Abstract
Objective
Factors underlying progressive brain volume changes in schizophrenia remain poorly understood. We investigate whether a gene polymorphism influencing neuroplasticity may contribute to longitudinal brain volume alterations.
Method
High-resolution magnetic resonance images of the whole brain were obtained on 119 patients with recent-onset schizophrenia-spectrum disorders. Changes in brain volumes averaging 3 years were compared between BDNF val66met genotype groupings. Exploratory analyses were further conducted to examine relationships between antipsychotic treatment and brain volume changes, as well as the effects of BDNF genotype on changes in cognition and symptoms.
Results
There were significant genotype effects on within-subject changes in frontal lobe gray matter (GM), lateral ventricles and sulcal CSF volumes. Met-allele-carriers had significantly greater reductions in frontal GM and reciprocal enlargements in lateral ventricles and sulcal (especially frontal and temporal) CSF volumes than Val homozygous patients. Independent of BDNF genotype, more antipsychotic exposure between MRI scans correlated with greater frontal GM volume reductions particularly among initially treatment naïve patients. There were no statistically significant genotype effects on within-subject changes in cognition or symptoms.
Conclusions
BDNFMet variant may be one of several factors affecting progressive brain volumes changes in schizophrenia.
From computerized tomography (CT) studies completed in the 1980s through the mid-1990s, cross-sectional and longitudinal assessments of lateral ventricle volumes in schizophrenia patients indicate that ventricular enlargement is already evident in first-episode psychosis, does not correlate with illness duration, and does not appear to be progressive (1, 2). However, contrary to these early CT studies, which are limited by low spatial resolution, small sample sizes and reliance on a single brain volume measure, the growing list of longitudinal MRI studies (3-11) provides increasingly convergent evidence for progressive brain volume changes during the lifelong course of schizophrenia. Furthermore, most cross-sectional MRI studies, though not all (12), that investigated the relationships between brain volumes and illness duration (13), or compared brain volumes between recently ill patients versus chronic patients (14) have also suggested that there are ongoing brain volume changes in schizophrenia patients.
Although longitudinal and cross-sectional MRI studies on schizophrenia patients during the past decade provide compelling evidence that there are progressive volumetric changes in the frontal and temporal lobes following illness onset, the mechanisms underlying ongoing fronto-temporal tissue volume reductions and CSF volume expansions are unclear, and remain intensely debated (15, 16). What factors might mediate progressive brain volume decrement in schizophrenia patients? How important are these changes in the clinical management of patients? Potential causes for brain volume changes include pathophysiology of schizophrenia, neuroplasticity secondary to antipsychotics, impoverished environment, fluid imbalance, nutrition or lifestyle, and measurement artifacts. In this study, the primary aim is to determine if a functional gene polymorphism, which influences neuroplasticity and has been implicated in schizophrenia, may mediate progressive brain volume changes in schizophrenia patients.
Brain-derived neurotrophic factor (BDNF) is a trophic protein vital for neurodevelopment as well as in modulating activity-dependent synaptic plasticity among mature neurons, particularly in the hippocampus and neocortex (17-19). Studies indicate that the methionine (Met) variant of a common single nucleotide polymorphism (SNP; rs6265), which produces valine (Val) to Met substitution at codon 66 in the proBDNF protein, is associated with inefficient BDNF trafficking, reduced activity-dependent BDNF release, and poorer hippocampus-mediated memory (20-25). Furthermore, in previous cross-sectional MRI studies, we and others found Met-allele-carrier schizophrenia patients had smaller frontal and temporal gray matter (GM) volumes than Val homozygotes (22, 26, 27).
How might a single nucleotide substitution in the gene encoding the proBDNF protein confer poorer cognitive performance and smaller brain volumes? Similar to other neurotrophins, BDNF is synthesized as a precursor peptide (proBDNF). Like other pro-neurotrophins, pro-BDNF is important for proper folding, dimerization and targeting of the mature BDNF (28). During intracellular trafficking through the Golgi network, the proBDNF domain is cleaved and the remaining mature BDNF protein is packaged into secretory vesicles. When hippocampal neurons (21) or cerebral cortical neurons (20) were transfected with BDNFMet variant, there was less efficient localization of mature BDNF to secretory vesicles compared to the wild-type BDNFVal. Thus, substitution of valine with methionine in the proBDNF is believed to disrupt folding and dimerization of BDNF and, in turn, results in defective intracellular protein trafficking and diminished BDNF synthesis (20, 21). Additionally, mechanisms by which BDNFMet variant decreases GM brain volumes may be mediated during neurodevelopment through BDNF’s neurotrophic effects (23, 29). In a relatively BDNF-deficient milieu during embryogenesis, fewer neurons survive and surviving neurons have smaller soma size and diminished dendritic growth (17). Alternatively, BDNFMet variant may further influence GM brain volumes beyond neurodevelopment through modulating neuroplasticity in mature neurons (18).
One approach to understanding when BDNF exerts its influence on brain volumes is to examine the relationships between BDNF val66met genotype status and longitudinal changes in brain volumes. If the effects of BDNF occur exclusively during neurodevelopment, one would not expect BDNF genotype to influence longitudinal brain volume changes in adults who are in their third or fourth decades of life. However, if BDNF val66met genotype has significant effects on longitudinal brain volume changes in young adult schizophrenia patients, it suggests that BDNF mediates brain volumes beyond the period of neurodevelopment, possibly via BDNF’s role in neuroplasticity (17, 18, 30).
Given that the BDNFMet variant is associated with diminished BDNF trafficking and BDNF release (20, 21) and diminished BDNF signaling in mature neurons decreases dendritic arborization (18), we hypothesize that Met-allele-carriers (heterozygotes and Met homozygotes) will have greater GM brain volume reductions than Val homozygotes. The primary aim of this study was to determine if BDNF val66met genotype status mediates progressive brain volume changes in schizophrenia. In addition, we will also explore two related questions: 1) the association between antipsychotic treatment and progressive brain volume changes, based on evidence involving animals (31-34) and humans (10, 35-37) indicating that antipsychotic medications may contribute to brain volume changes, and 2) the effects of BDNF val66met genotype on longitudinal changes in cognition and clinical symptoms.
Methods
Subjects
Subjects were obtained through the ongoing Iowa Longitudinal Study of Recent Onset Psychoses (38). After complete description of the study to the subjects, written informed consent was obtained. The study design and method have been previously described. In brief, the study consists of subjects with first-episode schizophrenia or schizophrenia-spectrum disorders. At the time of intake into the study, subjects undergo an extensive evaluation, which included standardized clinical rating scales (such as the Comprehensive Assessment of Symptoms and History (CASH) (39)), a neuropsychological battery, and magnetic resonance imaging (MRI) of the brain. Following intake assessment, subjects are evaluated at 6-month intervals using longitudinal follow-up versions of the clinical rating scales. At the 2-, 5-, 9-year, and 3-yearly thereafter, the extensive assessments performed at intake are repeated, including MRI of the brain and neuropsychological testing.
