Abstract
Objective To examine mediating processes linking parental involvement to diabetes management (adherence and metabolic control) during adolescence. Methods A total of 252 young adolescents (M age = 12.49 years, SD = 1.53, 53.6% females) with type 1 diabetes reported their parents’ involvement in diabetes management (relationship quality, monitoring, and behavioral involvement), their own externalizing and internalizing behaviors, diabetes-self efficacy, and adherence behaviors. HbA1c was drawn from medical records. Results SEM analyses indicated that the associations of mothers’ and fathers’ relationship quality with diabetes outcomes were mediated by adolescents’ perceptions of self-efficacy and externalizing behaviors, and the associations of fathers’ monitoring and behavioral involvement with adherence were partially mediated by adolescents’ self-efficacy. There were also direct (non-mediated) associations between mothers’ monitoring and adherence, and fathers’ monitoring and adherence and metabolic control. Conclusions Quality of the parent–adolescent relationship and monitoring are important for better adherence and metabolic control among adolescents through higher diabetes self-efficacy.
Keywords: adherence, metabolic control, parental involvement, self-efficacy, type 1 diabetes
Optimal diabetes management during adolescence involves sustained levels of parental involvement across this time (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997; Wysocki et al., 1996). Both adherence and metabolic control are enhanced when parents are involved with their adolescent through a high quality relationship (Miller-Johnson et al., 1994), actively monitoring their adolescents’ behavior (Berg et al., 2008; Ellis et al., 2007) and behavioral management in diabetes tasks (Wysocki et al., 1996). Although parental involvement is beneficial for diabetes management, we know very little about the process whereby it is linked with diabetes outcomes and whether this process is similar for mothers’ versus fathers’ involvement. In the present study we examined how young adolescents’ perspectives of three facets of parental involvement (relationship quality, monitoring, and behavioral involvement) related to better adherence and metabolic control and tested the mediating role of adolescents’ perceptions of diabetes self efficacy and internalizing (i.e., withdrawn, anxiety, depressive, and somatic complaints) and externalizing (i.e., rule-breaking and aggression) behaviors.
Consistent with developmental considerations of parental involvement (Beveridge & Berg, 2007; Dishion & McMahon, 1998), analyses based on the same dataset for the present study demonstrated that young adolescents’ perspectives of both maternal and paternal involvement were comprised of three interrelated latent factors (Palmer et al., in press): relationship quality, monitoring, and behavioral involvement. Each of these facets of parental involvement has been associated with diabetes outcomes. High-quality relationships characterized by acceptance from parents facilitate better adherence and metabolic control (Miller-Johnson et al., 1994; Skinner, John, & Hampson, 2000). Parental monitoring, consisting of regular contact with adolescents regarding their daily activities and knowledge about those activities (Dishion & McMahon, 1998), has been linked to better adherence and metabolic control (Berg et al., 2008; Ellis et al., 2007). Behavioral involvement (e.g., daily assistance regarding diabetes activities) has also been associated with better diabetes management (Anderson et al., 1997; Wysocki et al., 1996). The current study extends our prior work by examining the mechanisms linking parental involvement to adherence and metabolic control.
Parental involvement may affect adherence and, in turn, metabolic control by reducing risk factors in the young adolescent (Beveridge & Berg, 2007). This may be particularly true in young adolescents as they become more independently responsible for their diabetes management (Palmer et al., 2009) and spend more time away from home (Larson & Richards, 1991). In the diabetes literature, high quality relationships are associated with an array of positive adolescent processes including reduced risk of externalizing and internalizing behaviors (Paley, Conger, & Gordon, 2000). Studies from the developmental literature reveal high quality parent–adolescent relationships are associated with lower internalizing behaviors (Beveridge & Berg, 2007) and lower internalizing behaviors predict better adherence in young adolescents with diabetes (Korbel, Wiebe, Berg, & Palmer, 2007). Parental monitoring of general adolescent behaviors (e.g., knowing who your child’s friends are) may reduce risky behaviors such as externalizing behaviors, which can indirectly affect positive diabetes outcomes (Horton, Berg, & Wiebe, 2009). Monitoring of adolescents’ behavior may also have a more direct effect on positive diabetes management outcomes by restricting adolescents’ behavior so that metabolic control is improved (e.g., restricting adolescents from eating at fast food restaurants with friends because of their poor food choices). Finally, behavioral involvement may promote good metabolic control by increasing adolescents’ adherence to self-care tasks (Anderson et al., 1997; Palmer et al., 2009; Wysocki et al., 1996).
Parental involvement may also promote adherence and good metabolic control by fostering protective factors such as self-efficacy, which is especially important as young adolescents increasingly find themselves in problematic settings away from their parents (Beveridge, Berg, Wiebe, & Palmer, 2006). Parents are thought to play an important role in the development of their children’s self-efficacy, with self-efficacy being highest when parents support their autonomy and are involved in their daily lives (Pomerantz and Eaton, 2001). A high quality relationship characterized by acceptance, independence encouragement, and open communication may promote positive self-efficacy, which in turn may lead to adaptive behavior (Bandura, 1997; Bong, 2008). In support of this idea, self-efficacy for diabetes management mediated the relationship between support of family and friends and better regimen adherence in adolescents with diabetes (Skinner et al., 2000).
