SUMMARY
The number of acutely ill hospitalized medical patients at risk for acute venous thromboembolism (VTE) has not been well defined. Therefore, we used the 2003 United States Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample database to estimate VTE events among hospitalized medical patients. We then modeled the potential reduction in VTE with universal utilization of appropriate pharmacological thromboprophylaxis. We calculated that 8,077,919 acutely ill hospitalized medical patients were at risk for VTE. Heart failure, respiratory failure, pneumonia, and cancer were the most common medical diagnoses. We estimated that 196,134 VTE-related events occurred in 2003, afflicting two out of every 100 acutely ill hospitalized medical patients. These VTE-related events were comprised of 122,235 symptomatic deep vein thromboses, 32,654 symptomatic episodes of pulmonary embolism, and 41,245 deaths due to VTE. In our model, rates of pharmacological thromboprophylaxis prescription were low for various acute medical illnesses, ranging from 15.3% to 49.2%. However, with universal thromboprophylaxis, 114,174 VTE-related events would have been prevented. In conclusion, acutely ill medical patients represent a large population vulnerable to the development of VTE during hospitalization. The number of VTE-related events would be halved with universal thromboprophylaxis. Further efforts focused on improving VTE prevention strategies in hospitalized medical patients are warranted.
Keywords: Venous thromboembolism, Deep vein thrombosis, Pulmonary embolism, Medical patients, Prophylaxis
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is an often preventable complication of medical illness associated with substantial healthcare costs (1). DVT and PE may result in debilitating long-term complications of post-thrombotic syndrome (2) and chronic thromboembolic pulmonary hypertension (3), respectively. Common conditions among hospitalized medical patients, such as heart failure, chronic obstructive pulmonary disease, acute infection, atherosclerotic vascular disease, and malignancy, increase the risk of VTE (4). Recent hospitalization has been implicated in the development of VTE in the outpatient setting (5). Despite published and widely disseminated guidelines for the prevention of VTE among hospitalized medical patients (6, 7), underutilization of thromboprophylaxis continues to be a problem in the United States (8), Canada (9), and worldwide (10). Hospitalized medical patients are less likely to receive thromboprophylaxis than their surgical counterparts (4, 10). The objective of this study is to use the U.S. Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample database in combination with a probability model to estimate VTE events among hospitalized medical patients and the potential impact of universal thomboprophylaxis in this vulnerable population.
MATERIALS AND METHODS
Population
To identify acutely ill medical patients, we queried the 2003 HCUP Nationwide Inpatient Sample using previously described methods (11). We used the Clinical Classification Software (CCS) and Procedure Category Labels (PRCCS) to classify and collapse similar medical diagnosis codes into a smaller number of categories. We searched the Nationwide Inpatient Sample for acutely ill medical patients who were at increased risk of VTE using the following diagnoses: heart failure (codes 103, 108), respiratory failure (codes 127, 131), cancer (codes 11, 44), sepsis (code 2), acute myocardial infarction (code 100), non-surgical trauma (codes 225–231, 233–234), pneumonia (code 122), paralysis or coma (codes 82, 85), stroke (code 109) and arthropathy or spondylopathy (codes 202–205). We limited our search to the primary, secondary, and tertiary Clinical Classification Software Category for diagnosis positions (DXCCS1, DXCCS2, and DXCCS3). We included only patients older than 40 years of age and hospitalized for at least two days. To generate the projected national admission estimates of acutely ill medical patients for all U.S. acute care hospitals, we used the Nationwide Inpatient Sample core file of discharge weights.
