Abstract
Background
Impulsivity is a hallmark characteristic of drug addiction and a prominent feature of externalizing disorders such as psychopathy that are commonly comorbid with drug addiction. In a previous study (Vassileva et al., 2007) we have shown that psychopathic heroin addicts evidence more impulsive decision-making on the Iowa Gambling Task relative to non-psychopathic heroin addicts. The goal of the current study was to investigate whether the observed impulse-control deficits in psychopathic heroin addicts would generalize to other neurocognitive domains of impulsivity, such as delay discounting and behavioral inhibition among a group of relatively “pure” heroin addicts in Bulgaria who participated in our previous study.
Methods
We tested 92 currently abstinent male heroin addicts, classified as psychopathic or non-psychopathic based on the Hare Psychopathy Checklist – Revised (PCL-R). We administered two neurocognitive tasks of impulsivity: (1) Delayed Rewards Discounting Task, a measure of temporal discounting of rewards; and (2) Passive Avoidance Learning Task, a measure of behavioral inhibition.
Results
Psychopathic heroin addicts were not impaired relative to non-psychopathic heroin addicts on the Delayed Rewards Discounting Task and the Passive Avoidance Learning Task, on the latter of which they showed better attentional capacity.
Conclusions
These results indicate that psychopathic heroin users are not uniformly impaired across neurocognitive domains of impulsivity. Combined with our previous findings, these results suggest that the presence of psychopathy may exacerbate decision-making deficits in psychopathic heroin addicts, but it may not have significant effect on other neurocognitive domains of impulsivity in this population.
Keywords: impulsivity, heroin addiction, psychopathy, decision-making, delay discounting, behavioral inhibition
1.0 Introduction
Drug addiction is conceptualized as a chronic relapsing disease characterized by long-term neuroadaptive changes in the brain and associated long-lasting impairments in neurocognitive functioning (Koob and Volkow, 2010). Some of the most notable neurocognitive deficits in substance dependent individuals (SDIs) are observed in the area of inhibitory and impulse control, proposed to be the core mechanisms underlying the compulsive pattern of drug seeking and use that persists despite negative health and social consequences for the drug user (Goldstein and Volkow, 2002; Jentsch and Taylor, 1999). There is accumulating evidence that drug users consistently show neurocognitive deficits in impulse control, yet compared to other drugs of abuse such as stimulants, cocaine, or cannabis, the long-term neurocognitive effects of opiates have received considerably less research attention, even though opiates continue to account for the largest proportion of people in drug treatment worldwide (United Nations Office on Drugs and Crime, 2008).
Evidence from the few studies available to date indicates that heroin users show impairments in impulse control that include impulsive decision-making (Brand et al., 2008; Fishbein et al., 2007; Verdejo-Garcia and Perez-Garcia, 2007; Verdejo-Garcia et al., 2007), impaired behavioral inhibition (Mintzer and Stitzer, 2002), increased risk-taking (Bornovalova et al., 2005), and increased discounting of delayed rewards (Kirby et al., 1999; Kirby and Petry, 2004; Madden et al., 1997). However, findings are often hard to interpret, given that with few exceptions (Fishbein et al., 2007; Vassileva et al., 2007), most neurocognitive studies of heroin users are based on polysubstance users, which makes it impossible to dissociate the neurocognitive effects of heroin from the confounding effects of other drugs.
Further, neurocognitive studies of heroin users often fail to control for the confounding effects of common comorbid psychiatric conditions such as Antisocial Personality Disorder (ASPD) or psychopathy, known to adversely affect neurocognitive functioning in a fashion similar to drug addiction. In a previous study of neurocognitive functioning in heroin users (Vassileva et al., 2007), we successfully circumvented these methodological challenges by conducting the study in Bulgaria, where patterns of heroin use are unique in that polysubstance dependence among heroin users is still relatively uncommon. We found that the presence of psychopathy among relatively “pure” heroin users with no significant history of dependence on other substances is associated with impulsive decision-making, as indexed by impaired performance on the Iowa Gambling Task. Yet, given the multidimensional nature of impulsivity, the question still remains of whether the observed neurocognitive deficits in impulsivity among psychopathic heroin addicts are limited to impulsive decision-making in particular, or whether they would generalize to other neurocognitive domains of impulsivity. In the current study, we expand our investigation of impulsivity among psychopathic heroin addicts, by examining patterns of performance in two additional neurocognitive domains of impulsivity, namely delay discounting and behavioral inhibition.
Impulsivity, clinically defined as “an individual’s predisposition toward rapid, unplanned reactions to internal or external stimuli without regards to the negative consequences of these reactions to themselves or others” (Moeller et al., 2001) is implicated in virtually all kinds of addictive behaviors (de Wit and Richards, 2004; Jentsch and Taylor, 1999). Although there has been a notable interest in impulsivity in the addiction literature, research has been plagued by the multifactorial nature of the construct (Evenden, 1999), which has presented a significant problem for investigating its biological underpinnings (Evenden, 1999). Although impulsivity is often thought of as a personality trait or a symptom of various psychiatric disorders, many contemporary conceptualizations of impulsivity involve distinct performance-based neurocognitive manifestations of the construct. Generally, neurocognitive measures typically capture one of three domains of impulsivity. The first domain is that of impulsive decision-making (Bechara et al., 1994), which reflects impaired ability to make decisions in accordance with long-term rather than short-term goals (Bechara et al., 2001) and is considered to reflect myopia for future consequences (Bechara, 2005). This type of impulsivity is sometimes referred to as “cognitive impulsivity” (Verdejo-Garcia et al., 2008) and is typically measured in the laboratory with gambling or betting tasks such as the Iowa Gambling Task (Bechara et al., 2001), the Cambridge Gambling Task (Rogers et al., 1999), or the Game of Dice Task (Brand et al., 2005). Conceptually similar is the domain of delayed rewards discounting, referring to the reduction in the present value of a future reward as the delay to that reward increases (Kirby et al., 1999). It is measured in the laboratory with delayed rewards discounting tasks, which involve making a selection between smaller immediate rewards and larger delayed rewards (Bickel and Marsch, 2001). The third major domain of impulsivity captured by neurocognitive tasks is related to impaired behavioral inhibition, manifested as inability to inhibit or withhold a prepotent or an already initiated response. This type of impulsivity is sometimes referred to as “motor impulsivity” (Bechara et al., 2000; Dougherty et al., 2003) and is measured with tasks as the Go/No-Go Discrimination Task or the Stop Signal Task. Substance dependent individuals show deficits on virtually all of these tasks (Bechara et al., 2001; Bechara and Damasio, 2002; Bornovalova et al., 2005; Fishbein et al., 2007; Kirby and Petry, 2004; Lejuez et al., 2004; Petry, 2003; Rogers et al., 1999; Verdejo-Garcia and Perez-Garcia, 2007; Verdejo-Garcia et al., 2007), whereas heroin users in particular appear to be impaired primarily on delayed reward discounting and decision-making tasks (Fishbein et al., 2007; Kirby et al., 1999; Madden et al., 1997; Odum et al., 2000), although research employing tasks of behavioral inhibition in this population is very limited.
