Abstract
Objective
To describe the roles community members can and should play in, and an asset-based strategy used by Chicago’s South Side Health and Vitality Studies for, building sustainable, large-scale community health research infrastructure. The Studies are a family of research efforts aiming to produce actionable knowledge to inform health policy, programming, and investments for the region.
Methods
Community and university collaborators, using a consensus-based approach, developed shared theoretical perspectives, guiding principles, and a model for collaboration in 2008, which were used to inform an asset-based operational strategy. Ongoing community engagement and relationship-building support the infrastructure and research activities of the Studies.
Results
Key steps in the asset-based strategy include: 1) continuous community engagement and relationship building, 2) identifying community priorities, 3) identifying community assets, 4) leveraging assets, 5) conducting research, 6) sharing knowledge and 7) informing action. Examples of community member roles, and how these are informed by the Studies’ guiding principles, are provided.
Conclusions
Community and university collaborators, with shared vision and principles, can effectively work together to plan innovative, large-scale community-based research that serves community needs and priorities. Sustainable, effective models are needed to realize NIH’s mandate for meaningful translation of biomedical discovery into improved population health.
Keywords: Asset-based, community, community-based, community-engaged, community role, research infrastructure, urban health, GOURD, collaboratory, inequities, Community maven
INTRODUCTION
Community and university collaborators for Chicago’s South Side Health and Vitality Studies share the vision that the region will become one of the top three healthiest urban communities and a platform for health and health care innovations. Collaborators include clergy, physicians, social workers, business people, nurses, community organizers, civic leaders, social scientists, informaticists, students and dozens of faculty across divisions and schools. The Studies use an asset-based community development strategy (Kretzmann and McKnight, 1997) to build sustainable, large-scale health research infrastructure. The strategy centers research on the community's priorities and assets rather than solely on its needs (Kretzmann and McKnight, 1997; Sharpe et al., 2000), and engages community and university members as equal partners (Israel et al., 1998; Mathie and Cunningham, 2003).
Chicago’s South Side, a 95 square mile are of 34 of the city’s 77 communities, is home to a diverse population of more than 860,000 residents, 71% identifying as African American (US Census Bureau, 2011). The South Side is widely known for its secular and faith-based community organizing legacy, African American civil rights and political leaders, and cultural icons. The South Side's higher educational assets consist of five four-year institutions and three community colleges. Lake Michigan, one of the world’s largest fresh water sources, forms the eastern boundary.
Despite its many assets, the South Side is overburdened by lack of basic resources such as grocery stores (Mari Gallagher Research & Consulting Group, 2006), and chronic social inequities including weak transportation infrastructure (University of Illinois at Chicago, 2005; University of Illinois at Chicago, 2009), violent crime (Chicago Police Department, 2009), poverty, and unemployment (U.S. Census Bureau, 2009), all of which contribute substantially to the population's disproportionately poor health and vitality.
Centrally located, the University of Chicago houses the South Side’s only academic medical center, a top-ranked medical school (Association of American Medical Colleges, 2010), and leading schools of social work, law and business. Chicago’s South Side has served as “the urban laboratory” for many catalytic social scientific discoveries (Bulmer, 1984; Sánchez-Jankowski, 2008; Shils, 1991; Van Overtveldt, 2007). However, this work has largely been “on” and “in” the community, rather than “with” and “for” the community, a type of research that has been described by some as "parachute” research (Bastida et al., 2010). This “South Side story” is familiar to many urban university communities (Mayfield, 2001). The majority of the nation’s 126 academic medical centers are located in communities where the health of the population, typically minority racial or ethnic groups, is poor compared to the institutions’ health expertise (Foreman, 2004).
National and world health organizations are investing in solutions to racial and ethnic health inequities, advocating moral and economic arguments (Institute of Medicine, 2006; World Health Organization, 2001). In 2000, the US Congress passed the Minority Health and Health Disparities Research and Education Act (PL 106-52), forming the National Center on Minority Health and Health Disparities. In 2006, the NIH established the Clinical Translational Science Award (CTSA), a backbone funding mechanism for academic medical research (NCRR, 2010). CTSA funding requires academic medical centers to collaborate with community members on medical issues of highest priority to the community and to generate measurable community benefit (NIH, 2010; CTSA Community Engagement Key Function Committee, 2009).