The 119 subjects (M:F=83:36; 113 Caucasians, 2 African-Americans, 4 Hispanics) in this report were selected from the larger overall sample based on having 1) CASH diagnosis of DSM schizophrenia-spectrum disorders (schizophrenia (N=107), schizophreniform disorder (N=4) or schizoaffective disorder (N=8)), 2) undergone at least two brain MRI scans, i.e. at intake and one follow-up scan, and 3) available BDNF genotype data. At initial assessment, mean age was 26.4 years (SD=6.77), and the sample had minimal prior treatment: 50 neuroleptic-naïve; Mean antipsychotic treatment duration=9.2 months (SD=17.0). In subjects who have more than one follow-up MRI scan, the first available scan was used so as to reduce heterogeneity in follow-up duration (Mean=2.96 years (SD=1.56)).
MRI acquisition and image processing
Magnetic resonance images of the whole brain were obtained on a 1.5-Tesla GE (General Electric Medical Systems, Milwaukee, Wisconsin) Signa MR scanner. Three different MR sequences were acquired for each subject (i.e. T1-weighted spoiled grass, proton density (PD) and T2-weighted images). The images were processed using the locally developed BRAINS (Brain Research: Analysis of Images, Networks, and Systems) software package. The imaging parameters as well as detailed descriptions of image analysis methods have been provided elsewhere (40, 41). In brief, the T1-weighted images were spatially normalized and re-sampled so that the anterior-posterior axis of the brain was realigned parallel to the anterior-posterior commissure line, and the interhemispheric fissure was aligned on the other two axes. The T2 and PD weighted images were aligned to the spatially normalized T1 weighted image using an automated image registration program. These images were then subjected to a linear transformation into standardized stereotaxic Talairach atlas space to generate automated measurements of frontal, temporal, parietal, and occipital lobes, cerebellum, and subcortical regions (40). To further classify tissue volumes into gray matter (GM), white matter (WM) and cerebrospinal fluid (CSF), we employed a discriminant analysis method of tissue segmentation based on automated training class selection that utilized data from the T1, T2 and PD sequences (41). In this study, we examined six brain volume measures: frontal lobe GM, temporal GM, parietal GM, occipital GM, lateral ventricles, and sulcal CSF.
Neurocognitive and Symptom Assessments
Study subjects were administered a comprehensive battery of neuropsychological tests by psychometrists who have been trained in standardized assessment and scoring procedures. Testing generally took approximately 4 hours to complete and, when necessary, occurred over several sessions. In order to provide comprehensive yet efficient assessment of the relationships between cognitive performance and BDNF polymorphism, 27 neuropsychological test scores were grouped into cognitive domains on the basis of a priori theoretical considerations (42, 43). These five domains were: verbal memory, processing speed/attention, problem solving, language skills, and visuospatial skills. These theoretical groupings of cognitive domains have good internal consistency, and their internal reliability have been tested using Cronbach’s alpha (42, 44). The median Cronbach’s alpha for the five cognitive domains was 0.80 (range=0.75 to 0.85). Prior to deriving cognitive domain scores for subjects in this study, the raw test score from each of the neuropsychological test variable was converted to a z score (Mean=0, SD=1) based on test performance of the sample at intake assessment. Scores were reversed where necessary so that a larger negative score indicates poorer performance below the mean. From these z scores, each domain score is the summed average of its component neuropsychological test variables.
Using the Scale for Assessment of Positive Symptoms (SAPS) and Scale for Assessment of Negative Symtpoms Symptom (SANS) (39), symptom severity at the time of intake and follow-up were assessed along three domains: psychotic, negative and disorganized. The psychotic domain was defined as sum of the hallucinations and delusions global ratings from SAPS; disorganized domain was sum of the positive formal thought disorder, bizarre/disorganized behavior, and inappropriate affect global ratings from SAPS; and negative domain was defined as sum of the affective flattening, alogia, avolition/apathy, and anhedonia/asociality global ratings from SANS. The maximum possible scores for the psychotic, disorganized and negative dimensions are 10, 15 and 20 respectively and higher scores indicate more severe symptoms.
Genetic Analyses
DNA was prepared by high-salt extraction from whole blood. BDNF val66met genotyping was performed using the fluorogenic 5′ nuclease method (TaqMan®, Applied Biosystems (ABI), Foster City, CA) using reagents obtained from ABI, including VIC and FAM labeled probes and TaqMan® Universal PCR Master Mix. PCR and allele calling were performed on a StrataGene Mx3000P qPCR thermocycler. Replicate samples were included on all genotyping plates to ensure accurate allele calling.
Statistical analyses
In neuronal cell cultures, inefficient BDNF trafficking is observed when Met variant is expressed alone or when Met and Val variants are co-expressed (20, 21). Therefore, since Met-allele-carrier status is associated with impaired BDNF secretion, heterozygotes and Met homozygotes in this study were categorized as ‘Met group’, and compared against Val homozygotes (‘Val group’).
To investigate the effects of BDNF genotype on progressive brain volume changes, repeated measures analysis of covariance (ANCOVA--also known as multivariate analysis of variance, or MANOVA) was used to examine whether genotype grouping (Met-allele-carriers versus Val homozygotes) had significant interactions with longitudinal within-subject changes in each region-of-interest (ROI). In the general linear statistical model for each of the six ROI (frontal lobe GM, temporal GM, parietal GM, occipital GM, lateral ventricles, and sulcal CSF), intake and follow-up volumes were the dependent measures (within-subject factors). The independent measure was genotype grouping. Total brain compartment volume, age at intake scan, inter-scan interval and inter-scan antipsychotic exposure (dose years; 1 dose year=100mg CPZ-equivalent/day for 1 year) were entered as covariates. Total brain compartment volume adjusts for individual differences in overall cranial size. Age at intake scan was used as a covariate since age is known to influence brain volumes. Likewise, inter-scan interval was also entered as a covariate because of differences in time duration between intake and follow-up scans among the subjects. For ROIs where genotype grouping had significant interactions with within-subject factors of repeated measures in brain volumes (i.e. brain volume changes over time differed significantly across genotype groupings), post hoc analyses used paired t-tests to examine changes in these ROIs over time within each genotype grouping.
To explore the effects of BDNF genotype on longitudinal changes in neurocognition and psychopathology, a similar statistical approach of repeated measures ANCOVA was used. In the general linear statistical model for each of the five cognitive domain scores (Verbal Memory, Speed/Attention, Problem Solving, Language and Visuospatial Abilities) and three symptom domain ratings, intake and follow-up scores were the dependent measures (within-subject factors). The independent measure was genotype grouping. Gender, age at baseline assessment, inter-scan interval, and inter-scan antipsychotic exposure (dose years) were entered as covariates. Full-scale IQ was an additional covariate in the analyses of neurocognition.
Lastly, exploratory regression analyses were performed to examine if the relationships between longitudinal changes in MRI brain volumes and changes in neurocognition were different across BDNF genotype groupings.
Results
Genotype (Met/Met=3.4%, Val/Met=34.5%, Val/Val=62.1%) and allele (20.6% Met) frequency distributions were consistent with those expected of Caucasian samples. Met and Val groups did not differ significantly in age, inter-scan interval, or on factors associated with poor outcome in schizophrenia – male gender, early age of illness onset or poor premorbid social adjustment (Table 1).
Table 1.