In addition to its involvement in addictive behaviors, impulsivity has also been implicated in externalizing disorders that are highly comorbid with drug addiction, such as Antisocial Personality Disorder (ASPD) and psychopathy. In fact, drug and alcohol addiction were part of the original criteria for antisocial personality disorder (at the time called sociopathic personality disorder) in the DSM-I (American Psychiatric Association, 1952). The prevalence of lifetime substance use disorders in individuals with ASPD has been reported to be as high as 90% (Regier et al., 1990). The extremely high comorbidity of substance abuse and ASPD has led some to question whether ASPD should be viewed as independent of substance abuse (Gerstley et al., 1990; Regier et al., 1990), as it has been argued (Darke et al., 1998; Reardon et al., 2002) that it is possible to meet diagnostic criteria for ASPD on the basis of illicit drug use alone. A potentially more informative alternative to the somewhat over-inclusive diagnosis of ASPD is the construct of psychopathy (Hare, 1991); a disorder characterized by poor behavioral controls and antisocial lifestyle much at a par with ASPD, but also characterized by personality style consisting of distinct affective and interpersonal characteristics, not covered by the ASPD criteria. In fact, the proposed draft criteria for the upcoming revision of the Diagnostic and Statistical Manual (DSM-V) include many of the affective and interpersonal characteristics of psychopathy that are not currently covered by the ASPD criteria, and it has been proposed that the disorder be renamed to “Antisocial/Psychopathic Type” (American Psychiatric Association, 2010). ASPD and psychopathy have been associated with neurocognitive deficits in impulsivity, predominantly in the domain of behavioral inhibition (Dolan and Park, 2002; Newman and Kosson, 1986; Vollm et al., 2010). With regards to decision-making and delayed reward discounting, research still appears inconclusive with some studies reporting impulse control deficits (Blair et al., 2001; van Honk et al., 2002; Vassileva et al., 2007), whereas in other studies (Losel and Schmucker, 2004; Schmitt et al., 1999) psychopaths fail to exhibit such deficits.
The goal of the present study was to determine whether psychopathy in heroin addicts would be associated with neurocognitive deficits in two domains of impulsivity, which we did not investigate in our earlier study on decision-making in this population. In order to avoid the confounding effects of polysubstance use, we conducted the study in Bulgaria, where heroin addiction is highly prevalent but polysubstance dependence is still relatively rare. We administered two neurocognitive tasks, measuring two different dimensions of impulsivity: (1) Delayed Rewards Discounting Task, a measure of temporal discounting of monetary rewards; and (2) Passive Avoidance Learning Task, a “motivated Go/No-go” type of task, measuring one’s ability to inhibit inappropriate motor responses based on different reward and punishment contingencies. We hypothesized that the presence of psychopathy in heroin addicts would be associated with greater impairments in the two neurocognitive domains of impulsivity evaluated in the current study.
2.0 Methods
2.1 Participants
Participants were 92 currently abstinent male heroin users, ages 18–50, who were tested at St-Naum University Hospital of Neurology and Psychiatry in Sofia, Bulgaria. Participants were recruited by informational flyers distributed at outpatient drug treatment centers. The study was approved by the Institutional Review Boards of University of Illinois – Chicago and St-Naum University Hospital and written informed consent was obtained from all participants prior to any study procedures.
All subjects met DSM-IV criteria for heroin dependence. Participants were abstinent from drug and alcohol use at the time of testing, which was verified by a rapid urine toxicology screen and an alcohol Breathalyzer test. None of the subjects were on opioid substitution therapy. All subjects reported being HIV-seronegative. Exclusion criteria included: (1) positive rapid urine toxicology screen for opioids, cocaine, amphetamines, or marijuana; (2) positive alcohol Breathalyzer test; (2) history of open head injury or closed head injury with loss of consciousness exceeding 30 min; (3) CNS illness or injury; (4) schizophrenia, major depression, or bipolar disorder; (5) current psychotropic medication; (6) current dependence on alcohol, amphetamines, cocaine, or cannabis; (7) estimated IQ scores below 75.
Participants were classified into psychopathic (n=20) and non-psychopathic groups (n=72) based on scores on the Psychopathy Checklist – Revised (Hare, 1991).
2.2 Assessment
The Structured Clinical Interview for DSM-IV Substance Abuse Module (SCID-SAM: (First et al., 1996), translated into Bulgarian was used to assess for substance dependence. The Bulgarian translation of the Hare Psychopathy Checklist, Revised (PCL-R; Hare, 1991) was used to assign participants to psychopathic and non-psychopathic groups. We employed the standard cutoff score of 25 on the PCL-R typically used in studies with SDIs (Rutherford et al., 1999) and in European studies (Cooke et al., 2005; Cooke and Michie, 1999; Hare and Neumann, 2009) to classify participants as psychopathic or non-psychopathic. The Ravens Progressive Matrices was used to estimate IQ. In addition, we administered self-report questionnaires to assess depression (Beck et al., 1996) and anxiety (Spielberger, 1971).