Parental involvement has typically been examined in the context of the mother-child relationship, with fathers thought to serve largely a supportive role to mothers’ efforts (Quittner & DeGirolamo, 1998). Nevertheless, paternal influences have particular significance during the transition from childhood to adolescence (Gavin & Wysocki, 2006; Schulman & Seiffge-Krenke, 1997) and adolescents are at highest risk when mothers and fathers are both involved at low levels (Wysocki et al., 2009). In our own work examining mothers’ and fathers’ involvement simultaneously, fathers’ monitoring was uniquely related to diabetes outcomes, particularly when fathers displayed low levels of monitoring (Berg et al., 2008).
In the present study, we examined whether relationship quality, monitoring, and behavioral involvement were associated with adherence and metabolic control by reducing externalizing and internalizing behaviors and promoting self-efficacy. Through structural equation modeling (SEM) of young adolescents’ perceptions of mothers’ and fathers’ involvement we examined possible indirect and direct pathways between parental involvement and metabolic control through risk and protective factors. We predicted that both relationship quality and monitoring would predict higher adherence and lower HbA1c by reducing risk (externalizing and internalizing) and bolstering self-efficacy. However, our previous work indicates that relationship quality and monitoring are related (Palmer et al., in press) and may not uniquely affect diabetes outcomes when examined together.
Methods
Participants
Participants included 252 young adolescents (M age = 12.49 years, SD = 1.53, 53.6% females) diagnosed with type 1 diabetes mellitus, their mothers (M age = 39.64 years, SD = 6.34) and 188 fathers (M age = 42.08 years, SD = 6.32) recruited from a university/private partnership (76%) and a community-based private practice (24%), that followed similar treatment and clinic procedures. Eligibility criteria included that young adolescents were between 10 and 14 years of age, had diabetes more than 1 year (M = 4.13 years, SD = 3), and were able to read and write either English or Spanish. For each adolescent, one mother and one father were eligible to participate. Adolescents were required to be living with their participating mother. Step-mothers or adoptive mothers (3.2%) were eligible if they had lived with the adolescent for at least 1 year. If both a biological father and a step-father or adoptive father were eligible for participation, we recruited the father that adolescents reported was most involved in their diabetes management (74.6% of fathers were biological). Families were largely Caucasian (94%) and middle class with most (73%) reporting household incomes averaging $50,000 or more annually, 51% of mothers and 58% of fathers reporting education levels of associate’s (2-year college) degrees or beyond, and an average Hollingshead Index value of 42.04, indicating an average medium business, minor professional, technical status.
Of the qualifying individuals approached, 66% agreed to participate in the study, the first wave of a 3-year longitudinal study (most common reasons for refusal included distance of commute 18%, too busy 21%, not interested 30%, uncomfortable with being studied 14%, and time commitment 5%). Comparisons of eligible adolescents who participated versus those who did not indicated that participants versus non-participants were older (12.5 vs. 11.6 years, t (367) = 6.2, p < .01, η2 = .10) but did not differ on gender, pump status, Hba1c or time since diagnosis (p's > .20). Approximately half (50.8%) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI). Mothers of adolescents on MDI reported physicians recommended an average of 4.14 insulin injections (SD = 1.81, range: 0–10) and 5.53 blood glucose checks per day (SD = 1.70, range: 1–11).
Procedure
The study was approved by the appropriate Institutional Review Board, with parents providing informed consent and adolescents written assent to participate. At their diabetes clinics participants received questionnaires to be completed individually prior to a laboratory appointment where they completed additional questionnaires. The measures reported here are a subset of those included in the larger study. The present study uses our prior work examining measurement models for parental involvement (Palmer et al., in press) as the basis for our modeling.
Measures
Descriptive statistics for all measures for the current study can be found in Table I.
Table I.
Correlations and Descriptive Statistics for Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Acceptance (M) | 1.00 | .58** | .59** | .44** | .53** | .28** | .08 | .10 | .10 | .18** | .33** | .35** | .27** | .24** | −.23** | −.27** | .29** | .29** | −.14* |
| 2. Acceptance (F) | 1.00 | .33** | .68** | .37** | .54** | .00 | .24** | −.03 | .31** | .23** | .47** | .14* | .39** | −.26** | −.28** | .26** | .34** | −.22** | |
| 3. Independence & encouragement (M) | 1.00 | .56** | .37** | .03 | .03 | −.06 | .06 | −.03 | .37** | .16** | .31** | .10 | −.22** | −.19** | .28** | .27** | −.03 | ||
| 4. Independence & encouragement (F) | 1.00 | .26** | .32** | .00 | .17** | −.04 | .25** | .27** | .50** | .22** | .39** | −.17** | −.21** | .19** | .28** | −.15* | |||
| 5. Communication (M) | 1.00 | .50** | .09 | .13* | .10 | .18** | .34** | .26** | .30** | .24** | −.30** | −.31** | .23** | .27** | −.11† | ||||