Comparison of sociodemographics, illness characteristics and antipsychotic treatment (Mean (SD) or Number (%)) between 45 BDNF Met-allele carriers and 74 BDNF Val homozygous schizophrenia patients
| Met carriers | Val homozygotes | Statistic (p) a | |
|---|---|---|---|
| Age at initial scan (years) | 26.3 (7.2) | 26.5 (6.5) | 0.15 (0.88) |
| Inter-scan interval (years) | 2.6 (1.4) | 3.1 (1.6) | 1.84 (0.07) |
| Gender : Number males (%) | 29 (64.4) | 54 (73.0) | 0.96 (0.33) |
| Age of illness onset (years) | 24.8 (7.6) | 24.3 (6.1) | 0.36 (0.72) |
| Premorbid social adjustment b | 8.6 (4.6) | 9.7 (4.1) | 1.26 (0.21) |
| Neuroleptic naïve at initial scan: N (%) | 23 (51.1) | 27 (36.5) | 2.46 (0.12) |
| Percentage of inter-scan interval treated with: | |||
| Any antipsychotics | 86.8 (25.3) | 83.7 (29.2) | 0.59 (0.56) |
| Non-clozapine atypicals | 49.7 (42.1) | 51.8 (42.5) | 0.26 (0.79) |
| Typical antipsychotics | 39.2 (36.7) | 40.3 (38.8) | 0.15 (0.88) |
| Clozapine | 8.9 ( 16.3) | 5.2 (14.4) | 1.28 (0.20) |
| Ever needed clozapine treatment: N (%) | 12 (26.7) | 12 (16.2) | 1.90 (0.17) |
| Antipsychotic dose (CPZ mg-equiv/day) | 484.7 (361.0) | 541.2 (530.3) | 0.69 (0.49) |
| Dose year (100mg CPZ/day × 1 year) | 13.3 (12.7) | 18.2 (29.2) | 1.57 (0.12) |
| Medication compliance | 1.8 (0.8) | 1.9 (0.9) | 1.00 (0.32) |
Independent group t-tests comparing group means (SD; df=117) except for gender, neuroleptic naivity, and ever needed clozapine treatement (χ2, df=1),
Modified Premorbid Social Adjustment Scale
At baseline scan, 50 subjects were neuroleptic naïve. The proportions of neuroleptic naïve patients in each BDNF genotype grouping did not differ significantly (Table 1; χ2=2.46, p=0.12). Being a long-term longitudinal study, antipsychotic treatment during the inter-scan interval was naturalistic. Patients received antipsychotic treatment for much of the time period between scans (Mean=84.9% of the inter-scan interval (SD=27.7)). Non-clozapine atypicals were the predominant class of antipsychotics. Twenty-four patients (20.2%) required clozapine treatment during the inter-scan interval. Mean antipsychotic dose for the sample was 519.8mg chlorpromazine (CPZ)-equivalent/day (SD=472.6). Compliance with antipsychotic treatment was between Good to Excellent (Mean=1.87 (SD=0.86); rated on a 5-point scale with 1 being ‘Excellent’ and 2 being ‘Good’). None of these antipsychotic treatment measures differed significantly between BDNF genotype groupings (Table 1).
Longitudinal changes in MRI brain volumes between BDNF genotype groupings
Least square means for MRI brain volumes at baseline and at follow-up assessment are summarized in Table 2. There was a significant genotype main effect on within-subject changes in frontal GM volume (F=4.20, dfs=1,113, p=0.05). Met-allele-carriers showed significant reductions in frontal GM volume at follow-up assessment compared to baseline (Mean=−4.83 cc; T=2.08, df=44, p=0.04). Follow-up frontal GM volumes did not differ significantly from baseline among Val homozygotes (Mean=−0.98 cc; T=0.56, df=73, p=0.58). There were no significant genotype main effects on within-subject changes in temporal, parietal or occipital GM volumes (Table 2; F≤0.73, dfs=1,113, p≥0.40).
Table 2.
Comparison of longitudinal changes in MRI brain volumes (Least Square Mean (SD) (cc)) between 45 BDNF Met-allele carriers and 74 BDNF Val homozygous schizophrenia patients
| Met carriers | Val homozygotes |
Genotype F (p) a |
Treatment b F (p) c |
||
|---|---|---|---|---|---|
| Frontal GM | Baseline | 265.3 (15.3) | 265.1 (20.4) | 4.02 (0.05) | 3.22 (0.08) |
| Follow-up | 260.5 (15.2) | 266.1 (16.0) | |||
| Temporal GM | Baseline | 154.6 (8.5) | 154.6 (9.6) | 0.73 (0.40) | 0.45 (0.51) |
| Follow-up | 153.0 (10.2) | 154.9 (10.4) | |||
| Parietal GM | Baseline | 137.3 (8.3) | 138.2 (9.5) | 0.38 (0.54) | 1.21 (0.27) |
| Follow-up | 137.1 (9.0) | 139.1 (9.0) | |||
| Occipital GM | Baseline | 67.2 (8.9) | 69.6 (7.5) | 0.11 (0.74) | 0.72 (0.40) |
| Follow-up | 68.6 (7.7) | 70.5 (6.7) | |||
| Lateral Ventricles | Baseline | 15.4 (6.2) | 16.1 (6.7) | 7.38 (0.01) | 2.56 (0.11) |
| Follow-up | 16.8 (6.4) | 16.5 (6.9) | |||
| Sulcal CSF | Baseline | 69.1 (28.97) | 72.2 (34.76) | 6.55 (0.01) | 0.44 (0.51) |
| Follow-up | 85.9 (28.96) | 76.6 (32.35) |
Multivariate repeated measures analysis of covariance: Main effects of genotype on within-subject brain volume changes (dfs=1,113; covariates total brain compartment, age, interscan interval, treatment)
Antipsychotic treatment during inter-scan interval (dose years; 1 dose year=100mg chlorpromazine-equivalent/day for 1 year)
Multivariate repeated measures analysis of covariance: Main effects of antipsychotic treatment on within-subject brain volume changes (dfs=1,113; covariates total brain compartment, age, interscan interval, genotype)
Significant genotype main effects were also found on within-subject changes in lateral ventricles and sulcal CSF volumes (Table 2; F≥6.55, dfs=1,113, p≤0.01). Compared to baseline, Met-allele-carriers had significant enlargements in lateral ventricles and sulcal CSF volumes at follow-up assessment (Mean=1.30cc or 16.12cc respectively; T≥3.95, df=44, p≤0.0003). Within-subject changes in these CSF volumes were not statistically significant in Val homozygotes (T≤1.67, df=73, p≥0.10). Furthermore, differential changes in sulcal CSF volumes between genotype groupings were restricted to frontal and temporal lobes. Significant genotype main effects were found on within-subject changes in frontal CSF and temporal CSF volumes (F≥6.71, dfs=1,113, p≤0.01), but not in parietal CSF or occipital CSF volumes (F≤1.84, dfs=1,113, p≥0.18). Met-allele-carriers again showed greater frontal CSF (Mean=11.94cc) and temporal CSF (Mean=1.63cc) volume enlargements than Val homozygotes (Mean=4.69cc or −0.47cc respectively).
Antipsychotic treatment during inter-scan interval and its inter-relationships with brain volume changes and BDNF genotype groupings
To examine the inter-relationships between antipsychotic treatment and BDNF genotype on longitudinal MR brain volume changes, antipsychotic exposure during the inter-scan interval (dose years; 1 dose year=100mg CPZ-equivalent/day for 1 year) was included as a covariate in the repeated measures general linear models (Table 2). For frontal GM volume changes, antipsychotic treatment main effect approached but did not achieve statistical significance (F=3.22, dfs=1,113, p=0.08). There were no statistically significant antipsychotic treatment main effects on within subject changes in the other MRI brain volume measures either (F≤2.56 dfs=1,113, p≥0.11).
