients with EOPCs versus median age of young patients with NENs, Mann–Whitney U test, p = 0.087
The median value of age of patients with EOPC was 6.0 years higher than the median value of age of young patients with NENs (Mann–Whitney U test, p = 0.087, Table 1). Lack of (statistical) significance concerning that comparison might result from relatively small numbers of patients included, but we believe that difference was of no “clinical” significance. Previously reported PanIN prevalence rates in individuals in their 30s and 40s seemed to be comparable [23, 29]. It is not known, however, whether densities of PC precursor lesions in individuals in their 30s and 40s are the same.
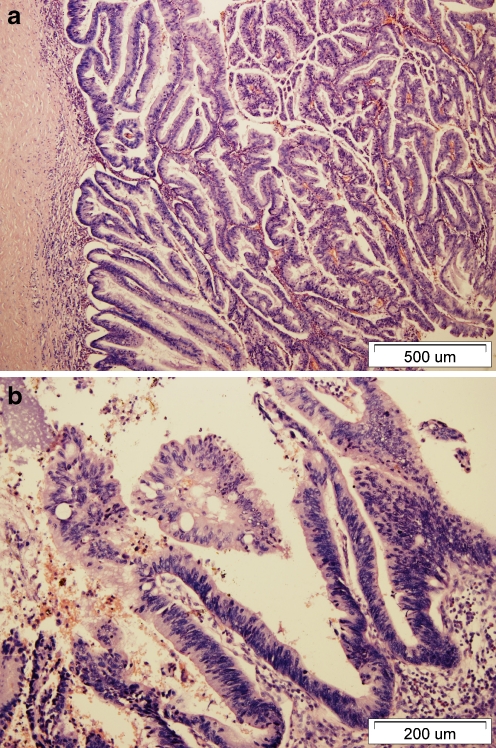
Only 1 out of 23 EOPC cases (4.4%) was derived from IPMN. That was colloid carcinoma [45] associated with intestinal type IPMN with moderate and focally high-grade dysplasia present within the main pancreatic duct and additionally in a branch duct. In contrast, 8 out of 39 (20.5%) studied cases of PC in older patients were associated with IPMNs. That difference was of no statistical (Fisher’s exact test, p = 0.136) but possibly of clinical significance. Among older patients with PCs, two cases of colloid carcinomas were associated with intestinal type IPMNs, three cases of tubular carcinomas were associated with pancreaticobiliary-type IPMNs (one with focal oncocytic differentiation), two cases of tubular carcinomas were associated with gastric foveolar-type IPMNs and a single case of tubular carcinoma was associated with IPMN of mixed differentiation. All cases were present in main pancreatic ducts and in some proportion of branch ducts. The detailed data on clinical–pathological characteristics of all EOPC cases are to be described in a separate manuscript (in preparation).
EPP in patients with EOPCs (main study group)
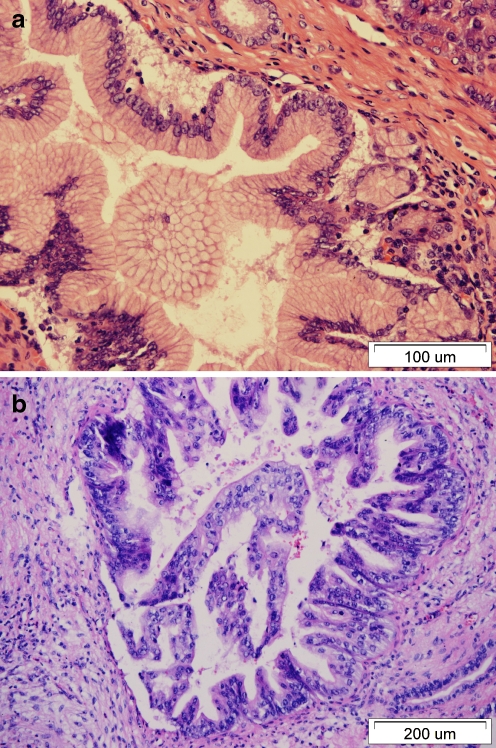
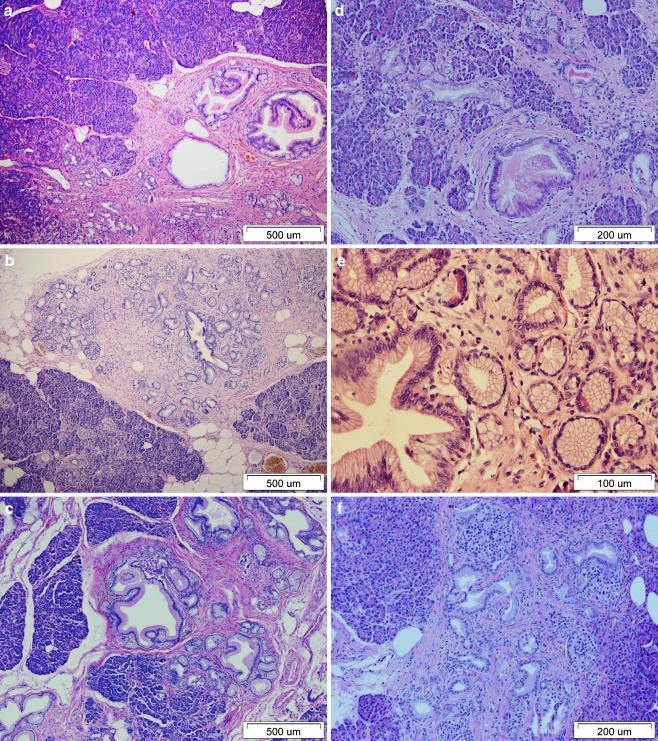
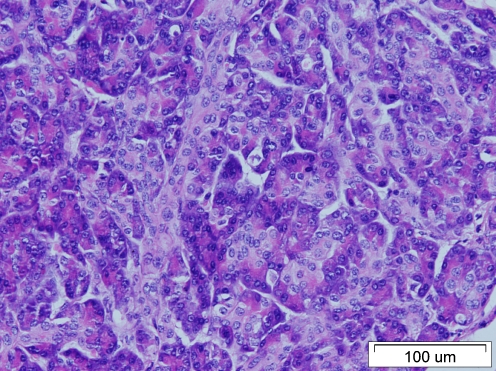
Among 23 studied patients, PanINs (Fig. 1a–b) were found in 22 (95.6%) of them. PanINs-3 were found in nine (39.1%) cases. The overall PanIN density ranged from 0.0 to 2.00 lesions cm−2 of EPP. The PanIN-3 density ranged from 0.0 to 0.60 lesions cm−2 of EPP. As mentioned earlier, a single PC developed from IPMN (Fig. 2a–b). IPMNs or incipient IPMNs were not found in any other EOPC cases. FLAs (Fig. 3a–f) were present in 13 cases (from one to five lesions per case); in seven of them, they showed features of mucinous tubular complexes. The FLA to PanIN rate ranged from 0.0 to 0.66, whereas the rate of mucinous tubular complexes to PanINs ranged from 0.0 to 0.33. Two patients showed features of moderate to marked chronic obstructive pancreatitis. Fat necrosis was seen focally in six cases. Amyloid deposits in islets, small oligocystic serous adenoma, PanIN-1A within the main pancreatic duct (not included in the above counts) were present in one case each. In one patient, there was a neuroendocrine tumor G1 coexistent with PC. In EPP of a single case, diffuse centroacinar cell hyperplasia (Fig. 4), but no PanINs were found. The significance of this finding remained unknown. In several cases, invasive carcinoma secondarily involved pre-existing ducts (Fig. 5a–b).
