Abstract
Artery of Percheron is a normal variant of the paramedian branches of posterior cerebral artery. This artery supplies the paramedian areas of the thalami and upper midbrain. Occlusion of this artery is rare and results in a multitude of neurological signs and symptoms, which might prompt the physician think of an aetiology other than vascular insults, and therefore change the management plan. The authors report two ischaemic strokes, which developed because of this arterial occlusion; their presentation differed from each other.
Background
Occlusion of the artery of Percheron is rare, and the resultant stroke picture is very variable, which might prompt the physician think of an inflammatory, infectious or malignant cause of this cerebral dysfunction. General physicians and neurologists should be familiar with this arterial ischemic stroke.
Case presentation
Case number 1
A 49-year-old diabetic man visited our Accident and Emergency (A&E) with a 1 h history of sudden and severe dizziness and gait instability. There was no vomiting. He was not hypertensive and his long-standing type II diabetes was well controlled with oral glibenclamaide. Within the next 2 h, the patient's consciousness gradually deteriorated and finally he became confused. There was complete left-sided ptosis and dilated pupil. The right planter was up-going. His 12-lead electrocardiogram (ECG) and echocardiography were normal. A non-contrast brain CT was unremarkable (figure 1), as the emergency physician said. A provisional diagnosis of upper brainstem stroke was made. One day later, the patient became comatose with a Glasgow Coma Scale of 3 and his limbs were flaccid with bilateral up-going planters. An urgent MRI with contrast was done (figures 2 and 3); abnormal signal intensity was found in the paramedian thalami and upper brainstem. The radiologist put a differential diagnosis of acute demyelinating encephalomyelitis (ADEM), toxoplasmosis and primary central nervous system (CNS) lymphoma. The patient's medications (aspirin, simvastatin and enalapril) were stopped. Serum toxoplasma antibodies and lumbar puncture were done; both were negative. The neurology department was consulted on day 3 of admission. After we examined the patient and skimmed the patient's brain CT scan and MRI films, we made a diagnosis of bilateral paramedian thalamic infarction and midbrain infarction; occlusion of the artery of Percheron was the most likely cause.
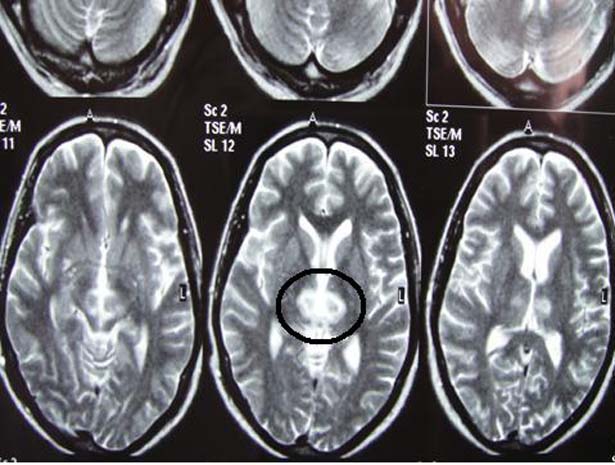
Figure 1.

Non-contrast brain CT of the patient in case number one, which was interpreted as normal by the emergency physician. Note the bilateral paramedian thalamic hypodensities (black arrows).
Figure 2.
Axial T2-weighted brain MRI of patient number one. There are hyperintense signal abnormalities in the paramedian thalami.
Figure 3.
