Abstract
Evidence demonstrating the potential value of cardiopulmonary exercise testing (CPET) to accurately detect myocardial ischemia secondary to macro-vascular disease is beginning to emerge. Despite distinct mechanisms mediating ischemia in micro-vascular and macrovascular coronary artery disease (CAD), the net physiologic effect of exercise-induced left ventricular (LV) dysfunction is common to both. The abnormal physiologic response to CPET may, therefore, be similar in patients with macro- and micro-vascular ischemia. The following case report describes the CPET abnormalities in a patient with suspected microvascular CAD and the subsequent improvement in LV function following three weeks of medical therapy with the anti-ischemic drug ranolazine.
Introduction
While cardiopulmonary exercise testing (CPET) is an important diagnostic modality in the clinical assessment of patients with heart failure, its potential utility in defining physiologic abnormalities in other patient populations has recently garnered attention. Belardinelli et al. (1) demonstrated, in patients with documented macro-vascular coronary artery disease (CAD) and reversible perfusion defects on myocardial perfusion imaging, assessment of CPET variables increased the sensitivity of the standard stress electrocardiogram (ECG) from 46% to 87% and the specificity from 66% to 74%. The physiologic basis for applying CPET gas exchange measurements in this population is predicated on their ability to accurately identify the onset of ischemia-induced left ventricular (LV) dysfunction during physical exertion and to more precisely quantify the magnitude of physiologic impairment.(2)
Micro-vascular ischemia is becoming increasingly recognized as a significant cause of morbidity, especially in women with angiographically normal coronary arteries.(3) Because standard exercise stress testing in women is frequently associated with appreciable rates of false-positive results, it has limited diagnostic accuracy in detecting microvascular ischemia.(4) Despite distinctly different pathophysiologic processes mediating macro- and micro-vascular ischemia, exercise-induced LV dysfunction may be a feature common to both conditions. CPET may, therefore, prove to be a valuable diagnostic tool in patients with myocardial ischemia of microvascular origin. This case study describes the CPET response of a patient with suspected microvascular ischemia prior to and following an anti-ischemic therapy.
Case Report
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology.
Baseline Assessment
A 59 year-old female with a history of hypertension and rheumatic fever presented with exertional chest discomfort and dyspnea over the preceding several months. She had a 12- pack year tobacco use history that ended at age 30. Her current medications included atenolol, estrogen and aspirin.
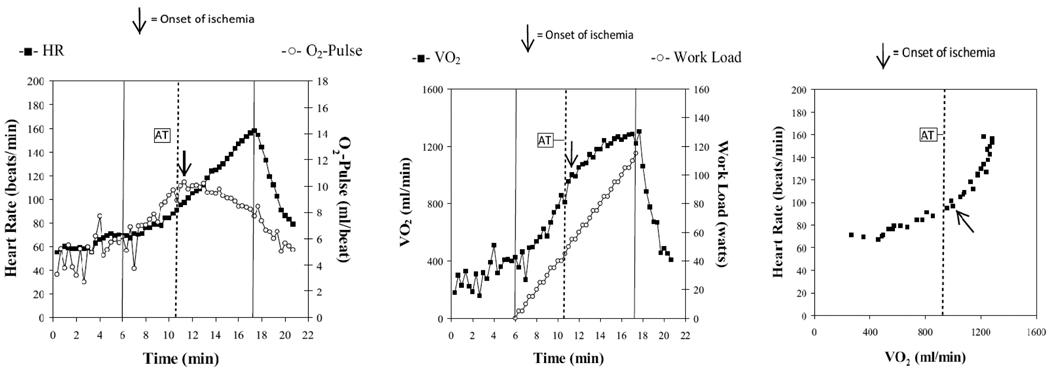
The patient performed exercise on a cycle ergometer, stopping secondary to dyspnea and reaching a peak respiratory exchange ratio and heart rate (HR) of 1.37 and 98% of age-predicted, respectively. She achieved a peak VO2 of 19.2 mlO2•kg−1•min−1 (94% predicted) and an anaerobic threshold (AT) of 13.9 mlO2•kg−1•min−1. Her O2 uptake kinetics, assessed by the change in VO2 as a function of increasing work rate (ΔVO2/ΔWR), and O2-pulse (VO2/HR) diverted from their expected normal linear trajectory at a HR of ~90 beats per minute, a change commonly observed with exercise-induced myocardial dysfunction. Figure 1 illustrates the patients O2-pulse, ΔVO2/ΔWR response and VO2-HR response. The ECG revealed ~1.0 mm horizontal ST-segment depression in the inferior and lateral leads. The CPET and ST-segment abnormalities were noted at ~55 and ~65 watts, respectively.