| 6. Communication (F) | 1.00 | .00 | .26** | .05 | .33** | .11† | .42** | .15* | .41** | −.27** | −.38** | .20** | .25** | −.18** | |||||
| 7. Intrusive support (M) | 1.00 | .50** | .43** | .23** | .19** | .12† | .38** | .22** | .04 | .17** | −.06 | .10 | .03 | ||||||
| 8. Intrusive support (F) | 1.00 | .12† | .56** | .04 | .31** | .09† | .58** | −.04 | −.04 | −.01 | .14* | −.10 | |||||||
| 9. Frequency of help (M) | 1.00 | .33** | .17** | .09 | .33** | .14* | .00 | .01 | −.11 | .04 | .07 | ||||||||
| 10. Frequency of help (F) | 1.00 | .08 | .45** | .12† | .61** | −.11† | −.14* | −.03 | .12† | −.20** | |||||||||
| 11. General monitoring (M) | 1.00 | .44** | .57** | .29** | −.22** | −.11† | .19** | .46** | −.08 | ||||||||||
| 12. General monitoring (F) | 1.00 | .20** | .67** | −.20** | −.22** | .05 | .26** | −.26** | |||||||||||
| 13. Diabetes monitoring (M) | 1.00 | .33** | −.07 | −.02 | .17** | .38** | −.10 | ||||||||||||
| 14. Diabetes monitoring (F) | 1.00 | −.12† | −.17** | .19** | .38** | −.27** | |||||||||||||
| 15. Externalizing behavior | 1.00 | .54** | −.31** | −.24** | .28** | ||||||||||||||
| 16. Internalizing behavior | 1.00 | −.24** | −.11† | .19** | |||||||||||||||
| 17. Self–efficacy | 1.00 | .40** | −.20** | ||||||||||||||||
| 18. Adherence | 1.00 | −.31** | |||||||||||||||||
| 19. HbA1c | 1.00 | ||||||||||||||||||
| Mean | 4.39 | 4.24 | 4.05 | 3.99 | 4.00 | 3.82 | 2.50 | 1.87 | 4.57 | 3.47 | 4.26 | 3.52 | 4.10 | 3.04 | 7.91 | 12.14 | 6.72 | 3.94 | 8.38 |
| Standard deviation | .65 | .81 | .62 | .77 | .66 | .75 | .80 | .81 | .89 | 1.50 | .62 | .96 | .79 | 1.06 | 6.97 | 9.34 | 1.66 | .57 | 1.58 |
(M) = adolescents’ reports on mothers; (F) = adolescents’ reports on fathers.
†p < .10; *p < .05; **p < .01.
Parental Involvement
Relationship Quality
Three scales measured the latent construct of relationship quality. This included two subscales from the Mother–Father–Peer Scale (MFP) from Epstein (1983) measuring acceptance and independence encouragement. The acceptance scale consisted of five items assessing the adolescent’s perception of the degree to which the parent communicated love, acceptance, and appreciation of the child ranging from 1 = strongly disagree to 5 = strongly agree. An average score was obtained. The current sample demonstrated good internal consistency (α for adolescents’ reports on mothers = .73, α for adolescents’ reports on fathers = .83). The independence encouragement scale consisted of seven items assessing the degree to which adolescents believed their parents promoted and encouraged their independence ranging from 1 = strongly disagree to 5 = strongly agree. An average score was obtained. The current sample demonstrated good internal consistency (α for adolescents’ reports on mothers = .79, α for reports on fathers = .87). Finally, the communication subscale of the Inventory of Parent and Peer Attachment from Armsden and Greenberg (1987) consisted of five items assessing communication with parents ranging from 1 = almost never or never true to 5 = almost always or always true. Reverse scoring was used for three items prior to an average score being computed; reliability was adequate (α for adolescents’ reports on mothers = .64, α for fathers = .69).
Monitoring
Two subscales measured the latent construct of monitoring. Five items assessed adolescents’ perceptions of their parents’ general knowledge of their daily activities (Barber, 1996), ranging from 1 = doesn’t know and 5 = knows everything. An average score was computed. The current sample demonstrated excellent reliability (α for adolescents’ reports on mothers = .80, α for reports on fathers = .85). Five additional items captured adolescents’ perceptions of their parents’ knowledge of diabetes care behaviors (Berg et al., 2008), with responses ranging from 1 = doesn’t know to 5 = knows everything. An average score was computed (α for adolescents’ reports on mothers = .90, α for reports on fathers = .91).
Behavioral Involvement
Two scales measured this latent construct. The Intrusive Support Scale from Pomerantz and Eaton (2001) consisted of four items capturing how often adolescents received unasked-for-assistance from parents with responses ranging from 1 = never to 4 = all of the time. An average score was computed (α for adolescents’ reports on mothers = .83, α for fathers = .87). Two items were developed by the authors (one assessing perceptions of mothers, the other fathers) to assess how frequently mothers and fathers provided assistance with diabetes tasks: “In an average week, how often does your mother/father help you with your diabetes?” The response choices were 0 days (never) = 1 to daily = 5.
Diabetes Self-Efficacy
Adolescents completed the Self-Efficacy for Diabetes Self-Management scale (SEDM, Iannotti et al., 2006), reporting their confidence in managing 10 difficult diabetes situations (ranging from 1 = not at all sure to 10 = completely sure, α = .83).
Internalizing and Externalizing Behavior
Young adolescents’ internalizing and externalizing behaviors were assessed using the Youth Self-Report (YSR, Achenbach, 1991). Adolescents responded to 31 items assessing internalizing behaviors (involving scales of withdrawn, anxiety and depression, and somatic complaints; α = .91) and 32 items assessing externalizing behaviors (e.g., comprised of the sum of two subscales, rule-breaking and aggressive behavior α = .88) on a scale from 0 = not true to 2 = very true. We used raw scores rather than T-scores, as recommended by Drotar, Stein and Perrin (1995) when individuals are in the normal rather than the clinical range.