Influenced in part by these events, the University of Chicago Medical Center began an in-depth review of its relationship with the South Side, its primary service area (Hill and Madara, 2005). In 2002, a community organizing strategy was initiated to build a coordinated system of health care, forming the first-ever collaborative of community health providers for this region (the South Side Healthcare Collaborative) (http://www.uchospitals.edu/programs/community/programs/sshc.html). This effort grew into the Urban Health Initiative (UHI) which advanced as a top priority of the institution and the core community engagement strategy for the university’s successful 2007 CTSA bid. The UHI’s South Side Health and Vitality Studies, housed within the Center for Community Health and Vitality, aim to produce actionable knowledge to inform health, health policy and health investments in the region. This family of studies includes: 1) asset mapping; 2) population health research; and 3) collection of regional data into a multipurpose, widely accessible “collaboratory” for health research. The effort is heavily informed by experiences of other urban health research teams using community-engaged methods (Jones and Wells, 2007; Lantz et al., 2001; Metzler et al., 2003; Moreno et al., 2009; Norris et al., 2007; Seifer, 2006; Shah et al., 2003), but is unique in that it focuses on building large-scale community health research infrastructure, rather than testing a specific disease-focused hypothesis or intervention.
Here, Chicago’s South Side Health and Vitality Studies are presented as a case study of the roles community members can and should play in building sustainable, large-scale community health research infrastructure.
METHODS
Shared theoretical perspectives, guiding principles, our collaboration model and decision-making structure, and the ways these relate to an asset-based operational strategy, provide a customizable framework for community engagement in large-scale health research (Figure 1).
Figure 1. South Side Health and Vitality Studies’ Stages of Building Community-Engaged Health Research Infrastructure.
The four stages of building community-engaged health research infrastructure began with shared theoretical perspectives that emerged through small- and large-group discussion at research meetings and retreats of community and university collaborators. These perspectives translated to practical guiding principles that were articulated and iterated over time with input from and approval of the Studies collaborators. These principles inform a model for community and university engagement that identifies the key roles that collaborators play in the asset-based operating infrastructure for large-scale community health research.
Shared values from community and academic work have emerged through discussion and reflection at large and small working group team meetings and echo those from community organizing (Bishop, 1994), community-based participatory research (Israel et al., 1998; Mathie and Cunningham, 2003), and community research ethics (Ross et al., 2010a; Ross et al., 2010b). These values inform the role community and university members play and are reflected in the Studies’ principles (Figure 2) and engagement model (Figure 3). The Studies’ asset-based strategy integrates these perspectives into an operational infrastructure for accomplishing short- and long-term research goals (Figure 4).
Figure 2. South Side Health and Vitality Studies Guiding Principles and Values.
The Studies’ principles for collaboration and design harmonize with established community organizing and community research values and with additional values that have emerged from the collaborative process.
Figure 3. Model of Community and University Engagement for the South Side Health and Vitality Studies.
The centrality of South Side residents reflects that the South Side Health and Vitality Studies conducts science in service to the community with community members serving in multiple roles. The Center for Community Health and Vitality serves a translational and programmatic role to ensure that new knowledge is used to promote health and vitality by linking community members with university faculty and researchers and by providing technical assistance and training. Developed from discussions among community and university collaborators by Stacy Lindau, MD, MAPP; Deborah Burnet, MD; Dawnavan Davis, PhD; Colleen Grogan, PhD; Daniel Johnson, MD; Waldo Johnson, Jr., PhD; Rick Kittles, PhD; Matthew Stagner, PhD; and Eric Whitaker, MD, MPH for the University of Chicago South Side Health and Vitality Studies. First presented by Whitaker (2009).
Figure 4. Conceptual model of asset based operational infrastructure for the South Side Health and Vitality Studies using an adaptation of Asset-Based Community Development Strategy (Kreztmann and McKnight, 1997).

