Abstract
The authors present the case of a 68-year-old lady with a 35-year history of bipolar affective disorder (BPAD) type I, who developed frontotemporal dementia (FTD). Description of the psychopathology is illustrated with examples of patient's writings in order to demonstrate cognitive abilities at different stages. The diagnosis is supported by MRI and SPECT scans. The authors discuss the difficulties in differentiating the clinical presentation of chronic BPAD and FTD and examine the evidence for two important questions: Is there a relationship between BPAD and FTD and is there a relationship between lithium and risk of dementia? This is, to the best of our knowledge, the first reported SPECT scan finding in a case of frontotemporal dementia following chronic bipolar affective disorder.
Background
This case highlights the difficulties in differentiating the clinical presentation of chronic bipolar affective disorder (BPAD) and frontotemporal dementia (FTD). We discuss the relationship between BPAD and FTD and the management dilemmas in this patient with two important questions:. Is there an association between BPAD and FTD and is there a neuroprotective effect of long-term lithium therapy?
Existing research has been inconclusive, showing that BPAD is associated with cognitive deficits independent of mood state. Executive functions in elderly subjects with BPAD are impaired when compared with controls1 and mood disorder is a risk factor for developing global cognitive dysfunction in later life.2 Frontal lobe white matter abnormalities3 4 have been reported on functional imaging in BPAD. The term ‘postbipolar dementia’ has been recently used to describe cognitive impairment, which does not satisfy diagnostic criteria for frontotemporal5 or any other major dementia subgroup.6
However, there are some inconsistencies, with studies identifying major psychiatric illness as a risk factor for dementia.6 The research into the effect of lithium has yielded contrary and inconclusive data.7
Case presentation
We present the case of Mrs A, a 68-year-old lady with a 35-year history of BPAD type I, who presented in September 2007 with a relapse of a manic episode involving pressured speech, elated mood and disinhibited behaviour. This occurred following discontinuation of long-term lithium therapy due to worsening of her renal function. Prior to this, she had been stable in her mental state since 1984, when lithium was introduced for the first time. Lithium was the first and, until 2007, the only mood stabiliser used in managing her mood disorder. An initial dose of 600 mg was subsequently titrated to 800 mg daily and maintained at that level. Her only relapse was a short period of depression and subsequent hypomania in 2001, when her mother passed away.
In line with NICE guidelines for management of bipolar disorder,8 initial treatment included semisodium valproate, as a second-line mood stabiliser, at a dose of 750 mg, and quetiapine titrated up to a dose of 300 mg. Manic symptoms improved, but she later developed low mood, anhedonia and lethargy. The patient became aggressive and irritable. Soon after, cognitive impairment became evident and Mini Mental State Examination (MMSE) scores fluctuated, ranging from 17 to 24. Mrs A lost points on MMSE mainly on tasks for orientation, attention and concentration. A CT brain, performed at that time, revealed mild widening of frontal sulci and enlarged frontal horns of lateral ventricles. The MRI scan was technically limited due to uncooperative behaviour, but confirmed similar findings (figure 1).
Figure 1.
MRI scan showing mild widening of frontal sulci and enlarged frontal horns of lateral ventricles.
She did not cooperate with formal neuropsychological testing, but bedside tests revealed a decline in attention, concentration, verbal fluency and language. The following 18 months demonstrated a fluctuating course with depressive features, cognitive difficulties and disturbed behaviour. The patient started showing the following symptoms of FTD (Neary's Consensus Criteria)5:
-
▶
decline in social, interpersonal and personal conduct
-
▶
hyperorality with environmental exploration using lips and tongue
-
▶
predilection for sweets
-
▶
perseverative and stereotyped behaviour
-
▶
utilization behaviour illustrated by drinking from any cup left around
-
▶
aspontaneity
-
▶
intermittent mutism.
Progressive cognitive decline over the next year was exemplified by worsening inability to write a sentence (figures 2 and 3). Associated symptoms and signs were ataxic gait, intermittent urinary incontinence, aggressive behaviour and polydipsia. Investigations excluded normal pressure hydrocephalus, syndrome of inappropriate antidiuretic hormone secretion and other metabolic abnormalities.
Figure 2.