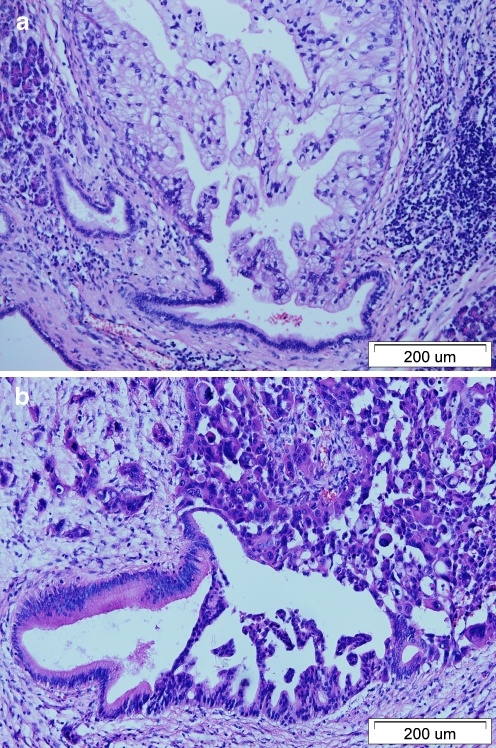
Fig. 1.
a–b PanIN in patients with EOPCs. a PanIN-1B. b PanIN-3 (micropapillary pattern)
Fig. 2.
a–b IPMN in patient with EOPC. That was intestinal type neoplasm within the main pancreatic duct and branch ducts which progressed to colloid (mucinous noncystic) carcinoma (not shown)
Fig. 3.
a–f FLA related to low-grade PanIN in patients with EOPCs. Intralobular fibrosis, acinar dropout, “naked” islets, ductules with mucinous metaplasia (mucinous tubular complexes). In some tubular complexes, residual acinar cells intermixed with mucin-rich metaplastic cells (d, e). Mucinous tubular complexes in close proximity to residual islets (f)
Fig. 4.
Centroacinar cell hyperplasia
Fig. 5.
a–b Secondary cancerization of pre-existing ducts by invasive carcinoma. Conventional ductal adenocarcinoma with abundant intracellular mucin involving normal branch duct (a) and undifferentiated carcinoma (b) involving branch duct with PanIN-1A (all figures in hematoxylin and eosin)
EPP in young patients with NENs (control group 1)
Among the 13 NENs studied, PanINs were found in eight cases. PanIN-1A lesions in the main pancreatic ducts were found in two additional cases. In a single patient, ductules with PanINs-1A were entrapped within tumor mass (so-called ductuloinsular neuroendocrine tumor). Incipient IPMNs and high-grade PC precursor lesions were absent. FLAs associated with PanINs were present in seven cases. In four of these cases, mucinous tubular complexes were found. In one patient, mucinous nonneoplastic cyst, amyloid islet depositions as well as islet microadenomatosis were found. In another patient, a small squamoid cyst was found. Focus of fat necrosis and focal squamous cell metaplasia of branch pancreatic duct were found in one case each. Features of moderate chronic pancreatitis were present in two cases. A single patient showed histopathological features of groove (paraduodenal) pancreatitis with duodenal intramural cyst.
EPP in older patients with PC (control group 2)
PanINs were found in all 39 cases studied. PanINs-3 were visualized in 30 (76.9%) out of 39 cases. The figures concerning PanIN prevalence in older patients obviously cannot be compared to the parallel values in EOPC group since the studied EPP areas in both groups did evidently differ. The overall PanIN density ranged from 0.21 to 1.89 lesions cm−2 of EPP. The PanIN-3 density ranged from 0.0 to 0.44 lesions cm−2 of EPP. As mentioned earlier, eight cases were associated with IPMNs. Incipient IPMNs were found in branch ducts of all of these eight patients, but they presented different grades of dysplasia, morphological types, and extent of EPP involvement. A single incipient IPMN of low-grade dysplasia and gastric foveolar differentiation was found in the EPP area peripheral to the invasive lesion in a single case of conventional PC related to the PanIN-3. The FLA to PanIN rate in older patients with PCs ranged from 0.0 to 0.79, whereas the rate of mucinous tubular complexes to PanINs ranged from 0.0 to 0.64. Twelve patients showed features of moderate to marked chronic obstructive pancreatitis. Fat necrosis was seen focally in seven cases. Pseudocysts were found in two cases. Squamous cell metaplasia of pancreatic dusts was seen in 11 cases; in two of them, it was extensively distributed in EPP. Neuroendocrine microadenomas were noticed in four patients (in one of them, two lesions were visualized). Squamoid cyst was found in a single patient. In another single patient, well-developed epithelioid granulomas with Langhans cells but without necrosis were found in EPP and in several peripancreatic lymph nodes. PanINs-1A, PanINs-1B, PanINs-2, and PanINs-3 in main pancreatic duct were found in 1, 3, 1, and 1 patient, respectively.
Comparison of densities of PC precursor lesions in patients with EOPCs and in young patients with NENs
Densities of PanINs of all grades were significantly larger in EPP of patients with EOPCs as compared to EPP of young patients with NENs (Table 2). However, there were no differences concerning the rate of FLAs to PanINs and the rate of mucinous tubular complexes to PanINs between those groups of patients.
Table 2.
