Abstract
Objective
Many individuals entering treatment are involved in social networks and activities that heighten relapse risk. Consequently, treatment programs facilitate engagement in social recovery resources, such as Alcoholics Anonymous (AA), to provide a low risk network. While it is assumed that AA works partially through this social mechanism, research has been limited in rigor and scope. This study used lagged mediational methods to examine changes in pro-abstinent and pro-drinking network ties and activities.
Method
Adults (N = 1,726) participating in a randomized controlled trial of alcohol use disorder treatment were assessed at intake, and 3, 9, and 15 months. Generalized linear modeling (GLM) tested whether changes in pro-abstinent and pro-drinking network ties and drinking and abstinent activities helped explain AA's effects.
Results
Greater AA attendance facilitated substantial decreases in pro-drinking social ties and significant, but less substantial increases in pro-abstinent ties. Also, AA attendance reduced engagement in drinking-related activities and increased engagement in abstinent activities. Lagged mediational analyses revealed that it was through reductions in pro-drinking network ties and, to a lesser degree, increases in pro-abstinent ties that AA exerted its salutary effect on abstinence, and to a lesser extent, on drinking intensity.
Conclusions
AA appears to facilitate recovery by mobilizing adaptive changes in the social networks of individuals exhibiting a broad range of impairment. Specifically by reducing involvement with pro-drinking ties and increasing involvement with pro-abstinent ties. These changes may aid recovery by decreasing exposure to alcohol-related cues thereby reducing craving, while simultaneously increasing rewarding social relationships.
Keywords: Alcoholics Anonymous, social networks, self help groups, alcoholism, alcohol dependence
1. Introduction
Prominent theories and research highlight the importance of social processes and social network characteristics as potent correlates of alcohol use and the relapse-recovery process (Bandura, 1997; Beattie and Longabaugh, 1999; Fals-Stewart et al., 2003; Groh et al., 2008; Laudet et al., 2002; Marlatt and Gordon, 1985; McCrady, 2004: Moos, 2007; Rosenquist et al, 2010; Witbrodt and Kaskutas, 2005). From a treatment perspective, assessing what patients do and with whom, are critical variables to consider in relapse prevention planning. Treatment programs typically work with patients to help them identify and cope with high risk individuals, settings, and activities that may undermine recovery efforts. Programs also make targeted referrals to socially-based continuing care resources in the community, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) (Humphreys, 1997; Laudet and White, 2005; Fenster, 2006; Kelly and Yeterian, 2008) to enhance protective influences post discharge. Such organizations can provide access to dense social networks comprised of abstinent role models that encourage sober and rewarding activities (Alcoholics Anonymous, 1957; Litt et al, 2009; Moos, 2007).
Evidence from a large number of studies reveals that AA and NA participation is strongly associated with abstinence and recovery (Kaskutas, 2009; Emrick et al., 1993; Humphreys, 2004;Timko et al, 2000), may potentiate and extend the benefits of SUD treatment (Emrick et al, 1993; Fiorentine and Hillhouse, 2000; Kelly and Yeterian, 2008; Kelly et al., 2010; Moos and Moos, 2004), and may help reduce health care costs while producing better recovery rates (Humphreys and Moos, 2001; 2007; Humphreys et al, 1996). One of the mechanisms through which AA may confer these recovery-related benefits is by mobilizing adaptive social network changes that, in turn, support sober activities. Changes in what one does, and with whom, could reduce exposure to alcohol-related cues, thereby reducing cue-induced craving and relapse risk (Fox et al., 2007).
The influence of social networks on a variety of health behaviors, including alcohol use, has become a central focus in recent years (Galea et al., 2004; Rosenquist et al., 2010; Valente, 2010) and emerging research on the mechanisms of AA's effects points to a role for social processes. For example, Humphreys et al. (1999) found 12-month cognitive and behavioral coping, friendship quality, and network support for abstinence partially mediated the relationship between 12-step involvement following inpatient treatment and 12-month outcomes. Social support in the first 12 months of mutual-help involvement has also been shown to mediate the relationship between affiliation and substance use two years later among individuals with co-occurring substance and mental disorders (Laudet et al., 2004). Research has supported the role of social networks, particularly AA-related support, in long-term recovery. In a mixed sample of inpatients and outpatients, Kaskutas et al. (2002) found that social network influences were mediators of 12-month abstinence. Specifically, a larger social network and greater network support for abstinence partially explained the relationship between greater AA involvement and better outcomes. In tests of individual predictors, reducing pro-drinking influences and increasing AA-related support for abstinence were most important (Kastukas et al., 2002). However, in a subsequent analysis, only AA-specific network support mediated alcohol abstinence three years after treatment (Bond et al., 2003).
Due to the prognostic implications of patients’ social network ties and activities, different professionally-led treatments have been compared regarding their ability to effectively counteract this social relapse risk. A recent randomized study with alcohol dependent outpatients conducted by Litt et al. (2009) attempted to increase social network support for abstinence by systematically encouraging patients to make use of the social aspects of AA. Using the Important People and Activities (IPA) instrument (Clifford and Longabaugh, 1991) to measure abstinent network members and their behavioral and attitudinal support for drinking or abstinence, the investigators compared this social Network Support (NS) intervention to two separate active comparison treatments. Results revealed that those in the 12-step oriented NS condition gained 20% more days abstinent as well as greater AA attendance and involvement at 2-year follow-up. Furthermore, AA participation and the number of abstinent friends in the NS condition were found to partially mediate this effect (Litt et al, 2009).
In Project MATCH (Project MATCH Research Group, 1993), patients that had heavy drinking social networks at the start of treatment who were randomly assigned to a treatment designed to facilitate AA participation (i.e., Twelve-Step Facilitation [TSF]) had better long-term outcomes after three years than patients assigned to either a cognitive behavioral or motivational intervention. This treatment matching effect was partially mediated by AA attendance during the 3-year follow-up period (Longabaugh et al, 1998, 2001). This matching effect was not observed at the 1-year follow-up on measures of alcohol use. However, a further analysis of Project MATCH data examined this same attribute by treatment interaction matching effect but on 1-year post-treatment alcohol-related consequences using growth mixture modeling. Results from this analysis once again revealed greater benefit for outpatients assigned to TSF, but in this case at 1 year post-treatment (Wu and Witkiewitz, 2008).