2.3 Neurocognitive Tasks of Impulsivity
2.3.1 Passive Avoidance Learning Task (PALT)
We administered an adaptation of the Passive Avoidance Learning Task (Newman and Kosson, 1986), a type of computerized Go/No-Go discrimination task on which psychopathic individuals are commonly impaired (Newman et al., 1985; Newman and Kosson, 1986; Newman and Schmitt, 1998). The PALT involves mixed incentives (rewards and punishments) assessing the ability to respond to cues that have been previously paired with rewards and to withhold responding to cues that have been paired with punishment. This version of the task is sometimes referred to as “motivated go/no-go task” (Nigg, 2001) and is not identical to standard non-motivational go/no-go tasks, which typically do not include reward and/or punishment contingencies. Briefly, participants are told to learn by trial and error to respond to “good” numbers (S+) to earn reward and withhold a response to “bad” numbers (S−) to avoid punishment. Stimuli consist of 8 two-digit numbers presented in a pseudo random order for 80 trials and equally divided between S+ and S− stimuli. Each participant received a 4 trial reward pretreatment with only the S+ stimuli in order to establish a dominant response set for reward. Data from the reward pretreatment trials were not included in the analyses. Test trials began immediately after the reward pretreatment with no noticeable break. Following procedures of Newman and colleagues (Newman and Schmitt, 1998), each participant’s keypress response resulted in a visual, auditory, and monetary feedback. Correct responses were followed by a message “You win 10 cents!” appearing on the computer screen, a high-pitched tone, and the experimenter gave the participant a red plastic chip worth 10 cents. Incorrect responses were followed by a message “You lose 10 cents”, a low-pitched tone, and the experimenter removed a chip from the participant. No rewards were won or lost when a subject did not respond. Participants were told that the overall goal of the task was to earn as much money as possible and that they would redeem 10 cents for each chip that they had accumulated at the end of the experiment. We examined passive avoidance errors/errors of commission (failure to withhold responses to S− stimuli) as a primary index of impulsive responding, and errors of omission (failure to respond to S+ stimuli), typically used as an index of inattentiveness. Data were analyzed with repeated measures ANOVA, with group (psychopaths, non-psychopaths) as the between subjects factor and error type (commission, omission) as the within subjects factor.
2.3.2 Delayed Reward Discounting Task (DRDT)
The delay discounting model of impulsivity defines impulsive choice as the choice of a smaller sooner reward over a larger later reward (Ainslie, 1975). In general, as discount rates increase, people are progressively more inclined to choose immediate over delayed rewards (Kirby, 2009). In this respect, higher discount rates serve as a behavioral index of impulsivity and delay discounting has shown good external and criterion validity as such (Kirby, 2009). A number of studies reveal that SDIs discount delayed rewards at significantly higher rates than non-SDIs (reviewed in Reynolds, 2006), consistent with clinical observations that SDIs typically choose a smaller immediate reward (i.e. taking the drug) over larger but delayed rewards (e.g. improved health, better financial status, etc.).
We assessed delayed reward discounting using the Monetary-Choice Questionnaire (MCQ) following procedures used by Kirby and colleagues (Kirby et al., 1999). The questionnaire consists of a set of 27 choices between smaller immediate rewards (S) available today and larger delayed rewards (L) available at delays ranging from 7 to 186 days. Given that discount rates usually decrease as the amount of the rewards increase (Kirby, 1997), the 27 questions were grouped in one of three categories based on the approximate magnitudes of the delayed rewards: small ($25–35), medium ($50–60) and large ($75–85). In order to encourage accurate responding, participants were given a 1-in-6 chance to receive an actual reward upon task completion (Kirby et al., 1999), consisting of 1/10th of the value of one of their previous choices. We decided to adjust downward the value of the actual reward based on ethical concerns that the dollar-amount values in the MCQ were excessively high by Bulgarian standards. The US currency of the reward values was replaced with the equivalent in Bulgarian Leva.
Discount rate parameters were estimated from participants’ patterns of choices across the nine questions in each of the three magnitude categories (Kirby et al., 1999). The discount rate was determined by k, a hyperbolic discount parameter that indexes how rapidly the participants’ valuation of the reward declines as the delay interval increases. We estimated the value of k that would yield indifference between S and L for each of the 27 questions using the following equation: V=A/(1+kD), where V is the present value of reward A available at delay D, and k is the discount rate parameter (Mazur, 1987). For example, in the question: “Would you prefer $31 today or $85 in 7 days?” k has a value of 0.25. A participant with a k of 0.25 would be indifferent between the two rewards. A choice of the immediate reward would result in a k greater than 0.25. Likewise, participants choosing the delayed reward would obtain a k smaller than 0.25.
Estimated k values were assigned according to the highest proportion of the participant’s choices consistent with that value. Within each magnitude category (small, medium, large) the 9 choices that the participant makes define 10 ranges where the value of k might fall. Within each reward magnitude, each participant is assigned a k value that has the highest proportion of his or her choices consistent with that value (Kirby and Petry, 2004). An overall value of k for each participant can also be calculated from the geometric mean of the 3 k values. Consistency is defined as the discount rate that produces the highest relative consistency across trials and, therefore, gives the best estimate of the participant’s k value (Kirby et al., 1999). However, participants’ choices are not always consistent with a single value of k. Participants who evidenced more than 2 inconsistent choices on any of the 3 magnitude conditions were excluded from the analyses (Kirby et al., 1999).
Data were analyzed with repeated measure ANOVA, with group (psychopaths, non-psychopaths) as the between subjects factor and reward magnitude (small, medium, large) as the within subjects factor.
3.0 Results
3.1 Participants’ Characteristics
The psychopathic and non-psychopathic groups were well matched on demographic, mental health, and substance use characteristics (Table 1). Psychopathic heroin addicts had significantly greater history of incarceration than the non-psychopathic heroin addicts [X2(1)=23.1, p<.000]. In fact, all participants (n=6) who reported having a history of incarceration were from the psychopathic group. Nonetheless, 70% of participants in the psychopathic group reported no history of incarceration.
Table 1.
