Abstract
Purpose
To assess whether black blood T2* cardiovascular magnetic resonance is superior to conventional white blood imaging of cardiac iron in patients with thalassaemia major (TM).
Materials and methods
We performed both conventional white blood and black blood T2* CMR sequences in 100 TM patients to determine intra and inter-observer variability and presence of artefacts. In 23 patients, 2 separate studies of both techniques were performed to assess interstudy reproducibility.
Results
Cardiac T2* values ranged from 4.5 to 43.8 ms. The mean T2* values were not different between black blood and white blood acquisitions (20.5 vs 21.6 ms, p = 0.26). Compared with the conventional white blood diastolic acquisition, the coefficient of variance of the black blood CMR technique was superior for intra-observer reproducibility (1.47% vs 4.23%, p < 0.001), inter-observer reproducibility (2.54% vs 4.50%, p < 0.001) and inter-study reproducibility (4.07% vs 8.42%, p = 0.001). Assessment of artefacts showed a superior score for black blood vs white blood scans (4.57 vs 4.25; p < 0.001).
Conclusions
Black blood T2* CMR has superior reproducibility and reduced imaging artefacts for the assessment of cardiac iron, in comparison with the conventional white blood technique, which make it the preferred technique for clinical practice.
Introduction
Beta thalassaemia major (TM) is an inherited anaemia and without regular blood transfusions patients die during childhood. Although transfusions improve health and survival, the consequent tissue iron deposition leads to organ damage in the long term. Those treated only with transfusions usually die early from cardiac failure secondary to myocardial siderosis [1,2], and therefore long term iron chelation treatment with deferoxamine became the standard treatment of choice to control iron levels from its introduction in the late 1960s. However, long term use of deferoxamine often does not prevent the eventual accumulation of myocardial iron, left ventricular dysfunction and death from heart failure. Although myocardial dysfunction is directly linked with cardiac iron burden [3], it often occurs late and can be hard to reverse once established. Therefore direct assessment and early treatment of iron loading is pivotal in the management of these patients, along with tailored cardiac chelation therapy which may reverse or prevent myocardial dysfunction [4,5]. Over the last decade, there has been a marked reduction in deaths attributable to tissue iron overload within the UK which coincides with the introduction of T2* cardiovascular magnetic resonance (CMR) as a diagnostic tool [6]. Life expectancy for patients in high income countries with good compliance to therapy is now over 50 years, although survival in low income areas is still poor [7].
The relaxation parameter T2* is shortened by field inhomogeneities induced by tissue iron. Gradient echo CMR can measure T2* decay, and a value of <20 ms is considered to be indicative of iron overload [8]. The first T2* sequence described was a multi breath-hold mid-ventricular short axis acquisition with end-diastolic gating [8]. A single breath-hold sequence was later developed which reduced scan time, improved image registration between images, and had good reproducibility [9]. This technique has become the mainstay of clinical evaluation and follow-up of TM patients. It has been installed on CMR scanners from different vendors at multiple sites throughout the world with reproducible results [10], and has been used to investigate the cardiac efficacy of chelating agents [11-13]. Despite this success, the white blood technique has some undesirable characteristics: the contrast between blood pool and myocardium may be suboptimal, and despite flow compensation, artefacts from motion and blood flow may compromise measurement accuracy. More recently, a double inversion recovery 'black blood' sequence has been reported which suppresses the blood signal, and a preliminary comparison with white blood T2* imaging suggested good reproducibility [14]. The aim of this study was therefore to compare the inter and intra-observer reproducibility between the established white blood sequence and the newer black blood sequence in a large group of patients, and to evaluate the interstudy reproducibility and artefacts when using the black blood sequence.
Materials and methods
We studied 100 TM patients to compare the black blood and white blood acquisitions. The cohort included 50 consecutive patients with cardiac siderosis (T2* <20 ms) and 50 consecutive patients with no cardiac iron (T2* > 20 ms) as measured using the conventional white blood T2* acquisition. Cardiac T2* values ranged from 4.5 to 43.8 ms across all patients. The age range was 11-50 years (mean 27) and 51% were female. All patients underwent both the conventional white blood and the new black blood T2* scan to test intra and inter-observer reproducibility. To test inter-study reproducibility, 23 patients with T2* values from 6.9 to 46.1 ms had a second scan for both black and white blood acquisitions on the same day.