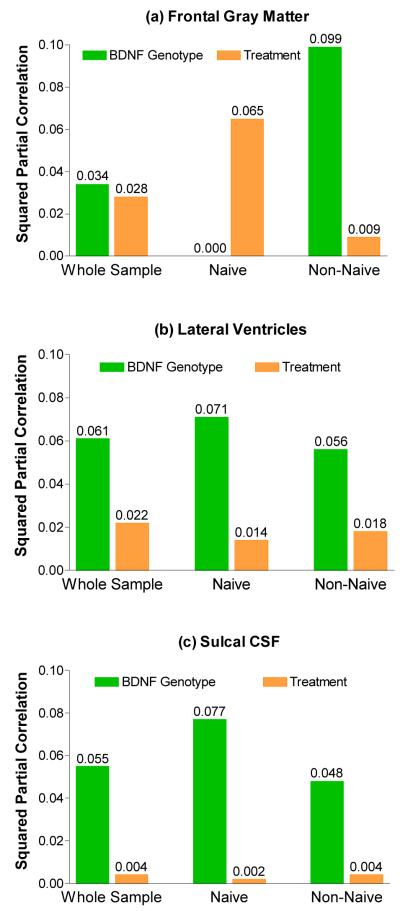
Additionally, for brain regions where there were significant repeated measures within-subject genotype main effects (i.e. frontal GM, lateral ventricles and sulcal CSF), we used regression analyses to explore the effects sizes and relative independent contributions from BDNF genotype and from antipsychotic exposure on variance in longitudinal brain volume changes. Type II squared partial correlations between brain volume changes and genotype grouping and between brain volume changes and treatment are summarized in Figure 1.
Figure 1.
Variance in MRI brain volume changes associated with BDNF genotype status and antipsychotic treatment.
BDNF genotype accounted for 3.4% (T=2.01, dfs=1,118, p=0.05) of the variance in frontal GM volume changes while antipsychotic treatment contributed an additional 2.8% (T=1.79, dfs=1,118, p=0.08) of variance in frontal GM volume changes (Figure 1a). Higher dose years correlated significantly with greater frontal GM volume reductions (Spearman partial r=−0.20, df=117, p=0.03). However, these inter-relationships varied according to antipsychotic treatment status at baseline scan.
For patients who had been neuroleptic naïve at baseline scan, antipsychotic treatment accounted for 6.5% (T=1.75, dfs=1,118, p=0.09) of variance in frontal GM changes while BDNF genotype had no independent contributions (squared partial r=0.00; T=0.05, p=0.96). Higher dose years correlated significantly with greater frontal GM volume reductions (Spearman partial r=−0.32, df=48, p=0.03). Conversely, among patients who had already been receiving antipsychotic treatment at the time of baseline scan, the relative independent contributions to variance in frontal GM volume changes were 9.9% from BDNF genotype (T=2.63, dfs=1,118, p=0.01), and 0.9% from antipsychotic treatment (T=0.76, dfs=1,118, p=0.45).
Variance in lateral ventricle and sulcal CSF volume changes accounted for by BDNF genotype were larger (~6%) than those from antipsychotic treatment (≤2%; Figure 1b and 1c). These inter-relationships did not differ substantially according to antipsychotic treatment status at baseline scan.
Longitudinal changes in neurocognition and symptom severity between BDNF genotype groupings
Least square means for cognitive domain scores and symptom severity at baseline and at follow-up assessment are summarized in Table 3. Each of the 5 cognitive domain scores improved significantly at follow-up (within-subject Time main effect; F≥8.19, dfs=1,109 or 1,113, p≤0.005). Negative symptoms at follow-up were also significantly less severe than at baseline (within-subject Time main effect; F=4.18, dfs=1,114, p=0.04). Severity of psychotic and disorganized symptoms declined at follow-up although these approached but did not achieve statistical significance (within-subject Time main effect; F≤3.53, dfs=1,114, p≥0.06).
Table 3.
Comparison of longitudinal changes in cognitive domain scores (Least Square Mean (SD) (z-score)) and symptom severity between 45 BDNF Met-allele carriers and 74 BDNF Val homozygous schizophrenia patients
| Met carriers | Val homozygotes |
Genotype F (p) a |
Treatment b F (p) c |
||
|---|---|---|---|---|---|
| Cognitive Domains | |||||
| Verbal Memory | Baseline | −0.18 (0.60) | 0.09 (0.64) | 0.65 (0.42) | 1.15 (0.29) |
| Follow-up | −0.16 (0.77) | 0.22 (0.71) | |||
| Speed/Attention | Baseline | −0.09 (0.58) | 0.04 (0.49) | 0.48 (0.49) | 0.27 (0.60) |
| Follow-up | −0.01 (0.66) | 0.06 (0.57) | |||
| Problem Solving | Baseline | −0.08 (0.37) | 0.04 (0.34) | 0.12 (0.73) | 4.67 (0.03) |
| Follow-up | −0.06 (0.51) | 0.08 (0.43) | |||
| Language | Baseline | 0.07 (0.60) | −0.01 (0.49) | 0.05 (0.83) | 0.05 (0.83) |
| Follow-up | 0.08 (0.64) | 0.01 (0.55) | |||
| Visuospatial Abilities | Baseline | −0.13 (0.54) | 0.06 (0.47) | 0.02 (0.89) | 12.27 (0.001) |
| Follow-up | −0.08 (0.74) | 0.09(0.58) | |||
| Symptom Domains d | |||||
| Psychotic | Baseline | 3.7 (2.3) | 3.4 (2.6) | 0.02 (0.88) | 0.01 (0.94) |
| Follow-up | 3.0 (2.4) | 2.7 (2.3) | |||
| Disorganized | Baseline | 2.4 (2.2) | 2.1 (2.4) | 2.26 (0.14) | 0.39 (0.54) |
| Follow-up | 1.7 (1.6) | 2.1 (2.3) | |||
| Negative | Baseline | 8.8 (3.9) | 9.3 (3.5) | 0.02 (0.89) | 0.30 (0.59) |
| Follow-up | 8.5 (3.3) | 8.9 (3.9) |
Multivariate repeated measures analysis of covariance: Main effects of genotype on within-subject brain volume changes (dfs=1,109 for verbal memory; dfs=1,113 for other cognitive domains; covariates full-scale IQ, age, interscan interval, treatment)
Antipsychotic treatment during inter-scan interval (dose years; 1 dose year=100mg chlorpromazine-equivalent/day for 1 year)
Multivariate repeated measures analysis of covariance: Main effects of antipsychotic treatment on within-subject brain volume changes (dfs=1,109 for verbal memory; dfs=1,113 for other cognitive domains; covariates full-scale IQ, age, interscan interval, genotype)
Psychotic symptom domain: sum of delusions and hallucinations global ratings from the SAPS; Disorganized symptom domain: sum of the bizarre (disorganized) behavior, positive thought disorder, and inappropriate affect global ratings from the SAPS; Negative symptom domain: sum of alogia, anhedonia, avolition, and affective flattening global ratings from the SANS
However, none of these longitudinal changes in neurocognition or in symptom severity differed significantly between genotype groupings. There were no significant genotype main effects on repeated measures within-subject changes in cognitive domain scores (Table 3; F≤0.65, dfs=1,109 or 1,113, p≥0.42) or in symptom severity (F≤2.26, dfs=1,114, p≥0.14). Antipsychotic treatment received during the interscan interval had no significant main effects on within-subject changes in symptom severity (F≤0.39, dfs=1,114, p≥0.54) or cognitive performance (F≤1.15, dfs=1,109 or 1,113, p≥0.29) except on Problem Solving and Visuospatial Abilities domain scores (F≥4.67, dfs=1,113, p≤0.03; partial r≥−0.20, df=118, p≤0.03).