This conceptual model illustrates an adaptation of asset-based community development strategy for the purpose of large-scale community-engaged health research. Continuous relationship building drives the cycle toward informed action. The impact of informed action is assessed, in part, by the re-evaluation of community priorities. The asset mapping project began with outreach from university faculty and community affairs staff to leaders of strong organizations (human assets) in six pilot communities surrounding the university campus. Community and university members began meeting regularly on campus and jointly identified how asset mapping would serve to advance community health and vitality priorities. Assets on the team were identified through individual contributions at and between meetings. Assets in the community were mapped by teams of university students and community members who gave input on the mapping protocols and feedback on field experiences. This information was integrated to field research procedures and ongoing community engagement activities. New knowledge about community assets was shared at standing meetings of the Studies, via media coverage, on the internet, and at a large retreat where community and university members worked with the data in small, facilitated teams to generate use cases, feedback, and reassessment of priorities. At the retreat, collaborators indicated a desire for expanding the mapping to include service information. The team jointly prepared a foundation grant, submitted by the university PI, that is now supporting service mapping activities.
I. Identify Shared Theoretical Perspectives
Community organizing values, including social networking, leadership development, and empowerment (Bishop, 1994), are reflected in the Studies’ multi-faceted approach to engaging diverse collaborators in health research planning, participation, and knowledge dissemination. Institutional and external funding have been used to hire full-time community engagement professionals who recruit and retain community collaborators, proactively engage key leaders, and monitor the Studies’ fidelity to its engagement principles. In addition, the Studies use a social networking protocol, designed by community organizers, to generate uptake and use of data. Implementation involves “community mavens” (respected community experts with a desire to share knowledge), armed with training, netbooks, and transportation to collect community data and to help generate community engagement in the Studies’ activities.
Many community-based participatory research (CBPR) values overlap with those from community organizing (NCMHD, 2010). CBPR defines ways community members should be involved in health research, including: 1) prioritizing community needs, health issues, and assets, 2) cooperative development of research and research ethics infrastructure, including participation and co-learning for mutual benefit, and 3) using data to inform and engage community members (Israel et al., 1998; Mathie and Cunningham, 2003). Although the Studies are a joint community and university effort (an important characteristic of CBPR), the impetus, scientific operations and seed funding originated and continue to be heavily operated from the university (Figure 5). In recognition of this, we describe our approach as “community engaged research,” similar to Wells and Jones’ description of “community partnered research” (Wells and Jones, 2009).
Figure 5. Evolution of Roles, Operations, and Decision-Making Structure of the South Side Health and Vitality Studies.
This timeline illustrates key milestones and activities for the engagement between university and community collaborators for the Studies as well as the development of diverse funding sources over the course of the Studies to date.
II. Articulating Guiding Principles for Community-University Engagement
The principles guide strategic decision-making, operations, and collaborator interactions and fall into two categories: 1) community and university engagement, and 2) study design. The principles integrate the overlapping values of community organizing, CBPR and research ethics (Figure 2). Our group articulated additional values, including continuous learning, sustainability, and innovation. The principles evolved from twelve substantive revisions based on consensus-driven group deliberations (Israel et al., 2001) over the first year, are regularly revisited, and are expected to iterate as the Studies grow.
The organizational and decision-making structure continues to evolve as the project matures. The Studies currently use a consensus-based decision model (Israel et al., 2001) based on the Studies’ principles. The principal investigator, in our case a university faculty member, is ultimately responsible for decisions, with guidance from a senior advisory panel including the directors of the UHI and the Center for Community Health and Vitality (Figure 6). It is important to note that the principal investigator of community-engaged or other health research pursuits does not have to be a university faculty member. In fact, the National Institutes of Health and other important health research funders have policies and funding mechanisms that allow for leadership sharing across institutions (NIH, 2009a) and/or that promote collaborative leadership between academic entities and community-based organizations (NCMHD, 2010; NIH, 2006; NIH, 2009b) ) . The lead or principal investigator for a research protocol should possess the skills, resources, and credibility necessary to execute ultimate oversight of and responsibility for the project (NIH, 2009a).