Statistical Model
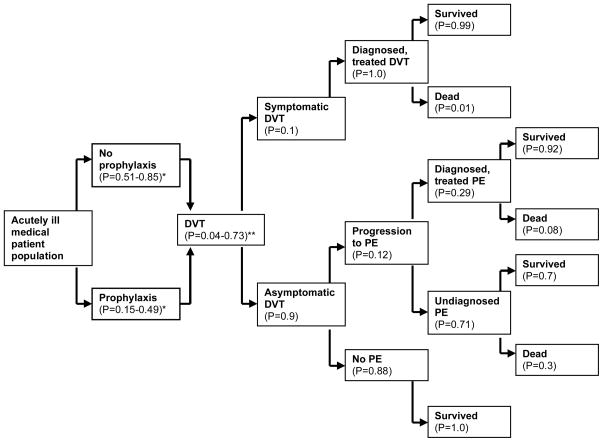
To estimate VTE events and VTE-related deaths for the year 2003, we entered each acutely ill medical patient population individually into an event probability model (Figure 1) used previously to estimate the annual number of VTE-related events among hospitalized patients in the European Union (12). Pharmacological thromboprophylaxis prescribing rates for each medical diagnosis were obtained from publications that evaluated the utilization of American College of Chest Physicians (ACCP) recommendations for thromboprophylaxis in at-risk hospitalized medical patients (8, 13). We defined pharmacological prophylaxis as any prescription of prophylactic anticoagulation. We extracted the probabilities of DVT and PE, with and without thromboprophylaxis, for each medical diagnosis from the published literature (Table 1) (14–21). To estimate symptomatic VTE events and mortality, we used the estimates of likelihood of diagnosis and treatment developed by Oster and colleagues (22). We followed the European consensus estimates that 10% of DVT events would be symptomatic and that 11.5% of these DVT events would result in PE (12). We did not incorporate recurrent VTE-related events in 2003 into the probability model. We assumed that symptomatic DVT would be treated and therefore would not result in PE. VTE-related mortality included estimates of sudden death, death following diagnosed and treated VTE, and death following undiagnosed and untreated disease. Death was defined as all-cause mortality.
Figure 1.
Venous thromboembolism (VTE) event probability model for acutely ill hospitalized medical patients. DVT, deep vein thrombosis; P, probability; PE, pulmonary embolism.
*Probability varies according to the specific medical diagnosis.
**Probability varies according to the specific medical diagnosis and use of thromboprophylaxis.
Table 1.
Probabilities of deep vein thrombosis (DVT) and pulmonary embolism (PE), with and without thromboprophylaxis, for each medical diagnosis. DVT, deep vein thrombosis; PE, pulmonary embolism.
| Medical diagnosis | Probability of DVT without prophylaxis | Probability of DVT with prophylaxis | Probability of PE without prophylaxis | Probability of PE with prophylaxis |
|---|---|---|---|---|
| Heart failure | 0.146 | 0.040 | 0.015 | 0.004 |
| Respiratory failure | 0.131 | 0.051 | 0.014 | 0.005 |
| Pneumonia | 0.165 | 0.046 | 0.017 | 0.005 |
| Cancer | 0.195 | 0.097 | 0.020 | 0.010 |
| Acute myocardial infarction | 0.240 | 0.075 | 0.025 | 0.008 |
| Arthropathy/spondylopathy | 0.207 | 0.100 | 0.021 | 0.010 |
| Stroke | 0.727 | 0.102 | 0.075 | 0.011 |
| Sepsis | 0.155 | 0.063 | 0.016 | 0.007 |
| Non-surgical trauma | 0.181 | 0.060 | 0.019 | 0.006 |
| Paralysis/coma | 0.160 | 0.040 | 0.017 | 0.004 |
Statistical Analysis
One-way sensitivity analyses were initially conducted with all inputs adjusted by ±50%. If any analysis indicated a greater than 1% impact on the overall output of the model (total mortality), the parameters were included in a probabilistic sensitivity analysis. A probabilistic sensitivity analysis, which helps assess the consequences of decision uncertainty by analyzing the effects of changing model parameters, was conducted by altering thromboprophylaxis uptake rates (23). Monte Carlo simulation (24) is a type of probabilistic sensitivity analysis in which the model runs many times using randomly sampled values for specific parameters to gauge the impact of uncertainty. Second order Monte Carlo simulation is performed for parameters that are expected to have a nonlinear effect on calculations. Confidence intervals were generated via second order Monte Carlo simulation performed in Microsoft Excel 2003 version 11.8 (Microsoft Corp., Redmond, WA).
RESULTS
Characteristics of Hospitalized Medical Patients
We calculated that 8,077,919 acutely ill hospitalized medical patients were at risk for VTE in 2003 (Table 2). Among these patients, heart failure, respiratory failure, pneumonia, and cancer were the most common medical diagnoses. We estimated that 2,939,539 acutely ill medical patients at increased risk for VTE would have suffered from cardiovascular and cerebrovascular disease, including heart failure, acute myocardial infarction, and stroke.