Metabolic Control
Adolescents’ glycosylated hemoglobin (HbA1c) levels were obtained (lower scores reflect better control) using the Bayer DCA2000 by clinic staff. HbA1c values were collected on average 12.42 days before the laboratory visit (SD = 8.25, range 0–44 days). HbA1c and other illness information were gathered through medical records.
Adherence
Adolescents completed a 16-item Self Care Inventory (adapted from La Greca et al., 1995) to assess adherence to the diabetes regimen over the preceding month (1 = never to 5 = always did this as recommended without fail). Items were updated and two items were added with the assistance of a certified diabetes educator to reflect the current focus on carbohydrate counting and adjusting insulin. Average scores across items were computed. Scores on this scale have good internal consistency (α = .85 in our sample) and correlate well with more time-intensive interview methods for measuring adherence (La Greca et al., 1995).
Statistical Analyses
Data were analyzed using SEM performed in EQS, version 6.1 (Bentler, 2005). The goal of the analyses was to develop a model linking parental involvement to diabetes outcomes through a set of psychosocial mediators. Based on our previous work from the current sample (Palmer et al., in press), parental involvement was modeled as three separate, but related latent factors: (1) relationship quality (comprised of acceptance, independence encouragement, and communication), (2) monitoring (comprised of general and diabetes-specific monitoring), and (3) behavioral involvement (comprised of frequency of help and intrusive support). Adolescents’ reports of mothers’ and fathers’ involvement were analyzed separately, as we were interested in the overall effects for each as opposed to a couple-effect that would be produced if run together. For both maternal and paternal involvement, we began by testing a full mediation model, in which the latent factors of parental involvement had indirect effects on adherence and metabolic control through three mediators: externalizing behavior, internalizing behavior, and self-efficacy. We then tested a partial mediation model, allowing the latent factors of parental involvement to have direct effects on adherence and metabolic control, in addition to the indirect effects through the three mediating variables. To determine the significance of indirect effects, we used bootstrapped standard errors. The fit of each model was evaluated using commonly accepted goodness of fit indices that are believed to function acceptably for this sample size (Hu & Bentler, 1998; Marsh, Balla, & MacDonald, 1988). We compared the full versus partial mediation models using the Satorra-Bentler scaled χ2 difference test, and selected the better fitting model as our final model.
Prior to the SEM analyses, data were screened for missing values and departures from normality. A mean (item) replacement strategy was used when individuals were missing less than 20% of the items for a particular scale (M % per participant = 0.2, number of values replaced across all scales = 16). We detected significant multivariate non-normality in the data for the maternal and paternal SEM analyses (Mardia’s normalized estimates > 5.00, see Bentler, 2005). Therefore, for each SEM model, we report robust results that have been corrected for non-normality (Bentler & Dijkstra, 1985; Byrne, 2006; Satorra & Bentler, 1988).
Results
Maternal Involvement Analyses
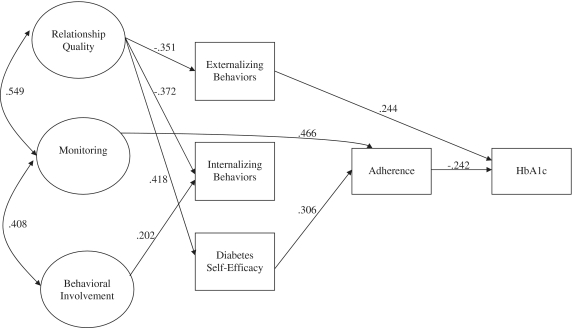
We began by testing a full mediation model, allowing the three maternal involvement latent factors (relationship quality, monitoring, and behavioral involvement) to influence adherence and metabolic control indirectly, through three mediators: externalizing behavior, internalizing behavior, and diabetes self-efficacy. Results indicated that this model was not a good fit to the data (χ2S–B [37, n = 236] = 91.76, p < .01; CFI = .892; RMSEA = .079). Next, we estimated a partial mediation model, allowing maternal involvement to have both direct and indirect effects on diabetes outcomes. In contrast to the full mediation model, the partial mediation model allowed for the possibility that the three mediators would not fully account for the associations between maternal involvement and diabetes outcomes. The partial mediation model was a good fit to the data (χ2S–B [31, n = 236] = 45.00, p = .05; CFI = .973; RMSEA = .044), and a significantly better fit than the full mediation model (Satorra-Bentler scaled χ2 difference [6] = 52.65, p < .001). We selected the partial mediation model as the final model (see Figure 1, presented with standardized coefficients and non-significant parameters removed).
Figure 1.
Results of a structural model depicting associations between latent constructs of maternal involvement and adolescent diabetes outcomes: Satorra-Bentler χ2 (47) = 64.752, p = .044; CFI = .965; RMSEA = .040 (robust fit indices). Significant correlations and standardized path coefficients (p < .05) are presented in the figure. Although not presented in the figure, two additional correlations were included in the model: r (externalizing, internalizing) = .459, and r (externalizing, self-efficacy) = –.173.