There were significant between-subject genotype main effects on Verbal Memory, Problem Solving and Visuospatial Abilities domain scores (F≥4.19, dfs=1,109 or 1,113, p≤0.04). Met allele-carriers had greater impairment than Val homozygotes on these cognitive domains (univariate genotype main effects on baseline Verbal Memory domain score (F=4.65, dfs=1,114, p=0.03), follow-up Verbal Memory (F=6.44, dfs=1,114, p=0.01), baseline Problem Solving (Baseline: F=3.04, dfs=1,117, p=0.08), follow-up Problem Solving (F=2.85, dfs=1,117, p=0.09), baseline Visuospatial Abilities (F=4.53, dfs=1,117, p=0.03), and follow-up Visuospatial Abilities (F=2.49, dfs=1,117, p=0.12)). Between-subject genotype main effects on Speed/Attention and Language domain scores were not statistically significant (F≤0.78, dfs=1,113, p≥0.38). Symptom severity also did not differ significantly between genotype groupings (between-subject genotype main effects; F≤0.63, dfs=1,114, p≥0.43).
Differential effects of BDNF genotype on the relationships between frontal GM volume changes and longitudinal changes in neurocognition
Since Met allele carriers showed greater frontal GM volume reductions, we explored how longitudinal changes in frontal GM volume may be related to changes in neurocognition, and if such relationships differed between genotype groupings. We first tested the overall effect of frontal GM volume change scores on all five cognitive domain change scores in a joint omnibus multivariate regression test. Frontal GM volume change (follow-up volume minus baseline volume) was the independent variable. The 5 cognitive domain change scores were entered simultaneously as dependent variables. Covariates in the joint omnibus test were total brain compartment volume, age at intake scan, inter-scan interval and dose year. A frontal GM volume change-by-genotype interaction term was also entered in the regression model.
In the joint omnibus test, there was a significant overall main effect of frontal GM volume change on longitudinal changes in neurocognition (F=2.70, dfs=5,103, p=0.02). The frontal GM volume change-by-genotype interaction term was also statistically significant (F=3.75, dfs=5,103, p=0.004), which indicated that the relationships between frontal GM volume changes and changes in cognitive domain scores differed between genotype groupings. Pearson partial correlation coefficients for the relationships between frontal GM volume change scores and cognitive domain change scores within each genotype group are summarized in Table 4. Among Val homozygotes, enlargements in frontal GM volumes were significantly associated with worsening Verbal Memory performance (Table 4 and Supplementary Figure 1a; Pearson partial r=−0.32, df=69, p=0.007). In Met allele carriers, frontal GM volume reductions correlated with greater decline in Verbal Memory performance although this was not statistically significant (Pearson partial r=0.16, df=42, p=0.31). Post hoc univariate analyses found significant frontal GM volume change-by-genotype interaction effects on Verbal Memory change scores (F=8.52, dfs=1,114, p=0.004).
Table 4.
Relationships between MRI frontal gray matter volume changes and changes in cognitive domain scores across BDNF genotype groupings (Pearson partial ra (p))
| Cognitive Domains | Met carriers b | Val homozygotes c |
|---|---|---|
| Verbal memory | 0.16 (0.31) | −0.32 (0.007) |
| Speed/Attention | −0.02 (0.91) | −0.03 (0.81) |
| Problem solving | −0.00 (0.98) | 0.06 (0.65) |
| Language | −0.03 (0.85) | −0.16 (0.18) |
| Visuospatial abilities | 0.10 (0.54) | 0.28 (0.02) |
Adjusting for total brain compartment, age, interscan interval and dose year
df=42 for verbal memory; df=43 for others
df=69 for verbal memory; df=71 for others
Among Val homozygotes, reductions in frontal GM volume correlated significantly with worsening of Visuospatial Abilities (Table 4 and Supplementary Figure 1b; Pearson partial r=0.28, df=71, p=0.02). Although frontal GM volume-visuospatial relationships were weaker among Met allele carriers (Pearson partial r=0.10, df=43, p=0.54), the association was in the same direction as that observed among Val homozygotes. For Speed/Attention, Problem Solving and Language cognitive domains, there were no significant correlations between changes in frontal GM volumes and changes in cognitive domain scores (Table 4; Pearson partial ∣r∣≤0.16, df=43 or 71, p≥0.18).
Discussion
In this study, we investigated the effects of BNDF val66met genotype on longitudinal changes in MRI brain volumes, neurocognition and symptom severity early in the course of schizophrenia. We found Met-allele-carriers had greater reductions in frontal GM volume as well as greater expansions in lateral ventricles and sulcal (especially frontal and temporal) CSF volumes than Val homozygotes. Although the contributions from BDNF genotype and antipsychotic treatment on progressive frontal GM volume reductions were similarly modest in the overall sample, their relative effects appear to vary depending on intake antipsychotic treatment status. Even though Met allele carriers had poorer Verbal Memory and Visuospatial Abilities than Val homozygotes, longitudinal changes in cognition or in symptom severity did not differ between BDNF genotype groupings. Lastly, our study suggests that the relationships between frontal GM changes and changes in cognition may be different across BDNF genotypes, particularly with respect to verbal memory.
That Met-allele-carriers show progressive frontal GM reductions and larger CSF volume expansions than Val homozygotes are consistent with recent cross-sectional MRI studies (22, 26), which have reported associations between BDNFMet variant and smaller frontal and temporal GM volumes. The mechanisms by which BDNFMet variant affects brain volumes may be mediated via BDNF’s neurotrophic effects during neurodevelopment (30). Since BDNFMet variant is associated with inefficient intracellular BDNF trafficking and reduced BDNF secretion (20, 21), the resultant BDNF-deficient milieu during neurodevelopment may lead to diminished neuronal proliferation, fewer neurons, small soma size and reduced dendritic growth (17), and in turn smaller gross brain volumes measured using in vivo MR imaging. Our current findings of progressive brain volume changes among schizophrenia patients in their mid-20’s to early 30’s suggest that BDNFMet variant may also influence brain plasticity in young adults. Since BDNFMet variant reduces activity-dependent BDNF release (20, 21) and diminished BDNF signaling in mature neurons results in decreased dendritic arborization and neuronal loss (18), the progressive gross brain volume changes observed in this study may represent ongoing neuroplastic effects of BDNF.
Although our study suggests that BDNF val66met genotype status may be one of the factors mediating progressive brain volume changes after illness onset in schizophrenia, potential confounders need to be considered. Both genotype groupings were comparable with regard to well-replicated predictors of poor outcome in schizophrenia (i.e. poor premorbid social adjustment, early age of illness onset, and male gender). Thus, the association between BDNFMet variant and progressive brain volumetric deficits in schizophrenia appears to be unrelated to such predictors of poor outcome.