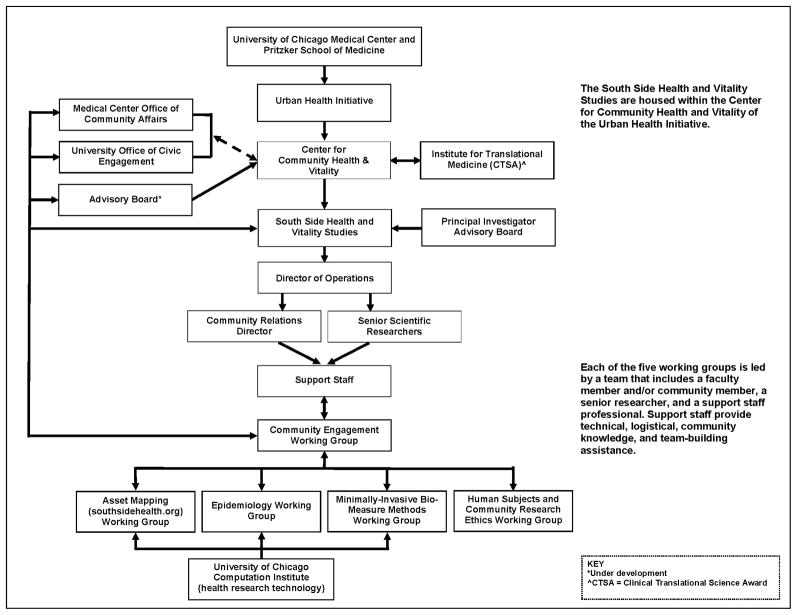
Figure 6. South Side Health and Vitality Studies Organizational Chart.
This illustrates the interactions between university entities, faculty, community, and professional community engagement and research staff. While the organizational chart appears hierarchical, the structure operates as a team, with decisions relying heavily on consensus.
III. Creating a Model of Community-University Engagement
The Studies’ collaborative research model places community residents at the center, signifying “science in service to community,” (as opposed to science for the sake of knowledge, alone) and identifies the roles of community members and other stakeholders (Figure 3). For example, the Studies’ asset mapping project involves community members as research collaborators, paid consultants and data collectors, students, and study participants. Data are shared online within weeks of collection. Users include community members, university researchers, business people, and policy makers, who provide feedback via the internet, mavens, and at collaborator meetings.
IV. Developing an Operating Infrastructure using Asset-Based Community Development
The Studies’ asset-based approach for health research harmonizes with the Asset-Based Community Development (ABCD) method used by community organizers for urban development (Kretzmann and McKnight, 1997). Figure 4 illustrates the adaptation of ABCD to the Studies’ operational design, a cyclical, relationship-driven process fueled by the community's priorities and problem-solving capacity. A relationship-driven process includes continuous investment in building and rebuilding relationships to inform actions that benefit the community’s health and vitality. Once positive action is taken, success is partly evaluated by reassessing community priorities and the quality of community engagement.
RESULTS AND DISCUSSION
This section describes key infrastructure-building activities using the ABCD operational steps (Kretzmann and McKnight, 1997) (Figure 4), emphasizing the role of community members (Figure 3) and linking these activities to our guiding principles (Figure 2).
Step 1. Continuous Engagement and Relationship-Building
Community engagement is an ongoing process of relationship building, essential to every operational step and overall sustainability. First, faculty reached out to the medical center’s community and government affairs offices, the university’s civic engagement leaders, local elected officials and faith leaders, and established channels of ongoing, bilateral communication (Figure 5). Consistent with the guiding principles, the team recruits collaborators to maximize diversity of geographic involvement (with a goal of 34 community representation) and of substantive expertise in priority areas such as nutrition, prevention, cancer, and oral health.
In addition to inviting community leaders identified through social networks and elected officials, the Studies' meetings are public and widely publicized via community engagement professionals working with the Studies. Standing meetings are planned months in advance at alternating times to maximize participation. We publish a widely circulated monthly email newsletter, share information via a website (http://www.sshvs.org), and host blog (http://southsidehealth.wordpress.com) and Twitter accounts (http://www.twitter.com/sshvs) with contributions from community and university collaborators.
To expand community engagement and build trust, grant applications aim to maximize parity in funding for community components. The direct cost budget ratio is roughly $2.5:1 (university:community) for currently funded projects. We financially support local organizations and businesses by renting community space and contracting for catering, parking, technical support and other needs. This builds good will, exposes collaborators to the breadth of South Side assets and increases community leaders’ awareness about the Studies.
Step 2. Identifying Community Priorities
The Studies’ organizational structure includes an operations team that supports working groups composed of community and university collaborators (Figure 6). These groups and their members formed in response to community priorities and in areas of faculty strength. Priorities have been articulated as substantive health topics (eg, reduced obesity, cancer prevention, public safety, dental care, mental health) and as deliverables (eg, quality health care, useable data to win grants and contracts, workforce development) and iterate over time.