In the final maternal involvement model (χ2S–B [47] = 64.752, p = .04; CFI = .965; RMSEA = .040), relationship quality was directly associated with each of the hypothesized mediators (lower externalizing and internalizing behaviors, higher self-efficacy), and indirectly associated with better adherence (through self-efficacy, p < .05) and lower (i.e. better) HbA1c (through externalizing symptoms and self-efficacy and adherence, p's < .05). Behavioral involvement was associated with more internalizing behavior, but was not associated with diabetes outcomes. Maternal monitoring was not associated with any of the mediators, but was directly associated with better adherence and indirectly associated with lower HbA1c via adherence (p < .05). Among the hypothesized mediators, diabetes self-efficacy was directly associated with better adherence and indirectly associated (through adherence) with lower HbA1c (p < .05); externalizing behavior was directly associated with higher HbA1c, but was not associated with adherence; and internalizing behavior was not associated with either adherence or HbA1c when examined simultaneously with other potential mediators. These results suggest that the association of maternal relationship quality with adherence was mediated by self-efficacy, and that the association of relationship quality with HbA1c was mediated by self-efficacy and externalizing behavior. In contrast, the association of maternal monitoring with diabetes outcomes did not appear to occur through any of the hypothesized mediators. The final maternal involvement model explained 12.3% of the variance in externalizing behavior, 17.9% of the variance in internalizing behavior, 17.5% of the variance in diabetes self-efficacy, 37.6% of the variance in adherence, and 13.9% of the variance in metabolic control (HbA1c).
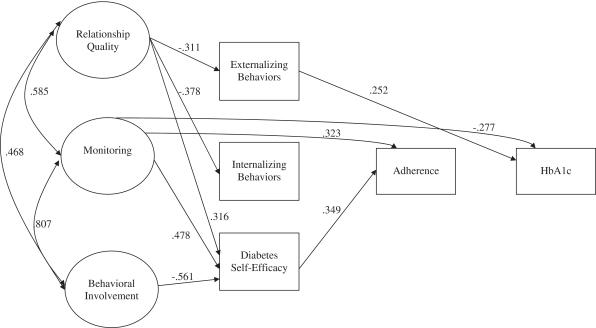
Paternal Involvement Analyses
A second, parallel set of analyses were conducted to examine the associations between adolescents’ reports of fathers’ involvement and diabetes outcomes. Similar to the results for mothers, a full mediation model was not a good fit to the data (χ2S–B [37, n = 230] = 130.92, p < 0.01; CFI = .869; RMSEA = .105). A partial mediation model, however, was an adequate fit to the data: χ2S–B (31, n = 230) = 92.31, p < .01; CFI = .915; RMSEA = .093. The partial mediation model was a better fit than the full mediation model (Satorra-Bentler scaled chi-square difference [6] = 37.21, p < .001), and was thus selected as the final model (χ2S–B (45) = 111.53, p < .01; CFI = .908; RMSEA = .080, see Figure 2, presented with standardized coefficients and non-significant parameters removed).
Figure 2.
Results of a structural model depicting associations between latent constructs of paternal involvement and adolescent diabetes outcomes: Satorra-Bentler χ2 (45) = 111.53, p < .01; CFI = .908; RMSEA = .080 (robust fit indices). Significant correlations and standardized path coefficients (p < .05) are presented in the figure. Although not presented in the figure, two additional correlations were included in the model: r (externalizing, internalizing) = .441, and r (externalizing, self-efficacy) = –.208.
Consistent with the model for mothers’ involvement (Figure 2), high paternal relationship quality was directly associated with each of the hypothesized mediators (lower externalizing and internalizing behaviors, higher self-efficacy) and indirectly associated with better adherence through higher self-efficacy (p < .05) and lower (i.e. better) HbA1c through lower externalizing behaviors (p < .05). In contrast to mothers, paternal monitoring was associated with higher diabetes self-efficacy and directly associated with lower HbA1c (p < .05). Paternal behavioral involvement was associated with lower diabetes self-efficacy and indirectly associated with lower adherence through self-efficacy beliefs (p < .05). The final paternal involvement model accounted for 9.7% of the variance in externalizing behavior, 14.3% of the variance in internalizing behavior, 22.1% of the variance in diabetes self-efficacy, 27.4% of the variance in adherence, and 16.6% of the variance in metabolic control (HbA1c).
Discussion
Parental involvement in the form of a high quality parent–adolescent relationship was indirectly associated with better adherence and metabolic control through lower externalizing behaviors and higher self-efficacy. Parental monitoring had more direct associations with adherence (for both maternal and paternal monitoring) and metabolic control (only for paternal monitoring). These results add to the literature on parental involvement and diabetes by demonstrating the unique contribution of components of parental involvement and the processes whereby these components are associated with better adherence and metabolic control.
Consistent with the broader developmental literature (Beveridge & Berg, 2007), a high quality parent–adolescent relationship was associated with risk and protective factors, with lower externalizing behaviors related directly to better metabolic control and high self-efficacy associated with better adherence and, indirectly, with HbA1c (through adherence). A high quality parent–adolescent relationship (warmth and acceptance, high communication, and encouraging independence) is important for diabetes management during adolescence and may serve as a basis for other facets of parental involvement such as monitoring to develop (Kerns, Aspelmeier, Gentzler, & Grabill, 2001). Although a high quality relationship with both mothers and fathers was associated with lower internalizing behaviors, internalizing behaviors were not associated with adherence or with metabolic control when externalizing and self-efficacy were controlled. These results suggest that when controlling for the shared variance between internalizing and externalizing behaviors, externalizing behaviors may be most predictive of poor metabolic control.