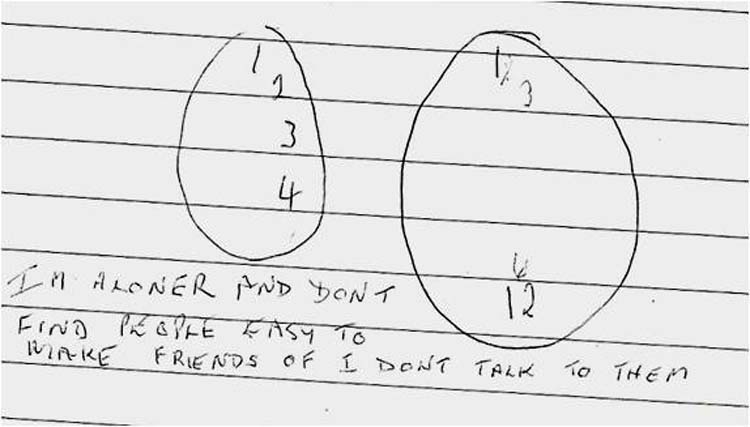
Clock drawing test and sentence writing task in October 2008.
Figure 3.
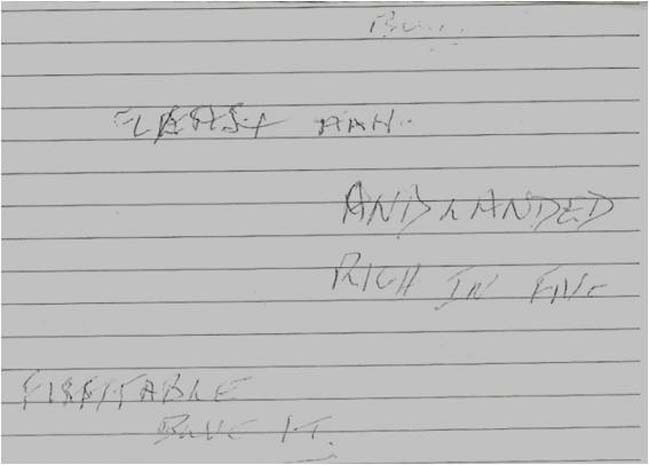
Sentence writing task in April 2009.
Depressive illness with mood congruent delusions (somatic and nihilistic) was treated by adding sertraline 150 mg. This SSRI was chosen, in line with NICE guidelines for the management of bipolar disorder,8 because of its safety over tricyclic (TCAs) and monoamine oxidase inhibitor antidepressants. Moreover, there is a suggested lower risk of switching, in comparison with TCAs.9 Semisodium-valproate and quetiapine were discontinued after a year-long trial due to lack of efficacy. As there was no response to sertraline, it was augmented with mirtazepine 45 mg.10
Electroconvulsive therapy (ECT) was tried in accordance with NICE guidance ‘to achieve rapid and short-term improvement of severe symptoms after an adequate trial of other treatment options has proven ineffective’.8 Unfortunately, neither antidepressants nor ECT significantly relieved her depressive symptomatology. After a review by nephrologists, on the balance of risks and benefits, lithium was carefully reintroduced at a dose of 200 mg and then increased to 400 mg to obtain a therapeutic serum level. Risperidone and olanzapine were also tried in adequate doses to control nihilistic and somatic delusions, which the patient found extremely distressing. However, she was not able to tolerate this due to side effects of marked sedation. Consequently, aripiprazole 15 mg, as a less sedative antipsychotic, was introduced and better tolerated. As her agitation and physical aggression continued to deteriorate, carbamazepine 400 mg daily was added11 and led to stabilisation of behavioural disturbances. Combined therapy comprising daily doses of lithium carbonate 400 mg, carbamazepine 400 mg and aripiprazole 15 mg helped stabilise her mood, resolve delusional ideas and improve behavioural disturbances. However, her frontal lobe symptoms persisted.
Investigations
EEG and lumbar puncture with cerebrospinal fluid studies were unremarkable. A repeat CT scan a year into her admission showed no further progression of frontal lobe atrophy.
A SPECT scan obtained 18 months into her admission in June 2009 using Tc99m HMPAO (hexamethyl propylene amine oxime) revealed reduced blood flow in both frontal and temporal lobes, more marked on the left side (figure 4). These SPECT findings are highly suggestive of a diagnosis of FTD.