Figure 1.
AT: Anaerobic threshold, determined by the V-slope method
VO2: Oxygen uptake, milliliters per minute (ml/min)
HR: Heart rate, beats per minute
The patient subsequently underwent 2-dimensional echocardiography, gated SPECT sestamibi myocardial perfusion scintigraphy, and cardiac catheterization. All studies showed no structural heart disease, normal epicardial coronary anatomy and the absence of any significant flow-limiting stenoses. Despite the normal coronary angiogram, the abnormal CPET response, a positive stress ECG and dyspnea at peak exercise effectively reproduced the ischemic cascade and suggested a diagnosis of microvascular ischemia as the etiology of her symptoms.
Post-Pharmacologic Intervention
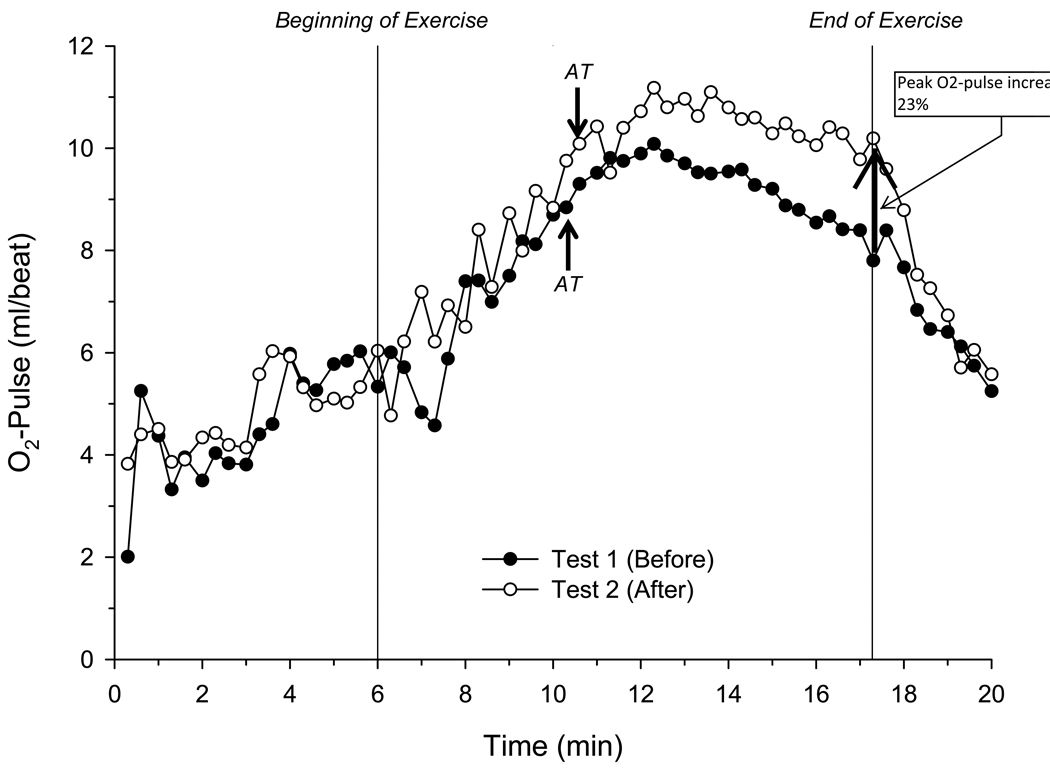
As a result of her abnormal baseline assessment suggestive of myocardial ischemia, the patient was prescribed ranolazine, a novel anti-ischemic agent that blocks late inward sodium current at the onset of cellular ATP depletion,(5) at a dose of 500 mg twice daily for 1 week with up-titration to 1000 mg twice daily thereafter. CPET was repeated after three weeks of therapy. Compared to the baseline study, key CPET findings during follow-up testing revealed that the patient: 1) Terminated exercise due to leg fatigue only, 2) Attained a peak RER of 1.24, 3) Achieved a peak VO2 of 23.5 mlO2•kg−1•min−1 and AT @ 15.0 mlO2•kg−1•min−1 (22% and 7.9% improvements compared to baseline, respectively), 4) Did not exhibit flattening of the O2-pulse until a HR of 100 bpm, 5) Showed a peak O2-pulse that was 23% higher at follow-up as compared with baseline, 6) Demonstrated a more linear ΔVO2/ΔWR, 7) Displayed a peak HR in test 2 that was 10 beats lower than in test 1, and 8) Showed a delay in onset of ischemic ECG changes (O2-pulse trajectory changed at ~65 watts of work followed by ST depression noted at ~90 watts). Figure 2 illustrates the pre and post treatment O2-pulse responses. Note that the O2 pulse at any given workload is higher in test 2 as compared with test 1.