PC precursor lesions in extratumoral parenchyma of patients with EOPCs and patients in control groups 1–2
| Variable | Main study group: EOPCs (n = 23) | Control group 1: NENs of the pancreas in young patients (n = 13) | Control group 2: ductal pancreatic adenocarcinomas in older patients (n = 39) |
|---|---|---|---|
| Studied area of EPP (cm2, median, IQR) | 6.0 (4.0–7.0) | 6.0 (4.0–9.5) | 19.0 (15.5–33.0) |
| Prevalence of PanINs-1A | 22/23 | 7/13 | 39/39 |
| Density of PanINs-1A (no. of lesions cm−2, median, IQR) | 0.40 (0.24–0.77) | 0.11 (0.0–0.21), p = 0.0001 a | 0.19 (0.12–0.27), p = 0.0002 b |
| Prevalence of PanINs-1B | 21/23 | 7/13 | 39/39 |
| Density of PanINs-1B (no. of lesions cm−2, median, IQR) | 0.34 (0.17–0.50) | 0.07 (0.0–0.21), p = 0.006 a | 0.26 (0.16–0.42), p = 0.536b |
| Prevalence of PanINs-2 | 15/23 | 0/13 | 37/39 |
| Density of PanINs-2 (no. of lesions cm−2, median, IQR) | 0.17 (0.0–0.25) | 0.0 (0.0–0.0), p = 0.0003 a | 0.12 (0.06–0.16), p = 0.683b |
| Prevalence of PanINs-3 | 9/23 | 0/13 | 30/39 |
| Density of PanINs-3 (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.17) | 0.0 (0.0–0.0), p = 0.012 a | 0.07 (0.02–0.12), p = 0.069b |
| Overall prevalence of PanINs | 22/23 | 8/13 | 39/39 |
| Overall density of PanINs (no. of lesions cm−2, median, IQR) | 1.20 (0.75–1.33) | 0.17 (0.0–0.42), p = 0.0001 a | 0.71 (0.47–1.04), p = 0.003 b |
| Prevalence of FLA | 13/23 | 7/13 | 38/39 |
| Rate of FLA to PanINs (median, IQR) | 0.17 (0.0–0.33) | 0.32 (0.21–1.0), p = 0.077 a | 0.29 (0.19–0.52), p = 0.018 b |
| Prevalence of mucinous tubular complexes | 7/23 | 4/13 | 28/39 |
| Rate of mucinous tubular complexes to PanINs (median, IQR) | 0.0 (0.0–0.13) | 0.1 (0.0–0.58), p = 0.135 a | 0.17 (0.0–0.28), p = 0.002 b |
| Prevalence of low-grade incipient IPMNs | 0/23 | 0/13 | 7/39 |
| Density of low-grade incipient IPMNs (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0), NA | 0.0 (0.0–0.0), p = 0.034 b |
| Prevalence of moderate-grade incipient IPMNs | 1/23 | 0/13 | 7/39 |
| Density of moderate-grade incipient IPMNs (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0), p = 0.488 | 0.0 (0.0–0.0), p = 0.154b |
| Prevalence of high-grade incipient IPMNs | 0/23 | 0/13 | 8/39 |
| Density of high-grade incipient IPMNs (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0), NA | 0.0 (0.0–0.0), p = 0.022 b |
| Overall prevalence of incipient IPMNs | 1/23 | 0/13 | 9/39 |
| Overall density of incipient IPMNs (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0), p = 0.488 | 0.0 (0.0–0.0), p = 0.059 b |
| Overall prevalence of precursor lesions of PC | 22/23 | 8/13 | 39/39 |
| Overall density of precursor lesions of PC (no. of lesions cm−2, median, IQR) | 1.20 (0.87–1.33) | 0.17 (0.0–0.42), p = 0.0001 a | 0.75 (0.48–1.08), p = 0.008 b |
| Overall prevalence of high-grade precursor lesions of PC | 9/23 | 0/13 | 32/39 |
| Overall density of high-grade precursor lesions of PC (no. of lesions cm−2, median, IQR) | 0.0 (0.0–0.17) | 0.0 (0.0–0.0), p = 0.012 a | 0.09 (0.05–0.18), p = 0.024 b |
EOPC Early onset pancreatic cancer, NEN neuroendocrine neoplasm, EPP extratumoral pancreatic parenchyma, IQR interquartile range, PanIN pancreatic intraepithelial neoplasia, FLA focal lobular atrophy, IPMN intraductal papillary mucinous neoplasm, NA not available (cannot be calculated), PC pancreatic cancer
aMedian values of studied variables in patients with EOPCs versus median values in young patients with NENs, Mann–Whitney U tests, statistically significant results are in bold
bMedian values of studied variables in patients with EOPCs versus median values in older patients with ductal pancreatic adenocarcinomas, Mann–Whitney U tests, statistically significant results are in bold
Comparison of densities of PC precursor lesions in patients with EOPCs and in older patients with PCs
Densities of PanINs-1B, PanINs-2, and PanINs-3 in EPP of patients with EOPCs and older patients with PCs were comparable (Table 2). In contrast, density of PanINs-1A was twofold larger in cases of EOPC than in older PC cases. This fact contributed to statistically significant difference of overall PanIN density between the main study group and control group 2. In contrast, rate of FLAs to PanINs and the rate of mucinous tubular complexes to PanINs were higher in older patients with PCs in comparison with patients with EOPCs. Since more cases of PC in older patients with PCs than cases of EOPC were related to IPMNs, it was not surprising that the densities of incipient IPMNs (except those of moderate grade) were higher in the former group. Overall density of PC precursor lesions was larger patients with EOPCs, but overall density of high-grade PC precursor lesions was higher in older patients with PCs.
Correlation between patients’ age and PanINs’ densities
We did not find significant correlations between patients’ age and overall PanIN density in EOPC patients and in young patients with NENs (Spearman’s rank correlation coefficients, p = 0.992 and p = 0.725, respectively). In contrast, overall PanIN density was rather weakly but significantly positively correlated with age of older patients with PC (r = 0.330, p = 0.040). Similar levels of correlation were found between age of older patients with PCs and their overall PC precursor density and overall high-grade PC precursor density, but not incipient IPMN density (specific data not shown).