Table 2.
Estimates of acutely ill hospitalized medical patients at risk for venous thromboembolism (VTE) and thromboprophylaxis prescribing rates, by diagnosis.
| Diagnosis | Total patient population | Prophylaxis prescribing rate (%) |
|---|---|---|
| Heart failure | 1,848,861 | 40.1 |
| Respiratory failure | 1,490,543 | 31.0 |
| Pneumonia | 1,149,882 | 31.0 |
| Cancer | 1,055,435 | 27.6 |
| Acute myocardial infarction | 582,294 | 43.0 |
| Arthropathy/spondylopathy | 534,854 | 15.3 |
| Stroke | 508,384 | 49.2 |
| Sepsis | 420,000 | 15.3 |
| Non-surgical trauma | 418,696 | 20.3 |
| Paralysis/coma | 68,970 | 15.3 |
| TOTAL | 8,077,919 | - |
Estimates of Venous Thromboembolic Events
We estimated that 196,134 VTE-related events occurred in 2003, afflicting two out of every 100 acutely ill hospitalized medical patients (Table 3). These VTE-related events were comprised of 122,235 symptomatic DVTs (62%), 32,654 symptomatic PEs (17%), and 41,245 deaths due to VTE (21%). VTE-related events were most frequent among acutely ill medical patients with heart failure, stroke, cancer, respiratory failure, and pneumonia.
Table 3.
Estimates of venous thromboembolic events in acutely ill hospitalized medical patients with current thromboprophylaxis rates. CI, confidence interval; DVT, deep vein thrombosis; PE, pulmonary embolism.
| Diagnosis | Prophylaxis rate (%) | Symptomatic DVT events (95% CI) | Symptomatic PE events (95% CI) | VTE-related deaths (95% CI) | Total VTE Events |
|---|---|---|---|---|---|
| Heart failure | 40.1 | 19,135 (11,091–31,426) | 5,112 (2,137–12,628) | 6,457 (2,950–15,870) | 30,704 |
| Respiratory failure | 31.0 | 15,830 (9,170–27,659) | 4,229 (1,784–10,300) | 5,341 (2,048–12,814) | 25,400 |
| Pneumonia | 31.0 | 14,731 (6,565–22,775) | 3,935 (1,329–7,775) | 4,970 (1,548–9,751) | 23,636 |
| Cancer | 27.6 | 17,726 (6,273–22,070) | 4,735 (1,171–7,050) | 5,981 (1,423–8,828) | 28,442 |
| Stroke | 49.2 | 21,327 (10,674–30,108) | 5,697 (2,013–11,824) | 7,196 (2,474–14,699) | 34,220 |
| Acute myocardial infarction | 43.0 | 9,844 (4,719–17,369) | 2,630 (908–5,498) | 3,322 (1,152–7,241) | 15,796 |
| Non-surgical trauma | 20.3 | 6,550 (2,424–8,742) | 1,750 (502–2,807) | 2,210 (590–3,684) | 10,510 |
| Arthropathy/spondylopathy | 15.3 | 10,196 (3,118–11,041) | 2,724 (609–3,665) | 3,440 (781–4,640) | 16,360 |
| Sepsis | 15.3 | 5,919 (2,275–8,718) | 1,581 (499–2,807) | 1,998 (627–3,701) | 9,498 |
| Paralysis/coma | 15.3 | 977 (414–1,464) | 261 (81–464) | 330 (100–621) | 1,568 |
| Total | 28.8 | 122,235 (57,014–181,372 | 32,654 (11,033–64,818) | 41,245 (13,693–81,849) | 196,134 |
Venous Thromboembolism Prophylaxis
Rates of pharmacological thromboprophylaxis prescription were universally low across the various acute medical illnesses, ranging from 15.3% to 49.2% (Table 2). Thromboprophylaxis rates were highest among acutely ill hospitalized medical patients with stroke (49.2%), acute myocardial infarction (43.0%), and heart failure (40.1%). 72% of cancer patients, 80% of non-surgical trauma patients, and 85% of patients with paralysis or coma did not receive thromboprophylaxis.