Figure 4.
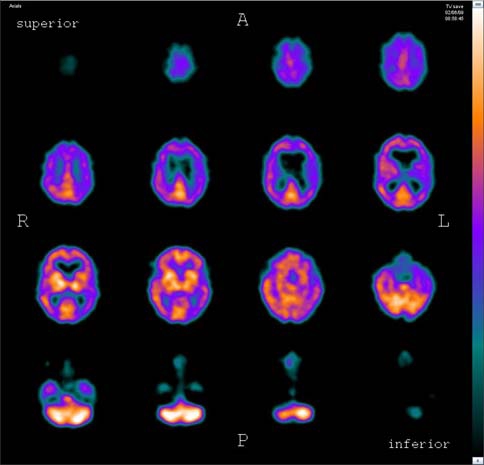
Tc99m HMPAO SPECT scan showing hypoperfusion in frontal and temporal lobes.
Differential diagnosis
Although our understanding of this patient revolves around a bipolar disorder-frontotemporal dementia axis, with pronounced frontal lobe deficits, it was important to have a wide perspective and address a number of possibilities on the list of differential diagnoses. We initially aimed to exclude any reversible causes of cognitive impairment such as vitamin B12 deficiency and hypothyroidism. It was also important to exclude other causes of chronic delirium. The finding of polydipsia necessitated investigations for diabetes mellitus, hypercalcaemia, syndrome of inappropriate antidiuretic hormone secretion and similar metabolic abnormalities. Thus fasting serum glucose, thyroid function tests, electrolytes and urine and serum osmolality were tested. Ataxic gait, intermittent urinary incontinence and confusion required investigations to exclude normal pressure hydrocephalus. However, a CT head scan and lumbar puncture helped us reject this hypothesis. Brain imaging also failed to reveal any evidence of space-occupying lesions such as frontal lobe tumours or subdural haematoma, which were also considered as differential diagnoses. The patient was also screened for malignancies in a view of possible paraneoplastic syndrome.
Other conditions of note for differential diagnosis were other dementias, most importantly, Alzheimer's and dementia with Lewy bodies.
Treatment
Treatment followed recommendations from NICE guidelines on management of bipolar disorder. The initial acute manic episode was treated with the combination of second-line agents, an anticonvulsant (semisodium-valproate) and antipsychotic (quetiapine) as outlined above.
Her depressive episode was treated with an SSRI (sertraline) and augmented with mirtazepine after failure to respond. When both treatments failed to achieve significant improvement, ECT was tried. The patient reached stable mood with reintroduction of lithium and further improvement in psychotic and behavioural symptoms with addition of carbamazepine and aripiprazole as detailed above.
Outcome and follow-up
The patient continued to deteriorate, and after 2 years of inpatient stay she was discharged to a specialist nursing home for elderly people with dementia. Follow-up a year later showed further deterioration with prominent aggression, hostility and poor speech fluency.
Discussion
Although the initial presentation was suggestive of relapse of long-standing BPAD, further development raised suspicions of on underlying progressive frontotemporal impairment. There is evidence to support a relationship between BPAD and cognitive decline. In a small prospective study comparing subjects with bipolar disorder and controls, subjects with bipolar disorder experienced a significantly more rapid rate of decline than controls.12 Executive functions in elderly subjects with BPAD are impaired when compared with controls.1 13 If there is a valid relationship between BPAD and FTD, then there may be a number of reasons including medication, lifestyle factors, physical health as well as a possible shared genetic or developmental origin. In one case study, for instance, lithium toxicity due to drug-drug interactions was suggested as a cause of the cognitive decline.14 However, lithium has also been associated with a reduced risk of dementia.15 More convincing evidence of a relationship between FTD and BPAD has emerged from a recent case series in which subjects diagnosed with BPAD later developed FTD.16 With regard to anatomical correlates in FTD and BPAD, there is evidence demonstrating reduced grey matter volume in the dorsolateral and dorsomedial prefrontal cortex in subjects with the bipolar disorder.17 These regions are also implicated as pathological substrates in FTD.18 Further advances in and reconciliation of genetic findings in both FTD and BPAD may yield important insights into both disorders.
Learning points.