Another potential confounding factor is antipsychotic treatment. Long-term exposure to antipsychotics in monkeys has been shown to reduce fresh brain weights and volumes by ~10%, irrespective of haloperidol or olanzapine treatment (31). It has been suggested that these antipsychotic induced brain volume reductions may be related to reduced glial cell production, and to decreased dendritic arborization and dendritic spine density (32). In this study, we found BDNF genotype and antipsychotic treatment each independently accounted for approximately 3% of the variance in frontal GM changes for the whole sample. Greater antipsychotic treatment correlated with greater frontal GM volume reduction. However, the nature of this association cannot be satisfactorily resolved in a naturalistic study such as this. More antipsychotic treatment may simply be an indicator for illness severity. That is, patients with more severe forms of schizophrenia may not only received higher doses of antipsychotics, but they may also exhibit greater progressive frontal GM volume reductions because of the more deteriorative nature of their illnesses. Therefore, it is not possible to make causal inferences in a definitive manner. However, when viewed in conjunction with reduced fresh brain weights and volumes in monkeys chronically treated with haloperidol or olanzapine (31, 32), our findings do suggest that antipsychotic treatment may contribute to progressive frontal GM volume reductions in schizophrenia.
The relative prominence of antipsychotic treatment effects among initially neuroleptic naïve patients further supports the view that antipsychotics may play a role in mediating progressive frontal GM loss. In patients who had been neuroleptic naïve at intake scan, antipsychotic treatment accounted for ~7% of the variance in frontal GM volume reductions. On the other hand, the effects of antipsychotic treatment on frontal GM volume reductions were comparatively smaller (~1%) in patients who were already receiving antipsychotic treatment by the time of the intake MR scan. Among these initially non-naïve patients, most of the frontal GM volume reductions related to antipsychotic treatment may have already occurred prior to the intake scan; such that any additional frontal GM reductions during the inter-scan interval were predominantly associated with BDNF Met-allele-carrier status. This differential predominance of BDNF genotype and antipsychotic treatment effects on the variance in frontal GM volume reductions between the two sub-groups of patients in this study clearly requires replication. Future controlled treatment studies of first-episode and chronic schizophrenia patients are needed to further clarify the relative contributions of BDNF genotype and antipsychotic treatment on progressive brain volume changes.
What are the clinical implications of these findings? Does frontal GM volume reduction correlate with greater decline in cognition, and in particular, affecting Met-allele-carriers differently? In the joint omnibus test assessing brain volume-cognition overall relationship, we found frontal GM volume changes had significant effects on changes in cognition. Specifically, frontal GM volume reductions were associated with less improvement in Visuospatial Abilities regardless of BDNF genotype status. The brain volume-cognition relationships between BDNF genotypes for Verbal Memory are more complex to interpret. Frontal GM volume reductions non-significantly correlated with greater decline in Verbal Memory performance among Met-allele-carriers. As a group, Met-allele-carriers showed greater frontal GM volume reductions and had poorer Verbal Memory performance than Val homozygotes even though longitudinal changes in Verbal Memory scores were no different from cognitive changes seen in Val homozygotes. On the other hand, enlargements in frontal GM volumes were significantly associated with worsening Verbal Memory performance among Val homozygotes. Val homozygotes did not show significant longitudinal changes in frontal GM volumes or in Verbal Memory performance. The clinical significance of these divergent frontal GM-Verbal Memory relationships across BDNF genotype groupings remains unclear, and may have been more evident if we had similar frontal GM-Verbal Memory relationships from healthy volunteers to compare against. Therefore, future studies should seek to clarify the associations between brain volume and cognitive changes across BDNF genotype among healthy individuals without schizophrenia.
Even though our findings implicate antipsychotic treatment as a contributory factor for progressive frontal GM volume reductions in schizophrenia, and that frontal GM volume reductions correlate with greater cognitive decline, it is premature to suggest changing the current status of antipsychotics as the mainstay treatment for schizophrenia. There is a substantial body of literature supporting the efficacy of antipsychotics in ameliorating psychotic symptoms and in reducing the risk of symptom recurrence in schizophrenia (45). Recurrence of psychotic symptoms often causes severe disruptions to the lives of patients and family members, and can have devastating consequences. Minimizing the risk of psychotic relapses through maintenance antipsychotic treatment remains an important goal in the long term treatment of patients with schizophrenia. Although this class of drugs may be the best we currently have to offer patients, recent large scale clinical trials have reiterated the limitations of antipsychotics in the management of schizophrenia (46, 47). Besides targeting psychotic symptoms, major efforts are already underway to address the current lack of available treatments for cognitive deficits and negative symptoms of schizophrenia (48, 49). However, beyond antipsychotic, pro-cognition agents and treatments for negative symptoms, there is a further need for interventions that target the fundamental pathophysiological processes underlying schizophrenia, including therapies that limit progressive brain volume reductions. A major challenge in developing novel treatments against schizophrenia is our current limited understanding of the factors mediating progressive neural changes in schizophrenia. Nonetheless, if putative BDNF-deficient Met-allele-carriers show greater frontal GM volume reductions, pharmacological strategies that increase BDNF bioavailability (50) and enhance the neuroplastic effects of BDNF could potentially begin to address the current unmet need for interventions that curb ongoing brain volume reductions in schizophrenia.
In conclusion, schizophrenia is characterized by subtle, ongoing brain tissue volume reductions following illness onset. Factors and mechanisms underlying progressive brain volume reductions require continued investigation so as to develop treatments that may more radically address the pathophysiology of schizophrenia. Our study suggests that BDNF, through its influence on neuroplasticity, contributes to progressive brain volume changes in schizophrenia.