Step 3. Identifying Community Assets
Building on community assets and university strengths in health research, computation, and informatics, the Studies invested in developing a scaleable protocol for mapping built and service assets (Aronson et al., 2007; Kretzmann and McKnight, 1997; Minkler and Hancock, 2003; Sharpe et al., 2000). This project was prioritized because it aligned operationally with the asset-based approach, created jobs and training opportunities, and provided an immediate, tangible and useful deliverable to the community. Furthermore, asset mapping allowed the team to build trust and shared value for community health data without involvement of human research subjects.
An asset-mapping working group was formed, including leaders from six communities (five predominantly African American and contiguous to the university, and one largely Hispanic community). Team members met and established ongoing ties with aldermanic offices to discuss the project's purpose and the potential value of the data. A community education campaign distributed paper fliers, emails to more than 1000 community contacts, and a press release that earned positive media coverage (Lee, 2009).
Field teams of community and university students mapped more than 2200 non-residential built establishments (eg clinics, churches, grocery stores) with overwhelmingly positive community interactions. Within weeks, data were available on www.SouthSideHealth.org. At a community-based retreat, more than one hundred community and university members worked in small groups to test the website, generate use cases, and prioritize next steps. Community members suggested expanding mapping to include service assets (eg health care, child care, handicap accessibility); these ideas were translated into new proposals for funding. The Studies have since been awarded local, federal and corporate funding to support service mapping and expansion of mapping into additional communities.
Step 4. Leveraging Assets
Once assets are identified, leveraging occurs by optimizing shared benefit through knowledge gained via community engagement and relationship-building. For example, leaders from one community organization inquired about jointly funding asset mapping in their community. They brought data management expertise and a supervised group of high school students hired via a public grant. We contributed our mapping protocol, field training, equipment (eg, PDAs), and informatics expertise. Through this partnership, students gained meaningful work experience, the community gathered data integral to advancing its work, and the Studies developed a use case for its asset mapping protocol, expanded its public database and sustained its training principle.
Step 5. Conducting Research
The Studies’ collaborative model illustrates the roles of community members in the Studies' research. We are raising funds to initiate a population-based study of health that will follow individuals over time to understand social determinants of health at a community level (Brunner and Marmot, 1999; Robert Wood Johnson Foundation, 2008). Five working groups (Figure 6) support this effort: 1) epidemiology, 2) community engagement, 3) health research technology, 4) minimally invasive biological measure methods, and 5) human subjects and community research ethics.
The human subjects and ethics working group plays a key role in relationship-building, trust and creation of shared ownership. This group provides ethics training to community members (Collaborative Institutional Training Initiative, 2010) and is translating community research ethics literature (Ross et al., 2010a; Ross et al., 2010b) into a human subjects protocol reflecting the values of the community. Key considerations beyond individual human subject protections include group consent, group risk and benefit, and maximizing public data access while minimizing threats to autonomy and confidentiality.
Step 6. Sharing Knowledge: Giving GOURDs
Inspired by the principle of sharing data that can benefit community, we created a practice of “GOURDs”: Gifts of Useable Research Data. GOURDs are shared by collaborators with new potential partners and are tailored to the data interests of the organization. Examples include: 1) asset maps of retail food outlets, shared with a company interested in improving nutrition, 2) technology use data shared with the City of Chicago Department of Innovation and Technology, and 3) data showing the absence of well-child care sites, shared with an organization promoting children's health. GOURDs engage new partners by enhancing the relevance of the Studies to their priorities while disseminating knowledge and building trust.
Step 7. Informed Action
The ABCD model requires that the Studies inform actions to promote health and vitality in our community. The Center for Community Health and Vitality (Figure 3), physically located in the community, uses the Studies’ data to inform programmatic investments. These investments respond to community priorities by creating: 1) linkages to best practices (eg “community grand rounds” engage university experts in a community-driven format to share knowledge on priority health topics), 2) community member access to health data and data support, and 3) training, health workforce development, and entrepreneurship opportunities.