Of note was that Project MATCH patients electing to attend AA, irrespective of which treatment they initially received, had significantly better outcomes overall (Tonigan et al, 2003). How AA attendance led to these improvements has become a focus of investigation (e.g., Kelly et al, 2010a; Kelly et al, 2010b; Tonigan et al, 2002), but whether AA's association with better outcomes found in MATCH can be explained by AA's ability to mobilize social process changes has yet to be examined. In the present study, we make use of the large, multisite, sample collected in Project MATCH and employ a prospective design to examine the extent to which AA independently influences four social recovery processes: reductions in high risk social network ties; increases in low risk social network ties; reductions in drinking-related activities; and increases in abstinence-related activities. We conduct lagged meditational tests that yield estimates of the proportion of the direct effect of AA on drinking outcomes that is accounted for by each of these four purported mechanisms. We hypothesize that more frequent AA attendance will be associated with more abstinence and less intense alcohol use. Also, greater AA attendance will be associated with decreased involvement with high-risk social network ties (i.e., those individuals that condone or support alcohol use), increased involvement with low risk social network ties (i.e., individuals supportive of abstinence), increased engagement in abstinent-related activities, and decreased engagement in drinking-related activities. We also investigate whether AA's ability to adaptively influence these social network variables depends on the starting (study intake) level of that variable (e.g., does AA's ability to effectively reduce pro-drinking influences depend on the extent of those pro-drinking influences at study intake). Finally, we predict that recovery-supportive changes among these four social processes will be associated with positive outcomes, and that the effect of AA on subsequent alcohol use, will be partially mediated by these processes.
2. Method
2.1. Subjects
This study utilizes the Project MATCH outpatient (n = 952; 72% male) and aftercare (n = 774; 80% male) samples followed through 15 months. Inclusion criteria were current and primary DSM-III-R diagnosis of alcohol abuse or dependence, a minimum age of 18, and a minimum sixth grade reading level. Section 3.1 below provides further details.
2.2. Procedures
Subjects were randomly assigned to one of three individually-delivered, psychosocial interventions: Cognitive Behavioral Therapy (CBT; Kadden et al., 1992), Motivational Enhancement Therapy (MET; Miller et al., 1992), and Twelve-Step Facilitation Therapy (TSF; Nowinski et al., 1995). TSF and CBT were delivered in 12 weekly sessions; MET sessions were delivered only at weeks 1, 2, 6 and 12. Participants were reassessed at 3, 6, 9, 12 and 15 months following treatment, and follow-up rates remained over 90%. More complete details can be found in Project MATCH Research Group (1997).
2.3. Alcohol and AA measures
2.3.1. Alcohol use
Alcohol consumption was assessed using the Form 90 (Miller and Del Boca, 1994), which combines an interview procedure with calendar-based and drinking pattern estimations. The Form 90 also collects data on drug use, treatment, incarceration, and AA involvement in the past 90 days.
2.3.2. Alcoholics Anonymous attendance
AA attendance was assessed using the Form 90, which captured the number of AA meetings attended during the past 90 days at intake and 3, 6, 9, 12, and 15 months. The proportion days attending AA was created by dividing the number of days attended by the total number of days in the period.
2.4. Social Network Support and Activity measures
These constructs were assessed using the Important People and Activities (IPA) Instrument (Clifford and Longabaugh, 1991). This measure captures the drinking status and influence of the most important people in patients’ networks along multiple dimensions including patients’ social activities.
The IPA collects detailed data on four “important” people in an open item stating: “please name the four people most important to you in the past 6 months”. For these four people, patients were asked how each reacted to their abstinence or drinking. The response options were the same for each: 1 = left, or made you leave when you were not drinking/drinking, 2 = didn't accept, 3 = neutral, 4 = accepted, 5 = encouraged, 8 = person did not know about not drinking/drinking, and 9 = not applicable. A person was recorded as allowing/encouraging abstinence/drinking if they endorsed either code 4 or code 5. They were recorded as “discouraging” abstinence/drinking if they endorsed either code 1 or code 2. In preliminary analyses, we found that there was a strong correlation between encouraging abstinence and discouraging drinking, and vice versa. On this basis, we combined these into a paired items, pro-abstinence and pro-drinking. A person was coded as “pro-abstinence” if s/he either encouraged abstinence or discouraged drinking, or both. A person was coded as “pro-drinking” if s/he either encouraged drinking or discouraged abstinence, or both. The number of each type of network members was summed to produce a scale range 0-4. Someone could list four people all neutral about drinking, in which case they would get a count of 0 for both measures.
Respondents were asked to list activities during the past 6 months “which you spend a lot of time doing, or activities you did, perhaps spending less time, but which were important to you and the way you lived.” For each activity, participants were asked how often others drank during the activity. Participants were allowed to list only the four most important activities. The items had the following response options: 0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = usually, and 5 = always. From these data we counted “abstinent activities” as those where others drank never or rarely (codes 0 and 1, both items having to be non-missing). Something was counted as “drinking activities” if others drank often to always (codes 3-5). The number of each type of activity was summed to produce a scale 0-4.
2.5. Statistical methods
2.5.1. Data preparation and descriptive analyses
The dependent variables (percent days abstinent [PDA], drinks per drinking day [DDD]) and the independent AA attendance variable were transformed prior to analyses (PDA/arcsine transformed; DDD/square root transformed, and AA attendance/log transformed; Tabachnick and Fidell, 2001). Due to the number of tests conducted and the large sample sizes, the threshold for statistical significance was set at .01 for the main legs of the mediational analyses, as a partial Bonferroni correction.