Self-efficacy for diabetes management appeared to be an important mediator of the association between relationship quality and diabetes management. Although a high quality relationship was associated with both lower externalizing behaviors and higher self-efficacy, only self-efficacy was associated with better metabolic control through adherence. The pathway from higher diabetes self-efficacy to greater adherence and lower HbA1c is consistent with daily diary work linking daily self-efficacy to adherence and blood glucose control (Fortenberry, Butler, Butner, Berg, Upchurch, & Wiebe, 2009). Furthermore, this pathway is consistent with the social-cognitive theory underlying self-efficacy (e.g., Iannotti et al., 2006), where confidence in one’s ability to complete diabetes-management tasks in the face of difficulties should be evident in behavioral aspects of diabetes management. These results point to self-efficacy as an important benefit associated with a high quality parent–adolescent relationship, a factor that may be especially crucial for young adolescents who are beginning to manage their diabetes more independently from their parents. The importance of self-efficacy in mediating the role of positive parental involvement on other health risk behaviors such as drug use (Watkins et al., 2006) suggests that self-efficacy may be important not only across adolescence but beyond in emerging adulthood.
Greater parental monitoring was important in understanding better adherence (for both mothers’ and fathers’ models) and metabolic control (indirectly through adherence for mothers’ model, directly for fathers’ model), consistent with work that identifies monitoring as a key component to parental involvement in diabetes care (Berg et al., 2008; Ellis et al., 2007). Previous work suggested that monitoring had beneficial effects on metabolic control by reducing externalizing behaviors, but this indirect effect was not found in this study (Horton et al., 2009). We interpret these different results as largely reflecting the substantial link between relationship quality and monitoring. Thus, the unique contribution of monitoring to diabetes management appears quite different when other related aspects of parental involvement are controlled.
From the models tested here, it appears that we do not yet fully understand how monitoring may be beneficial for diabetes management, as no indirect path existed between monitoring and adherence via externalizing or internalizing behaviors or self-efficacy. The more direct paths from monitoring to adherence and metabolic control may involve parents setting limits when adherence is poor, and for fathers this may particularly occur when metabolic control is poor.
The models for young adolescents’ perceptions of mothers’ and fathers’ involvement were quite similar, with the primary differences being the direct effects of fathers’ monitoring on HbA1c and the lack of association between adherence and HbA1c in fathers’ model. These results add to the growing literature on the importance of fathers’ involvement (Berg et al., 2008; Gavin & Wysocki, 2006) and indicate that the process whereby their involvement has beneficial effects is quite similar to that for mothers’ involvement. The quality of young adolescents’ relationships with mothers and with fathers had associations with adherence and HbA1c through lowering externalizing behaviors and bolstering self-efficacy. One of the differences between the models for mothers and fathers was the lack of a significant relationship between adherence and HbA1c in the father model. We view this result as arising largely from the inclusion of other pathways in the model, most likely reflecting the direct effect of monitoring on HbA1c in the father model. The zero-order correlation between adherence and HbA1c in our sample is similar to other findings in the literature (Weinger, Welch, Butler, & LaGreca, 2005).
Contrary to expectations, fathers’ behavioral involvement (assistance with diabetes care behaviors) was associated with poorer self-efficacy and adherence and mothers’ behavioral involvement was associated with more internalizing behaviors. Because this study was cross-sectional, these results may reflect that low self-efficacy may lead to greater fathers’ behavioral involvement and internalizing behaviors may elicit mothers’ greater behavior involvement. The negative associations between behavioral involvement and self-efficacy, adherence, and internalizing behaviors may also have resulted from the positive associations between behavioral involvement and both relationship quality and monitoring, such that the benefits typically associated with behavioral involvement (Anderson et al., 1997) were captured by related aspects of parental involvement. Once relationship quality and monitoring were controlled, what was left in the measurement of behavioral involvement may have been ways that parents were involved in an intrusive manner—involved without the adolescent requesting assistance and thereby conflicting with the autonomy needs of the adolescent (Pomerantz & Eaton, 2001). However, this interpretation should be viewed with caution as our measure of behavioral involvement was different from other measures, such as the Diabetes Responsibility Scale (Palmer et al., 2009) or the Diabetes Family Responsibility Questionnaire (Anderson et al., 1990), which could account for the different results.
The results should be interpreted in the context of some limitations. First, the cross-sectional nature of our data precludes us from making strong mediational conclusions; we cannot establish temporal precedence as our measures were all gathered at one point in time. However, our ongoing longitudinal analyses are consistent with the mediational role of self-efficacy (King, Berg, Butler, & Wiebe, 2010). Second, our results are limited to adolescents’ reports of mothers’ and fathers’ involvement. Parents did not report on all aspects of parental involvement, prohibiting us from including their reports in our modeling. Third, our results are restricted to the metrics of parental involvement and the mediators that were measured. Other metrics of parental involvement such as psychological control may have been mediated through internalizing behaviors (Butler, Skinner, Gelfand, Berg, & Wiebe, 2007). Furthermore, additional mediational processes that could be examined include how adolescents navigate their peer environment (Drew, Wiebe, & Berg, 2010) or solve diabetes problems when they occur (Wysocki et al., 2008), among others. Finally, our results are restricted in generalizability as our sample of families included predominantly intact white, English-speaking, middle-class participants.