CONCLUSION
Community and university collaborators working with shared vision and institutional support can engage to build mutually beneficial community-based health research infrastructure. Sustainable, effective models for large-scale, community-engaged health research may aid translation of biomedical discoveries into improved population health (Roussos and Fawcett, 2000; Woolf, 2008). Simultaneously, a solid, agile community engagement infrastructure presents health research and development opportunities that can benefit the community, the academic medical center and the broader public (Ahmed and Palermo, 2010; Flicker, 2008; Viswanathan et al., 2004). Empirical data are needed to determine the impact of CBPR-type approaches on effective translation of large-scale health research and the remediation of health inequities (Cook, 2008; Wallerstein and Duran, 2010).
Acknowledgments
The authors acknowledge the creativity and contributions of the dozens of community and university collaborators for the Studies, including key university contributors Colleen Grogan, PhD, Diane Lauderdale, PhD, Martha Van Haitsma, PhD with colleagues at the University of Chicago Survey Lab, Jonathan C. Silverstein, MD with colleagues at the Computation Institute, Stephen Brown, MSW with the Urban Health Initiative, Todd Schuble, MS in Social Science Computing of the Social Science Division of the University of Chicago, and Leif Elsmo, Executive Director of Community and External Affairs at the University of Chicago Medical Center. Community and university members of the following working groups for the South Side Health and Vitality Studies’ have reviewed and approved this manuscript, including the working groups on Community Engagement, Research Ethics and Human Subjects, and Resource Mapping. Todd Schuble and Shane Desautels are paid consultants of the South Side Health and Vitality Studies. No compensation was provided for others involved in the writing or review of this manuscript, beyond the terms of their employment. The authors would like to acknowledge research assistance and help with preparation of the manuscript for submission from Emily Abramsohn, Matthew Dias, Karen Lee, Jason Liu, Andreea Mihai, and George R. Smith, Jr. The authors are grateful for the assistance of these individuals who are paid employees of Dr. Lindau and the South Side Health and Vitality Studies. The South Side Health and Vitality Studies receive funding from the Urban Health Initiative of the University of Chicago Medical Center, the Chicago Community Trust, the National Institutes of Health ARRA 1RC4AG038176-01 the Walter G. Zoller Memorial Fund at the University of Chicago, the George Kaiser Family Foundation, the Otho S. A. Sprague Memorial Institute, PepsiCo, and individual philanthropists, Dr. Patrick Soon-Shiong, Ellen H. Block, and Patricia O. Cox. Dr. Lindau is currently supported by a research career development award from the National Institutes of Health (1K23AG032870).
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmed SM, Palermo AG. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010;100:1380–7. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronson RE, et al. Neighborhood mapping and evaluation: a methodology for participatory community health initiatives. Matern Child Health J. 2007;11:373–83. doi: 10.1007/s10995-007-0184-5. [DOI] [PubMed] [Google Scholar]
- Association of American Medical Colleges. Medical School Missions Management Tool 2010. Revised version prepared for the use of University of Chicago Division of the Biological Sciences and the Pritzker School of Medicine; 2010. [DOI] [PubMed] [Google Scholar]
- Bastida E, et al. Ethics and community-based participatory research: perspectives from the field. Health Promot Pract. 2010;11:16–20. doi: 10.1177/1524839909352841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop R. Initiating Empowering Research. New Zealand Journal of Educational Studies. 1994;29:175–188. [Google Scholar]
- Brunner E, Marmot M. Social Organization, Stress, and Health. In: Marmot M, Wilkinson RG, editors. Social Determinants of Health. Oxford University Press; Oxford: 1999. pp. 17–43. [Google Scholar]
- Bulmer M. The Chicago School of Sociology: Institutionalization, Diversity, and the Rise of Sociological Research. University of Chicago Press; Chicago: 1984. [Google Scholar]
- Chicago Police Department. CLEARMAP Crime Summary. Retrieved November 5, 2010 from http://gis.chicagopolice.org/CLEARMap_crime_sums/startPage.htm#.
- Clinical and Translational Science Awards (CTSA) Community Engagement Key Function Committee. Researchers and Their Communities: The Challenge of Meaningful Community Engagement. 2009 Retrieved November 5, 2010 from http://www.ctsaweb.org/index.cfm?fuseaction=committee.viewCommittee&com_ID=3&abbr=CEKFC.