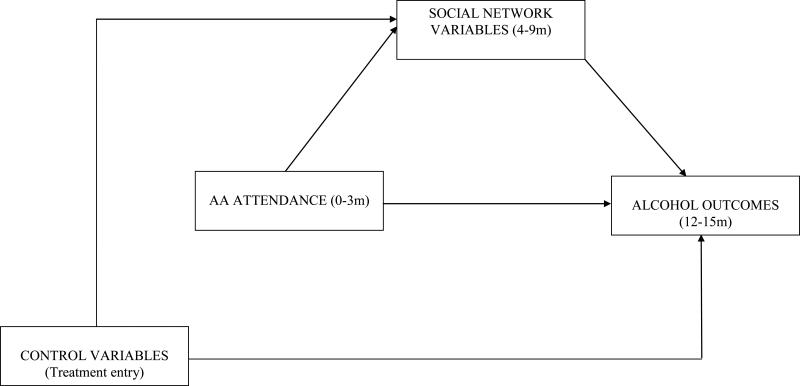
2.5.2. Lagged, controlled mediation analyses
To examine the relationship between AA attendance, the four network variables (i.e., pro-abstinence, pro-drinking, abstinent activities, drinking activities), and alcohol use, we used a general linear model (GLM) controlling for baseline covariates. We ran these models separately for the aftercare and outpatient samples and for each alcohol use outcome variable (PDA, DDD) to examine: (1) the independent (AA attendance) to dependent variable path, (2) the independent to mediator (network support/activities) path, and (3) the mediator to dependent variable path. To make the tests prospective (lagged), we used time points in which predictors were used for outcomes (i.e., AA attendance past 90 days at month 3 to predict network support/activities at month 9 [past 6 months] and alcohol use at month 15 [past 90 days]; similarly, we used network support/activities at month 9 to predict drinking at month 15 [past 90 days]). The static covariates were age, ethnicity, gender, marital status, employment status, number of prior alcohol-related treatments, treatment assignment, treatment site, the relevant baseline level of the dependent variable (i.e., network support/activities, PDA, DDD). Figure 1 shows this model.
Figure 1.
Lagged Mediational Model.
2.5.3. Missing data
To address missing data, we used multiple imputation (Little and Rubin, 2002). Missing data for key variables ranged from 0.05% for baseline AA attendance to 7.8% for drinking at months 13-15. Since missing data patterns were non-monotone (i.e., many were intermittently missing), the Markov Chain Monte Carlo (MCMC) method for multiple imputation was used (Gilks et al., 1996). We performed ten imputations using MI and MIANALYZE in SAS 9.2, and reported statistics are averaged across imputations (Barnard and Rubin, 1999).
2.5.4. Tests of statistical mediation
Mediation analyses were conducted using methods described by MacKinnon and colleagues (MacKinnon and Dwyer, 1993; MacKinnon et al., 2002). The method tests directly for the existence of a significant path from the independent variable (A) through the mediator (B) to the outcome (C) by computing a product of the standardized regression coefficients for the A-B and B-C associations. The Z score can then be compared to critical significance levels developed by MacKinnon. This joint significance test has been shown to produce optimal power and the most accurate Type I error rates in all cases compared to other methods, including the Sobell t-test of for mediation (see MacKinnon et al., 2002).
3. Results
3.1. Sample descriptive data
Participants were 1,726 alcohol dependent patients comprised of 774 patients recruited following a residential treatment (aftercare sample) and 952 patients recruited without prior residential treatment (outpatient sample). Patients were on average 40 years old, 20.5% female, 34.8% married and 49.3% employed full-time. Of the aftercare patients, 80.5% were White, 14.8% were Hispanic, 3.5% were black and 1.2% were of another ethnicity. Of the outpatients, 79.8% were white, 5.6% were Hispanic, 12.3% were black and 2.2% were of another ethnicity. Overall, outpatients were significantly younger, more residentially stable, and less dependent on alcohol than the aftercare patients (Goodman et al., 1992; Timko et al., 1993). A smaller proportion of outpatients (45%) than aftercare patients (62%) reported prior AUD treatment. The majority of patients in each arm (95% outpatient, 98% aftercare) met criteria for dependence as opposed to abuse using the Structured Clinical Interview for DSM-III-R (Spitzer and Williams, 1985).
3.2. Relation between AA, network support/activities, and alcohol use over time
3.2.1. AA and alcohol use outcomes
Table 1 shows the relationship between AA and subsequent (lagged) alcohol use (PDA; DDD) among outpatient and aftercare patients. As anticipated, there were consistent associations between more frequent AA attendance during months 0-3 and less frequent, and less intense, alcohol use at 12-15 month follow-up. Among the covariates examined, age had a negative association with PDA among outpatients with younger adults drinking more frequently than older adults (b = -.0044, p < .0001). In the aftercare sample, a greater number of prior treatments was associated with more intensive drinking (DDD; b = .1775, p < .001).
Table 1.
GLM results for AA attendance (0-3m) predicting transformed PDA and DDD (13-15m) for the Outpatient and Aftercare samplesa
| Variable | b (se) | t (df) | p |
|---|---|---|---|
| Outpatient Sample | |||
| baseline PDA | .0046(.0005) | 8.36(398) | <.0001 |
| Lagged AA attendance | .0046(.0007) | 5.83(409) | <.0001 |
| | |||
| Aftercare Sample | |||
| baseline PDA | .0021(.0006) | 3.21(481) | .0014 |
| Lagged AA attendance | .0034(.0005) | 6.49(462) | <.0001 |
| | |||
| Outpatient Sample | |||
| baseline DDD | .0269(.0025) | 4.33(462) | <.0001 |
| Lagged AA attendance | -.0124(.0025) | -4.99(362) | <.0001 |
| | |||
| Aftercare Sample | |||
| baseline DDD | .0237(.0052) | 6.56(457) | <.0001 |
| Lagged AA attendance | -.0118(.0018) | -6.37(465) | <.0001 |
Control variables included in the models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, treatment assignment, baseline network support/activity variables. PDA=Percent Days Abstinent; DDD=Drinks per Drinking Day.
3.2.2. AA and network support/activities
Table 2 shows the relationships between AA attendance and the four network support/activity variables. Consistent across aftercare and outpatient participants, greater AA attendance was associated with increases in pro-abstinent network ties and in abstinent activities as well as decreases in pro-drinking network ties and drinking activities at 9 months after controlling for baseline covariates. There was one interaction detected among aftercare patients. Specifically, high AA attendance (i.e., attending AA three or more times per week) during months 0-3 increased 9m abstinent activities more (mean difference = 1.39) for patients who had very low levels of abstinent activities at intake, but did not significantly increase abstinent activities for those already high in abstinent activities at intake (mean difference = 0.08; t = -2.62, p =. 009). Among the covariates examined, a greater number of prior treatments was associated with a reduced 9-month pro-drinking network among outpatients. Also among outpatients, males had significantly more drinking activities (b = -.2996, p < .001) and fewer abstinent activities (b = .3438, p < .01) than females. In addition, unmarried status was associated with more drinking activities among outpatients (b = .2841, p < .001).