All patients were scanned using a 1.5 T scanner (Siemens Sonata, Erlangen, Germany) with a 6 channel phased array cardiac receiver coil and ECG gating. A mid-ventricular short axis slice was obtained for all scans. The white blood acquisition used a multiecho gradient-echo sequence (flip angle 20°, matrix 128 × 256 pixels, sample bandwidth 810 Hz/pixel, slice thickness 10 mm and field of view 40 cm). The short axis images were acquired within a single breath-hold at 8 echo times from 2.54 to 17.90 ms at approximately 2 ms increments. For white blood diastolic imaging, the images were acquired immediately after the R-wave. For the black blood acquisitions, a double inversion recovery (DIR) pulse was applied on the R-wave and the inversion time extended into diastole, generating a similar set of 8 images at increasing echo times [14].
Image analysis was performed using Thalassaemia tools (a plug in of CMRtools, Cardiovascular Imaging Solutions, London, UK). A full thickness ROI incorporating the ventricular septum was selected avoiding blood pool and cardiac vessels [15,16]. T2* was derived by using an exponential curve fit, SI = SI0.exp-(TE/T2*), where SI is signal intensity, TE is the echo time and SI0 is a constant representing signal intensity at time zero. A truncation method was used to account for background noise at the longer echo times and improve curve fit[17], although this was not generally necessary for the black blood acquisitions (Figure 1). Analyses for all sequences were performed by two experienced investigators. Each data-set was anonymised and presented to observers in random order. Intra-observer reproducibility was assessed using 2 sets of measurements derived by observer 1. To test inter-observer reproducibility, the first read results were compared with those of observer 2. Inter-study reproducibility was assessed by observer 1 using data from the repeated studies. Analysis of image quality was conducted by 2 observers using the following 5 point scale: 0 - Very poor image quality with unusable images; 1 - Poor image quality, just able to make out the heart but a lot of artifact; 2 - Average image quality, not all of septum clearly seen and a lot of artifact; 3 - Good image quality with moderate septal artifact; 4 - Very good quality, with minimal septal artifacts; 5 - Excellent image quality with no significant septal artifact. To quantify the reproducibility, the coefficient of variance (CoV) was calculated from the standard deviation of the differences between analyses divided by their mean. A paired, two-tailed Student's t-test was performed on the natural log transformation of squared differences between methods to assess differences in measurement variability between methods [18]. Friedman's test was used to analyze the image quality scores. A p value of < 0.05 was considered significant. The local research ethics committee approved the study and patients gave informed consent.
Figure 1.
Signal decay is rapid in heavily iron loaded hearts causing the curve to plateau for the longer echo times. The upper frame shows how later points that fall below background noise level are removed to improve curve fit (red crosses) using the truncation method (R2= 0.9989 with truncation). For the black blood acquisition (b) background noise is reduced thus the curve fit is good for the full range of echo times without truncation (R2 = 0.9995) which reduces the likelihood of analysis errors.
Results
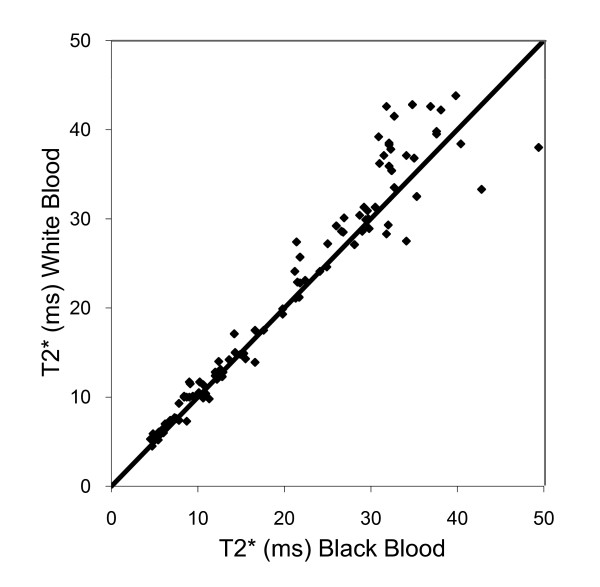
There was no significant difference between the mean cardiac T2* values for all 100 patients for the black blood acquisition and the conventional white blood sequence with diastolic imaging (20.5 ms vs 21.6 ms; p = 0.26). Differences between black and white blood acquisitions were also not significant for the iron loaded (n = 50, p = 0.31) and non-iron loaded (n = 50, p = 0.081) subgroups. The scatter plot of white blood vs black blood T2* showed the values lay close to the line of identity (Figure 2).