Participants’ Characteristics
| Non-psychopaths (n=72) | Psychopaths (n=20) | p | |
|---|---|---|---|
| Age | 26.64 (6.31) | 26.00 (4.89) | .68 |
| Years of Education | 11.04 (1.76) | 11.20 (2.24) | .74 |
| Estimated IQ | 102.95 (12.66) | 110.60 (12.89) | .09 |
| BDI-II | 11.76 (7.72) | 10.70 (5.57) | .57 |
| STAI-State | 38.08 (9.53) | 37.85 (9.85) | .92 |
| STAI-Trait | 40.68 (9.73) | 43.65 (10.27) | .24 |
| Days since last used heroin (Medians, Inter Quartile Range) | 165 (401) | 150 (289) | .43 |
| Years of heroin use | 4.25 (2.15) | 4.23 (1.79) | .98 |
| Past alcohol dependence (%) | 1 (1.4%) | 0 | |
| Past cannabis dependence (%) | 0 | 2 (10%) | |
| Past stimulant dependence (%) | 0 | 0 | |
| Past cocaine dependence (%) | 0 | 0 |
Note: Unless otherwise noted, data are presented as means and standard deviations
BDI-II: Beck Depression Inventory, 2nd Edition; STAI: State-Trait Anxiety Inventory
3.2 Passive Avoidance Learning Task
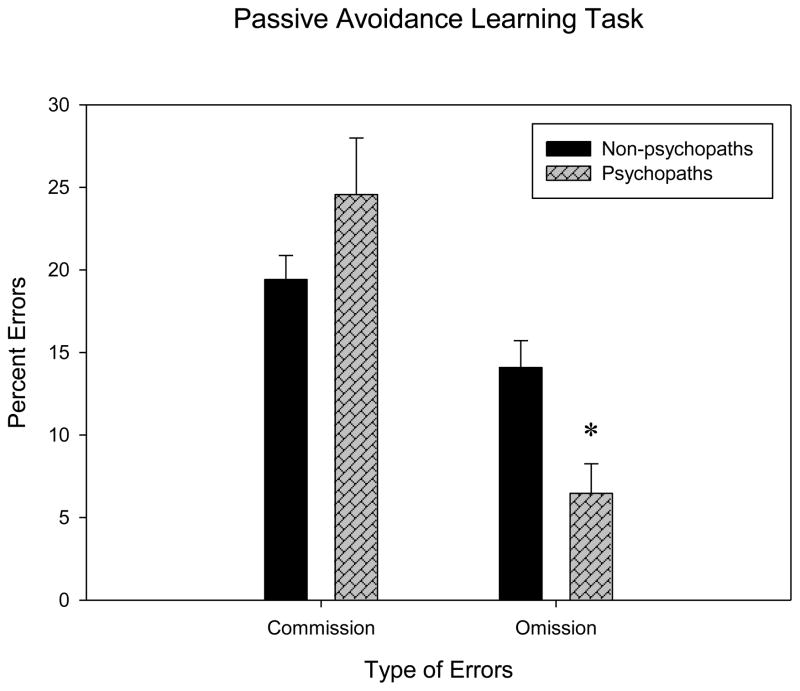
Six participants had missing data on the task due to technical difficulties with the computer program; therefore results are based on data from 17 psychopathic heroin addicts and 69 non-psychopathic heroin addicts. Both errors of commission and errors of omission on the Passive Avoidance Learning Task were not normally distributed; therefore the data were logarithmically transformed and analyses performed on the transformed data. Consistent with the literature, the ANOVA revealed a significant main effect for type of errors [F(1,67)=15.85, p<.0001; partial η2=.19], indicating that participants committed significantly more errors of commission than omission. In addition, we observed a marginally significant effect of psychopathy [F(1,67)=3.89, p<.053; partial η2=.06] and a significant interaction between type of errors and psychopathy [F(1,67)=6.29, p<.02; partial η2=.09]. When the interaction was explored by planned comparisons, results indicated that psychopathic heroin addicts made significantly fewer errors of omission than non-psychopathic heroin addicts [F(1,67)=8.34; p<.005; partial η2=.11], but there were no significant group differences in errors of commission [F(1,84)=1.55; p<.22; partial η2=.02] (see Table 2 and Figure 1).
Table 2.
Performance of psychopathic and non-psychopathic heroin addicts on impulsivity tasks
| Non-Psychopaths | Psychopaths | |
|---|---|---|
| Passive Avoidance Learning | ||
| Errors of commission (%) | 19.42 (12.21) | 24.56 (14.37) |
| Errors of omission (%) | 14.09 (13.87) | 6.47 (6.38) |
| Delayed Reward Discounting | ||
| Small Magnitude | .13 (.10) | .12 (.08) |
| Medium Magnitude | .12 (.09) | .10 (.08) |
| Large Magnitude | .12 (.09) | .10 (.07) |
Note: Data are presented as means and standard deviations. For ease of interpretation, scores reflect non-transformed values
Figure 1.
Performance of Psychopathic and Non-Psychopathic Heroin Addicts on the Passive Avoidance Learning Task
3.3 Delayed Rewards Discounting Task
Three participants had missing data on the task and one participant had more than two inconsistent choices, therefore they were excluded from the analyses. Data from the Delayed Rewards Discounting Task were also not normally distributed, therefore we applied a logarithmic transformation in order to approximately normalize the distribution of k values (Kirby et al., 1999). We did not observe significant group main effect [F(1,87)=.21; p=.65; partial η2=.002] or interaction effect [F(2,174)=..71; p=.49; partial η2=.008]. For descriptive characteristics of the data, please refer to Table 2.
4. Discussion
In this study, we examined whether the neurocognitive deficits in impulsive decision-making that we previously observed in psychopathic heroin addicts (Vassileva et al., 2007) would generalize to other neurocognitive domains of impulsivity, such as delayed rewards discounting and behavioral inhibition. Current results indicate that psychopathic heroin addicts do not show impulse control deficits in these domains of impulsivity relative to non-psychopathic heroin addicts. Contrary to our hypotheses, not only were psychopathic heroin addicts not more impulsive on these two tasks, but in fact there was evidence that they displayed superior attentional capacity on the Passive Avoidance Learning Task relative to non-psychopathic heroin addicts, as indicated by the significantly fewer errors of omission that they committed on the task.