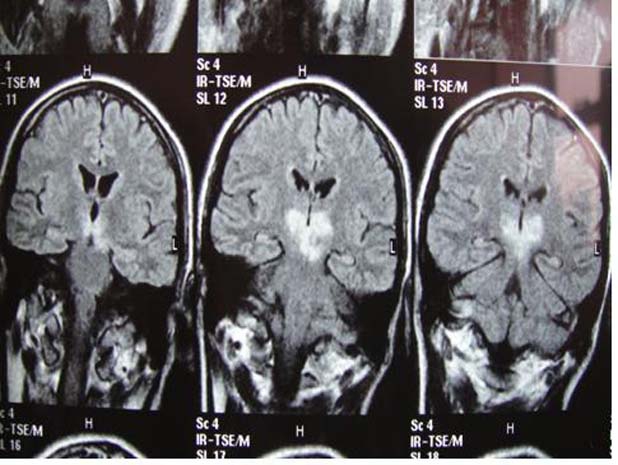
Coronal T2 FLAIR brain MRI of our first patient. Note the persistent hyperintense signal abnormality (which did not suppress on the FLAIR film) at the paramedian thalami and the left side of the rostral midbrain. The patient presented with acute thalamopeduncular syndrome.
Case number 2
A 16-year-old boy was brought to A&E 2 ½ h after developing sudden onset of drowsiness and agitation. There were no focal or lateralising neurological deficits. His brain CT scan was normal (figure 4). His blood tests were within the normal reference range and toxicology screen was negative. The boy's mother said that her son does not do drugs, as far as she knows. A differential diagnosis of conversion disorder and acute psychosis was made and the patient's family discharged him after staying 1 day in the psychiatry department. After 1 day of his hospital discharge, the patient became stuporous, rigid and unable to eat or drink. The patient's family re-visited the A&E. The patient was afebrile but no neck stiffness was present. The emergency physician treated him empirically as CNS infection; lumbar puncture was unremarkable, however. One day later, the patient became comatose but both planters were down. Neurological consultation was done. We ordered brain MRI (figures 5, 6). The radiologist suggested ADEM. We discussed the MRI films with another radiologist; a diagnosis of artery of Percheron occlusion was made. His 12-lead ECG, transoesophageal and transthoracic echocardiography and thrombophilia screen were unremarkable.
Figure 4.
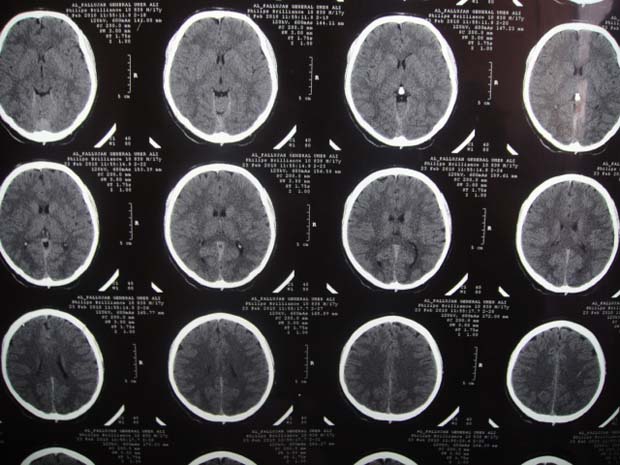
Brain CT scan with no contrast in patient number two at the time of admission. It was unremarkable.
Figure 5.
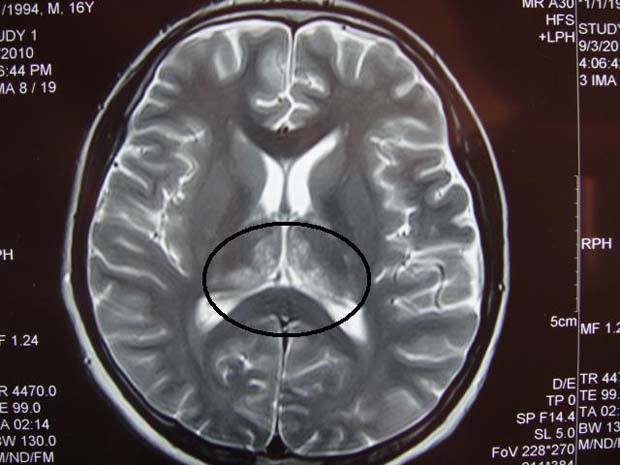
Axial T2-weighted brain MRI film of patient number two. Note the hyperintense signals at both paramedian thalami (within the black circle).