Table 2.
GLM results for AA attendance (0-3m) predicting network support/activities (4-9m) for the Outpatient and Aftercare samplesa
| Variable | b (se) | t (df) | p |
|---|---|---|---|
| Outpatient Sample | |||
| baseline pro-abstinence network | .5564(.0595) | 9.35(265) | <.0001 |
| AA | .0107(.002l) | 4.97(321) | <.0001 |
| AA X baseline pro-abst network | -.0033(.0034) | -0.97(117) | .3345 |
| | |||
| Aftercare Sample | |||
| baseline pro-abstinence network | .3583(.0754) | 4.75(182) | <.0001 |
| AA | .0058(.0014) | 4.19(396) | <.0001 |
| AA X baseline pro-abst network | -.0012(.0027) | -0.47(264) | .6402 |
| | |||
| Outpatient Sample | |||
| baseline pro-drinking network | .2720(.0705) | 3.86(415) | <.0001 |
| AA | -.0064(.0021) | -2.97(300) | .0032 |
| AA X baseline pro-drink network | -.0017(.0033) | -.53(427) | .5944 |
| | |||
| Aftercare Sample | |||
| baseline pro-drinking network | .0900(.0611) | 1.47(369) | .1413 |
| AA | -.0044(.0012) | -3.56(216) | .0005 |
| AA X baseline pro-drink network | -.0042(.0023) | -1.84(404) | .0664 |
| | |||
| Outpatient Sample | |||
| baseline abstinent activities | .3252(.0619) | 5.25(253) | <.0001 |
| AA | .0089(.0029) | 2.98(269) | .0032 |
| AA X baseline abstinent activities | -.0010(.0020) | -0.52(283) | .6067 |
| | |||
| Aftercare Sample | |||
| baseline abstinent activities | .1826(.0745) | 2.45(323) | .0172 |
| AA | .0085(.0019) | 4.43(171) | <.0001 |
| AA X baseline abstinent activities | -.0050(.0019) | -2.62(207) | .0094 |
| | |||
| Outpatient Sample | |||
| baseline drinking activities | .2166(.0613) | 4.84(447) | <.0001 |
| AA | -.0055(.0020) | -2.69(438) | .0074 |
| AA X baseline drinking activities | .0011(.0028) | 0.38(461) | .7055 |
| | |||
| Aftercare Sample | |||
| baseline drinking activities | .1340(.0577) | 2.32(430) | .0207 |
| AA | -.0073(.0013) | -5.38(383) | <.0001 |
| AA X baseline drinking activities | -.0031(.0023) | -1.35(370) | .1755 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, treatment assignment, treatment site.
3.2.3. Relationship between network support/activities and alcohol use outcomes
With the exception of drinking activities among outpatients in predicting DDD (p=.06), when examined as individual predictors, both pro-abstinent and pro-drinking social ties and abstinent and drinking activities were significantly associated with PDA and DDD in the expected directions (ps<.006). However, when these mediators were combined in one model to predict drinking outcomes abstinent and drinking activities were no longer significant (see table 3). For both outpatient and aftercare participants, pro-abstinent network ties were significantly positively associated, and pro-drinking network ties were significantly negatively associated, with PDA. For DDD, only pro-drinking social networks met our criterion for statistical significance (i.e., <.01; see Table 3) among outpatient and aftercare participants. For significant covariates, younger age (b = -.0048, p < .001) and greater prior treatment episodes (b = -.0312, p < .01) were associated with lower PDA among outpatient participants. For DDD, prior treatment was positively associated with drinking intensity in both outpatient and aftercare samples (b = .1110, p < .005, b = .1900, p < .001).
Table 3.
GLM results for network support/activities (4-9m) predicting PDA and DDD (13-15m) for the Outpatient and Aftercare samplesa
| Variable | b (se) | t (df) | p |
|---|---|---|---|
| Outpatient Sample (PDA) | |||
| baseline pro-abstinence network | -.0400(.0126) | -3.18(407) | .0016 |
| baseline pro-drinking network | -.0045(.0128) | -0.35(316) | .7258 |
| baseline abstinent activities | .0135(.0100) | 1.34(304) | .1822 |
| baseline drinking activities | .0119(.0134) | 0.89(395) | .3747 |
| baseline PDA | .0044(.0005) | 9.14(445) | <.0001 |
| pro-abstinence network | .0693(.0124) | 5.60(319) | <.0001 |
| pro-drinking network | -.0972(.0122) | -7.97(428) | <.0001 |
| abstinent activities | .0106(.0099) | 1.06(262) | .2884 |
| drinking activities | -.0222(.0174) | -1.28(309) | .2021 |
| | |||
| Aftercare Sample (PDA) | |||
| baseline pro-abstinence network | -.0176(.0158) | -1.11(269) | .2667 |
| baseline pro-drinking network | .0006(.0149) | 0.04(340) | .9655 |
| baseline abstinent activities | .0256(.0125) | 2.05(340) | .0413 |
| baseline drinking activities | .0466(.0166) | 2.81(397) | .0051 |
| baseline PDA | .0019(.0006) | 3.45(347) | .0006 |
| pro-abstinence network | .0395(.0147) | 2.62(309) | .0076 |
| pro-drinking network | -.1038(.0164) | -6.29(408) | <.0001 |
| abstinent activities | .0262(.0123) | 2.12(181) | .0350 |
| drinking activities | -.0487(.0214) | -2.27(282) | .0238 |
| | |||
| Outpatient Sample (DDD) | |||
| baseline pro-abstinence network | .0324(.0404) | 0.80(435) | .4235 |
| baseline pro-drinking network | .0374(.0406) | 0.92(387) | .3585 |
| baseline abstinent activities | -.0140(.0321) | -0.44(327) | .6633 |
| baseline drinking activities | .0073(.0453) | 0.17(380) | .8666 |
| baseline DDD | .0331(.0061) | 5.44(300) | <.0001 |
| pro-abstinence network | -.0806(.0395) | -2.43(367) | .0158 |
| pro-drinking network | .2649(.0401) | 6.61(366) | <.0001 |
| abstinent activities | -.0455(.0316) | -1.44(332) | .1501 |
| drinking activities | -.0144(.0575) | -0.25(226) | .8032 |
| | |||
| Aftercare Sample (DDD) | |||
| baseline pro-abstinence network | .0625(.0572) | 1.09(256) | .2757 |
| baseline pro-drinking network | .0442(.0546) | 0.81(266) | .4187 |
| baseline abstinent activities | -.0201(.0594) | 0.45(319) | .6556 |
| baseline drinking activities | -.1504(.0594) | -2.53(395) | .0117 |
| baseline DDD | .0216(.0049) | 4.43(438) | <.0001 |
| pro-abstinence network | -.0697(.0623) | -1.16(77) | .2512 |
| pro-drinking network | .2634(.0623) | 4.23(234) | <.0001 |
| abstinent activities | -.0560(.0483) | 1.32(79) | .1859 |
| drinking activities | .0993(.0749) | -1.16(417) | .2494 |
Variables included in these models but not shown above: age, gender, ethnicity, marital status, employment, number of prior alcohol treatments, treatment assignment. PDA=Percent Days Abstinent; DDD=Drinks per Drinking Day.