Supplementary Material
Acknowledgments
This research was supported in part by NIMH Grants MH68380, MH31593, MH40856 and MH43271
References
- 1.Schulz SC, Koller MM, Kishore PR, Hamer RM, Gehl JJ, Friedel RO. Ventricular enlargement in teenage patients with schizophrenia spectrum disorder. Am J Psychiatry. 1983;140(12):1592–5. doi: 10.1176/ajp.140.12.1592. [DOI] [PubMed] [Google Scholar]
- 2.Illowsky BP, Juliano DM, Bigelow LB, Weinberger DR. Stability of CT scan findings in schizophrenia: results of an 8 year follow-up study. J Neurol Neurosurg Psychiatry. 1988;51(2):209–13. doi: 10.1136/jnnp.51.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeLisi LE, Sakuma M, Tew W, Kushner M, Hoff AL, Grimson R. Schizophrenia as a chronic active brain process: a study of progressive brain structural change subsequent to the onset of schizophrenia. Psychiatry Res. 1997;74(3):129–40. doi: 10.1016/s0925-4927(97)00012-7. [DOI] [PubMed] [Google Scholar]
- 4.Gur RE, Cowell P, Turetsky BI, Gallacher F, Cannon T, Bilker W, Gur RC. A follow-up magnetic resonance imaging study of schizophrenia. Relationship of neuroanatomical changes to clinical and neurobehavioral measures. Arch Gen Psychiatry. 1998;55(2):145–52. doi: 10.1001/archpsyc.55.2.145. [DOI] [PubMed] [Google Scholar]
- 5.Lieberman J, Chakos M, Wu H, Alvir J, Hoffman E, Robinson D, Bilder R. Longitudinal study of brain morphology in first episode schizophrenia. Biol Psychiatry. 2001;49(6):487–99. doi: 10.1016/s0006-3223(01)01067-8. [DOI] [PubMed] [Google Scholar]
- 6.Mathalon DH, Sullivan EV, Lim KO, Pfefferbaum A. Progressive brain volume changes and the clinical course of schizophrenia in men: a longitudinal magnetic resonance imaging study. Arch Gen Psychiatry. 2001;58(2):148–57. doi: 10.1001/archpsyc.58.2.148. [DOI] [PubMed] [Google Scholar]
- 7.Cahn W, Pol HE, Lems EB, Van Haren NE, Schnack HG, Van Der Linden JA, Schothorst PF, Van Engeland H, Kahn RS. Brain Volume Changes in First-Episode Schizophrenia: A 1-Year Follow-up Study. Arch Gen Psychiatry. 2002;59(11):1002–10. doi: 10.1001/archpsyc.59.11.1002. [DOI] [PubMed] [Google Scholar]
- 8.Ho BC, Andreasen NC, Nopoulos P, Arndt S, Magnotta V, Flaum M. Progressive structural brain abnormalities and their relationship to clinical outcome: a longitudinal magnetic resonance imaging study early in schizophrenia. Arch Gen Psychiatry. 2003;60(6):585–94. doi: 10.1001/archpsyc.60.6.585. [DOI] [PubMed] [Google Scholar]
- 9.Kasai K, Shenton ME, Salisbury DF, Hirayasu Y, Onitsuka T, Spencer MH, Yurgelun-Todd DA, Kikinis R, Jolesz FA, McCarley RW. Progressive Decrease of Left Heschl Gyrus and Planum Temporale Gray Matter Volume in First-Episode Schizophrenia: A Longitudinal Magnetic Resonance Imaging Study. Arch Gen Psychiatry. 2003;60(8):766–775. doi: 10.1001/archpsyc.60.8.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lieberman JA, Tollefson GD, Charles C, Zipursky R, Sharma T, Kahn RS, Keefe RSE, Green AI, Gur RE, McEvoy J, Perkins D, Hamer RM, Gu H, Tohen M, for the HSG Antipsychotic Drug Effects on Brain Morphology in First-Episode Psychosis. Arch Gen Psychiatry. 2005;62(4):361–370. doi: 10.1001/archpsyc.62.4.361. [DOI] [PubMed] [Google Scholar]
- 11.Pantelis C, Yucel M, Wood SJ, Velakoulis D, Sun D, Berger G, Stuart GW, Yung A, Phillips L, McGorry PD. Structural Brain Imaging Evidence for Multiple Pathological Processes at Different Stages of Brain Development in Schizophrenia. Schizophr Bull. 2005;31(3):672–696. doi: 10.1093/schbul/sbi034. [DOI] [PubMed] [Google Scholar]
- 12.Lim KO, Tew W, Kushner M, Chow K, Matsumoto B, DeLisi LE. Cortical gray matter volume deficit in patients with first-episode schizophrenia. Am J Psychiatry. 1996;153(12):1548–53. doi: 10.1176/ajp.153.12.1548. [DOI] [PubMed] [Google Scholar]
- 13.Velakoulis D, Wood SJ, Smith DJ, Soulsby B, Brewer W, Leeton L, Desmond P, Suckling J, Bullmore ET, McGuire PK, Pantelis C. Increased duration of illness is associated with reduced volume in right medial temporal/anterior cingulate grey matter in patients with chronic schizophrenia. Schizophr Res. 2002;57(1):43–9. doi: 10.1016/s0920-9964(01)00307-3. [DOI] [PubMed] [Google Scholar]
- 14.Molina V, Sanz J, Sarramea F, Benito C, Palomo T. Lower prefrontal gray matter volume in schizophrenia in chronic but not in first episode schizophrenia patients. Psychiatry Res. 2004;131(1):45–56. doi: 10.1016/j.pscychresns.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Mathalon DH, Rapoport JL, Davis KL, Krystal JH. Neurotoxicity, Neuroplasticity, and Magnetic Resonance Imaging Morphometry. Arch Gen Psychiatry. 2003;60(8):846–848. doi: 10.1001/archpsyc.60.8.846. [DOI] [PubMed] [Google Scholar]
- 16.Weinberger DR, McClure RK. Neurotoxicity, Neuroplasticity, and Magnetic Resonance Imaging Morphometry--Reply. Arch Gen Psychiatry. 2003;60(8):848–849. doi: 10.1001/archpsyc.60.8.846. [DOI] [PubMed] [Google Scholar]
- 17.Gorski JA, Zeiler SR, Tamowski S, Jones KR. Brain-derived neurotrophic factor is required for the maintenance of cortical dendrites. J Neurosci. 2003;23(17):6856–65. doi: 10.1523/JNEUROSCI.23-17-06856.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu B, Zang K, Ruff NL, Zhang YA, McConnell SK, Stryker MP, Reichardt LF. Cortical Degeneration in the Absence of Neurotrophin Signaling: Dendritic Retraction and Neuronal Loss after Removal of the Receptor TrkB. Neuron. 2000;26(1):233–45. doi: 10.1016/s0896-6273(00)81153-8. [DOI] [PubMed] [Google Scholar]
- 19.Lu B. BDNF and activity-dependent synaptic modulation. Learn Mem. 2003;10(2):86–98. doi: 10.1101/lm.54603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen ZY, Patel PD, Sant G, Meng CX, Teng KK, Hempstead BL, Lee FS. Variant brain-derived neurotrophic factor (BDNF) (Met66) alters the intracellular trafficking and activity-dependent secretion of wild-type BDNF in neurosecretory cells and cortical neurons. J Neurosci. 2004;24(18):4401–11. doi: 10.1523/JNEUROSCI.0348-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Egan MF, Kojima M, Callicott JH, Goldberg TE, Kolachana BS, Bertolino A, Zaitsev E, Gold B, Goldman D, Dean M, Lu B, Weinberger DR. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112(2):257–69. doi: 10.1016/s0092-8674(03)00035-7. [DOI] [PubMed] [Google Scholar]