Figure 6.

Coronal T2 FLAIR brain MRI image of the patient in case number two. The hypersignal abnormalities are localised to both paramedian thalami; these signals were not suppressed on the FLAIR film (black arrows).
Treatment
Both patients were managed as ischemic stroke.
Outcome and follow-up
The first patient regained his consciousness gradually over 2 weeks to a degree of mild drowsiness. He demonstrated right-sided pyramidal weakness and up-planter and left oculomotor nerve palsy, a constellation that suggests midbrain Weber's syndrome. The patient was discharged from our neurology department after 3 weeks of his admission. One month later, he returned back for a scheduled visit. The patient was conscious and had grade 2 right-sided pyramidal weakness, and his left oculomotor nerve palsy was unchanged (figure 7).
Figure 7.

In response to our request, ‘raise your arms,’ the patient was able to lift up his left upper limb only. Note the left-sided complete ptosis.
The second patient's level of consciousness improved over 3 weeks. At that time, he was drowsy and had ‘catatonia.’ There was vertical gaze palsy, in addition. He was discharged from the neurology department 3 days later. We saw the patient after 2 weeks; he was still catatonic and unable to drink fluids or swallow solids. His planters were down.
Discussion
During the 70s of the past century, G Percheron, the French neurologist,1–3 published three papers describing the vascular anatomy of the posterior circulation, which supplies the human thalamus. According to Percheron, there are four variants of paramedian perforating arteries to the thalami (figure 8). In most people, these arteries arise from the proximal segments of both posterior cerebral arteries, on each side; this is type I variant. When paramedian penetrating arteries arise directly from the proximal segment of one of the posterior cerebral arteries, type IIa is found. However, in some people, a single arterial trunk stems off the P1 segment of one of the posterior cerebral arteries and this trunk then divides to supply both thalami and the upper midbrain (type IIb); this is the artery of Percheron. Type III is defined by the presence of a single arterial arc that links the proximal segments of both posterior cerebral arteries, and from this arc, the paramedian thalamic perforating arteries arise. Therefore, Percheron artery exemplifies the presence of a small single artery that supplies bilateral vital structures.
Figure 8.
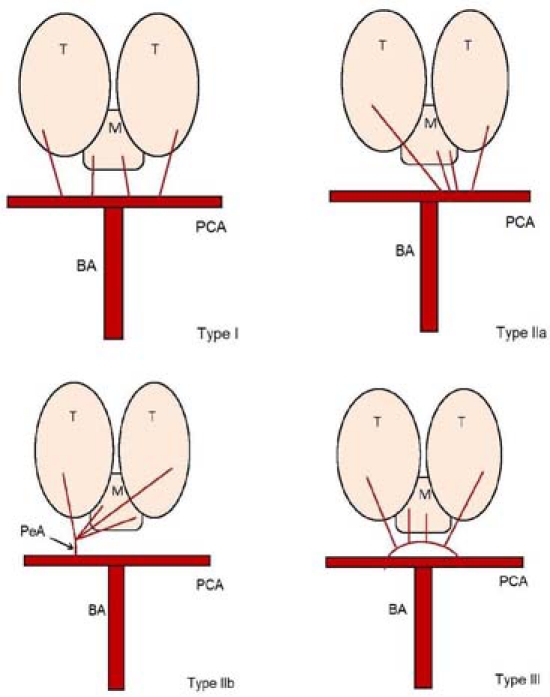
A diagram illustrating the four variants of the arterial supply to the human thalami and upper mesencephalon. Note that Percheron artery represents type IIb (T, thalamus; M, midbrain; PCA, posterior cerebral artery; BA, basilar artery; PeA, Percheron artery).