3.2.4. Social networks and activities as mediators of AA's effect on alcohol use
We conducted mediation analyses for the cases where all paths in the lagged models were statistically significant using the MacKinnon method noted previously. As shown in Table 4, there was significant consistent mediation observed for pro-abstinent and pro-drinking network ties across the outpatient and aftercare samples on PDA. This ranged from a low of 7% of the direct effect between AA and PDA (mediated by pro-abstinent network ties for aftercare patients) to a high of 16% of the direct effect (mediated by pro-abstinent network ties for outpatients). AA-influenced reductions in pro-drinking network ties explained 13% of the effect on PDA for both patient samples. In contrast, there was less consistency in the meditational effects of the social network variables for intensity of drinking (DDD). Having more pro-abstinent network ties did not help explain lower DDD in relation to AA attendance for either outpatient or aftercare patients. However, reductions in pro-drinking network ties explained a portion of the effect of AA on DDD among outpatient (14% of the direct effect) and aftercare patients (12% of the direct effect).
Table 4.
The proportion of the Direct Effect (DE) of AA attendance (0-3m) on subsequent alcohol use outcomes (13-15m) accounted for by each hypothesized social network mechanism (4-9m) controlling for baseline covariates
| Z Mack | p | % of DE mediated | ||
|---|---|---|---|---|
| OP (PDA) | Pro-abstinent network | 3.72 | <.01 | 16% |
| Pro-drinking network | 2.78 | <.02 | 13% | |
| Abstinent activities | - | - | - | |
| Drinking activities | - | - | - | |
| AC (PDA) | Pro-abstinent network | 2.25 | <.03 | 7% |
| Pro-drinking network | 3.10 | <.01 | 13% | |
| Abstinent activities | - | - | - | |
| Drinking activities | - | - | - | |
| OP (DDD) | Pro-abstinent network | - | - | - |
| Pro-drinking network | -2.71 | <.02 | 14% | |
| Abstinent Activities | - | - | - | |
| Drinking Activities | - | - | - | |
| AC (DDD) | Pro-abstinent network | - | - | - |
| Pro-drinking network | -2.72 | <.02 | 12% | |
| Abstinent Activities | - | - | - | |
| Drinking Activities | - | - | - |
PDA=Percent Days Abstinent; DDD=Drinks per Drinking Day; OP=Outpatient; AC=Aftercare.
3.2.5 Subsidiary Analyses
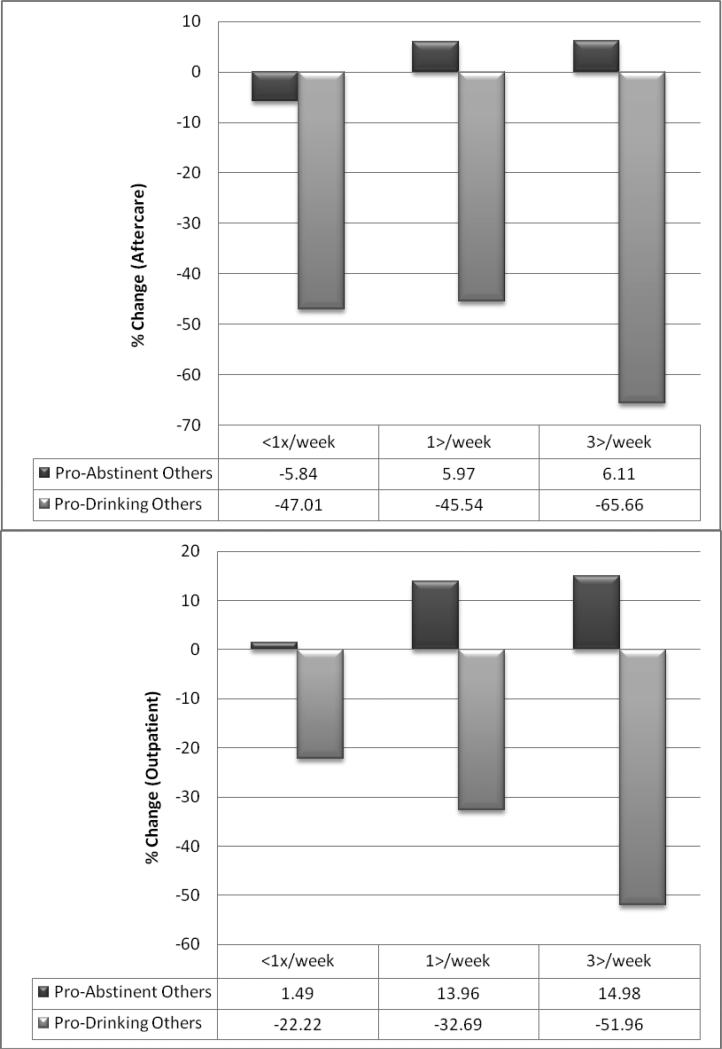
To elucidate the practical significance of these findings we examined how different levels of AA attendance were related to salutary changes among network ties, and how changes in network ties, in turn, related to changes in alcohol use.
