Abstract
Objectives
To evaluate efficacy of short term intranasal corticosteroid (mometasone furoate) treatment in pediatric sleep-disordered breathing (SDB) patients.
Methods
A prospective, observational study was done. A total of 41 children (2-11 years old) were enrolled into this study. All patients received 4-weeks course of mometasone furoate 100 µg/day treatment. They were evaluated at pretreatment and immediately after treatment with obstructive sleep apnea (OSA)-18 quality of life survey and lateral neck X-ray. Also, the assessment of each patients included history, skin prick test or CAP test, and sinus radiography. We compared the OSA-18 survey score and adenoidal-nasopharyngeal (AN) ratio between before and after treatment.
Results
Total OSA-18 score and AN ratio decreased significantly after treatment regardless of allergy, sinusitis, and obesity (P=0.003, P=0.006). There was no complication after treatment of mometasone furoate.
Conclusion
Pediatric SDB patients with adenoid hypertrophy could be effectively treated with 4-weeks course of mometasone furoate. Allergy, obesity, and sinusitis did not affect on the result of treatment.
Keywords: Steroid, Topical administration, Sleep disorder, Adenoid, Pediatrics, Allergy
INTRODUCTION
Sleep-disordered breathing (SDB) in childhood describes a spectrum of abnormalities ranging from primary snoring to obstructive sleep apnea syndrome (OSAS). Chronic sleep-related airway obstruction results in repetitive hypoxemia and sleep disturbance that can cause neurocognitive disturbance, growth failure, and cor pulmonale (1).
The most common symptoms associated with this disorder are habitual snoring, difficulty breathing, witnessed apneas, restless sleep, and daytime neurobehavioral problems (2). Frequent snoring was observed at 3.2% and occasionally at 16.7% in an epidemiological study (3). Sleep apnea has been reported at between 1% and 3% of children and occurs most frequently in children between 2 and 6 years old (4). Pediatric SDB is usually managed with adenotonsillectomy which needs general anesthesia and sometimes is associated with complication including bleeding and perioperative respiratory compromise. As adjunctive treatments, nonsurgical alternatives for reduction of adenoid size are limited. However, recent studies showed that topical nasal corticosteroid spray reduced adenoid size and improved symptoms of nasal airway obstruction and OSAS (1, 2). Topical nasal corticosteroid spray is considered to be the first line treatment for allergic rhinitis which is also associated with sleep disturbance through nasal obstruction, enlargement of tonsils and adenoids, and an elongated face (5, 6). However, there are few results which show its effect in the SDB children irrespective of allergic rhinitis, sinusitis and body weight.
This study was aimed to evaluate the efficacy of short term mometasone furoate in pediatric SDB patients with parental questionnaire (obstructive sleep apnea-18, OSA-18) and lateral neck X-ray and to identify the effect of allergy, sinusitis, and obesity on treatment result.
MATERIALS AND METHODS
Study population
This prospective, observational study was approved by the Institutional Review Board of the Samsung Medical Center. Forty one (32 males, 9 females), two to eleven year-old children, who visited otolaryngology clinic due to sleep disordered breathing were recruited between March 2006-July 2007, based on the following inclusion criteria: 1) history of habitual snoring for the last 3 months or longer, and 2) adenoid hypertrophy confirmed with simple X-ray findings or endoscopic examination by otolaryngologist. Children were excluded from the study if they met any of the exclusion criteria: 1) presence of symptoms of acute respiratory infection; 2) use of nasal or systemic corticosteroid or antibiotics within 4 weeks prior to the study; 3) prior tonsil or adenoid surgery; and 4) a history of craniofacial, neuromuscular, or genetic disorders.
Diagnostic criteria and method
Informed consent for participation in this study was obtained from the parent or legal guardian of each child enrolled. Initial assessment of each patient upon entering the study included the following: history and physical examination (including body weight and height), parental questionnaire (OSA-18), sinus X-ray, adenoid X-ray, and skin prick test or Pharmacia CAP system for detecting allergy. Allergic rhinitis was diagnosed in case that each child complaining typical allergic symptoms showed positive result in allergic test.