The results add to a growing body of literature linking parental involvement and diabetes outcomes during adolescence by measuring multiple facets of parental involvement and examining the process whereby these facets of parental involvement may be beneficial. This more multi-faceted approach to parental involvement may assist in unraveling what are the critical aspects of parental involvement to guide interventions in families with type 1 diabetes (Drotar, 2006) and to select key mediating mechanisms of these interventions. The current study indicates that during young adolescence a high-quality parent–adolescent relationship is key, including the adolescent feeling accepted by parents. Improving this aspect of parent–child relationships is one component among many in interventions such as the Behavioral Family Systems Therapy (Wysocki et al., 2006) and Family Focused Teamwork Intervention (Laffel et al., 2003), which have resulted in improvements in diabetes outcomes. Interventions targeting this aspect of parental involvement are best accomplished early in development when attachment relationships are formed (Berlin, Zeanah, & Lieberman, 2008). Our work also indicated that interventions should include fathers as their monitoring has additional effects on HbA1c. The inclusion of multiple facets of parental involvement will allow the field to understand better the interrelated nature of parental involvement and their unique contributions in understanding diabetes management outcomes.
Funding
Research was supported by grant R01 DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Conflicts of interest: None declared.
References
- Achenbach T M. Burlington. VT: University of Vermont; 1991. Manual for the Child Behavior Checklist. [Google Scholar]
- Anderson B J, Auslander W F, Jung K C, Miller J P, Santiago J V. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15:477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Anderson B J, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: Relationships to blood-glucose monitoring, adherence, and metabolic control in young adolescents with IDDM. Journal of Pediatrics. 1997;130(2):257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- Armsden G C, Greenberg M T. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence. 1987;16(5):427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- Barber B K. Parental psychological control: Revisiting a neglected construct. Child Development. 1996;67:3296–3319. [PubMed] [Google Scholar]
- Bentler P M. EQS structural equations program, Version 6.1. Encino, CA: Multivariate Software; 2005. [Google Scholar]
- Bentler P M, Dijkstra T. Efficient estimation via linearization in structural models. In: Krishnaiah P R, editor. Multivariate Analysis IV. Amsterdam: North-Holland; 1985. pp. 9–42. [Google Scholar]
- Berg C A, Butler J M, Osborn P, King G, Palmer D L, Butner J, Murray M, Lindsay R, Donaldson D, Foster C, Swinyard M, Wiebe D J. Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31(4):678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- Berlin L J, Zeanah C H, Lieberman A F. Prevention and intervention programs for supporting early attachment security. In: Cassidy J, Shaver P R, editors. Handbook of attachment: Theory, research, and clinical applications. 2nd. New York: The Guilford Press; 2008. pp. 745–761. [Google Scholar]
- Beveridge R M, Berg C A. Parent-adolescent collaboration: An interpersonal model for understanding optimal interactions. Clinical Child and Family Psychological Review. 2007;10(1):25–52. doi: 10.1007/s10567-006-0015-z. [DOI] [PubMed] [Google Scholar]
- Beveridge R M, Berg C A, Wiebe D J, Palmer D A. Mother and adolescent representations of illness ownership and stressful events surrounding diabetes. Journal of Pediatric Psychology. 2006;31:818–827. doi: 10.1093/jpepsy/jsj094. [DOI] [PubMed] [Google Scholar]
- Bong M. Effects of parent-child relationships and classroom goal structures on motivation, help-seeking avoidance, and cheating. Journal of Experimental Education. 2008;76(2):191–217. [Google Scholar]
- Butler J M, Skinner M, Gelfand D, Berg C A, Wiebe D J. Maternal parenting style and adjustment in adolescents with type I diabetes. Journal of Pediatric Psychology. 2007;32(10):1227–1237. doi: 10.1093/jpepsy/jsm065. [DOI] [PubMed] [Google Scholar]
- Byrne B M. Structural equation modeling with EQS: Basic concepts, applications, and programming. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2006. [Google Scholar]
- Dishion T J, McMahon R J. Parental monitoring and the prevention of child and adolescent problem behavior: a conceptual and empirical formulation. Clinical Child and Family Psychology Review. 1998;1(1):61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Drew L, Wiebe D J, Berg C A. The mediating role of extreme peer orientation on the relationships between adolescent-parent relationship and diabetes management. Journal of Family Psychology. 2010;24:299–306. doi: 10.1037/a0019352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drotar D. Psychological interventions in childhood chronic illness. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Drotar D, Stein R E K, Perrin E C. Methodological issues in using the Child Behavior Checklist and its related instruments in clinical child psychology research. Journal of Clinical Child Psychology. 1995;24:184–192. [Google Scholar]
- Ellis D A, Podolski C L, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology. 2007;32(8):907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- Epstein S. Scoring and interpretation of the Mother-Father-Peer scale. 1983 Unpublished manuscript. [Google Scholar]
- Fortenberry K T, Butler J M, Butner J, Berg C A, Upchurch R, Wiebe D J. Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine. 2009;37:1–9. doi: 10.1007/s12160-009-9086-7. [DOI] [PubMed] [Google Scholar]