Figure 2 shows the relationship between different frequencies of AA attendance and the percent change in both pro-abstinent and pro-drinking network ties from treatment intake to the 9-month follow-up. As shown, increasing AA attendance appears to exert a substantial monotone effect on decreasing pro-drinking network ties and a similar, although less substantial, linear effect on increasing pro-abstinent network ties. Among aftercare patients, increasing attendance from none or once or twice per week to three or more times per week reduced the number of pro-drinking network ties by a further 20% (from -45.54 to -65.66); among outpatients this reduction was in the range of 20-30%. Similarly, increasing AA attendance from none to three times per week was associated with a 10% and 15% increase in the number of pro-abstinent network ties among the aftercare and outpatient samples, respectively.
Figure 2.
Relationship between frequencies of AA attendance and changes in pro-abstinent and pro-drinking network ties.
In terms of changes in alcohol use, the influence of pro-drinking network ties on PDA and DDD was more influential than pro-abstinent network ties. For example, for every pro-drinking network tie present among aftercare patients there was a 9.6% reduction in PDA and a 20.1% increase in DDD; among outpatients there was 6.5% reduction in PDA and a 35.9% increase in DDD. In contrast, for every pro-abstinent network tie present among aftercare patients there was a smaller magnitude 3.4% increase in PDA and 5.0% decrease in DDD; among outpatients this effect translated into a 3.7% increase in PDA and a 9.9% decrease in DDD.
4. Discussion
This study found that AA attendance was consistently associated with better alcohol use outcomes as well as increases in abstinent activities and social network support for abstinence, and decreases in drinking activities and social network support for drinking. In addition, when examined separately, social ties and activities both predicted drinking outcomes, but when combined it was network ties rather than activities that were most influential in relation to better alcohol use outcomes. Lagged mediational analyses revealed that AA's association with greater abstinence was partially explained by its ability to both increase pro-abstinent network ties and decrease pro-drinking network ties, whereas its association with decreased intensity of alcohol use was partially explained by reductions in pro-drinking network ties only. Subsidiary analyses revealed the relatively greater benefit of reducing pro-drinking ties compared to increasing pro-abstinent ties, on alcohol use outcomes, and that greater AA attendance was associated with larger magnitude reductions in pro-drinking influences compared to increases in pro-abstinent influences.
Controlling for a number of confounding variables, including MATCH treatment assignment and the intake level of each hypothesized mechanism, attending AA during the first 3 months of the trial was associated with significant subsequent increases in the two social network support mediators and in the two social activity mediators. These results indicate that, over and above the therapeutic impact of the outpatient-delivered MATCH treatments, participation in AA increases network ties associated with abstinence and reduces network ties associated with drinking. It also enhances engagement in abstinent activities and reduces engagement in drinking activities. This pattern of findings was consistent across both the aftercare and outpatient arms of the trial, suggesting AA appears to mobilize adaptive social network and activity changes across individuals exhibiting a broad range of alcohol-related involvement and impairment.
When examined in the same lagged model predicting alcohol abstinence (PDA), only reductions in pro-drinking network ties and increases in pro-abstinent network ties conferred a unique and independent effect across both patient samples and in the expected directions. This suggests that while reducing drinking-related and increasing abstinence-related social activities may be helpful for sobriety, it is by increasing engagement with pro-abstinent ties, while also decreasing engagement with pro-drinking ties, that may make the most difference to sobriety. The subsidiary analyses also highlight the fact that at this stage of the recovery process, it is the reduction in pro-drinking networks that confers the greatest benefit on abstinence and drinking intensity.
The clinical implications of these findings are two-fold. First, as has been reported previously (Tonigan et al, 2003), regardless of the type of formal treatment, attending AA is likely to enhance abstinence. Second, whether patients attend AA or not, clinicians may wish to emphasize, in particular, the avoidance of former drinking acquaintances. Further, active engagement with abstinent acquaintances may provide an additional benefit. This emphasis on increasing alternative (non alcohol-related) rewarding social ties is a principal goal in well-supported approaches to treating addiction (e.g., the Community Reinforcement Approach; Azrin, 1976; Azrin et al., 1982). Regarding intensity of alcohol use (i.e., DDD), our analyses found mediational effects for reductions in pro-drinking ties only. The pattern of findings suggests when it comes to heavy alcohol use and relapse, pro-drinking network ties are detrimental even in the presence of pro-abstinent ties, and AA appears to work at least partially in reducing drinking intensity by reducing pro-drinking social networks.
Our analyses revealed that AA was associated both with significant increases in the pro-abstinence social network and significant decreases in the pro-drinking social network, which were both found to be mechanisms through which AA leads to greater rates of abstinence. These findings suggest that AA may exert its beneficial effects through two independent social mechanisms. However, as depicted in figure 2 the larger effect was related to AA's influence on reducing pro-drinking social ties. Most importantly, AA attendance may reduce relapse risk by reducing exposure to, or engagement with, people that support alcohol use. In addition, however, AA may also reduce relapse risk by enhancing the rewarding aspects of sobriety that come with greater engagement in a social recovery network. In other words, at this stage in the recovery process, high risk avoidance may be particularly important, but alternative and safe, social engagement may provide a smaller but additional benefit. AA appears to facilitate both.
4.1. Limitations
This study has some limitations, which should be considered. The sample was mostly male and Caucasian and participants were recruited to participate in a rigorous controlled trial. Thus, it is unknown to what extent these findings extend to other groups, particularly non-treatment-seeking populations. Although we found that the measures of our hypothesized social mechanisms were sensitive to change and were successful mediators of AA attendance, social influence is clearly a highly complex and multidimensional construct (Valente, 2010). Furthermore, the four social processes were examined simultaneously in relation to drinking outcomes. Although the inter-correlations among these variables were generally low, this analysis yielded potentially more conservative estimates than might have been obtained had each mediator's effect on drinking been obtained separately. In addition, although we employed a lagged design, our findings relate specifically to the influence of AA attendance during outpatient-delivered treatment on subsequent social network/activity changes and subsequent alcohol use. Inferences to the influence of AA on social processes later in recovery should not be made without further longitudinal investigation. Additional research is needed to determine how optimally to measure and model these complex phenomena and to determine how they may shape human behavior over time (Valente, 2010).