We checked paranasal sinus X-ray for detecting the presence of sinusitis and categorized into three group: no evidence of sinusitis, unilateral haziness, and bilateral haziness. For the evaluation of obesity, body weight was checked and we judged each child for obesity with their body weight, height, and age according to Korean pediatric standard growth curve. We regarded each child as obese in case that body weight belong to upper 10 percentile according to growth curve. Body weight was checked at before and after treatment for identification of bias according to change of body weight. All patients received 4 weeks course of single intranasal administration in each nostril with mometasone furoate (100 µg). After 4 weeks course of therapy, all patients were re-assessed to evaluate the efficacy of treatment.
Outcome measures
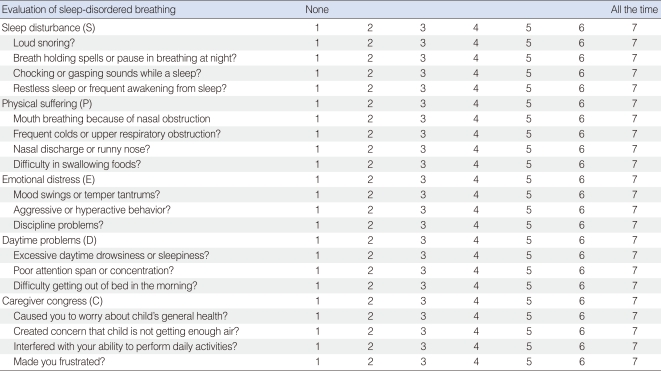
The primary outcome was measured with the OSA-18 survey (Table 1), a valid and reliable discriminative quality of life (QOL) measure for children with varying levels of SDB (7, 8). The OSA-18 has been previously shown to possess satisfactory test-retest reliability and internal consistency (7). The survey consists of 18 items grouped into 5 domains: sleep disturbance (4 items), physical suffering (4 items), emotional distress (3 items), daytime problems (3 items), and caregiver concerns (4 items). Items are scored on a 7-point ordinal scale and have excellent test-retest reliability.
Table 1.
Parental questionnaire (OSA-18) for sleep disordered breathing
OSA-18: Obstructive sleep apnea-18.
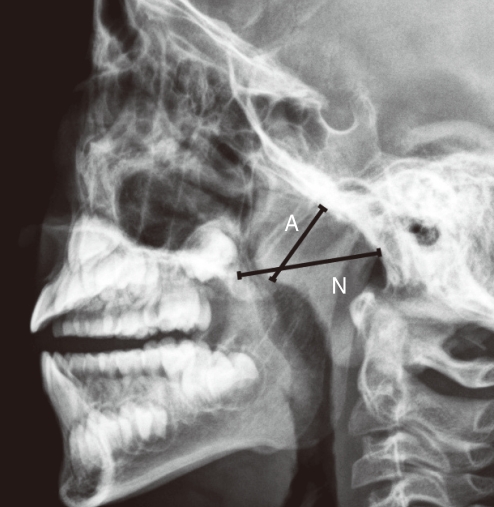
After completing questionnaire, OSA-18, they were evaluated for measuring adenoidal-nasopharyngeal (AN) ratios by using lateral radiographs of nasopharynx. Lateral radiographs of the nasopharynx were exposed with the patient in the erect position and the head fixed with a wall-mounted cephalostat and oriented with the Frankfort horizontal plane. The exposures were made with 70 kV, and the exposure time varied between 0.4 and 0.6 depending on the age of the children. For each of the radiographs, the AN ratio was computed according to the method of Fujioka et al. (9) (Fig. 1).
Fig. 1.
Method of assessing adenoid enlargement on lateral neck radiography. In this method the adenoidal measurement (A) represents the distance from the point of maximal convexity of the adenoid shadow to a line along the anterior margin of the basiocciput. The nasopharyngeal measurement (N) is the distance between the posterior border of the hard palate and the antero-inferior edge of the sphenobasioccipital synchondrosis.