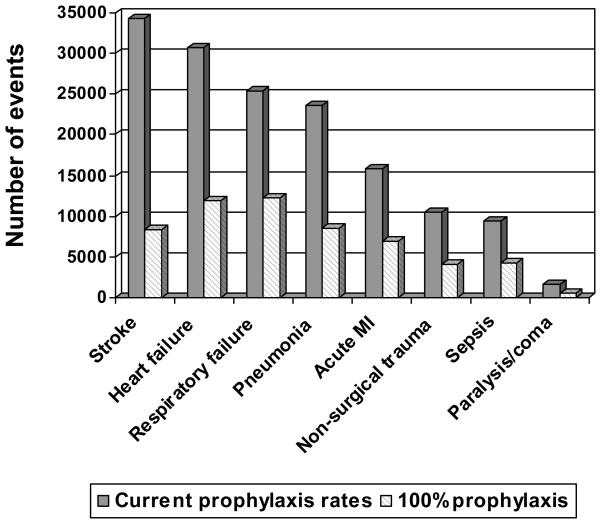
Compared with current rates of pharmacological prophylaxis prescription, 114,174 VTE-related events would have been prevented with 100% thromboprophylaxis utilization (Table 4). The number of symptomatic DVTs, symptomatic PEs, and VTE-related deaths would substantially decrease across all subgroups. The greatest reductions in VTE-related events would be observed in acutely ill medical patients with stroke (76%), paralysis or coma (72%), pneumonia (64%), non-surgical trauma (62%), heart failure (61%), sepsis (55%), acute myocardial infarction (56%), and respiratory failure (52%) (Figure 2).
Table 4.
Estimates of venous thromboembolic events in acutely ill hospitalized medical patients with 100% thromboprophylaxis. CI, confidence interval; DVT, deep vein thrombosis; PE, pulmonary embolism.
| Diagnosis | Prophylaxis rate (%) | Symptomatic DVT events (95% CI) | Symptomatic PE events (95% CI) | VTE-related deaths (95% CI) | Total VTE Events |
|---|---|---|---|---|---|
| Heart failure | 100 | 7,396 (4,769–26,261) | 1,976 (952–9,065) | 2,495 (1,268–11,439) | 11,867 |
| Respiratory failure | 100 | 7,602 (3,753–24,459) | 2,031 (800–7,903) | 2,565 (1,102–10,240) | 12,198 |
| Pneumonia | 100 | 5,290 (2,967–18,790) | 1,413 (695–5785) | 1,785 (852–7,714) | 8,488 |
| Cancer | 100 | 10,238 (2,856–19,144) | 2,735 (602–6,336) | 3,455 (757–7,891) | 16,428 |
| Stroke | 100 | 5,186 (1,307–9,984) | 1,385 (313–3,230) | 1,750 (373–4,006) | 8,321 |
| Acute myocardial infarction | 100 | 4,367 (2,508–14,078) | 1,167 (513–4,369) | 1,474 (645–5,592) | 7,008 |
| Non-surgical trauma | 100 | 2,512 (1,161–8,073) | 671 (261–2,625) | 848 (301–3,248) | 4,031 |
| Arthropathy/spondylopathy | 100 | 5,349 (1,455–10,372) | 1,429 (914–4,181) | 2,151 (995–5,598) | 8,929 |
| Sepsis | 100 | 2,646 (1,195–8,077) | 707 (255–2,657) | 893 (338–3,386) | 4,246 |
| Paralysis/coma | 100 | 276 (195–1,341) | 74 (42–418) | 94 (52–529) | 444 |
| Total | 100 | 50,862 (22,166–140,579) | 13,588 (5,347–46,569) | 17,510 (6,683–59,643) | 81,960 |
Figure 2.
Total venous thromboembolic events in acutely ill hospitalized medical patient populations with universal thromboprophylaxis utilization compared with current rates. MI, myocardial infarction.