Combined with our previous finding of more impulsive decision-making in psychopathic heroin users based on the same study sample (Vassileva et al., 2007), these results suggest that psychopathic heroin addicts are not uniformly impaired across various neurocognitive domains of impulsivity. Of three domains of impulsivity measuring decision-making, delay discounting, and behavioral inhibition, psychopathic heroin addicts evidenced more impulsive decision-making relative to non-psychopathic heroin addicts, yet their performance was not impaired in other domains of impulsivity. Therefore, the presence of psychopathy may exacerbate decision-making deficits in heroin addicts, but it may not have a significant effect on other domains of impulsivity in this population. This finding could have important clinical implications in light of reports showing that decision-making, but not behavioral inhibition or delay discounting, predict abstinence from illicit drug use among heroin addicts (Passetti et al., 2008).
The lack of group differences in performance on the two impulsivity tasks used in the current study may be related to the fact that both the PALT and the DRDT involved the possibility of receiving actual monetary rewards. In contrast, the IGT on which we previously showed that psychopathic heroin addicts are impaired relative to non-psychopathic heroin addicts (Vassileva et al., 2007) involves only hypothetical rewards. Though speculative, the possibility to receive real monetary rewards may be of sufficient motivational significance for psychopathic heroin addicts that it may differentially reduce the apparent impulse-control deficits that they display on tasks with no actual monetary contingencies, such as the IGT. This hypothesis is consistent with results from studies showing greater responsivity to reward in psychopaths with no concurrent impairments in passive avoidance learning (Scerbo et al., 1990) and with some of the earliest reports of this nature (Schmauk, 1970) indicating that psychopaths learn to avoid punishment better under a “tangible punishment” condition associated with loss of monetary rewards, than in “physical punishment” or “social punishment” conditions. It is also in line with recent reports revealing mesolimbic dopamine reward system hypersensitivity in psychopaths in response to actual monetary rewards (Buckholtz et al., 2010). In this line of thought, it is of interest whether the performance of psychopathic heroin addicts on the IGT would improve if the task incorporated actual monetary rewards. Recently, in one of the first within-subject design studies administering the IGT with and without monetary rewards, Vadhan and colleagues (Vadhan et al., 2009) reported that monetary rewards improve performance of cocaine addicts on the IGT. On the other hand, research with delay discounting procedures (reviewed in Bickel and Marsch, 2001) indicates that although the discounting functions in tasks that use hypothetical rewards are quantitatively similar to those that use actual rewards, discount rates are higher with actual than with hypothetical rewards. However, the reward dollar amounts used in studies with actual rewards are generally lower than those used in studies with hypothetical rewards (Kirby, 1997). With regards to the PALT and monetary rewards, many studies reporting passive avoidance learning deficits in psychopaths have used only points or other non-monetary incentives, and not actual monetary rewards (Blair et al., 2004; Kosson et al., 1990; Newman et al., 1985; Newman and Schmitt, 1998), therefore the effects of actual rewards on psychopaths’ performance are still not well understood.
Our finding that psychopaths evidence fewer errors of omission than non-psychopaths on the PALT and therefore show better attention than non-psychopaths under certain circumstances deserves discussion. Indeed, our study is not the first to show enhanced attentional capacities in psychopaths under certain circumstances. A number of studies (Newman et al., 1985; Newman and Kosson, 1986) have noted similar trends for fewer omission errors on the PALT in psychopaths. Scerbo and colleagues (Scerbo et al., 1990) found significantly fewer omission errors in psychopaths and suggested that they are capable of showing enhanced attention when sufficiently motivated to do so, which is in line with our findings. Similarly, research reveals that psychopaths show better attentional processing of relevant stimuli as indexed by enhanced P300 amplitudes (Raine, 1989, 1992; Raine & Venables, 1988). Research also shows that frontal lobes mediated attentional and working memory functions are often perfectly intact and even superior in psychopaths (in Flor et al., 2002). It has been suggested (Raine and Dunkin, 1990) that such compensatory strengths in certain attentional or cognitive abilities in psychopaths “could be capitalized on in therapeutic settings” and therefore may have significant implications for treatment. For example, if psychopaths are hypersensitive to reward and hyposensitive to punishment, intervention programs may be more effective if they emphasize the reward of prosocial behavior rather than punishment of antisocial behavior (Raine and Dunkin, 1990).
On the other hand, current results are not consistent with results from a number of studies reporting pronounced deficits in passive avoidance learning in psychopathic individuals (Newman et al., 1985; Newman and Kosson, 1986; Newman and Schmitt, 1998). This apparent discrepancy could be due to differences in the sample population under investigation, particularly the presence or absence of drug addiction. In fact, most of the studies reporting passive avoidance learning deficits in psychopaths do not provide any information on the drug using status of their participants (Newman and Kosson, 1986; Newman and Schmitt, 1998). Research reveals that the two-dimensional structure of the PCL-R-based psychopathy, commonly observed among prisoners and forensic psychiatric patients is not found among SDIs, who in contrast display a unidimensional structure of the construct (McDermott et al., 2000). Therefore, the structure of psychopathy in SDIs appears still not to be fully determined. Further, given that most extant studies with psychopathic individuals are based on participants recruited from federal prisons, it is not clear to what extent incarceration and criminality contribute to the abnormalities previously observed in these studies (Flor et al., 2002). In fact, virtually all of the studies reporting passive avoidance deficits have been based on samples of incarcerated psychopaths, whereas participants in our study were recruited from a community sample of heroin users, such that only 6.5% of our participants (all of whom were psychopaths) reported having a history of incarceration. It has been suggested (Widom, 1977) that the study of incarcerated psychopaths provides a biased sample of psychopathic individuals who may essentially represent “unsuccessful” psychopaths, whereas “successful” psychopaths typically manage to avoid incarceration. Using this criterion, many of our psychopathic participants would be considered “successful” psychopaths, given that 70% of them had no history of incarceration, even though they reported at times extensive criminal activity. Recent research reveals that structural brain abnormalities such as reduced prefrontal gray matter volume (Yang et al., 2005), increased callosal white matter volume and length (Raine et al., 2003), and asymmetrical hippocampi (Raine et al., 2004), appear to be limited to “unsuccessful” psychopaths, whereas no such abnormalities are noted in “successful” psychopaths. Similarly, “successful” psychopaths have shown superior neurocognitive executive functioning than both “unsuccessful” psychopaths and controls (Ishikawa et al., 2001). Together, these studies suggest that many of the previously reported neurocognitive and neuroimaging impairments in psychopaths may be limited to “unsuccessful” psychopaths. Therefore, the current results should not be readily generalized to psychopathic individuals from incarcerated samples or to psychopathic individuals with no history of substance dependence.