Statistics
The AN ratio was obtained by dividing the measurement for A by the value for N. A commercially available statistical program (SPSS ver. 11.5, SPSS Inc, Chicago, IL, USA) was used to perform the statistical analysis. Statistical comparisons of changes in OSA-18 score between before and after topical intranasal mometasone furoate treatment employed Wilcoxon signed rank test. A paired t-test was used for comparison of changes in AN ratio and body weight. Spearmann rank correlation analysis was employed to analyze the correlation between change in OSA-18 score and change in AN ratio. Mann-Whitney U-test was used to analyze the effect of allergy, obesity and sinusitis on the change of OSA-18 score. A P-value of less than 0.05 was considered statistically significant.
RESULTS
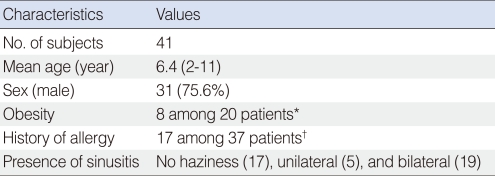
Table 2 summarizes the demographic data including the patient's age, sex, body weights, and history of allergy. All 41 children completed the 4-weeks course of intranasal mometasone furoate treatment. Compliance with daily nasal spray was comparable and there was no significant side effect such as dry nose and epistaxis.
Table 2.
Characteristics of patients
*20 of 41 children were checked body weight and height. We regarded each child as obese in case that body weight belongs to upper 10 percentile according to growth curve. †37 of 41 children were checked for allergy.
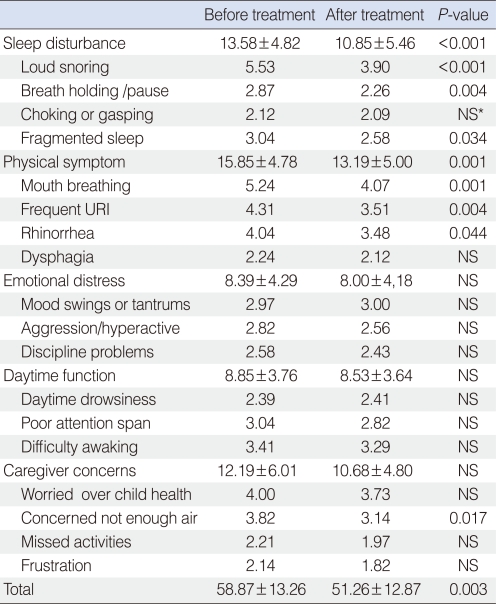
The changes of OSA-18 survey score after treatment are shown in Table 3. Sleep disturbance and physical suffering were the highest rated domains, followed by caregiver concerns, daytime problems, and emotional distress.
Table 3.
Parental questionnaire (OSA-18) results before and after intranasal corticosteroid treatment
*No statistically significant difference.
URI: upper respiratory infection; OSA-18: obstructive sleep apnea-18.
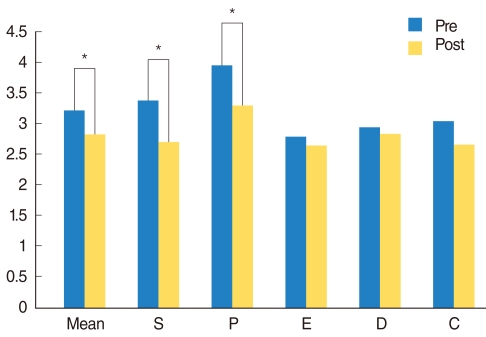
There was significant reduction in score of sleep disturbance domain (P<0.001) and physical symptom domain (P=0.001) after treatment. Also, total OSA-18 score decreased significantly (P=0.003) after the treatment (Fig. 2). Among 41 patients, 37 children were tested for allergy and 17 patients were proved to have allergic rhinitis based on their symptom and allergy test. And we could obtain the information of body weight and height in 20 children, and 8 children were proved to be obese. But, presence of allergy (P=0.065) and obesity (P=0.851) didn't affect the effect of nasal steroid on total OSA-18 score. There was no significant change in body weight between before and after treatment (P=0.954).
Fig. 2.