DISCUSSION
More than eight million hospitalized acutely ill medical patients were at increased risk of VTE events in 2003. We calculated that acutely ill medical patients suffered 196,134 hospital-acquired VTE-related events, including symptomatic DVT, symptomatic PE, or VTE-related death. The majority were admitted with common medical illnesses, including heart failure, respiratory failure, pneumonia, and cancer. Despite having medical conditions that amplify the risk of VTE, rates of pharmacological thromboprophylaxis were low, with fewer than 50% of patients in each medical subgroup receiving any prophylaxis.
Other studies have documented an elevated risk of VTE among Medical Service patients with heart failure, stroke, malignancy, and respiratory disease (25–28), with poor thromboprophylaxis utilization even among high-risk subgroups (29, 30). Despite trials demonstrating the safety and efficacy of pharmacological modalities (31–35), thromboprophylaxis continues to be underutilized.
The 2008 U.S. Surgeon General’s Call to Action to Prevent DVT and PE provides a roadmap for Quality Improvement initiatives to augment thromboprophylaxis utilization among hospitalized medical patients (36). Increasing healthcare provider recognition of VTE risk among hospitalized medical patients and promoting awareness of evidence-based guidelines for VTE prevention through continuing education programs are critical. Computer-based decision support approaches, such as provider order entry alerts, are effective techniques for improving thromboprophylaxis utilization and decreasing symptomatic DVT and PE among hospitalized patients (37, 38). When a hospital staff member monitors hospital admissions and alerts physicians that their high-risk patients are not receiving prophylaxis, symptomatic DVT and PE rates fall (39). However, this approach appears to be less effective than computer-based decision support systems (39).
Our analysis may be limited by the accuracy of the HCUP Nationwide Inpatient Sample database, which is based on medical record coding and may not capture all conditions and risk factors contributing to the development of VTE. Because prescribing practices vary widely, pharmacological thromboprophylaxis rates and their impact on VTE-related events may not be representative of individual medical centers. Our estimates do not take into account medical patients with contraindications to pharmacological thromboprophylaxis or those receiving mechanical prophylaxis. In addition, our estimates represent U.S. data from a single year and may not be generalizable to other populations or years. Although we believe other years would yield similar results, we acknowledge that publication of the Seventh Edition of American College Chest Physicians guidelines for the prevention of VTE in 2004 might have changed thromboprophylaxis rates in subsequent years.
Our study is strengthened by the use of a database that represents a wide variety of U.S. medical centers and patient populations. The HCUP Nationwide Inpatient Sample database also allowed us to provide estimates of VTE-related events for a large sampling of acutely ill medical patients that would not be practical in a conventional observational study. Finally, the use of an event probability model provided us with the means to estimate the effect of thromboprophylaxis on VTE-related events.
In conclusion, two out of every 100 hospitalized medical patients suffered a VTE-related event in 2003. The number of VTE-related events would be halved with universal thromboprophylaxis. These data should serve as a catalyst for further research, educational, and policy efforts aimed at improving VTE prevention in hospitalized medical patients.
What is known about this topic?
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is an often-preventable complication of medical illness and hospitalization.
Common conditions among hospitalized medical patients, such as heart failure, chronic obstructive pulmonary disease, acute infection, atherosclerotic vascular disease, and malignancy, increase the risk of VTE.
Despite published guidelines for the prevention of VTE, underutilization of thromboprophylaxis among hospitalized medical patients continues to be a problem.
What does this paper add?
We estimate that more than eight million hospitalized acutely ill medical patients are at-risk for VTE.
Based on current thromboprophylaxis rates, two out of every 100 hospitalized medical patients suffered a VTE-related event.
The number of VTE-related events could be halved if thromboprophylaxis were consistently prescribed to all at-risk hospitalized medical patients.
Acknowledgments
This study was supported, in part, by an unrestricted research grant from sanofi-aventis.
ABBREVIATIONS
- DVT
deep vein thrombosis
- PE
pulmonary embolism
- VTE
venous thromboembolism
Footnotes
This article is not an exact copy of the original published article in Thrombosis and Haemostasis. The definitive publisher-authenticated version of Thromb Haemost 2009 Sep; 102(3): 505-10 is available online at: http://www.schattauer.de/en/magazine/subject-areas/journals-a-z/thrombosis-and-haemostasis/contents/archive/issue/963/manuscript/11647.html.