4.2. Conclusions
The investigation of mechanisms of behavior change is a relatively new endeavor in the addiction treatment and recovery field. A number of mechanisms through which AA may exert its beneficial effects have been investigated. These have included investigations on negative affect (Kelly et al., 2009; Kelly et al., 2010a; Kelly et al., 2010b), spirituality (e.g., Zemore, 2007), common processes variables (e.g., motivation, coping, self-efficacy; Connors et al, 2001, Morgenstern et al, 1997; Kelly et al., 2000) and social network mechanisms (e.g., Bond et al, 2003; Kaskutas et al, 2002). Using a uniquely large clinical alcohol use disorder sample exhibiting a wide range of alcohol-related involvement and impairment as well as a lagged, prospective study design, we found that AA also seems to promote abstinence and recovery by mobilizing important changes in social processes. Most importantly by reducing exposure to and involvement with pro-drinking social ties, but also by increasing exposure to, and involvement with pro-abstinent social ties. One of the potential “downstream” mechanisms by which such changes may decrease relapse risk is by reducing or eradicating exposure to alcohol related cues, thereby reducing craving, while simultaneously allowing or encouraging individuals to experience new social connections that are potentially rewarding and help reinforce recovery. AA appears to be an influential community resource that is able to effectively mobilize adaptive social changes that, in turn, enhance the chances for recovery from alcohol use disorder.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alcoholics Anonymous . Alcoholics Anonymous Comes of Age. AA World Services; New York: 1957. [Google Scholar]
- Azrin NH. Improvements in the community reinforcement approach to alcoholism. Behav Res Ther. 1976;14:339–348. doi: 10.1016/0005-7967(76)90021-8. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Sisson RW, Meyers RJ, Godley MD. Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiatry. 1982;3:105–112. doi: 10.1016/0005-7916(82)90050-7. [DOI] [PubMed] [Google Scholar]
- Barnard J, Rubin DB. Miscellanea. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; New York: 1997. [Google Scholar]
- Beattie MC, Longabaugh R. General and alcohol-specific social support following treatment. Addict Behav. 1999;24(5):593–606. doi: 10.1016/s0306-4603(98)00120-8. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and alcoholics anonymous on abstinence. J Stud Alcohol. 2003;64(4):579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Longabaugh R. Manual for the administration of the Important People and Activities Instrument. Adapted for use by Project MATCH for NIAAA 5R01AA06698-05 Environmental Treatment of Alcohol Abusers. Center for Alcohol and Addiction Studies, Brown University; Providence, RI: 1991. [Google Scholar]
- Connors GJ, Tonigan JS, Miller W. Religiousness and Responsiveness to Alcoholism Treatments. Department of Health and Human Services; Bethesda, MD: 2001. [Google Scholar]
- Dennis M, Scott C, Funk R, Foss M. The duration and correlates of addiction and treatment careers. J Subst Abuse Treat. 2005;28:s51–s62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: What is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. Rutgers Center of Alcohol Studies; Piscataway, NJ: 1993. pp. 41–76. [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Birchler GR. Family therapy techniques. In: Rotgers F, Morgenstern J, Walters ST, editors. Treating substance abuse: Theory and technique. Guilford Press; New York: 2003. pp. 140–165. [Google Scholar]
- Fenster J. Characteristics of clinicians likely to refer clients to 12-Step programs versus a diversity of post-treatment options. Drug Alcohol Depend. 2006;83(3):238–246. doi: 10.1016/j.drugalcdep.2005.11.017. [DOI] [PubMed] [Google Scholar]
- Finney JW, Hahn AC, Moos RH. The effectiveness of inpatient and outpatient treatment for alcohol abuse: The need to focus on mediators and moderators of setting effects. Addiction. 1996;91:1773–1796. [PubMed] [Google Scholar]
- Fiorentine R, Hillhouse MP. Drug treatment and 12-step program participation: The additive effects of integrated recovery activities. J Subst Abuse Treat. 2000;18(1):65–74. doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- Fox HC, Bergquist KL, Hong KI, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol dependent individuals. Alcohol Clin Exp Res. 2007;31(3):395–403. doi: 10.1111/j.1530-0277.2006.00320.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Gilks WR, Richardson S, Spiegelhalter DJ, editors. Markov Chain Monte Carlo in practice. Chapman and Hall; London: 1996. [Google Scholar]
- Goodman AC, Holder HD, Nishiura E, Hankin RJ. An analysis of short-term alcoholism treatment cost functions. Med Care. 1992;30(9):795–810. doi: 10.1097/00005650-199209000-00004. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Keys CB. Social network variables in Alcoholics Anonymous: A literature review. Clin Psychol Rev. 2008;28(3):430–450. doi: 10.1016/j.cpr.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havassy B, Hall S, Wasserman D. Social support and relapse: Commonalities among alcoholics, opiate users, and cigarette smokers. Addict Behav. 1991;16(5):235–246. doi: 10.1016/0306-4603(91)90016-b. [DOI] [PubMed] [Google Scholar]
- Hser Y, Anglin MD. Addiction Treatment and Recovery Careers. In: Kelly JF, White WL, editors. Addiction Recovery Management: Theory, Science, and Practice. Springer; New York: in press. [Google Scholar]
- Humphreys K. Clinicians’ referral and matching of substance abuse patients to self-help groups after treatment. Psychiatr Serv. 1997;48(11):1445–1449. doi: 10.1176/ps.48.11.1445. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Circles of recovery: Self-help organizations for addictions. Cambridge University Press; Cambridge, UK: 2004. [Google Scholar]
- Humphreys K, Greenbaum MA, Noke JM, Finney JW. Reliability, validity, and normative data for a short version of the Understanding of Alcoholism scale. Psychol Addict Behav. 1996;10:38–44. [Google Scholar]
- Humphreys K, Mankowski E, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Ann Behav Med. 1999;21(1):54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol Clin Exp Res. 2001;25(5):711–716. [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Encouraging post-treatment self-help group involvement to reduce demand for continuing care services: Two-year clinical and utilization outcomes. Alcohol Clin Exp Res. 2007;31(1):64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Hunter-Reel D, McCrady B, Hildebrandt T. Emphasizing interpersonal factors: An extension of the Witkiewitz and Marlatt relapse prevention model. Addiction. 2009;104:1281–1290. doi: 10.1111/j.1360-0443.2009.02611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM. In: Cognitive-Behavioral Coping Skills Therapy Manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence, Project MATCH Monograph Series. Vol. 4, DHHS Publication No. (ADM) 92-1895. Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Litt M, Hester R, editors. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Kaskutas LA. Alcoholics Anonymous Effectiveness: Faith Meets Science. J Addict Dis. 2009;28(2):145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Dow S, Yeterian JD, Kahler CW. Can 12-step groups strengthen and extend the benefits of adolescent addiction treatment. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2010.02.019. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do People Recover from Alcohol Dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addict Res Theory. 2009;17(3) [Google Scholar]