Comparison of symptom score between pre and post-4weeks course of topical steroid treatment. S: sleep disturbance; P: physical suffering; E: emotional distress; D: daytime problems; C: caregiver concerns. *P<0.05.
Sinus X-ray was checked in all children and sinusitis were detected in 24 children. 19 children showed bilateral haziness of sinus on X-ray and 5 children showed unilateral haziness. Change in OSA-18 score showed no significant difference according to presence of sinusitis (P=0.488).
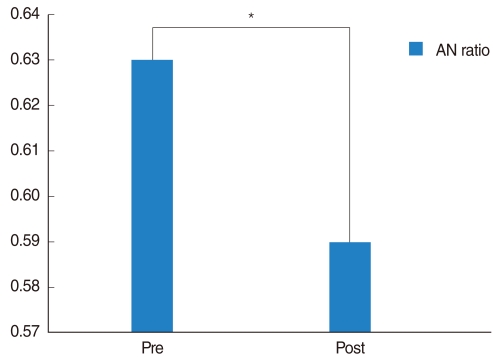
The mean AN ratio was 0.63±0.11 before the treatment and 0.59±0.12 after the treatment. There was a statistically significant difference (P=0.006) between before and after treatment (Fig. 3). There was no significant correlation between the changes of AN ratio and improvement of symptom score (P=0.858).
Fig. 3.
Comparison of adenoid-nasopharyngeal (AN) ratio between pre and post-4weeks course of topical steroid treatment. *P<0.05.
DISCUSSION
This prospective, observational study shows a significant improvement in both mean OSA-18 survey score and adenoidal-nasopharyngeal ratio in children with sleep disordered breathing after 4-weeks trial of intranasal monetasone furoate. Among OSA-18 items, loud snoring, breath holding, fragmented sleep, mouth breathing, frequent URI, and rhinorrhea were improved significantly. The mean OSA-18 survey score improved in 27 of 41 children (65.8%) treated with monetasone furonate. Physical suffering (mean score, 3.96) and sleep disturbance (mean score, 3.40) were the highest rated domains, and this result was identical to other study (4).
Among several commercially available steroid nasal sprays, we selected mometasone furoate for this study. This spray had been reported previously not to cause any adverse effect on nasal mucosa on long term use (10) and it has no effect on growth and hypothalamic-pituitary-adrenal axis. Above all things (11, 12), the systemic availability of the drug after topical administration is lower than that of other steroids (13).
In 2001, Brouilette et al. (1) tested the efficacy of another intranasal steroid treatment for OSAS. In this trial they investigated the effect of fluticasone propionate nasal spray versus placebo for 25 children suffering from OSAS, with results of polysomnography. In this study 69% of children who received fluticasone showed improvement in symptom score.
Recently Berlucchi et al. (14) assessed the efficacy of mometasone furonate in treatment of adenoid hypertrophy after 40 days course of treatment. Of patients enrolled, 77.7% of children showed symptomatic improvement, that is somewhat superior to our result. But, considering the relatively short course of treatment of our study, our result dose not seems to much different to that of previous study.
We used lateral neck X-ray for assessment of adenoid hypertrophy, and this method was widely used for decades. Fujioka et al. (9) in 1979 described AN ratio as an indicator of adenoidal size, and this method had been adopted in many other studies. Cohen et al. (15) in 1992 reported usefulness of lateral cervical radiographs in evaluation of adenoid size, and Major et al. (16) in 2006 systematically reviewed lateral cephalometric diagnosis in adenoid hypertrophy, and proved that the results of lateral neck X-ray showed good correlation with actual adenoid size.
Acoustic rhinometry have been known as useful tool in evaluating nasopharyngeal cross-sectional area and volume after adenoidectomy (17, 18). But short term use of mometasone nasal spray couldn't make so much reduction of adenoid size comparing with adenoidectomy. Considering the effect of nasal cycle on acoustic rhinometry and reduction of adenoid size after application of intransal spray, we didn't employ acoustic rhinometry as a tool to evaluate efficacy of short term nasal steroid spry for pediatric sleep disorderd breathing.