Discussion
Pathogenesis and histopathology of EOPC
Due to its rarity, there is relatively small amount of data concerning epidemiology, symptomatology, optimal treatments options, as well as long-term prognosis in EOPC [3, 4, 6, 9]. Bergmann et al. [3] and Lüttges et al. [9] presented data on histopathology and molecular characteristics of EOPC. The pathogenesis of EOPC is poorly understood. Some PC cases including EOPC ones may be associated with individual genetic predisposition [46]. Noteworthy, the percentage of EOPC patients with positive family history of PC (10.3%) [4] is similar to the percentage in overall population of patients with PC (8.5%) [47]. Our data were in concordance with those observations. Interestingly, none of 136 EOPC cases in the study of Duffy et al. [4] and none of EOPC cases in the present study were associated with inherited syndromes associated with elevated risk of developing PC. Only a single patient with EOPC in the present study was diagnosed with familial PC. The issue of familial PC was extensively reviewed previously [33, 46, 48].
PanINs prevalence and densities
Several groups of investigators studied the prevalence of PC precursor lesions in patients without clinically detectable pancreatic diseases and/or patients with different types of tumors of non-ductal origin [21, 23, 29, 37, 38, 49–51].
PanINs are very frequent in adult pancreata (up to 80% of cases studied), but the prevalence rates of PanIN of different grades of dysplasia differ significantly [16, 21, 23, 29, 49, 50]. PanINs-1A lesions are more prevalent (19–68.2% [21, 49–51]) as compared to PanINs-1B (12–20% [23, 49–51]) and PanINs-2 lesions (0–13.6% [49–51]). PanINs-3 lesions are very rare [37] or nonexistent in patients without PC [21, 23, 49–51]. In our opinion, the differences between studies concerning PanIN prevalence rates in patients without PC may be caused by a number of methodological causes, e.g., different criteria of inclusion of patients across the studies, extensiveness of EPP sampling, or technique of statistical reporting.
Concerning the issue of PanIN prevalence in individuals without detectable pancreatic diseases, PanINs are more prevalent in older persons in comparison to younger ones (reviewed in Refs. [16, 17]). However, it is not definitely clear if the grade of PanINs found in asymptomatic individuals increases with their age, since results of different studies are discrepant [21, 29, 37, 49, 50]. Even if such a correlation exists, it is rather weak [37]. There is no significant difference between genders in the prevalence of PanINs [21, 23, 29, 50]. The PanIN prevalence is not associated with history of tobacco smoking [19, 23] or alcohol abuse [23]. Is it not definitely clear whether PanIN prevalence is higher in the pancreatic head in comparison to other segments [16], since results of studies on that issue were inconsistent [21, 23, 26, 29].
In the present study, we assumed that prevalence of PanINs in patients with NENs may be an indicator of their prevalence in individuals without pancreatic diseases. That was acknowledged by Stelow et al. [37] and, very recently, by Recavarren et al. [38]. However, the average age of patients with NENs included in those reports was above 45 years; that is, they were in significant proportion older than patients with NENs included in the present study. This may explain why we did not see PanINs-2 and PanINs-3 in patients with NENs despite they were seen (albeit rarely) in patients with NENs described in those reports [37, 38].
It is clear that PanIN-2 and PanIN-3 lesions are not supposed to be found in young patients without PCs (vide control group 1 in the present study), but they exist in patients with PCs (both younger and older ones). The PanINs-3 prevalence in patients with EOPCs in the present study was 39.1%. It was much lower than the PanINs-3 prevalence in older patients (76.9%, high-grade incipient IPMNs not included). That was obviously caused by differences in the studied EPP areas between those groups; therefore, it was of no significance.
Recently, it was proposed that not only prevalence of PanINs of different grades but also their density in EPP may be of clinical significance [19]. The issue of densities of PC precursor lesions was also raised in earlier studies [21, 23]. It is not known whether PanIN densities differ in young and older patients with or without PCs and whether PanIN density may change in a particular individual during his/her lifetime. Lüttges et al. [21] did not find any differences in numbers of intraductal lesions (compatible with present-day PanINs and squamous cell metaplasias) in systematically sampled pancreata of autopsied patients aged 6–92 who died of nonpancreatic diseases. This may indicate that PanIN density is relatively constant during lifetime in individuals who did not develop PC.
There is more data on PanIN density in patients with PCs. Shi et al. [19] showed that EPP in patients with familial PCs contained 2.75 times more PanINs than EPP in patients with sporadic PCs (PanIN densities of 1.51 and 0.55 lesions cm−2 of EPP, respectively). The densities of all grades of PanINs were higher in familial PCs than in sporadic cases. Incipient IPMNs were detected in EPP in one third of familial PC cases, and their density was 11.8 times higher in familial PC cases than in sporadic ones [19]. The densities on PanINs in older patients with PCs reported in the present study (control group 2) were comparable, but slightly higher to those reported by Shi et al. [19] in their sporadic PC cases.
The median overall PanIN density in EOPC cases examined in the present study (1.20 lesions cm−2) was significantly higher than PanIN density in older patients with PCs (0.75 lesions cm−2) and slightly lower than previously mentioned PanIN density in familial PC cases in the study of Shi et al. [19]. This finding was quite intriguing since only one patient with EOPC in the present study was diagnosed with familial PC. However, it should be noticed that significant differences in PanIN densities between particular patients with PCs may exist. Shi et al. [19] showed that overall PanIN densities in patients with familial PCs and sporadic PCs may range from 0 to 3.8 and from 0 to 2.01 lesions cm−2 of EPP, respectively. We also noticed differences in overall PanIN density ranging from 0 up to 2 lesions cm−2 in both young and older patients with PCs. However, in any of the studied patients the overall PanIN density was not as high as 3.8 lesions cm−2 of EPP.
We did not observe statistically significant differences concerning densities of PanINs-1B, PanINs-2, and PanINs-3 between patients with EOPCs and older patients with PCs. In contrast, the PanIN-1A density in patients with EOPCs was significantly higher than in older patients with PCs. We are not aware on any other studies on the relationship between PanIN-1A density and age of patients with PCs. It is possible that some PanIN-1A lesions may progress to PanINs-1B, and therefore, their density in older patients with PCs may decline. However, as mentioned earlier, we did not see any increase of PanIN-1B density in older patients with PCs as compared to younger ones. PanIN-1B density in older patients with PCs was even paradoxically lower than in patients with EOPCs, but that difference was not statistically significant. Lüttges et al. [21] showed that prevalence of mucinous cell hypertrophy (present-day PanINs-1A) but not ductal papillary hyperplasia (present-day PanINs-1B and PanINs-2) increased with age of individuals without PCs.
In the present study, we also showed that densities of PanIN of all grades (including low-grade ones) were significantly higher in patients with EOPCs than in young patients with NENs.