- Kelly JF, Myers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychol Addict Behav. 2000;14:376–89. [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Magill M, Tonigan JS, Pagano M. Mechanisms of behavior change in Alcoholics Anonymous: Does AA improve alcohol outcomes by Reducing Depression symptoms? Addiction. 2010a;105:626–636. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Tonigan JS, Magill M, Pagano M. Negative Affect, Relapse, and Alcoholics Anonymous: Does AA work by reducing anger? J Stud Alcohol Drugs. 2010b;71:3. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. Mutual-help groups. In: O'Donohue W, Cunningham JR, editors. Evidence-Based Adjunctive Treatments. Elsevier; New York: 2008. pp. 61–105. [Google Scholar]
- Laudet AB, Cleland CM, Magura S, Vogel HS, Knight EL. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. Am J Community Psychol. 2004;34(3-4):175–185. doi: 10.1007/s10464-004-7413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, Savage R, Mahmood D. Pathways to long-term recovery: A preliminary investigation. J Psychoactive Drugs. 2002;34(3):305–311. doi: 10.1080/02791072.2002.10399968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, White WL. An exploratory investigation of the association between clinicians’ attitudes toward twelve-step groups and referral rates. Alcohol Treat Q. 2005;23(1):31–45. doi: 10.1300/J020v23n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt M, Kadden R, Kabela-Cormier E, Petry N. Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction. 2008;103(4):638–648. doi: 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RA, Rubin DB. Statistical Analysis with Missing Data. 2nd Edition John Wiley; New York: 2002. [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93(9):1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network Support for Drinking. Project MATCH Hypotheses: Results and Causal Chain Analyses, US Dept. of Health and Human Services, 01-4283. 2001 [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Donovan DM, editors. Assessment of addictive behaviors. 2nd ed. Guilford Press; New York: 2005. [Google Scholar]
- Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- McCrady BS. To have but one true friend: Implications for practice of research on alcohol use disorders and social networks. Psychol Addict Behav. 2004;18:113–121. doi: 10.1037/0893-164X.18.2.113. [DOI] [PubMed] [Google Scholar]
- McLellan AT. Have we evaluated addiction treatment correctly? Implications from a chronic care perspective. Addiction. 2002;97:249–252. doi: 10.1046/j.1360-0443.2002.00127.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Miller WR. Motivational interviewing: Research, practice, and puzzles. Addict Behav. 1996;21:835–842. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca F. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol. 1994;S12:s112–s118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Willbourne P. Mesa Grande: A methodological analysis of clinical trials of treatment for alcohol use disorders. Addiction. 2002;97(3):265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Moos R. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88:109–121. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. The interplay between help-seeking and alcohol-related outcomes: Divergent processes for professional treatment and self-help groups. Drug Alcohol Depend. 2004;75(2):155–164. doi: 10.1016/j.drugalcdep.2004.01.016. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: A study of its therapeutic effects and mechanisms of action. J Consult Clin Psychol. 1997;65(5):768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE. Methodological characteristics and quality of alcohol treatment outcome studies, 1970-1998: An expanded evaluation. Addiction. 2002;97:253–263. doi: 10.1046/j.1360-0443.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll KM. Twelve-Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. NIAAA Project MATCH Monograph Series: Vol. 1. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1995. [Google Scholar]
- Project MATCH Research Group Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17(6):1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- Rosenquist JN, Murabito J, Fowler J, Christakis N. The Spread of Alcohol Consumption Behavior in a Large Social Network, Annals of Internal Medicine. Ann Intern Med. 2010;152:426–433. doi: 10.1059/0003-4819-152-7-201004060-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott C, Dennis M. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104(6):959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB. Structured Clinical Interview for DSM-III (SCID) Biometrics Research Division, New York State Psychiatric Institute; New York: 1985. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4rd Ed. Harper Collins; New York: 2001. [Google Scholar]
- Timko C, Finney J, Moos R, Moos B. The process of treatment selection among previously untreated help-seeking problem drinkers. J Subst Abuse. 1993;5(3):203–220. doi: 10.1016/0899-3289(93)90064-i. [DOI] [PubMed] [Google Scholar]
- Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: Comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. J Stud Alcohol. 2000;6(4):529–540. doi: 10.15288/jsa.2000.61.529. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor T, DelBoca F, editors. Treatment Matching in Alcoholism. Cambridge University Press; New York: 2003. pp. 184–204. [Google Scholar]
- Valente TW. Social Networks and Health: Models, Methods, and Applications. Oxford; New York: 2010. [Google Scholar]
- Witbrodt J, Kaskutas LA. Does diagnosis matter? Differential effects of 12-step participation and social networks on abstinence. Am J Drug Alcohol Abuse. 2005;31:685–707. doi: 10.1081/ada-68486. [DOI] [PubMed] [Google Scholar]
- Wu J, Witkiewitz K. Network support for drinking: an application of multiple groups growth mixture modeling to examine client-treatment matching. J Stud Alcohol Drugs. 2008;69(1):21–9. doi: 10.15288/jsad.2008.69.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE. A role for spiritual change in the benefits of 12-step involvement. Alcohol Clin Exp Res. 2007;31(s3):s76–s79. doi: 10.1111/j.1530-0277.2007.00499.x. [DOI] [PubMed] [Google Scholar]