Figure 2.
Scatter plot of myocardial T2* values obtained from white blood and black blood acquisitions, showing the line of identity. Agreement is good for patients with T2* ≤ 20 (iron overloaded) but discrepancy increases with increasing T2*.
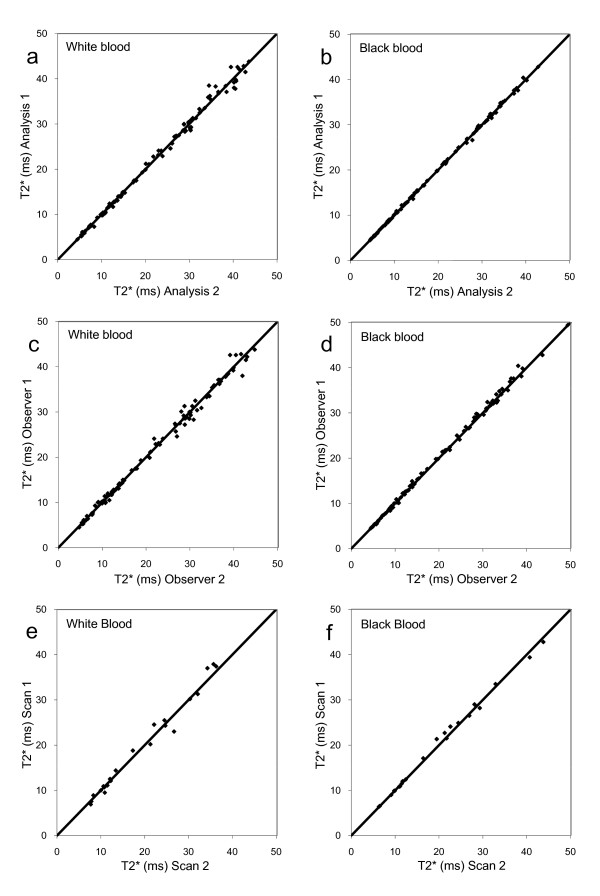
Intra and inter-observer reproducibility
The intra-observer coefficient of variability (CoV) across the full range of T2* values (n = 100) was significantly lower using the black blood compared with the white blood sequence (1.47% vs 4.23%, p < 0.001). In patients with iron overload (T2* <20 ms) the CoV was significantly lower for black blood than for white blood acquisition (1.68% vs 2.81%, p < 0.001). In patients with no iron overload (T2* >20 ms), the CoV was also significantly lower for black blood than white blood acquisition (1.28% vs 3.88%, p < 0.001). (Figure 3a, b). The inter-observer agreement findings were similarly superior for the black blood acquisition, with a CoV of 2.54% (black blood) compared with 4.50% (white blood) for all patients (p < 0.001), 2.91% vs. 4.28% for iron overloaded patients (p = 0.003) and 2.16% vs. 4.02% for patients with no iron loading (p = 0.03) (Figure 3c, d)
Figure 3.
Scatterplots of reproducibility data, in all cases showing the line of identity. a) White blood acquisition with scatter plots showing blinded intra-observer reproducibility for myocardial T2* assessment. b) Black blood data showing improved agreement between analyses. c) White blood acquisition with scatter plots showing blinded inter-observer reproducibility for myocardial T2* assessment. d) Black blood data showing improved agreement between analyses. e) White blood acquisition with scatter plots showing blinded inter-study reproducibility for myocardial T2* assessment. f) Black blood data showing improved agreement between analyses.
Inter-study reproducibility
For all patients (n = 23), the CoV for inter-study reproducibility was superior for black blood compared with white blood acquisition (4.07% vs 8.42%, p = 0.001). (Figure 3e, f) In patients with a T2* <20 ms (n = 12) the CoV was 2.21% for black blood and 7.04% for white blood (p = 0.003). In the patients with no iron loading (n = 11), the CoV was 3.93% and 7.87% respectively (p = 0.15).
Artefact scoring
The mean artefact score was superior for the black blood acquisition compared with white blood (4.57 vs 4.25, p < 0.001).