References
- 1.MacDougall DA, Feliu AL, Boccuzzi SJ, et al. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm. 2006;63:S5–15. doi: 10.2146/ajhp060388. [DOI] [PubMed] [Google Scholar]
- 2.Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008;149:698–707. doi: 10.7326/0003-4819-149-10-200811180-00004. [DOI] [PubMed] [Google Scholar]
- 3.Lang IM, Klepetko W. Chronic thromboembolic pulmonary hypertension: an updated review. Curr Opin Cardiol. 2008;23:555–559. doi: 10.1097/HCO.0b013e328311f254. [DOI] [PubMed] [Google Scholar]
- 4.Piazza G, Seddighzadeh A, Goldhaber SZ. Double trouble for 2,609 hospitalized medical patients who developed deep vein thrombosis: prophylaxis omitted more often and pulmonary embolism more frequent. Chest. 2007;132:554–561. doi: 10.1378/chest.07-0430. [DOI] [PubMed] [Google Scholar]
- 5.Spencer FA, Lessard D, Emery C, et al. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167:1471–1475. doi: 10.1001/archinte.167.14.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 7.Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence) Int Angiol. 2006;25:101–161. [PubMed] [Google Scholar]
- 8.Amin A, Stemkowski S, Lin J, et al. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost. 2007;5:1610–1616. doi: 10.1111/j.1538-7836.2007.02650.x. [DOI] [PubMed] [Google Scholar]
- 9.Kahn SR, Panju A, Geerts W, et al. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res. 2007;119:145–155. doi: 10.1016/j.thromres.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371:387–394. doi: 10.1016/S0140-6736(08)60202-0. [DOI] [PubMed] [Google Scholar]
- 11.Anderson FA, Jr, Zayaruzny M, Heit JA, et al. Estimated annual numbers of US acute-care hospital patients at risk for venous thromboembolism. Am J Hematol. 2007;82:777–782. doi: 10.1002/ajh.20983. [DOI] [PubMed] [Google Scholar]
- 12.Cohen AT, Agnelli G, Anderson FA, et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost. 2007;98:756–764. doi: 10.1160/TH07-03-0212. [DOI] [PubMed] [Google Scholar]
- 13.Yu HT, Dylan ML, Lin J, et al. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm. 2007;64:69–76. doi: 10.2146/ajhp060115. [DOI] [PubMed] [Google Scholar]
- 14.Warlow C, Terry G, Kenmure AC, et al. A double-blind trial of low doses of subcutaneous heparin in the prevention of deep-vein thrombosis after myocardial infarction. Lancet. 1973;2:934–936. doi: 10.1016/s0140-6736(73)92597-x. [DOI] [PubMed] [Google Scholar]
- 15.Sherman DG, Albers GW, Bladin C, et al. The efficacy and safety of enoxaparin versus unfractionated heparin for the prevention of venous thromboembolism after acute ischaemic stroke (PREVAIL Study): an open-label randomised comparison. Lancet. 2007;369:1347–1355. doi: 10.1016/S0140-6736(07)60633-3. [DOI] [PubMed] [Google Scholar]
- 16.Khorana AA, Francis CW, Culakova E, et al. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol. 2006;24:484–490. doi: 10.1200/JCO.2005.03.8877. [DOI] [PubMed] [Google Scholar]
- 17.Harenberg J, Schomaker U, Flosbach CM. Enoxaparin is superior to unfractionated heparin in the prevention of thromboembolic events in medical patients at increased thromboembolic risk. Blood. 1999;94 (suppl):399a. [Google Scholar]
- 18.Handley AJ. Low-dose heparin after myocardial infarction. Lancet. 1972;2:623–624. doi: 10.1016/s0140-6736(72)93016-4. [DOI] [PubMed] [Google Scholar]
- 19.Cohen AT, Turpie AG, Leizorovicz A, et al. Thromboprophylaxis with dalteparin in medical patients: which patients benefit? Vasc Med. 2007;12:123–127. doi: 10.1177/1358863X07079017. [DOI] [PubMed] [Google Scholar]
- 20.Alikhan R, Cohen AT, Combe S, et al. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX Study. Arch Intern Med. 2004;164:963–968. doi: 10.1001/archinte.164.9.963. [DOI] [PubMed] [Google Scholar]