In our study, 22 of 31 children (71%) who had tested with lateral neck radiography, showed decreased AN ratio after 4 weeks course of treatment (P=0.006). Demain and Goetz (19) in 1995 reported a study of standard dose aqueous nasal beclomethasone in treatment of adenoid hypertrophy. All Adenoid size was decreased in all enrolled patients after 8 weeks treatment and mean reduction in AN ratio was 29%. Cengel and Akyol (20) in 2006 studied change of adenoid size after 6 weeks course of intransal mometasone furonate treatment. 67.2% of enrolled children showed reduction of adenoid size after treatment. However there has been no proven mechanism about shrinkage of adenoid. Existence of inflammation had been proved in mucosal surface at soft plate in OSAS patients (21, 22). We think that this type of inflammation might exist in covering mucosa of adenoid which locates at narrowest area of upper airway. For this reason, application of topical steroid for 4 weeks might reduce the inflammation of covering mucosa of adenoid. Therefore, application of intransal steroid can be effective treatment option for reducing adenoid size.
We chose OSA-18 as the measuring tool for assessing the efficacy of intranasal steroid. In 2000, Franco et al. (23) proposed OSA-18 as a practical mean of office-based determination of quality-of-life impact for obstructive sleep apnea syndrome in children. In 2005, Michell and Kelly (24) used OSA-18 as indicator for treatment response after adenotonsillectomy in SDB children and mentioned that it was so useful. OSA-18 is composed of easily applicable 18 questions and has relatively high reproducibility (4), and it is known that OSA-18 shows good correlation with respiratory disturbance index (RDI) (25).
In our study, parents or caregivers could easily carry out the questionnaire and it takes only few minutes to fill up the form. For this reason, we thought that OSA-18 can be excellent tool for evaluating SDB children after treatment in office-based clinics or other clinics without polysomnography (PSG). Moreover, in the case of tertiary care clinics with PSG, OSA-18 can have a additional role in children not suitable for PSG.
There are a few options for evaluating the adenoid size in pediatric SDB patients. Among them lateral neck radiography and direct video rhinoscopy has been used widely. Mlynarek et al. (25) in 2004 reported that direct video rhinoscopy is better correlated to the severity of symptoms than are values obtained by lateral neck radiography. But fiberoptic examination of child's nasopharynx can be challenging and might not be suitable for all patients. In some children it is impossible to exam nasopharynx due to patient's noncooperation (26). For this reason we selected lateral neck radiography for assessing adenoid size. But we could not get data from all enrolled children. Some patients refused to let their children be exposed radiation in spite of harmless dose.
As the result of our study, allergic rhinitis and sinusitis had no influence on degree of change in adenoid size and in OSA-18 score. According to other report, adenoid size decreased significantly after intranasal steroid and there was notable difference in improvement after treatment according to allergy status (27). But there are not so many reports about effect of allergy on efficacy of intranasal steroid in pediatric SDB patients, so further research is required with large sample size.
We assumed that improvement in quality of life of SDB children is due to not only decreased AN ratio but also other factors such as increase nasal airway patency. Considering this result, intranasal steroid can be used in SDB children regardless of allergic status or sinusitis.
There are some limitations to this study. We could not have a control group due to lack of consent. At early period of this study, we wanted to have control group using placebo. But most parents and caregivers refused to participate in our study because of using placebo. The other limitation is that we didn't confirm the increased nasal airway patency with objective tool. In general, acoustric rhinometry has been used as popular tool for assessing nasal airway. But most cohorts of our study were under 5 years old, so it was impossible to get patient's cooperation during acoustic rhinometry.
In conclusion, We believe that 4-weeks course of intranasal steroid (mometasone furoate) can be a effective treatment option in pediatric SDB patients without significant complications. And this treatment works effectively regardless of allergic status, sinusitis, and obesity.