Discussion
In this study, we have shown improvement in intra and inter-observer variability together with inter-study reproducibility for black blood T2* imaging over the conventional white blood sequence in a large patient sample. For the conventional white blood sequence with no trigger delay, low signal contrast and the consequent difficulty in defining the myocardial/blood boundary may cause error in T2* measurement. This may result in white signal from the blood pool being incorporated into the decay curve for analysis. The errors may also be exacerbated by mis-registered, high signal blood pool artefacts which can be superimposed on the ROI. Adding the double inversion recovery pulse to generate the black blood images removes most of the blood signal (and hence artefacts) from the myocardium, making the measurement of T2* more robust. Importantly, the greatest disparity between white blood and black blood T2* values was seen when testing inter-study reproducibility in iron overloaded patients where we found a three-fold difference in the coefficient of variation. This discrepancy may be due to different levels of artefact in the myocardial septum resulting in changes in the overall signal intensity in the region of interest between scans. Indeed analysis of artefact scoring showed significantly poorer artefact scoring for the white blood acquisition which could potentially impart significant errors in longitudinal evaluation.
The improved analysis with reduced requirement for truncation of data points in patients with short T2* values (Figure 1), is an additional advantage in reducing analysis errors, particularly in less experienced centres. These findings combined with the improved reproducibility, suggest that the black blood technique should be used for routine clinical practice, providing centres can install a robust sequence as implemented by the scanner manufacturers. There are some disadvantages to the black blood acquisition however. Because of the time taken to achieve blood signal nulling, it is usually necessary to gate on alternate cardiac cycles, unless the RR interval is very long.
Conclusions
In conclusion, this study shows improved reproducibility and reduced artefacts for the black blood sequence in comparison with the previously validated white blood sequence, and therefore the black blood sequence should be considered the imaging technique of choice.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GCS carried out data acquisition and interpretation, statistical analysis, manuscript drafting and participated in study design. JPC and MHA performed additional data analysis. TH and DNF designed and optimised the CMR acquisition protocol. DJP was responsible for the initial study concept and the final manuscript. All authors read and approved the final manuscript.
This work was supported by the NIHR Cardiovascular Biomedical Research Unit of Royal Brompton Hospital and Imperial College. Dr He and Dr Alam are currently supported by the British Heart Foundation.
Contributor Information
Gillian C Smith, Email: g.smith@rbht.nhs.uk.
John Paul Carpenter, Email: j.carpenter@rbht.nhs.uk.
Taigang He, Email: t.he@imperial.ac.uk.
Mohammed H Alam, Email: m.alam@rbht.nhs.uk.
David N Firmin, Email: d.firmin@rbht.nhs.uk.
Dudley J Pennell, Email: d.pennell@imperial.ac.uk.
References
- Modell B, Letsky EA, Flynn DM, Peto R, Weatherall DJ. Survival and desferrioxamine in thalassaemia major. Br Med J. 1982;284:1081–4. doi: 10.1136/bmj.284.6322.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC, Romeo MA, Forni GL, Gamberini MR, Ghilardi R, Piga A, Cnaan A. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89:1187–93. [PubMed] [Google Scholar]
- Kirk P, Roughton M, Porter JB, Walker JM, Tanner MA, Patel J, Wu D, Taylor J, Westwood MA, Anderson LJ, Pennell DJL. Cardiac T2* magnetic resonance for prediction of cardiac complications in thalassemia major. Circulation. 2009;120:1961–8. doi: 10.1161/CIRCULATIONAHA.109.874487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe L, Olivieri N, Sallan D, Colan S, Rose V, Propper R, Freedman MH, Nathan DG. Prevention of cardiac disease by subcutaneous deferoxamine in patients with thalassemia major. N Engl J Med. 1985;312:1600–3. doi: 10.1056/NEJM198506203122503. [DOI] [PubMed] [Google Scholar]