Higher PanINs-1A density in patients with EOPCs as compared to young patients with NENs and older patients with PCs may indicate that in at least some EOPC patients, there is a tendency to develop multifocal low-grade PanINs. Although a great majority of these low-grade lesions did not progress to high-grade ones and invasive carcinomas (we did not observe any multifocal cancers in any of the studied cases), their relatively high density might reflect an alteration of some “gatekeeper” genes similarly as it was postulated by Shi et al. [19] in familial PC.
IPMNs prevalence
In the present study, only one EOPC (4.3%) was associated with IPMN. In contrast, as many as 20% of cases of PCs in older patients were associated with IPMNs. That percentage was higher than the prevalence of invasive carcinomas associated with IPMNs among resected ductal PCs reported in the large series presented by Poultsides et al. [52] (132/1260, 10.5%). At present, IPMNs do not seem to be particularly frequent PC precursor lesion among patients with EOPCs, but further studies related to this issue are needed.
Focal lobular atrophy
Detlefsen et al. [24] and Kloppel et al. [28] showed that FLAs are frequent feature of pancreata of persons without clinically detectable pancreatic disorders. Interestingly, it may be often but not always associated with intraductal lesions mainly PanIN-1B. That seemed to be age-related phenomenon [24, 28]. Adenomatous hyperplasia of pancreatic ducts [21, 29], which probably equals to mucinous tubular complexes [25], was reported in 40% of “normal” pancreata and 26.9% of cases of normal pancreata with “ductal hyperplasia” [21, 29]. Changes compatible with FLA may be found in approximately one third of normal pancreata with ductal hyperplasia [29]. Meckler et al. [53] described in detail parenchymal changes in members of the family with many cases of PCs. They found FLAs with cystic transformation and “mucinous metaplasia” of the intralobular ductules, PanINs of all grades, interstitial endocrine cell hyperplasia, numerous endocrine cells within ductal epithelial lining, and nuclear atypia in some endocrine cells and rarely mild inflammatory infiltrate, squamous cell metaplasia [53]. Later Brune at al. [26] showed that similar lesions but of high density may be found in patients without clinically detectable PC but with strong family history of PC. These patients presented multiple foci of PanINs of all grades as well as IPMNs with low-grade dysplasia [26]. FLAs were related to almost all PanIN lesions including PanINs-1A [26]. Brune et al. [26] also documented less frequent FLAs associated with PanINs (including PanIN-1A) in patients without PCs. Moreover, PanIN-1B lesions may undergo “cystic transformation” to gastric foveolar IPMN [16]. FLA related to PC precursor lesions may be actually focal or multifocal response to pancreatic duct obstruction, since it closely resembles obstructive chronic pancreatitis [28]. It is possible to detect lobular fibrosis which is caused by obstruction of lobular duct by intraductal lesion using endoscopic ultrasonography [26, 30–34, 54]. In rare cases, multicentric PanINs with associated lobular atrophy and fibrosis involving the entire pancreas may develop in patients with negative family history of PC [55]. PanINs and IPMNs lesions with or without associated FLAs were also documented in patients from families with familial PCs submitted to prospective screening programs [30, 32, 33].
Related issue is the rate of FLAs to PanINs in patients with and without PCs. Detlefsen et al. [24] found FLA in one of four autopsied patients with PanIN-1B lesions under the age of 60 years without clinical or grossly detectable pancreatic disease. In patients at the age of 60 or older, PanIN-1B–FLA complexes were found in 25/31 (80.6%) of cases [24]. Shi et al. [19] showed that the prevalence rates of FLAs in both familial and sporadic PC cases is related to the frequency of PC precursor lesions and they were 86% and 53%, respectively. The fact that the prevalence of PanIN-1B–FLA complexes in autopsied persons without evident pancreatic diseases at the age of 60 or older in the study of Detlefsen et al. [24] was higher than the prevalence of FLA in patients with sporadic PCs in the study of Shi et al. [19] is quite intriguing. It indicates that some not yet known factors may influence results of studies on FLAs. The parenchymal changes compatible with FLA diagnosis may be of different stage [26] and extent and the FLA prevalence may be related to the “threshold” of features, which are identified as sufficient for the diagnosis of FLA. The FLA prevalence may be also related to extensiveness of EPP sampling. We found FLAs in as many as 38/39 (97.4%) of older patients with PCs. However, EPP was very extensively sampled, and we saw a correlation between EPP area and the number of FLAs in EPP of those patients (specific data not shown). FLA changes are also similar in pathogenesis and histopathology to obstructive pancreatitis [24, 28]. Such changes are more prevalent in the portion of pancreas distal to the tumor, which obstruct the duct. In the present study, we examined a low number of tumors (PCs and NENs) localized in the body or tail of the pancreas and therefore were not able to assess whether the localization of tumor influenced the prevalence of FLA.
In the present study, the rate of FLA to PanINs and the rate of FLA with mucinous tubular complexes to PanINs in patients with EOPCs did not differ from those in young patients with NENs, but they were significantly lower than in older patients with PCs. This may indicate that the increase of these rates represent an age-related phenomenon in patients with PCs, similarly to patients without PCs [24]. We observed statistically significant correlations between the rate of FLA to PanINs (r = 0.368, p = 0.003) and the rate of FLA with mucinous tubular complexes to PanINs (r = 0.509, p = 0.0001) versus age in all studied patients with PCs.
Other lesions in pancreatic parenchyma of EOPC and control cases
Lesions other than PanINs/IPMNs/FLAs found in EPP of cases studied in the present study did not seem to be related to the development of PC. Their prevalence rates were too low to be reliably compared between the study groups. Interestingly, we did not observe any cases of microscopic hyperplasia of endocrine component or exocrine-to-endocrine metaplasia, which may be related to the obstruction of pancreatic ducts and may represent a field effect in both ductal and endocrine component in patients at high risk of PC development or patients with familial PCs [31, 41, 53]. In one single patient with EOPC, a separate NEN was found, but the significance of that finding was unclear. The EPP in that patient did not show any features of endocrine cell hyperplasia or microadenomatosis.
Study limitations
The limitation of the study resulted from the fact that not all EPP present in the specimen was submitted to histopathological examination. Majority of EOPCs were sampled and diagnosed before we introduced protocols of very extensive sampling of pancreatectomy specimens [56]. This may explain why PanIN-3 density was (albeit not significantly) lower in patients with EOPCs in comparison with older patients with PCs. In some cases of EOPCs, the studied EPP area might be not large enough to detect PanINs-3.