Future placebo controlled study will be required to ascertain the effect of short term steroid use for pediatric sleep disordered breathing.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Brouillette RT, Manoukian JJ, Ducharme FM, Oudjhane K, Earle LG, Ladan S, et al. Efficacy of fluticasone nasal spray for pediatric obstructive sleep apnea. J Pediatr. 2001 Jun;138(6):838–844. doi: 10.1067/mpd.2001.114474. [DOI] [PubMed] [Google Scholar]
- 2.Alexopoulos EI, Kaditis AG, Kalampouka E, Kostadima E, Angelopoulos NV, Mikraki V, et al. Nasal corticosteroids for children with snoring. Pediatr Pulmonol. 2004 Aug;38(2):161–167. doi: 10.1002/ppul.20079. [DOI] [PubMed] [Google Scholar]
- 3.Gislason T, Benediktsdóttir B. Snoring, apneic episodes, and nocturnal hypoxemia among children 6 months to 6 years old: an epidemiologic study of lower limit of prevalence. Chest. 1995 Apr;107(4):963–966. doi: 10.1378/chest.107.4.963. [DOI] [PubMed] [Google Scholar]
- 4.Sohn H, Rosenfeld RM. Evaluation of sleep-disordered breathing in children. Otolaryngol Head Neck Surg. 2003 Mar;128(3):344–352. doi: 10.1067/mhn.2003.4. [DOI] [PubMed] [Google Scholar]
- 5.Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2) LEN and AllerGen) Allergy. 2008 Apr;63(Suppl 86):8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 6.Fokkens W, Lund V, Mullol J European Position Paper on Rhinosinusitis and Nasal Polyps Group. EP3OS 2007: European position paper on rhinosinusitis and nasal polyps 2007. A summary for otorhinolaryngologists. Rhinology. 2007 Jun;45(2):97–101. [PubMed] [Google Scholar]
- 7.Silva VC, Leite AJ. Quality of life in children with sleep-disordered breathing: evaluation by OSA-18. Braz J Otorhinolaryngol. 2006 Nov–Dec;72(6):747–756. doi: 10.1016/s1808-8694(15)31041-7. [DOI] [PubMed] [Google Scholar]
- 8.Strocker AM, Carrer A, Shapiro NL. The validity of the OSA-18 among three groups of pediatric patients. Int J Pediatr Otorhinolaryngol. 2005 Feb;69(2):241–247. doi: 10.1016/j.ijporl.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Fujioka M, Young LW, Girdany BR. Radiographic evaluation of adenoidal size in children: adenoidal-nasopharyngeal ratio. AJR Am J Roentgenol. 1979 Sep;133(3):401–404. doi: 10.2214/ajr.133.3.401. [DOI] [PubMed] [Google Scholar]
- 10.Minshall E, Ghaffar O, Cameron L, O'Brien F, Quinn H, Rowe-Jones J, et al. Assessment by nasal biopsy of long-term use of mometasone furoate aqueous nasal spray (Nasonex) in the treatment of perennial rhinitis. Otolaryngol Head Neck Surg. 1998 May;118(5):648–654. doi: 10.1177/019459989811800514. [DOI] [PubMed] [Google Scholar]
- 11.Boner AL. Effects of intranasal corticosteroids on the hypothalamic-pituitary-adrenal axis in children. J Allergy Clin Immunol. 2001 Jul;108(1 Suppl):S32–S39. doi: 10.1067/mai.2001.115564. [DOI] [PubMed] [Google Scholar]
- 12.Schenkel EJ, Skoner DP, Bronsky EA, Miller SD, Pearlman DS, Rooklin A, et al. Absence of growth retardation in children with perennial allergic rhinitis after one year of treatment with mometasone furoate aqueous nasal spray. Pediatrics. 2000 Feb;105(2):E22. doi: 10.1542/peds.105.2.e22. [DOI] [PubMed] [Google Scholar]
- 13.Szefler SJ. Pharmacokinetics of intranasal corticosteroids. J Allergy Clin Immunol. 2001 Jul;108(1 Suppl):S26–S31. doi: 10.1067/mai.2001.115563. [DOI] [PubMed] [Google Scholar]