The complex anatomy and function of the human thalamus and its variable vascular supply are responsible for the protean clinical features when this structure is damaged by an ischemic infarction; in addition, the vascular overlap with the underlying midbrain will extend the spectrum of these clinical features to include midbrain signs.
Bogousslavsky and co-workers4 analysed 1000 consecutive patients with first stroke and found that isolated thalamic infarcts as a presenting feature comprised 11% of all strokes in the posterior circulation while midbrain ischemic infarctions constituted 7% only.
With respect to the prevalence of Percheron artery in the general population, the pertinent literature provides scarce information. Uz5 examined the brains of 15 cadavers; Percheron artery was found in one specimen only. To assess the incidence of bilateral thalamic strokes, Kumral and colleagues6 studied the registry of 2750 stroke patients; bithalamic infarctions occurred in 0.6% of their patients only. Saez and co-workers7 found that cigarette smoking was the most common risk factor for thalamic strokes in young patients, while in individuals older than 45 years, atherosclerosis-predisposing risk factors (of which, hypertension was the most common) were the usual culprits.
Lazzaro et al8 identified four patterns of ischemic infarctions when Percheron artery is occluded. They retrospectively reviewed the clinical presentation and imaging findings of 37 patients with arterial occlusion. Approximately, 43% of their patients demonstrated damage to both paramedian thalami and midbrain (this was the most common pattern), while 38% had ischemic damage to paramedian thalami only, without midbrain involvement. Around 14% of patients, the damage involved the anterior thalamic nuclei in addition to paramedian thalami and upper midbrain. The least common pattern (5%) was ischemic damage of bilateral paramedian and anterior thalami; the midbrain was spared here.
After analysing the medical literature (published from 1985 to 2006), Monet and co-workers9 concluded that the most common presenting features of bithalamic paramedian ischemic infarctions were vertical gaze palsy, memory impairment, confusion and coma.
The prognosis of thalamic infarctions is relatively good, when compared to thalamic haemorrhages.10 This also applies to paediatric cases.11
The sudden severe dizziness, gait instability and progressive deterioration in consciousness in patient number one suggested brainstem stroke. However, the initial brain CT scan of the patient showed hypodensity in both paramedian thalami, which was missed by the emergency physician. The subsequently done MRI revealed infarction in both paramedian thalami and the left half of the midbrain. The latter observation explains the Weber's syndrome–like presentation. This patient had the typical thalamopeduncular syndrome.12
The infarction in the second patient involved the paramedian thalami only. The patient presented with no weakness but rather with behavioural changes and later development of catatonia. The latter, although classically associated with schizophrenia, it rarely results from organic brain lesions such as bilateral thalamic or parietal lobe infarctions, or unilateral temporal lobe ischemic stroke.13
Although the presentation of the first patient was consistent with stroke, the treating physician changed the management plan after doing brain MRI. The age of the second patient and sudden behavioural changes pointed towards a psychotic disorder or brain infection; the brain MRI pictures prompted the physician think of an inflammatory demyelinating disease. Prior to his presentation, the patient was completely healthy; there was no explanation for this young patient's ischemic stroke.
Because of lack of expertise in our radiology department and the low yield of this investigation to capture Percheron artery, conventional cerebral angiography was not ordered. To date, through conventional angiography, only four authors were able to visualise this artery.8 14–16 Therefore, conventional cerebral angiography should not be done routinely in suspected cases of Percheron artery occlusion.
Artery of Percheron occlusion remains an uncommon event and the presenting features are highly variable. The initial brain CT scan may be totally unremarkable and brain MRI imaging shows abnormal signal intensities in the paramedian thalami with/without anterior thalamic or midbrain extension. The treating physician may think of infectious, inflammatory, demyelinating or functional aetiologies instead of vascular ones.
Learning points.
-
▶
Percheron artery is a normal variant of thalamic paramedian penetrating arteries, which arises from the P1 segment of one of the posterior cerebral arteries.