- 21.Alikhan R, Cohen AT, Combe S, et al. Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Fibrinolysis. 2003;14:341–346. doi: 10.1097/00001721-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Oster G, Tuden RL, Colditz GA. A cost-effectiveness analysis of prophylaxis against deep-vein thrombosis in major orthopedic surgery. JAMA. 1987;257:203–208. [PubMed] [Google Scholar]
- 23.Ades AE, Claxton K, Sculpher M. Evidence synthesis, parameter correlation and probabilistic sensitivity analysis. Health Econ. 2006;15:373–381. doi: 10.1002/hec.1068. [DOI] [PubMed] [Google Scholar]
- 24.Doubilet P, Begg CB, Weinstein MC, et al. Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach. Med Decis Making. 1985;5:157–177. doi: 10.1177/0272989X8500500205. [DOI] [PubMed] [Google Scholar]
- 25.Stein PD, Beemath A, Meyers FA, et al. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006;119:60–68. doi: 10.1016/j.amjmed.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 26.Shetty R, Seddighzadeh A, Piazza G, et al. Chronic obstructive pulmonary disease and deep vein thrombosis: a prevalent combination. J Thromb Thrombolysis. 2008;26:35–40. doi: 10.1007/s11239-007-0157-y. [DOI] [PubMed] [Google Scholar]
- 27.Kelly J, Rudd A, Lewis R, et al. Venous thromboembolism after acute stroke. Stroke. 2001;32:262–267. doi: 10.1161/01.str.32.1.262. [DOI] [PubMed] [Google Scholar]
- 28.Beemath A, Stein PD, Skaf E, et al. Risk of venous thromboembolism in patients hospitalized with heart failure. Am J Cardiol. 2006;98:793–795. doi: 10.1016/j.amjcard.2006.03.064. [DOI] [PubMed] [Google Scholar]
- 29.Seddighzadeh A, Shetty R, Goldhaber SZ. Venous thromboembolism in patients with active cancer. Thromb Haemost. 2007;98:656–661. [PubMed] [Google Scholar]
- 30.Piazza G, Seddighzadeh A, Goldhaber SZ. Heart failure in patients with deep vein thrombosis. Am J Cardiol. 2008;101:1056–1059. doi: 10.1016/j.amjcard.2007.11.051. [DOI] [PubMed] [Google Scholar]
- 31.Wein L, Wein S, Haas SJ, et al. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167:1476–1486. doi: 10.1001/archinte.167.14.1476. [DOI] [PubMed] [Google Scholar]
- 32.Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999;341:793–800. doi: 10.1056/NEJM199909093411103. [DOI] [PubMed] [Google Scholar]
- 33.Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004;110:874–879. doi: 10.1161/01.CIR.0000138928.83266.24. [DOI] [PubMed] [Google Scholar]
- 34.Dentali F, Douketis JD, Gianni M, et al. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med. 2007;146:278–288. doi: 10.7326/0003-4819-146-4-200702200-00007. [DOI] [PubMed] [Google Scholar]
- 35.Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006;332:325–329. doi: 10.1136/bmj.38733.466748.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The surgeon general’s call to action to prevent deep vein thrombosis and pulmonary embolism. U.S. Department of Health and Human Services; 2008. [Accessed 11/30/08]. Available at: www.surgeongeneral.gov/topics/deepvein/calltoaction/call-to-action-on-dvt-2008.pdf. [PubMed] [Google Scholar]
- 37.Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352:969–977. doi: 10.1056/NEJMoa041533. [DOI] [PubMed] [Google Scholar]
- 38.Lecumberri R, Marques M, Diaz-Navarlaz MT, et al. Maintained effectiveness of an electronic alert system to prevent venous thromboembolism among hospitalized patients. Thromb Haemost. 2008;100:699–704. doi: 10.1160/th08-05-0337. [DOI] [PubMed] [Google Scholar]
- 39.Piazza G, Rosenbaum E, Pendergast W, et al. Physician Alerts to Prevent Symptomatic Venous Thromboembolism in Hospitalized Patients. Circulation. 2009 Apr 13; doi: 10.1161/CIRCULATIONAHA.108.841197. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]