- 14.Berlucchi M, Salsi D, Valetti L, Parrinello G, Nicolai P. The role of mometasone furoate aqueous nasal spray in the treatment of adenoidal hypertrophy in the pediatric age group: preliminary results of a prospective, randomized study. Pediatrics. 2007 Jun;119(6):e1392–e1397. doi: 10.1542/peds.2006-1769. [DOI] [PubMed] [Google Scholar]
- 15.Cohen LM, Koltai PJ, Scott JR. Lateral cervical radiographs and adenoid size: do they correlate? Ear Nose Throat J. 1992 Dec;71(12):638–642. [PubMed] [Google Scholar]
- 16.Major MP, Flores-Mir C, Major PW. Assessment of lateral cephalometric diagnosis of adenoid hypertrophy and posterior upper airway obstruction: a systematic review. Am J Orthod Dentofacial Orthop. 2006 Dec;130(6):700–708. doi: 10.1016/j.ajodo.2005.05.050. [DOI] [PubMed] [Google Scholar]
- 17.Cho JH, Lee DH, Lee NS, Won YS, Yoon HR, Suh BD. Size assessment of adenoid and nasopharyngeal airway by acoustic rhinometry in children. J Laryngol Otol. 1999 Oct;113(10):899–905. doi: 10.1017/s0022215100145530. [DOI] [PubMed] [Google Scholar]
- 18.Piszcz M, Skotnicka B, Hassmann-Poznanska E. Acoustic rhinometry evaluation of adenoid hypertrophy and adenoidectomy efficacy. Otolaryngol Pol. 2008;62(3):300–304. doi: 10.1016/S0030-6657(08)70259-2. [DOI] [PubMed] [Google Scholar]
- 19.Demain JG, Goetz DW. Pediatric adenoidal hypertrophy and nasal airway obstruction: reduction with aqueous nasal beclomethasone. Pediatrics. 1995 Mar;95(3):355–364. [PubMed] [Google Scholar]
- 20.Cengel S, Akyol MU. The role of topical nasal steroids in the treatment of children with otitis media with effusion and/or adenoid hypertrophy. Int J Pediatr Otorhinolaryngol. 2006 Apr;70(4):639–645. doi: 10.1016/j.ijporl.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Kimoff RJ, Hamid Q, Divangahi M, Hussain S, Bao W, Naor N, et al. Increased upper airway cytokines and oxidative stress in severe obstructive sleep apnoea. Eur Respir J. 2010 Sep 16; doi: 10.1183/09031936.00048610. [Epub]. DOI: 10.1183/09031936.00048610. [DOI] [PubMed] [Google Scholar]
- 22.Sabato R, Guido P, Salerno FG, Resta O, Spanevello A, Barbaro MP. Airway inflammation in patients affected by obstructive sleep apnea. Monaldi Arch Chest Dis. 2006 Jun;65(2):102–105. doi: 10.4081/monaldi.2006.572. [DOI] [PubMed] [Google Scholar]
- 23.Franco RA, Jr, Rosenfeld RM, Rao M. First place--resident clinical science award 1999: quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000 Jul;123(1 Pt 1):9–16. doi: 10.1067/mhn.2000.105254. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell RB, Kelly J. Quality of life after adenotonsillectomy for SDB in children. Otolaryngol Head Neck Surg. 2005 Oct;133(4):569–572. doi: 10.1016/j.otohns.2005.05.040. [DOI] [PubMed] [Google Scholar]
- 25.Mlynarek A, Tewfik MA, Hagr A, Manoukian JJ, Schloss MD, Tewfik TL, et al. Lateral neck radiography versus direct video rhinoscopy in assessing adenoid size. J Otolaryngol. 2004 Dec;33(6):360–365. doi: 10.2310/7070.2004.03074. [DOI] [PubMed] [Google Scholar]
- 26.Selkin SG. Flexible fiberoptics and pediatric otolaryngology: a simple technique for examination and photodocumentation. Int J Pediatr Otorhinolaryngol. 1983 Jul;5(3):325–333. doi: 10.1016/s0165-5876(83)80046-9. [DOI] [PubMed] [Google Scholar]
- 27.Modrzyński M, Zawisza E, Mazurek H. The influence of medical treatment of the perennial allergic rhinitis on the adenoid size in children. Otolaryngol Pol. 2006;60(4):543–550. [PubMed] [Google Scholar]