Another limitation may be related to the presence of features of chronic pancreatitis in the studied cases since it may influence the prevalence of PC precursor lesions [23]. Moderate or marked features of chronic pancreatitis were present in a small proportion of patients with EOPCs and young patients with NENs but in 30% of older patients with PCs.
Surgical resection is possible only in a minority of patients with PCs. Since all EOPC cases described in the present study were resected, we cannot exclude that very aggressive cases of EOPCs (which are less likely to be resectable) show different types or extent of histopathological alterations in EPP.
Conclusion
PanINs is the most prevalent precursor lesion of EOPCs. PanINs of all grades are frequent but not the universal finding in EPP in patients with EOPCs. The density of all grades of PanINs in EPP is significantly higher in patients with EOPCs than in young patients with NENs. Density of PanINs-1A is higher in patients with EOPCs than in older patients with PCs, but densities of PanINs of other grades are comparable. Some of PanINs are related to FLAs with or without formation of mucinous tubular complexes. EOPCs less frequently than PCs in older patients are derived from IPMNs. Relatively high density of low-grade PanINs in EPP of patients with EOPCs as compared to young patients with NENs and older patients with PCs may result from unknown multifocal genetic alterations in pancreatic tissue of EOPC patients.
Acknowledgments
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA: A Cancer Journal for Clinicians. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Wisnoski NC, Townsend CM, Jr, Nealon WH, Freeman JL, Riall TS. 672 patients with acinar cell carcinoma of the pancreas: a population-based comparison to pancreatic adenocarcinoma. Surgery. 2008;144:141–148. doi: 10.1016/j.surg.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Bergmann F, Aulmann S, Wente MN, Penzel R, Esposito I, Kleeff J, Friess H, Schirmacher P. Molecular characterization of pancreatic ductal adenocarcinoma in patients under 40. J Clin Pathol. 2006;59:580–584. doi: 10.1136/jcp.2005.027292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duffy A, Capanu M, Allen P, Kurtz R, Olson SH, Ludwig E, Klimstra DS, O’Reilly EM. Pancreatic adenocarcinoma in a young patient population–12-year experience at Memorial Sloan Kettering Cancer Center. J Surg Oncol. 2009;100:8–12. doi: 10.1002/jso.21292. [DOI] [PubMed] [Google Scholar]
- 5.Baxter NN, Whitson BA, Tuttle TM. Trends in the treatment and outcome of pancreatic cancer in the United States. Ann Surg Oncol. 2007;14:1320–1326. doi: 10.1245/s10434-006-9249-8. [DOI] [PubMed] [Google Scholar]
- 6.Raimondi S, Maisonneuve P, Lohr JM, Lowenfels AB. Early onset pancreatic cancer: evidence of a major role of smoking and genetic factors. Canc Epidemiol Biomarkers Prev. 2007;16:1894–1897. doi: 10.1158/1055-9965.EPI-07-0341. [DOI] [PubMed] [Google Scholar]
- 7.Brune KA, Lau B, Palmisano E, Canto M, Goggins MG, Hruban RH, Klein AP. Importance of age of onset in pancreatic cancer kindreds. J Natl Cancer Inst. 2010;102:119–126. doi: 10.1093/jnci/djp466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soliman AS, El-Ghawalby N, Ezzat F, Bondy ML, Soultan A, Abdel-Wahab M, Fathy O, Ebidi G, Bassiouni N, El-Ghawalbi A, Levin B, Abbruzzese JL. Unusually high rate of young-onset pancreatic cancer in the East Nile Delta region of Egypt. Int J Gastrointest Cancer. 2002;32:143–151. doi: 10.1385/IJGC:32:2-3:143. [DOI] [PubMed] [Google Scholar]
- 9.Lüttges J, Stigge C, Pacena M, Klöppel G. Rare ductal adenocarcinoma of the pancreas in patients younger than age 40 years. Cancer. 2004;100:173–182. doi: 10.1002/cncr.11860. [DOI] [PubMed] [Google Scholar]
- 10.Bleyer A. Young adult oncology: the patients and their survival challenges. CA: A Cancer Journal for Clinicians. 2007;57:242–255. doi: 10.3322/canjclin.57.4.242. [DOI] [PubMed] [Google Scholar]
- 11.Bleyer A, Barr R, Hayes-Lattin B, Thomas D, Ellis C, Anderson B. Biology and clinical trials subgroups of the US National Cancer Institute progress review group in adolescent and young adult oncology. The distinctive biology of cancer in adolescents and young adults. Nat Rev Canc. 2008;8:288–298. doi: 10.1038/nrc2349. [DOI] [PubMed] [Google Scholar]
- 12.Zogopoulos G, Rothenmund H, Eppel A, Ash C, Akbari MR, Hedley D, Narod SA, Gallinger S. The P239S palladin variant does not account for a significant fraction of hereditary or early onset pancreas cancer. Hum Genet. 2007;121:635–637. doi: 10.1007/s00439-007-0361-z. [DOI] [PubMed] [Google Scholar]
- 13.James TA, Sheldon DG, Rajput A, Kuvshinoff BW, Javle MM, Nava HR, Smith JL, Gibbs JF. Risk factors associated with earlier age of onset in familial pancreatic carcinoma. Cancer. 2004;101:2722–2726. doi: 10.1002/cncr.20700. [DOI] [PubMed] [Google Scholar]
- 14.Hruban RH, Fukushima N. Pancreatic adenocarcinoma: update on the surgical pathology of carcinomas of ductal origin and PanINs. Mod Pathol. 2007;20:S61–S70. doi: 10.1038/modpathol.3800685. [DOI] [PubMed] [Google Scholar]
- 15.Singh M, Maitra A. Precursor lesions of pancreatic cancer: molecular pathology and clinical implications. Pancreatology. 2007;7:9–19. doi: 10.1159/000101873. [DOI] [PubMed] [Google Scholar]
- 16.Sipos B, Frank S, Gress T, Hahn S, Kloppel G. Pancreatic intraepithelial neoplasia revisited and updated. Pancreatology. 2009;9:45–54. doi: 10.1159/000178874. [DOI] [PubMed] [Google Scholar]