- Collaborative Institutional Training Initiative (CITI) Retrieved November 5, 2010 from https://www.citiprogram.org/Default.asp?
- Cook WK. Integrating research and action: a systematic review of community-based participatory research to address health disparities in environmental and occupational health in the USA. J Epidemiol Community Health. 2008;62:668–76. doi: 10.1136/jech.2007.067645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flicker S. Who benefits from community-based participatory research? A case study of the Positive Youth Project. Health Educ Behav. 2008;35:70–86. doi: 10.1177/1090198105285927. [DOI] [PubMed] [Google Scholar]
- Foreman SMD. Montefiore Medical Center in the Bronx, New York: Improving Health in an Urban Community. Acad Med. 2004;79:1154–1161. doi: 10.1097/00001888-200412000-00007. [DOI] [PubMed] [Google Scholar]
- Hill LD, Madara JL. Role of the urban academic medical center in US health care. JAMA. 2005;294:2219–20. doi: 10.1001/jama.294.17.2219. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Examining the health disparities research plan of the National Institutes of Health: unfinished business. 2006 Retrieved June 1, 2010 from http://iom.edu/Reports/2006/Examining-the-Health-Disparities-Research-Plan-of-the-National-Institutes-of-Health-Unfinished-Business.aspx. [PubMed]
- Israel BA, et al. The Detroit Community-Academic Urban Research Center: development, implementation, and evaluation. J Public Health Manag Pract. 2001;7:1–19. doi: 10.1097/00124784-200107050-00003. [DOI] [PubMed] [Google Scholar]
- Israel BA, et al. Review of Community-Based Research: Assessing Partnership Approaches to Improve Public Health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. Jama. 2007;297:407–10. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- Kretzmann JP, McKnight JL. Building Communities from the Inside Out: A Path Toward Finding and Mobilizing a Community's Assets. ACTA Publications; Illinois: 1997. [Google Scholar]
- Lantz PM, et al. Can communities and academia work together on public health research? Evaluation results from a community-based participatory research partnership in Detroit. J Urban Health. 2001;78:495–507. doi: 10.1093/jurban/78.3.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee W. Chicago South Side mapping project shows neighbors live worlds apart. Chicago Tribune; Chicago, IL: Jul 22, 2009. [Google Scholar]
- Mari Gallagher Research & Consulting Group. Examining the impact of food deserts on public health in Chicago. 2006 Retrieved November 5, 2010 from http://www.marigallagher.com/site_media/dynamic/project_files/1_ChicagoFoodDesertReport-Full_.pdf.
- Mathie A, Cunningham G. From Clients to Citizens: Asset-Based Community Development as a Strategy for Community-Driven Development. Development in Practice. 2003;13:474–486. [Google Scholar]
- Mayfield L. Town and gown in America: some historical and institutional issues of the engaged university. Education for Health. 2001;14:231–240. doi: 10.1080/13576280110056609. [DOI] [PubMed] [Google Scholar]
- Metzler MM, et al. Addressing urban health in Detroit, New York City, and Seattle through community-based participatory research partnerships. Am J Public Health. 2003;93:803–11. doi: 10.2105/ajph.93.5.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Hancock T. Community-Driven Asset Identification and Issue Selection. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. Jossey-Bass Publishers; San Francisco: 2003. pp. 135–154. [Google Scholar]
- Moreno G, et al. Eight years of building community partnerships and trust: the UCLA family medicine community-based participatory research experience. Acad Med. 2009;84:1426–33. doi: 10.1097/ACM.0b013e3181b6c16a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Research Resources (NCRR) Clinical and Translational Science Awards. 2010 Retrieved June 10, 2010, from http://www.ncrr.nih.gov/clinical_research_resources/clinical_and_translational_science_awards/
- National Center on Minority Health and Health Disparities (NCMHD) NCMHD community based participatory research initiative. 2010 Retrieved June 11, 2010, from http://www.ncmhd.nih.gov/our_programs/communityParticipationResearch.asp.
- National Institutes of Health (NIH) RFA-07-004, Community-based participatory research at NIMH. 2006 Retrieved December 30, 2010 from http://grants.nih.gov/grants/guide/pa-files/PAR-07-004.html.