-
▶
Percheron artery occlusion results in bilateral paramedian thalamic infarctions with/without midbrain infarction. Additional involvement of the anterior thalamus is uncommon.
-
▶
Vertical gaze palsy, memory impairment, acute confusional state and coma are the commonest presenting features; although the overall clinical picture is highly variable.
-
▶
Brain MRI is the best imaging modality to delineate the damaged areas.
-
▶
Conventional cerebral angiography should not be used routinely to diagnose Percheron artery occlusion.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Percheron G. The anatomy of the arterial supply of the human thalamus and its use for the interpretation of the thalamic vascular pathology. Z Neurol 1973;205:1–13 [DOI] [PubMed] [Google Scholar]
- 2.Percheron G. Arteries of the human thalamus. I. Artery and polar thalamic territory of the posterior communicating artery. Rev Neurol (Paris) 1976;132:297–307 [PubMed] [Google Scholar]
- 3.Percheron G. Arteries of the human thalamus. II. Arteries and paramedian thalamic territory of the communicating basilar artery. Rev Neurol (Paris) 1976;132:309–24 [PubMed] [Google Scholar]
- 4.Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Registry: analysis of 1,000 consecutive patients with first stroke. Stroke 1988;19:1083–92 [DOI] [PubMed] [Google Scholar]
- 5.Uz A. Variations in the origin of the thalamoperforating arteries. J Clin Neurosci 2007;14:134–7 [DOI] [PubMed] [Google Scholar]
- 6.Kumral E, Evyapan D, Balkir K, et al. Bilateral thalamic infarction. Clinical, etiological and MRI correlates. Acta Neurol Scand 2001;103:35–42 [DOI] [PubMed] [Google Scholar]
- 7.Saez de Ocariz M, Nader J, Santos J, Bautista M. Thalamic vascular lesions. Risk factors and clinical course for infarcts and hemorrhages. Stroke 1996;27:1530–36 [DOI] [PubMed] [Google Scholar]
- 8.Lazzaro NA, Wright B, Castillo M, et al. Artery of Percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol 2010;31:1283–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monet P, Garcia PY, Saliou G, et al. Bithalamic infarct: is there an evocative aspect? Radioclinical study. Rev Neurol (Paris) 2009;165:178–84 [DOI] [PubMed] [Google Scholar]
- 10.Schmahmann JD. Vascular syndromes of the thalamus. Stroke 2003;34:2264–78 [DOI] [PubMed] [Google Scholar]
- 11.Garg BP, DeMyer WE. Ischemic thalamic infarction in children: clinical presentation, etiology, and outcome. Pediatr Neurol 1995;13:46–9 [DOI] [PubMed] [Google Scholar]
- 12.Waterston JA, Stark RJ, Gilligan BS. Paramedian thalamic and midbrain infarction: the ‘mesencephalothalamic syndrome’. Clin Exp Neurol 1987;24:45–53 [PubMed] [Google Scholar]
- 12.Williams DT. Delirium and catatonia. In: Martin A, Volkmar FR, Lewis M. Lewis's Child and Adolescent Psychiatry: A Comprehensive Textbook. Philadelphia, PA: Lippincott Williams & Wilkins; 2007;653 [Google Scholar]
- 14.Kostanian V, Cramer SC. Artery of Percheron thrombolysis. AJNR Am J Neuroradiol 2007;28:870–1 [PMC free article] [PubMed] [Google Scholar]
- 15.Weidauer S, Nichtweiss M, Zanella FE, et al. Assessment of paramedian thalamic infarcts: MR imaging, clinical features and prognosis. Eur Radiol 2004;14:1615–26 [DOI] [PubMed] [Google Scholar]
- 16.Roitberg BZ, Tuccar E, Alp MS. Bilateral paramedian thalamic infarct in the presence of an unpaired thalamic perforating artery. Acta Neurochir (Wien) 2002;144:301–4; discussion 304 [DOI] [PubMed] [Google Scholar]