- 22.Ho BC, Milev P, O’Leary DS, Librant A, Andreasen NC, Wassink TH. Cognitive and magnetic resonance imaging brain morphometric correlates of brain-derived neurotrophic factor Val66Met gene polymorphism in patients with schizophrenia and healthy volunteers. Arch Gen Psychiatry. 2006;63(7):731–40. doi: 10.1001/archpsyc.63.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hariri AR, Goldberg TE, Mattay VS, Kolachana BS, Callicott JH, Egan MF, Weinberger DR. Brain-derived neurotrophic factor val66met polymorphism affects human memory-related hippocampal activity and predicts memory performance. J Neurosci. 2003;23(17):6690–4. doi: 10.1523/JNEUROSCI.23-17-06690.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pezawas L, Verchinski BA, Mattay VS, Callicott JH, Kolachana BS, Straub RE, Egan MF, Meyer-Lindenberg A, Weinberger DR. The brain-derived neurotrophic factor val66met polymorphism and variation in human cortical morphology. J Neurosci. 2004;24(45):10099–102. doi: 10.1523/JNEUROSCI.2680-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dempster E, Toulopoulou T, McDonald C, Bramon E, Walshe M, Filbey F, Wickham H, Sham PC, Murray RM, Collier DA. Association between BDNF val66 met genotype and episodic memory. Am J Med Genet B Neuropsychiatr Genet. 2005;134(1):73–5. doi: 10.1002/ajmg.b.30150. [DOI] [PubMed] [Google Scholar]
- 26.Szeszko PR, Lipsky R, Mentschel C, Robinson D, Gunduz-Bruce H, Sevy S, Ashtari M, Napolitano B, Bilder RM, Kane JM, Goldman D, Malhotra AK. Brain-derived neurotrophic factor Val66met polymorphism and volume of the hippocampal formation. Mol Psychiatry. 2005;10(7):631–6. doi: 10.1038/sj.mp.4001656. [DOI] [PubMed] [Google Scholar]
- 27.Agartz I, Sedvall GC, Terenius L, Kulle B, Frigessi A, Hall H, Jonsson EG. BDNF gene variants and brain morphology in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2006;141(5):513–23. doi: 10.1002/ajmg.b.30338. [DOI] [PubMed] [Google Scholar]
- 28.Rattenholl A, Lilie H, Grossmann A, Stern A, Schwarz E, Rudolph R. The pro-sequence facilitates folding of human nerve growth factor from Escherichia coli inclusion bodies. Eur J Biochem. 2001;268(11):3296–303. doi: 10.1046/j.1432-1327.2001.02232.x. [DOI] [PubMed] [Google Scholar]
- 29.Huang EJ, Reichardt LF. Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci. 2001;24:677–736. doi: 10.1146/annurev.neuro.24.1.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lessmann V, Gottmann K, Malcangio M. Neurotrophin secretion: current facts and future prospects. Prog Neurobiol. 2003;69(5):341–74. doi: 10.1016/s0301-0082(03)00019-4. [DOI] [PubMed] [Google Scholar]
- 31.Dorph-Petersen KA, Pierri JN, Perel JM, Sun Z, Sampson AR, Lewis DA. The Influence of Chronic Exposure to Antipsychotic Medications on Brain Size before and after Tissue Fixation: A Comparison of Haloperidol and Olanzapine in Macaque Monkeys. Neuropsychopharmacology. 2005;30(9):1649–61. doi: 10.1038/sj.npp.1300710. [DOI] [PubMed] [Google Scholar]
- 32.Konopaske GT, Dorph-Petersen K-A, Pierri JN, Wu Q, Sampson AR, Lewis DA. Effect of Chronic Exposure to Antipsychotic Medication on Cell Numbers in the Parietal Cortex of Macaque Monkeys. Neuropsychopharmacology. 2006 doi: 10.1038/sj.npp.1301233. advance online publication 25 October 2006; doi: 10.1038/sj.npp.1301233. [DOI] [PubMed] [Google Scholar]
- 33.Chakos MH, Shirakawa O, Lieberman J, Lee H, Bilder R, Tamminga CA. Striatal enlargement in rats chronically treated with neuroleptic. Biol Psychiatry. 1998;44(8):675–84. doi: 10.1016/s0006-3223(98)00029-8. [DOI] [PubMed] [Google Scholar]
- 34.Andersson C, Hamer RM, Lawler CP, Mailman RB, Lieberman JA. Striatal volume changes in the rat following long-term administration of typical and atypical antipsychotic drugs. Neuropsychopharmacology. 2002;27(2):143–51. doi: 10.1016/S0893-133X(02)00287-7. [DOI] [PubMed] [Google Scholar]
- 35.Chakos MH, Lieberman JA, Bilder RM, Borenstein M, Lerner G, Bogerts B, Wu H, Kinon B, Ashtari M. Increase in caudate nuclei volumes of first-episode schizophrenic patients taking antipsychotic drugs. Am J Psychiatry. 1994;151(10):1430–6. doi: 10.1176/ajp.151.10.1430. [DOI] [PubMed] [Google Scholar]
- 36.McCormick L, Decker L, Nopoulos P, Ho BC, Andreasen N. Effects of atypical and typical neuroleptics on anterior cingulate volume in schizophrenia. Schizophr Res. 2005;80(1):73–84. doi: 10.1016/j.schres.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 37.Dazzan P, Morgan KD, Orr K, Hutchinson G, Chitnis X, Suckling J, Fearon P, McGuire PK, Mallett RM, Jones PB, Leff J, Murray RM. Different effects of typical and atypical antipsychotics on grey matter in first episode psychosis: the AESOP study. Neuropsychopharmacology. 2005;30(4):765–74. doi: 10.1038/sj.npp.1300603. [DOI] [PubMed] [Google Scholar]
- 38.Flaum MA, Andreasen NC, Arndt S. The Iowa prospective longitudinal study of recent-onset psychoses. Schiz Bull. 1992;18(3):481–90. doi: 10.1093/schbul/18.3.481. [DOI] [PubMed] [Google Scholar]
- 39.Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry. 1992;49(8):615–23. doi: 10.1001/archpsyc.1992.01820080023004. [DOI] [PubMed] [Google Scholar]
- 40.Andreasen NC, Rajarethinam R, Cizadlo T, Arndt S, Swayze VW, 2nd, Flashman LA, O’Leary DS, Ehrhardt JC, Yuh WT. Automatic atlas-based volume estimation of human brain regions from MR images. J Comput Assist Tomogr. 1996;20(1):98–106. doi: 10.1097/00004728-199601000-00018. [DOI] [PubMed] [Google Scholar]
- 41.Harris G, Andreasen NC, Cizadlo T, Bailey JM, Bockholt HJ, Magnotta VA, Arndt S. Improving tissue classification in MRI: a three-dimensional multispectral discriminant analysis method with automated training class selection. J Comput Assist Tomogr. 1999;23(1):144–54. doi: 10.1097/00004728-199901000-00030. [DOI] [PubMed] [Google Scholar]
- 42.Milev P, Ho BC, Arndt S, Andreasen NC. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry. 2005;162(3):495–506. doi: 10.1176/appi.ajp.162.3.495. [DOI] [PubMed] [Google Scholar]
- 43.Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P, Gur RC. Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry. 1994;51(2):124–31. doi: 10.1001/archpsyc.1994.03950020048005. [DOI] [PubMed] [Google Scholar]
- 44.Ho BC, Alicata D, Ward J, Moser DJ, O’Leary DS, Arndt S, Andreasen NC. Untreated initial psychosis: relation to cognitive deficits and brain morphology in first-episode schizophrenia. Am J Psychiatry. 2003;160(1):142–8. doi: 10.1176/appi.ajp.160.1.142. [DOI] [PubMed] [Google Scholar]
- 45.Davis JM, Kane JM, Marder SR, Brauzer B, Gierl B, Schooler N, Casey DE, Hassan M. Dose response of prophylactic antipsychotics. J Clin Psychiatry. 1993;54(Suppl):24–30. [PubMed] [Google Scholar]
- 46.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 47.Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, Murray RM, Markwick A, Lewis SW. Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1) Arch Gen Psychiatry. 2006;63(10):1079–87. doi: 10.1001/archpsyc.63.10.1079. [DOI] [PubMed] [Google Scholar]
- 48.Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schiz Res. 2004;72(1):5. doi: 10.1016/j.schres.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 49.Kirkpatrick B, Fenton WS, Carpenter WT, Jr., Marder SR. The NIMH-MATRICS Consensus Statement on Negative Symptoms. Schizophr Bull. 2006;32(2):214–219. doi: 10.1093/schbul/sbj053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Leary PD, Hughes RA. Design of potent peptide mimetics of brain-derived neurotrophic factor. J Biol Chem. 2003;278(28):25738–44. doi: 10.1074/jbc.M303209200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.