- National Institutes of Health (NIH) Multiple principle investigators. 2009a Retrieved December 30, 2010, from http://grants.nih.gov/grants/multi_pi/
- National Institutes of Health (NIH) PAR-09-092, Academic-community partnership series. 2009b Retrieved December 30, 2010, from http://grants.nih.gov/grants/guide/pa-files/par-09-092.html.
- National Institutes of Health (NIH) RFA-RM-10-020, Institutional Clinical Translational Science Award. 2010 Retrieved December 30, 2010 from http://grants.nih.gov/grants/guide/rfa-files/RFA-RM-10-020.html.
- Norris KC, et al. Partnering with community-based organizations: an academic institution's evolving perspective. Ethn Dis. 2007;17:S27–32. [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation. Overcoming obstacles to health, Report from the Robert Wood Johnson Foundation to the Commission to Build a Healthier America. Robert Wood Johnson Foundation; Princeton, NJ: 2008. Retrieved November 5, 2010 from http://www.commissiononhealth.org/PDF/ObstaclesToHealth-Report.pdf. [Google Scholar]
- Ross LF, et al. Human subjects protections in community-engaged research: a research ethics framework. J Empir Res Hum Res Ethics. 2010a;5:5–17. doi: 10.1525/jer.2010.5.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LF, et al. Nine key functions for a human subjects protection program for community-engaged research: points to consider. J Empir Res Hum Res Ethics. 2010b;5:33–47. doi: 10.1525/jer.2010.5.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health. 2000;21:369–402. doi: 10.1146/annurev.publhealth.21.1.369. [DOI] [PubMed] [Google Scholar]
- Sánchez-Jankowski M. Cracks in the pavement: social change and resilience in poor neighborhoods. University of California Press; Berkeley, CA: 2008. [Google Scholar]
- Seifer SD. Building and sustaining community-institutional partnerships for prevention research: findings from a national collaborative. J Urban Health. 2006;83:989–1003. doi: 10.1007/s11524-006-9113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah AM, et al. A Participatory Approach to Designing a Community Health Survey: A Report on the Survey Development Process. 2003 Retrieved November 5, 2010 from http://www.policyarchive.org/handle/10207/bitstreams/21749.pdf.
- Sharpe PA, et al. Assets-oriented community assessment. Public Health Rep. 2000;115:205–11. doi: 10.1093/phr/115.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shils E. Remembering the University of Chicago: Teachers, Scientists, and Scholars. University of Chicago Press; Chicago: 1991. [Google Scholar]
- University of Illinois at Chicago. The case for transit-oriented development in the Greater Roseland Area. 2005 Retrieved November 5, 2010 from http://www.uic.edu/cuppa/voorheesctr/Publications/DCP%20TOD%202005%20REPORT.pdf.
- University of Illinois at Chicago. Transit equity matters: an equity index and regional analysis of the Red line and two other proposed CTA transit extensions. 2009 Retrieved November 5, 2010 from http://www.uic.edu/cuppa/voorheesctr/Publications/Transit%20Equity%20Matters%2012.09.pdf.
- US Census Bureau. 2005-2009 American Community Survey 5-Year Estimates. 2011 Retrieved January, 3 2011 from www.http://www.census.gov/acs/www/
- U.S. Census Bureau. 2006–2008 American Community Survey 3-Year Estimates [Online Data Set] Washington, DC: U.S. Government Printing Office; 2009. [Google Scholar]
- Van Overtveldt J. The Chicago School: How the University of Chicago Assembled the Thinkers Who Revolutionized Economics and Business. Agate B2; Chicago: 2007. [Google Scholar]
- Viswanathan M, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess. 2004 Summ;:1–8. [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl 1):S40–6. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Jones L. "Research" in community-partnered, participatory research. JAMA. 2009;302:320–1. doi: 10.1001/jama.2009.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker E. Laying the Groundwork for Community and University Engagement; Presented orally at Improving Health with Communities: The Role of Community Engagement in Clinical and Translational Research; Bethesda, MD. 2009. [Google Scholar]
- Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299:211–3. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- World Health Organization. World Conference Against Racism, Racial Discrimination, Xenophobia and Related Intolerance: Health and Freedom from Discrimination. 2001 Retrieved June 19, 2010 from http://www.who.int/hhr/activities/q_and_a/en/Health_and_Freedom_from_Discrimination_English_699KB.pdf.