-
▶
The development of FTD following BPAD can present a diagnostic challenge.
-
▶
SPECT studies can be useful in the diagnostic workup of complex dementia cases.
-
▶
This case adds to an emerging literature on a potential relationship between FTD and BPAD.
Acknowledgments
The authors would like to thank all their colleagues at the Michael Carlisle Centre.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Lebert F, Lys H, Haëm E, et al. [Dementia following bipolar disorder]. Encephale 2008;34:606–10 [DOI] [PubMed] [Google Scholar]
- 2.Gualtieri CT, Johnson LG. Age-related cognitive decline in patients with mood disorders. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:962–7 [DOI] [PubMed] [Google Scholar]
- 3.Bruno S, Cercignani M, Ron MA. White matter abnormalities in bipolar disorder: a voxel-based diffusion tensor imaging study. Bipolar Disord 2008;10:460–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sussmann JE, Lymer GK, McKirdy J, et al. White matter abnormalities in bipolar disorder and schizophrenia detected using diffusion tensor magnetic resonance imaging. Bipolar Disord 2009;11:11–18 [DOI] [PubMed] [Google Scholar]
- 5.Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 1998;51:1546–54 [DOI] [PubMed] [Google Scholar]
- 6.Cooper B, Holmes C. Previous psychiatric history as a risk factor for late-life dementia: a population-based case-control study. Age Ageing 1998;27:181–8 [DOI] [PubMed] [Google Scholar]
- 7.Deutsch SI, Rosse RB, Lakshman RM. Dysregulation of tau phosphorylation is a hypothesized point of convergence in the pathogenesis of Alzheimer's disease, frontotemporal dementia and schizophrenia with therapeutic implications. Prog Neuropsychopharmacol Biol Psychiatry 2006;30:1369–80 [DOI] [PubMed] [Google Scholar]
- 8.NICE Guidelines The Management of Bipolar Disorder in Adults, Children and Adolescents, in Primary and Secondary Care. National Clinical Practice Guideline Number 38. London, 2003 [Google Scholar]
- 9.Calabrese JR, Rapport DJ, Kimmel SE, et al. Controlled trials in bipolar I depression: focus on switch rates and efficacy. Eur Neuropsychopharmacol 1999;9(Suppl 4):S109–12 [DOI] [PubMed] [Google Scholar]
- 10.Carpenter LL, Yasmin S, Price LH. A double-blind, placebo-controlled study of antidepressant augmentation with mirtazapine. Biol Psychiatry 2002;51:183–8 [DOI] [PubMed] [Google Scholar]
- 11.Tariot PN, Erb R, Podgorski CA, et al. Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry 1998;155:54–61 [DOI] [PubMed] [Google Scholar]
- 12.Gildengers AG, Mulsant BH, Begley A, et al. The longitudinal course of cognition in older adults with bipolar disorder. Bipolar Disord 2009;11:744–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gunning-Dixon FM, Murphy CF, Alexopoulos GS, et al. Executive dysfunction in elderly bipolar manic patients. Am J Geriatr Psychiatry 2008;16:506–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhatnagar M, Palmer R. A 61-year-old with bipolar disorder and cognitive impairment: dementia or polypharmacy? Cleve Clin J Med 2008;75:284–8 [DOI] [PubMed] [Google Scholar]
- 15.Terao T, Nakano H, Inoue Y, et al. Lithium and dementia: a preliminary study. Prog Neuropsychopharmacol Biol Psychiatry 2006;30:1125–8 [DOI] [PubMed] [Google Scholar]
- 16.Velakoulis D, Walterfang M, Mocellin R, et al. Frontotemporal dementia presenting as schizophrenia-like psychosis in young people: clinicopathological series and review of cases. Br J Psychiatry 2009;194:298–305 [DOI] [PubMed] [Google Scholar]
- 17.Brooks JO, 3rd, Bonner JC, Rosen AC, et al. Dorsolateral and dorsomedial prefrontal gray matter density changes associated with bipolar depression. Psychiatry Res 2009;172:200–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schroeter ML, Raczka K, Neumann J, et al. Neural networks in frontotemporal dementia–a meta-analysis. Neurobiol Aging 2008;29:418–26 [DOI] [PubMed] [Google Scholar]