- 17.Andea AA, Basturk O, Adsay NV. Pancreatic intra-epithelial neoplasia: current clinicopathological and molecular considerations. Curr Diagn Pathol. 2005;11:80–94. doi: 10.1016/j.cdip.2004.11.008. [DOI] [Google Scholar]
- 18.Hruban RH, Takaori K, Klimstra DS, Adsay NV, Albores-Saavedra A, Biankin AV, Biankin SA, Compton CC, Fukushima N, Furukawa T, Goggins M, Kato Y, Kloppel G, Longnecker DS, Luttges J, Maitra A, Offerhaus GJA, Shimizu M, Yonezawa S. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28:977–987. doi: 10.1097/01.pas.0000126675.59108.80. [DOI] [PubMed] [Google Scholar]
- 19.Shi C, Klein AP, Goggins M, Maitra A, Canto M, Ali S, Schulick R, Palmisano E, Hruban RH. Increased prevalence of precursor lesions in familial pancreatic cancer patients. Clin Cancer Res. 2009;15:7737–7743. doi: 10.1158/1078-0432.CCR-09-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ottenhof NA, Milne AN, Morsink FH, Drillenburg P, Ten Kate FJ, Maitra A, Offerhaus GJ. Pancreatic intraepithelial neoplasia and pancreatic tumorigenesis: of mice and men. Arch Pathol Lab Med. 2009;133:375–381. doi: 10.5858/133.3.375. [DOI] [PubMed] [Google Scholar]
- 21.Lüttges J, Reinecke-Lüthge A, Möllmann B, Menke MA, Clemens A, Klimpfinger M, Sipos B, Klöppel G. Duct changes and K-ras mutations in the disease-free pancreas: analysis of type, age relation and spatial distribution. Virchows Arch. 1999;435:461–468. doi: 10.1007/s004280050428. [DOI] [PubMed] [Google Scholar]
- 22.Shi C, Hong SM, Lim P, Kamiyama H, Khan M, Anders RA, Goggins M, Hruban RH, Eshleman JR. KRAS2 mutations in human pancreatic acinar–ductal metaplastic lesions are limited to those with PanIN: implications for the human pancreatic cancer cell of origin. Mol Cancer Res. 2009;7:230–236. doi: 10.1158/1541-7786.MCR-08-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andea A, Sarkar F, Adsay VN. Clinicopathological correlates of pancreatic intraepithelial neoplasia: a comparative analysis of 82 cases with and 152 cases without pancreatic ductal adenocarcinoma. Mod Pathol. 2003;16:996–1006. doi: 10.1097/01.MP.0000087422.24733.62. [DOI] [PubMed] [Google Scholar]
- 24.Detlefsen S, Sipos B, Feyerabend B, Kloppel G. Pancreatic fibrosis associated with age and ductal papillary hyperplasia. Virchows Arch. 2005;447:800–805. doi: 10.1007/s00428-005-0032-1. [DOI] [PubMed] [Google Scholar]
- 25.Esposito I, Seiler C, Bergmann F, Kleeff J, Friess H, Schirmacher P. Hypothetical progression model of pancreatic cancer with origin in the centroacinar–acinar compartment. Pancreas. 2007;35:212–217. doi: 10.1097/mpa.0b013e31805d0190. [DOI] [PubMed] [Google Scholar]
- 26.Brune K, Abe T, Canto M, O’Malley L, Klein AP, Maitra A, Volkan Adsay N, Fishman EK, Cameron JL, Yeo CJ, Kern SE, Goggins M, Hruban RH. Multifocal neoplastic precursor lesions associated with lobular atrophy of the pancreas in patients having a strong family history of pancreatic cancer. Am J Surg Pathol. 2006;30:1067–1076. [PMC free article] [PubMed] [Google Scholar]
- 27.Hruban RH, Adsay NV, Albores-Saavedra J, Anver MR, Biankin AV, Boivin GP, Furth EE, Furukawa T, Klein A, Klimstra DS, Kloppel G, Lauwers GY, Longnecker DS, Luttges J, Maitra A, Offerhaus GJ, Pérez-Gallego L, Redston M, Tuveson DA. Pathology of genetically engineered mouse models of pancreatic exocrine cancer: consensus report and recommendations. Cancer Res. 2006;66:95–106. doi: 10.1158/0008-5472.CAN-05-2168. [DOI] [PubMed] [Google Scholar]
- 28.Kloppel G, Detlefsen S, Feyerabend B. Fibrosis of the pancreas: the initial tissue damage and the resulting pattern. Virchow Arch. 2004;445:1–8. doi: 10.1007/s00428-004-1021-5. [DOI] [PubMed] [Google Scholar]
- 29.Kozuka S, Sassa R, Taki T, Masamoto K, Nagasawa S, Saga S, Hasegawa K, Takeuchi M. Relation of pancreatic duct hyperplasia to carcinoma. Cancer. 1979;43:1418–1428. doi: 10.1002/1097-0142(197904)43:4<1418::AID-CNCR2820430431>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 30.Langer P, Kann PH, Fendrich V, Habbe N, Schneider M, Sina M, Slater EP, Heverhagen JT, Gress TM, Rothmund M, Bartsch DK. Five years of prospective screening of high-risk individuals from families with familial pancreatic cancer. Gut. 2009;58:1410–1418. doi: 10.1136/gut.2008.171611. [DOI] [PubMed] [Google Scholar]
- 31.Steinberg WM, Barkin JS, Bradley EL, III, DiMagno E, Layer P, Canto MI, Levy MJ. Should patients with a strong family history of pancreatic cancer be screened on a periodic basis for cancer of the pancreas? Pancreas. 2009;38:e137–e150. doi: 10.1097/MPA.0b013e3181a86b2c. [DOI] [PubMed] [Google Scholar]
- 32.Poley JW, Kluijt I, Gouma DJ, Harinck F, Wagner A, Aalfs C, van Eijck CH, Cats A, Kuipers EJ, Nio Y, Fockens P, Bruno MJ. The yield of first-time endoscopic ultrasonography in screening individuals at a high risk of developing pancreatic cancer. Am J Gastroenterol. 2009;104:2175–2181. doi: 10.1038/ajg.2009.276. [DOI] [PubMed] [Google Scholar]
- 33.Larghi A, Verna EC, Lecca PG, Costamagna G. Screening for pancreatic cancer in high-risk individuals: a call for endoscopic ultrasound. Clin Cancer Res. 2009;15:1907–1914. doi: 10.1158/1078-0432.CCR-08-1966. [DOI] [PubMed] [Google Scholar]
- 34.Canto MI, Goggins M, Hruban RH, Petersen GM, Giardiello FM, Yeo C, Fishman EK, Brune K, Axilbund J, Griffin C, Ali S, Richman J, Jagannath S, Kantsevoy SV, Kalloo AN. Screening for early pancreatic neoplasia in high-risk individuals: a prospective controlled study. Clin Gastroenterol Hepatol. 2006;4:766–781. doi: 10.1016/j.cgh.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Hruban RH, Pitman MB, Klimstra DS (2007) AFIP atlas of tumor pathology. Fourth series. Fascicle 6. Tumors of the pancreas. American Registry of Pathology–AFIP, Washington