Several limitations of this study should be noted. First, the HIV-serostatus of our participants was determined on the basis of self-report, therefore, some of our participants could have been HIV-seropositive and not aware of their HIV-serostatus. This is of concern, in light of the significantly deleterious effects of HIV on neurocognitive functioning. However, given that the prevalence of HIV among Bulgarian injection drug users (IDUs) is still relatively low and was even lower (0.59% in IDUs) at the time when the study was conducted (United Nations Programme on HIV/AIDS, 2010), we believe that the likelihood that some of our participants could have been HIV-seropositive is very low. Similarly, we did not assess history of smoking in our participants, and nicotine has well-known effects on neurocognitive function. Further, we did not include other measures of executive functioning or self-report personality measures of impulsivity in our battery, which would have strengthened our design. We have begun to address these limitations in our currently ongoing studies with drug users in Bulgaria, which now include rapid HIV testing, assessment of smoking history and status, and an expanded battery of neurocognitive and personality tests. Finally, although the selection of relatively “pure” heroin users helped us address a significant methodological limitation in the literature, this nonetheless limits the generalizability of our findings, given that most heroin users in Western Europe and North America are polysubstance users.
In summary, our program of research addressing neurocognitive impulsivity among psychopathic heroin addicts indicates that psychopathy is not invariably associated with impulsive responding among this population. Out of three neurocognitive domains of impulsivity that we have tested, in a previous study we found that psychopathy had an effect on impulsive decision-making (Vassileva et al., 2007), yet in the present study psychopathy did not appear to significantly affect other domains of impulsivity in heroin addicts. These results have significant implications for treatment programs that could be tailored to the specific type of neurocognitive impulsivity displayed by different sub-groups of SDIs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ainslie GW. Specious reward: A behavioral theory of impulsiveness and impulsive control. Psychol Bull. 1975;82:463–496. doi: 10.1037/h0076860. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 1. 1952. (DSM-I) Ref Type: Generic. [Google Scholar]
- American Psychiatric Association. Antisocial Personality Disorder, American Psychiatric Association DSM-5 Development. 2010 http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=16. 3-17-2010. Ref Type: Electronic Citation.
- Bechara A. Decision making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat Neurosci. 2005;8:1458–1463. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50:7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H. Decision-making and addiction (part I): impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40:1675–1689. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39:376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000;123(Pt 11):2189–2202. doi: 10.1093/brain/123.11.2189. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Blair RJ, Colledge E, Mitchell DG. Somatic markers and response reversal: is there orbitofrontal cortex dysfunction in boys with psychopathic tendencies? J Abnorm Child Psychol. 2001;29:499–511. doi: 10.1023/a:1012277125119. [DOI] [PubMed] [Google Scholar]
- Blair RJ, Mitchell DG, Leonard A, Budhani S, Peschardt KS, Newman C. Passive avoidance learning in individuals with psychopathy: modulation by reward but not by punishment. Pers Individ Dif. 2004;37:1179–1192. [Google Scholar]
- Bornovalova MA, Daughters SB, Hernandez GD, Richards JB, Lejuez CW. Differences in impulsivity and risk-taking propensity between primary users of crack cocaine and primary users of heroin in a residential substance-use program. Exp Clin Psychopharmacol. 2005;13:311–318. doi: 10.1037/1064-1297.13.4.311. [DOI] [PubMed] [Google Scholar]
- Brand M, Fujiwara E, Borsutzky S, Kalbe E, Kessler J, Markowitsch HJ. Decision-making deficits of Korsakoff patients in a new gambling taks with explicit rules: associations with executive functions. Neuropsychology. 2005;19:267–277. doi: 10.1037/0894-4105.19.3.267. [DOI] [PubMed] [Google Scholar]
- Brand M, Roth-Bauer M, Driessen M, Markowitsch HJ. Executive functions and risky decision-making in patients with opiate dependence. Drug Alcohol Depend. 2008;97:64–72. doi: 10.1016/j.drugalcdep.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Buckholtz JW, Treadway MT, Cowan RL, Woodward ND, Benning SD, Li R, Ansari MS, Baldwin RM, Schwartzman AN, Shelby ES, Smith CE, Cole D, Kessler RM, Zald DH. Mesolimbic dopamine reward system hypersensitivity in individuals with psychopathic traits. Nat Neurosci. 2010;13:419–421. doi: 10.1038/nn.2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke DJ, Michie C. Psychopathy across cultures: North America and Scotland compared. J Abnorm Psychol. 1999;108:58–68. doi: 10.1037//0021-843x.108.1.58. [DOI] [PubMed] [Google Scholar]
- Cooke DJ, Michie C, Hart SD, Clark D. Assessing psychopathy in the UK: concerns about cross-cultural generalisability. Br J Psychiatry. 2005;186:335–341. doi: 10.1192/bjp.186.4.335. [DOI] [PubMed] [Google Scholar]
