Abstract
Sweet's syndrome (SS) is an acute neutrophilic dermatosis characterised by abrupt onset of fever, leukocytosis and cutaneous eruption, with dermal neutrophilia on skin biopsy. Most cases are idiopathic but SS can be associated with various affections, especially neoplastic, inflammatory and infectious diseases. The authors report the case of an SS occurring in a patient with a known rheumatoid arthritis associated with a secondary Sjögren's syndrome, with incidental finding of concurrent lymph node tuberculosis. In case of SS, an associated disease (malignant, inflammatory or infectious diseases) must imperatively be searched for, knowing that two or more of these affections can coexist.
Background
Sweet's syndrome (SS) is the most common neutrophilic dermatosis (ND). It is most often idiopathic but may be associated with a wide range of diseases, especially malignant conditions, infectious diseases or inflammatory diseases.
Case presentation
We report the case of a 28-year-old woman with a 2-year history of seropositive and destructive rheumatoid arthritis (RA) associated with a secondary Sjögren's syndrome, who was treated by methotrexate (15 mg/week) and low-dose prednisone (5 mg/day). She presented with a widespread cutaneous eruption that involved the face, trunk and four limbs, associated with fever, arthralgia, bilateral conjunctivitis and deterioration of general condition. This symptomatology occurs 5 days after a nasopharyngitis. Clinical examination objectified the fever at 38.5 °C and demonstrated well-demarcated erythematous papules, with centrifugal extension involving the face, arm, back of the upper limbs, palms and knees (figure 1). Some of the papules were arranged in an annular pattern or became confluent to form plaques especially on the forehead and ears.
Figure 1.

Lesions of the arm: well-demarcated erythematous papules with centrifugal extension.
Investigations
Laboratory examinations found increased erythrocyte sedimentation rate (116 mm at the first hour), increased C reactive protein rate (120 mg/l) and leukocytosis with a neutrophil count of 8640 cells/mm3. A skin biopsy revealed a dense extensive neutrophilic infiltrate throughout the dermis with prominent oedema, mild endothelial swelling but no vasculitis was noted (figure 2).
Figure 2.
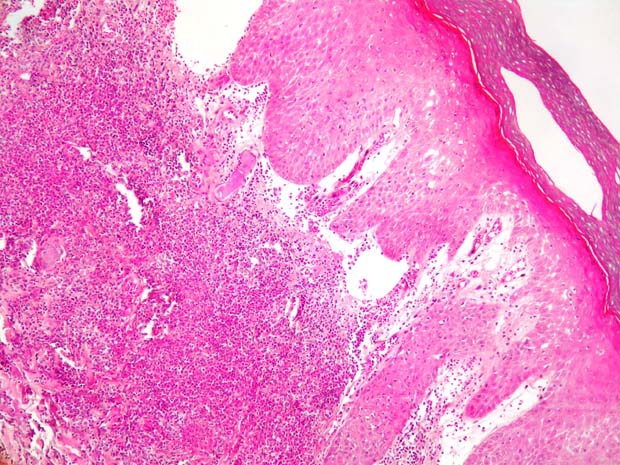
Skin biopsy H&E ×100: dense extensive neutrophilic infiltrate throughout the dermis, with prominent oedema in the upper dermis.
SS diagnosis has been retained according to the criteria developed by Su and Liu and modified by Von den Driesch.1 In addition to the two major criteria (abrupt onset of typical skin lesions and neutrophilic infiltration of the dermis), the patient had three minor criteria (fever and elevation in the erythrocyte sedimentation rate, C reactive protein level and neutrophil count). During follow-up, the systematic clinical examination also showed mobile and painless cervical lymph nodes. Cervical ultrasound revealed multiple cervical lymph nodes, the largest one measuring 5 cm long axis. The lymph node aspiration cytology was inconclusive. A tuberculin reaction was positive and the sputum test for Mycobacterium tuberculosis was negative. Chest x-ray was normal. A surgical adenomectomy has also been performed and histology confirmed the diagnosis of lymph node tuberculosis.
Treatment
An antitubercular therapy was initiated (2 months quadruple therapy on isoniazide, rifampicin, ethambutol and pyazoline, followed by 6-month bitherapy on isoniazide and rifampicin) with a favourable evolution.
Outcome and follow-up
No recurrence of SS was noted during 2-year follow-up.
Discussion
ND and especially SS are frequently associated with various affections, including inflammatory and infectious diseases. The association of SS to RA is classical, recently a new form of ND, rheumatoid ND, has even been reported in patients with severe RA.2 Also, several cases of SS associated with Sjögren's syndrome were reported in the literature.3 4 Some cases have also been described during or subsequently to an infectious disease.5 The association of SS with tuberculosis is not common, only few cases have been described in literature.6–8 In our case, SS occurs in a patient with a known RA associated with a secondary Sjögren's syndrome, with incidental finding of concurrent lymph node tuberculosis; this association has not been described previously to our knowledge.
Learning points.
-
▶
In case of SS, we must first search for a malignant condition (haematological or solid neoplasm) or more rarely an inflammatory disease (eg, RA, primary or secondary Sjögren's syndrome, systemic lupus erythematosus) or infectious disease (eg, tuberculosis).
-
▶
Two or more of these conditions can coexist.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.von den Driesch P. Sweet's syndrome (acute febrile neutrophilic dermatosis). J Am Acad Dermatol 1994;31:535–56; quiz 557–60 [DOI] [PubMed] [Google Scholar]
- 2.Lu CI, Yang CH, Hong HS. A bullous neutrophilic dermatosis in a patient with severe rheumatoid arthritis and monoclonal IgA gammopathy. J Am Acad Dermatol 2004;51(2 Suppl):S94–6 [DOI] [PubMed] [Google Scholar]
- 3.Osawa H, Yamabe H, Seino S, et al. A case of Sjögren's syndrome associated with Sweet's syndrome. Clin Rheumatol 1997;16:101–5 [DOI] [PubMed] [Google Scholar]
- 4.Bianconcini G, Mazzali F, Candini R, et al. Sweet's syndrome (acute febrile neutrophilic dermatosis) associated with Sjögren's syndrome. A clinical case. Minerva Med 1991;82:869–76 [PubMed] [Google Scholar]
- 5.Chen HH, Hsiao CH, Chiu HC. Successive development of cutaneous polyarteritis nodosa, leucocytoclastic vasculitis and Sweet's syndrome in a patient with cervical lymphadenitis caused by Mycobacterium fortuitum. Br J Dermatol 2004;151:1096–100 [DOI] [PubMed] [Google Scholar]
- 6.Singh RK. Acute febrile neutrophilic dermatosis following tuberculous infection. J Assoc Physicians India 2002;50:1322–3 [PubMed] [Google Scholar]
- 7.Abbyad R, Olivier V, Vandenbos F, et al. Tuberculosis discovered in a patient with Sweet's syndrome. Presse Med 2001;30:166. [PubMed] [Google Scholar]
- 8.Hsiao GH, Chiu HC. Atypical mycobacterial cervical lymphadenitis associated with Sweet's syndrome. Acta Derm Venereol 1995;75:237–9 [DOI] [PubMed] [Google Scholar]