- Gavin L, Wysocki T. Associations of paternal involvement in disease management with maternal and family outcomes in families with children with chronic illness. Journal of Pediatric Psychology. 2006;31(5):481–489. doi: 10.1093/jpepsy/jsj043. [DOI] [PubMed] [Google Scholar]
- Horton D, Berg C, Wiebe D. The role of parental monitoring in understanding the effect of externalizing behaviors on diabetes management during adolescence. Journal of Pediatric Psychology. 2009;34:1008–1018. doi: 10.1093/jpepsy/jsp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler P. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- Iannotti R J, Schneider S, Nansel T R, Haynie D L, Plotnick L P, Clark L M, Sobel D O, Imons-Morton B. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics. 2006;27(2):98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- Kerns K A, Aspelmeier J E, Gentzler A L, Grabill C M. Parent-child attachment and monitoring in middle childhood. Journal of Family Psychology. 2001;15(1):69–81. doi: 10.1037//0893-3200.15.1.69. [DOI] [PubMed] [Google Scholar]
- King P S, Berg C, Butler J, Wiebe D J. Longitudinal trends in maternal and paternal involvement and adolescents' adherence to the type 1 diabetes regimen. In: King P, editor. Longitudinal trajectories of chronic illness outcomes across adolescence. Seattle, WA: Symposium presented at Society for Behavioral Medicine; 2010. [Google Scholar]
- Korbel C, Wiebe D J, Berg C A, Palmer D L. Gender differences in adherence to type 1 diabetes management across adolescence: The mediating role of depression. Children’s Health Care. 2007;36(1):83–98. [Google Scholar]
- La Greca A M, Auslander W F, Greco P, Spetter D, Fisher E B, Jr, Santiago J V. I get by with a little help from my family and friends: Adolescents’ support for diabetes care. Journal of Pediatric Psychology. 1995;20(4):449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- Larson R W, Richards M H. Daily companionship in late childhood and early adolescence: Changing developmental contexts. Child Development. 1991;62:284–300. doi: 10.1111/j.1467-8624.1991.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Marsh H, Balla J, McDonald R. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychological Bulletin. 1988;103(3):391–410. [Google Scholar]
- Miller-Johnson S, Emery R E, Marvin R S, Clarke W, Lovinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. Journal of Consulting and Clinical Psychology. 1994;62(3):603–610. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- Paley B, Conger R, Gordon T. Parents’ affect, adolescent cognitive representations, and adolescent social development. Journal of Marriage and the Family. 2000;62:761–776. [Google Scholar]
- Palmer D L, Berg C A, Butler J, Fortenberry K, Murray M, Lindsay R, Donaldson D, Swinyard M, Foster C, Wiebe D J. Mothers', fathers', and children's perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology. 2009;34:195–204. doi: 10.1093/jpepsy/jsn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer D L, Osborn P, King P, Berg C A, Butler J, Butner J, Horton D, Wiebe D J. The structure of parental involvement and relations to disease management for youth with type 1 diabetes. Journal of Pediatric Psychology. doi: 10.1093/jpepsy/jsq019. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz E M, Eaton M M. Maternal intrusive support in the academic context: Transactional socialization processes. Developmental Psychology. 2001;37(2):174–186. doi: 10.1037/0012-1649.37.2.174. [DOI] [PubMed] [Google Scholar]
- Quittner A L, DeGirolamo A M. Family adaptation to childhood disability and illness. In: Ammerman R T, Campo J V, editors. Handbook of Pediatric Psychology and Psychiatry. Boston: Allyn & Bacon; 1998. pp. 70–102. [Google Scholar]
- Satorra A, Bentler P M. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg C C, editors. Latent variable analysis: Applications for developmental research. Thousand Oaks, CA: Sage; 1994. pp. 399–419. [Google Scholar]
- Schulman S, Seiffge-Krenke I. Fathers and adolescents: Developmental and clinical perspectives. New York: Routledge; 1997. [Google Scholar]
- Skinner T C, John M, Hampson S E. Social support and personal models of diabetes as predictors of self-care and well-being: A longitudinal study of adolescents with diabetes. Journal of Pediatric Psychology. 2000;25(4):257–267. doi: 10.1093/jpepsy/25.4.257. [DOI] [PubMed] [Google Scholar]
- Watkins J A, Howard-Barr E M, Moore M J, Werch C C. The mediating role of adolescent self-efficacy in the relationship between parental practices and adolescent alcohol use. Journal of Adolescent Health. 2006;38:448–450. doi: 10.1016/j.jadohealth.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Weinger K, Welch G W, Butler H A, LaGreca A M. Measuring diabetes self-care. Diabetes Care. 2005;28:1346–1352. doi: 10.2337/diacare.28.6.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Iannotti R, Weissberg-Benchell J, Laffel L, Hood K, Anderson B, Chen R. Diabetes problem solving by youths with type 1 diabetes and their caregivers: Measurement, validation, and longitudinal associations with glycemic control. Journal of Pediatric Psychology. 2008;33(8):875–884. doi: 10.1093/jpepsy/jsn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Linschied T R, Taylor A, Yeates K O, Hough B S, Naglieri J A. Deviation from developmentally appropriate self-care autonomy. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Nansel T R, Holmbeck G N, Chen R, Laffel L, Anderson B J, Weissberg-Benchell J. Collaborative involvement of primary and secondary caregivers: Associations with youths’ diabetes outcomes. Journal of Pediatric Psychology. 2009;34:869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]