- Darke S, Kaye S, Finlay-Jones R. Antisocial personality disorder, psychopathy and injecting heroin use. Drug Alcohol Depend. 1998;52:63–69. doi: 10.1016/s0376-8716(98)00058-1. [DOI] [PubMed] [Google Scholar]
- de Wit H, Richards JB. Dual determinants of drug use in humans: reward and impulsivity. Nebr Symp Motiv. 2004;50:19–55. [PubMed] [Google Scholar]
- Dolan M, Park I. The neuropsychology of antisocial personality disorder. Psychol Med. 2002;32:417–427. doi: 10.1017/s0033291702005378. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Bjork JM, Harper RA, Marsh DM, Moeller FG, Mathias CW, Swann AC. Behavioral impulsivity paradigms: a comparison in hospitalized adolescents with disruptive behavior disorders. J Child Psychol Psychiatry. 2003;44:1145–1157. doi: 10.1111/1469-7610.00197. [DOI] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology (Berl) 1999;146:348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis-I Disorders. Biometrics Research Department; 1996. [Google Scholar]
- Fishbein DH, Krupitsky E, Flannery BA, Langevin DJ, Bobashev G, Verbitskaya E, Augustine CB, Bolla KI, Zvartau E, Schech B, Egorova V, Bushara N, Tsoy M. Neurocognitive characterizations of Russian heroin addicts without a significant history of other drug use. Drug Alcohol Depend. 2007;90:25–38. doi: 10.1016/j.drugalcdep.2007.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flor H, Birbaumer N, Hermann C, Ziegler S, Patrick CJ. Aversive Pavlovian conditioning in psychopaths: peripheral and central processes. Psychophysiology. 2002;39:505–518. doi: 10.1017.S0048577202394046. [DOI] [PubMed] [Google Scholar]
- Gerstley LJ, Alterman AI, McLellan AT, Woody GE. Antisocial personality disorder in patients with substance abuse disorders: a problematic diagnosis? Am J Psychiatry. 1990;147:173–178. doi: 10.1176/ajp.147.2.173. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hare RD. Manual for the Hare Psychopathy Checklist - Revised. Toronto, Ontario, Canada: Multi-Health Systems; 1991. [Google Scholar]
- Hare RD, Neumann CS. Psychopathy: assessment and forensic implications. Can J Psychiatry. 2009;54:791–802. doi: 10.1177/070674370905401202. [DOI] [PubMed] [Google Scholar]
- Ishikawa SS, Raine A, Lencz T, Bihrle S, LaCasse L. Autonomic stress reactivity and executive functions in successful and unsuccessful criminal psychopaths from the community. J Abnorm Psychol. 2001;110:423–432. doi: 10.1037//0021-843x.110.3.423. [DOI] [PubMed] [Google Scholar]
- Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by reward-related stimuli. Psychopharmacology (Berl) 1999;146:373–390. doi: 10.1007/pl00005483. [DOI] [PubMed] [Google Scholar]
- Kirby KN. Bidding on the future: evidence against normative discounting of delayed rewards. Journal of Experimental Psychology: General. 1997;126:54–70. [Google Scholar]
- Kirby KN. One-year temporal stability of delay-discount rates. Psychon Bull Rev. 2009;16:457–462. doi: 10.3758/PBR.16.3.457. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosson DS, Smith SS, Newman JP. Evaluating the construct validity of psychopathy in black and white male inmates: three preliminary studies. J Abnorm Psychol. 1990;99:250–259. doi: 10.1037//0021-843x.99.3.250. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Simmons BL, Aklin WM, Daughters SB, Dvir S. Risk-taking propensity and risky sexual behavior of individuals in residential substance use treatment. Addict Behav. 2004;29:1643–1647. doi: 10.1016/j.addbeh.2004.02.035. [DOI] [PubMed] [Google Scholar]
- Losel F, Schmucker M. Psychopathy, risk taking, and attention: a differentiated test of the somatic marker hypothesis. J Abnorm Psychol. 2004;113:522–529. doi: 10.1037/0021-843X.113.4.522. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: drug and monetary rewards. Exp Clin Psychopharmacol. 1997;5:256–262. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Mazur J. An adjusting procedure for delayed reinforcement. In: Commons M, Mazur J, Nevin J, Rachlin H, editors. The Effect of Delay and of Intervening Events on Reinforcement Value. Erlbaum; New Jersey: 1987. pp. 55–73. [Google Scholar]
- McDermott PA, Alterman AI, Cacciola JS, Rutherford MJ, Newman JP, Mulholland EM. Generality of Psychopathy Checklist-Revised factors over prisoners and substance-dependent patients. J Consult Clin Psychol. 2000;68:181–186. [PubMed] [Google Scholar]
- Mintzer MZ, Stitzer ML. Cognitive impairment in methadone maintenance patients. Drug Alcohol Depend. 2002;67:41–51. doi: 10.1016/s0376-8716(02)00013-3. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Newman JP, Kosson DS. Passive avoidance learning in psychopathic and nonpsychopathic offenders. J Abnorm Psychol. 1986;95:252–256. [PubMed] [Google Scholar]
- Newman JP, Schmitt WA. Passive avoidance in psychopathic offenders: a replication and extension. J Abnorm Psychol. 1998;107:527–532. doi: 10.1037//0021-843x.107.3.527. [DOI] [PubMed] [Google Scholar]
- Newman JP, Widom CS, Nathan S. Passive avoidance in syndromes of disinhibition: psychopathy and extraversion. J Pers Soc Psychol. 1985;48:1316–1327. doi: 10.1037//0022-3514.48.5.1316. [DOI] [PubMed] [Google Scholar]
- Nigg JT. Is ADHD a disinhibitory disorder? Psychol Bull. 2001;127:571–598. doi: 10.1037/0033-2909.127.5.571. [DOI] [PubMed] [Google Scholar]
- Odum AL, Madden GJ, Badger GJ, Bickel WK. Needle sharing in opioid-dependent outpatients: psychological processes underlying risk. Drug Alcohol Depend. 2000;60:259–266. doi: 10.1016/s0376-8716(00)00111-3. [DOI] [PubMed] [Google Scholar]