- 36.Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. Lyon: International Agency for Research on Cancer; 2010. [Google Scholar]
- 37.Stelow EB, Adams RB, Moskaluk CA. The prevalence of pancreatic intraepithelial neoplasia in pancreata with uncommon types of primary neoplasms. Am J Surg Pathol. 2006;30:36–41. doi: 10.1097/01.pas.0000180440.41280.a5. [DOI] [PubMed] [Google Scholar]
- 38.Recavarren C, Labow DM, Liang J, Zhang L, Wong M, Zhu H, Wang J, Francis F, Xu R. Histologic characteristics of pancreatic intraepithelial neoplasia associated with different pancreatic lesions. Human Pathol. 2011;42:18–24. doi: 10.1016/j.humpath.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 39.Furukawa T, Kloppel G, Adsay NV, Albores-Saavedra J, Fukushima N, Horii A, Hruban RH, Kato Y, Klimstra DS, Longnecker DS, Lüttges J, Offerhaus GJ, Shimizu M, Sunamura M, Suriawinata A, Takaori K, Yonezawa S. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447:794–799. doi: 10.1007/s00428-005-0039-7. [DOI] [PubMed] [Google Scholar]
- 40.Kloppel G. Chronic pancreatitis of alcoholic and nonalcoholic origin. Semin Diagn Pathol. 2004;21:227–236. doi: 10.1053/j.semdp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 41.Lardon J, Bouwens L. Metaplasia in the pancreas. Differentiation. 2005;73:278–286. doi: 10.1111/j.1432-0436.2005.00030.x. [DOI] [PubMed] [Google Scholar]
- 42.Oertel JE. The pancreas. Nonneoplastic alterations. Am J Surg Pathol. 1989;13(Suppl 1):50–65. [PubMed] [Google Scholar]
- 43.Othman M, Basturk O, Groisman G, Krasinskas A, Adsay NV. Squamoid cyst of pancreatic ducts: a distinct type of cystic lesion in the pancreas. Am J Surg Pathol. 2007;31:291–297. doi: 10.1097/01.pas.0000213349.42143.ec. [DOI] [PubMed] [Google Scholar]
- 44.Kloppel G. Acute pancreatitis. Semin Diagn Pathol. 2004;21:221–226. doi: 10.1053/j.semdp.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 45.Liszka L, Pająk J, Zielińska-Pająk E, Gołka D. Colloid carcinoma of the pancreas: review of selected pathological and clinical aspects. Pathology. 2008;40:655–663. doi: 10.1080/00313020802436444. [DOI] [PubMed] [Google Scholar]
- 46.Jorgensen MT, Mortensen MB, Gerdes AM, De Muckadell OB. Familial pancreatic cancer. Scand J Gastroenterol. 2008;43:387–397. doi: 10.1080/00365520701775229. [DOI] [PubMed] [Google Scholar]
- 47.Hassan MM, Bondy ML, Wolff RA, Abbruzzese JL, Vauthey JN, Pisters PW, Evans DB, Khan R, Chou TH, Lenzi R, Jiao L, Li D. Risk factors for pancreatic cancer: case–control study. Am J Gastroenterol. 2007;102:2696–2707. doi: 10.1111/j.1572-0241.2007.01510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shi C, Hruban RH, Klein AP. Familial pancreatic cancer. Arch Pathol Lab Med. 2009;133:365–374. doi: 10.5858/133.3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosty C, Geradts J, Sato N, Wilentz RE, Roberts H, Sohn T, Cameron JL, Yeo CJ, Hruban RH, Goggins M. p16 inactivation in pancreatic intraepithelial neoplasias (PanINs) arising in patients with chronic pancreatitis. Am J Surg Pathol. 2003;27:1495–1501. doi: 10.1097/00000478-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 50.Ito R, Kondo F, Yamaguchi T, Kato K, Sakai Y, Saisho H, Yamazaki K. Pancreatic intraepithelial neoplasms in the normal appearing pancreas: on their relationship with age. Hepatogastroenterology. 2008;55:1103–1106. [PubMed] [Google Scholar]
- 51.Cubilla AL, Fitzgerald PJ. Morphological lesions associated with human primary invasive nonendocrine pancreas cancer. Cancer Res. 1976;36:2690–2698. [PubMed] [Google Scholar]
- 52.Poultsides GA, Reddy S, Cameron JL, Hruban RH, Pawlik TM, Ahuja N, Jain A, Edil BH, Iacobuzio-Donahue CA, Schulick RD, Wolfgang CL. Histopathologic basis for the favorable survival after resection of intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma of the pancreas. Ann Surg. 2010;251:470–476. doi: 10.1097/SLA.0b013e3181cf8a19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meckler KA, Brentnall TA, Haggitt RC, Crispin D, Byrd DR, Kimmey MB, Bronner MP. Familial fibrocystic pancreatic atrophy with endocrine cell hyperplasia and pancreatic carcinoma. Am J Surg Pathol. 2001;25:1047–1053. doi: 10.1097/00000478-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 54.Takaori K, Matsusue S, Fujikawa T, Kobashi Y, Ito T, Matsuo Y, Oishi H, Takeda H. Carcinoma in situ of the pancreas associated with localized fibrosis: a clue to early detection of neoplastic lesions arising from pancreatic ducts. Pancreas. 1998;17:102–105. doi: 10.1097/00006676-199807000-00015. [DOI] [PubMed] [Google Scholar]
- 55.Aimoto T, Uchida E, Nakamura Y, Matsushita A, Katsuno A, Chou K, Kawamoto M, Naito Z, Tajiri T. Multicentric pancreatic intraepithelial neoplasias (PanINs) presenting with the clinical features of chronic pancreatitis. J Hepatobiliary Pancreat Surg. 2008;15:549–553. doi: 10.1007/s00534-007-1269-7. [DOI] [PubMed] [Google Scholar]
- 56.Liszka L, Pajak J, Zielinska-Pajak E, Golka D, Mrowiec S, Lampe P. Different approaches to assessment of lymph nodes and surgical margin status in patients with ductal adenocarcinoma of the pancreas treated with pancreaticoduodenectomy. Pathology. 2010;42:138–146. doi: 10.3109/00313020903494060. [DOI] [PubMed] [Google Scholar]