- Brittenham GM, Griffith PM, Nienhuis AW, McLaren CE, Young NS, Tucker EE, Allen CJ, Farrell DE, Harris JW. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med. 1994;331:567–73. doi: 10.1056/NEJM199409013310902. [DOI] [PubMed] [Google Scholar]
- Modell B, Khan M, Darlison M, Westwood MA, Ingram D, Pennell DJ. Improved survival of thalassaemia major in the UK and relation to T2* cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2008;10:42. doi: 10.1186/1532-429X-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telfer P. Update on survival in thalassemia major. Hemoglobin. 2009;33:S76–80. doi: 10.3109/03630260903347336. [DOI] [PubMed] [Google Scholar]
- Anderson LJ, Holden S, Davis B, Prescott E, Charrier CC, Bunce NH, Firmin DN, Wonke B, Porter J, Walker JM, Pennell DJ. Cardiovascular T2-star (T2*) magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J. 2001;22:2171–9. doi: 10.1053/euhj.2001.2822. [DOI] [PubMed] [Google Scholar]
- Westwood M, Anderson LJ, Firmin DN, Gatehouse PD, Charrier CC, Wonke B, Pennell DJ. A single breath-hold multiecho T2* cardiovascular magnetic resonance technique for diagnosis of myocardial iron overload. J Magn Reson Imaging. 2003;18:33–9. doi: 10.1002/jmri.10332. [DOI] [PubMed] [Google Scholar]
- Kirk P, He T, Anderson LJ, Roughton M, Tanner MA, Lam WM, Au WY, Chu WC, Chan G, Galanello R, Matta G, Fogel M, Cohen AR, Tan RS, Chen K, Ng I, Lai A, Fucharoen S, Laothamatas J, Chuncharunee S, Firmin DN, Smith GS, Pennell DJ. International reproducibility of single breath-hold T2* magnetic resonance for cardiac and liver iron assessment among five thalassemia centers. J Magn Reson Imaging. 2010;32:315–9. doi: 10.1002/jmri.22245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennell DJ, Berdoukas V, Karagiorga M, Ladis V, Piga A, Aessopos A, Gotsis ED, Tanner MA, Smith GC, Westwood MA, Wonke B, Galanello R. Randomized controlled trial of deferiprone or deferoxamine in beta-thalassemia major patients with asymptomatic myocardial siderosis. Blood. 2006;107:3738–44. doi: 10.1182/blood-2005-07-2948. [DOI] [PubMed] [Google Scholar]
- Tanner MA, Galanello R, Dessi C, Smith GC, Westwood MA, Agus A, Roughton M, Assomull R, Nair SV, Walker JM, Pennell DJ. A randomized, placebo-controlled, double-blind trial of the effect of combined therapy with deferoxamine and deferiprone on myocardial iron in thalassemia major using cardiovascular magnetic resonance. Circulation. 2007;115:1876–84. doi: 10.1161/CIRCULATIONAHA.106.648790. [DOI] [PubMed] [Google Scholar]
- Pennell DJ, Porter JB, Cappellini MD, El-Beshlawy A, Chan LL, Aydinok Y, Elalfy MS, Sutcharitchan P, Li CK, Ibrahim H, Viprakasit V, Kattamis A, Smith G, Habr D, Domokos G, Roubert B, Taher A. Efficacy of deferasirox in reducing and preventing cardiac iron overload in beta-thalassemia. Blood. 2010;115:2364–71. doi: 10.1182/blood-2009-04-217455. [DOI] [PubMed] [Google Scholar]
- He T, Gatehouse PD, Kirk P, Tanner MA, Smith GC, Keegan J, Mohiaddin RH, Pennell DJ, Firmin DN. Black-blood T2* technique for myocardial iron measurement in thalassemia. J Magn Reson Imaging. 2007;25:1205–9. doi: 10.1002/jmri.20929. [DOI] [PubMed] [Google Scholar]
- Reeder SB, Faranesh AZ, Boxerman JL, McVeigh ER. In vivo measurement of T*2 and field inhomogeneity maps in the human heart at 1.5 T. Magn Reson Med. 1998;39:988–98. doi: 10.1002/mrm.1910390617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghugre NR, Enriquez CM, Coates TD, Nelson MD Jr, Wood JC. Improved R2* measurements in myocardial iron overload. J Magn Reson Imaging. 2006;23:9–16. doi: 10.1002/jmri.20467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He T, Gatehouse PD, Smith GC, Mohiaddin RH, Pennell DJ, Firmin DN. Myocardial T2* measurements in iron-overloaded thalassemia: An in vivo study to investigate optimal methods of quantification. Magn Reson Med. 2008;60:1082–9. doi: 10.1002/mrm.21744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon JC, Lorenz CH, Francis JM, Smith GC, Pennell DJ. Breath-Hold FLASH and FISP cardiovascular MR imaging: Left ventricular volume differences and reproducibility. Radiology. 2002;223:789–97. doi: 10.1148/radiol.2233011181. [DOI] [PubMed] [Google Scholar]