- Passetti F, Clark L, Mehta MA, Joyce E, King M. Neuropsychological predictors of clinical outcome in opiate addiction. Drug Alcohol Depend. 2008;94:82–91. doi: 10.1016/j.drugalcdep.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Petry NM. Discounting of money, health, and freedom in substance abusers and controls. Drug Alcohol Depend. 2003;71:133–141. doi: 10.1016/s0376-8716(03)00090-5. [DOI] [PubMed] [Google Scholar]
- Raine A. Evoked potentials and psychopathy. International Journal of Psychophysiology. 1989;8:1–16. doi: 10.1016/0167-8760(89)90013-5. [DOI] [PubMed] [Google Scholar]
- Raine A. Schizotypical and borderline features in psychopathic criminals. Personality and Individual Differences. 1992;13:717–722. [Google Scholar]
- Raine A, Dunkin J. The genetic and psychophysiological basis of antisocial behavior: implications for counseling and therapy. J Couns Dev. 1990;68:637–644. [Google Scholar]
- Raine A, Ishikawa SS, Arce E, Lencz T, Knuth KH, Bihrle S, LaCasse L, Colletti P. Hippocampal structural asymmetry in unsuccessful psychopaths. Biol Psychiatry. 2004;55:185–191. doi: 10.1016/s0006-3223(03)00727-3. [DOI] [PubMed] [Google Scholar]
- Raine A, Lencz T, Taylor K, Hellige JB, Bihrle S, LaCasse L, Lee M, Ishikawa S, Colletti P. Corpus callosum abnormalities in psychopathic antisocial individuals. Arch Gen Psychiatry. 2003;60:1134–1142. doi: 10.1001/archpsyc.60.11.1134. [DOI] [PubMed] [Google Scholar]
- Raine A, Venables PH. Enhanced P3 evoked potentials during a continuous performance task in psychopaths. Psychophysiology. 1988;25:30–38. doi: 10.1111/j.1469-8986.1988.tb00954.x. [DOI] [PubMed] [Google Scholar]
- Reardon ML, Lang AR, Patrick CJ. An evaluation of relations among antisocial behavior, psychopathic traits, and alcohol problems in incarcerated men. Alcohol Clin Exp Res. 2002;26:1188–1197. doi: 10.1097/01.ALC.0000023988.43694.FE. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol. 2006;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K, Baker NB, Hunter J, Carthy T, Booker E, London M, Deakin JF, Sahakian BJ, Robbins TW. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999;20:322–339. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- Rutherford M, Cacciola JS, Alterman AI, McKay JR, Cook TG. The 2-year test-retest reliability of the Psychopathy Checklist Revised in methadone patients. Assessment. 1999;6:285–292. doi: 10.1177/107319119900600308. [DOI] [PubMed] [Google Scholar]
- Scerbo A, Raine A, O’Brien M, Chan CJ, Rhee C, Smiley N. Reward dominance and passive avoidance learning in adolescent psychopaths. J Abnorm Child Psychol. 1990;18:451–463. doi: 10.1007/BF00917646. [DOI] [PubMed] [Google Scholar]
- Schmauk FG. Punishment, arousal, and avoidance learning in sociopaths. J Abnorm Psychol. 1970;76:325–335. doi: 10.1037/h0030398. [DOI] [PubMed] [Google Scholar]
- Schmitt WA, Brinkley CA, Newman JP. Testing Damasio’s somatic marker hypothesis with psychopathic individuals: risk takers or risk averse? J Abnorm Psychol. 1999;108:538–543. doi: 10.1037//0021-843x.108.3.538. [DOI] [PubMed] [Google Scholar]
- Spielberger CDGRLLRE. State-Trait Anxiety Inventory. Palo Alto: 1971. [Google Scholar]
- United Nations Office on Drugs and Crime. UNODC World Drug Report 2008. 2008 http://www.unodc.org/documents/wdr/WDR_2008/WDR_2008_eng_web.pdf. Ref Type: Electronic Citation.
- United Nations Programme on HIV/AIDS. [Accessed on 09-17-2010];UNAIDS Bulgaria 2010 Progress Report. 2010 http://data.unaids.org/pub/Report/2010/bulgaria_2010_country_progress_report_en.pdf.
- Vadhan NP, Hart CL, Haney M, van Gorp WG, Foltin RW. Decision-making in long-term cocaine users: Effects of a cash monetary contingency on Gambling task performance. Drug Alcohol Depend. 2009;102:95–101. doi: 10.1016/j.drugalcdep.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Honk J, Hermans EJ, Putman P, Montagne B, Schutter DJ. Defective somatic markers in sub-clinical psychopathy. Neuroreport. 2002;13:1025–1027. doi: 10.1097/00001756-200206120-00009. [DOI] [PubMed] [Google Scholar]
- Vassileva J, Petkova P, Georgiev S, Martin EM, Tersiyski R, Raycheva M, Velinov V, Marinov P. Impaired decision-making in psychopathic heroin addicts. Drug Alcohol Depend. 2007;86:287–289. doi: 10.1016/j.drugalcdep.2006.06.015. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehav Rev. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Perez-Garcia M. Profile of executive deficits in cocaine and heroin polysubstance users: common and differential effects on separate executive components. Psychopharmacology (Berl) 2007;190:517–530. doi: 10.1007/s00213-006-0632-8. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia AJ, Perales JC, Perez-Garcia M. Cognitive impulsivity in cocaine and heroin polysubstance abusers. Addict Behav. 2007;32:950–966. doi: 10.1016/j.addbeh.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Vollm B, Richardson P, McKie S, Reniers R, Elliott R, Anderson IM, Williams S, Dolan M, Deakin B. Neuronal correlates and serotonergic modulation of behavioural inhibition and reward in healthy and antisocial individuals. J Psychiatr Res. 2010;44:123–131. doi: 10.1016/j.jpsychires.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Widom CS. A methodology for studying noninstitutionalized psychopaths. J Consult Clin Psychol. 1977;45:674–683. [PubMed] [Google Scholar]
- Yang Y, Raine A, Lencz T, Bihrle S, LaCasse L, Colletti P. Volume reduction in prefrontal gray matter in unsuccessful criminal psychopaths. Biol Psychiatry. 2005;57:1103–1108. doi: 10.1016/j.biopsych.2005.01.021. [DOI] [PubMed] [Google Scholar]