Figure 2.
O2-Pulse: Oxygen Pulse, oxygen uptake (ml/min) divided by heart rate (beats per minute) O2-pulse = Stroke volume X C(a-v)O2
Discussion
Previous research in this area has focused on the utility of CPET to detect macro-vascular ischemia due to epicardial CAD.(1) To our knowledge, this is the first documentation of CPET abnormalities, which were improved by a pharmacologic intervention, in a patient with suspected microvascular ischemia and angiographically normal coronary arteries. It is becoming increasingly recognized that microvascular ischemia, particularly in women, is a significant cause of exertional intolerance and angina.(3) To better detect this condition and its functional significance with regard to left ventricular performance, new methods of evaluation must be identified. Peix et al previously demonstrated that postmenopausal women with normal coronary angiograms diagnosed with microvascular ischemia, frequently developed LV dysfunction during exercise testing.(6) Subjects with either macro- or micro-vascular ischemia may, therefore, demonstrate a similar CPET response, although myocardial perfusion imaging and coronary angiographic findings may show the presence or absence of significant epicardial CAD, respectively. Given the potential advantages of CPET to accurately detect and quantify reversible LV dysfunction in a non-invasive manner without radiation, utilization of this assessment technique in the evaluation and management of suspected microvascular ischemia may be clinically important. Incorporation of CPET may likewise be of diagnostic value to reduce the high rate of false positive stress ECG tests observed in women. Moreover, serial assessment with CPET enables a more accurate quantification of improvement in functional capacity (change in peak VO2) and also enables the physician to discern the mechanism of improvement (improved peak stroke volume in this case). Future investigations should be directed at more thoroughly evaluating the role of CPET in the diagnosis and assessment of treatment efficacy of myocardial ischemia.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
From Met-test, there was no funding associated with this paper
Reference List
- 1.Belardinelli R, Lacalaprice F, Carle F, et al. Exercise-induced myocardial ischaemia detected by cardiopulmonary exercise testing. Eur Heart J. 2003;24:1304–1313. doi: 10.1016/s0195-668x(03)00210-0. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhry S, Arena R, Wasserman K, et al. Exercise-Induced Myocardial Ischemia Detected by Cardiopulmonary Exercise Testing. Am J Cardiol. 2008 doi: 10.1016/j.amjcard.2008.10.034. Ref Type: In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Humphries KH, Pu A, Gao M, Carere RG, Pilote L. Angina with "normal" coronary arteries: sex differences in outcomes. Am Heart J. 2008;155:375–381. doi: 10.1016/j.ahj.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 4.Bellasi A, Raggi P, Merz CN, Shaw LJ. New insights into ischemic heart disease in women. J Calif Dent Assoc. 2008;36:107–114. [PubMed] [Google Scholar]
- 5.Stone PH. Ranolazine: New Paradigm for Management of Myocardial Ischemia, Myocardial Dysfunction, and Arrhythmias. Cardiology Clinics. 2008;26:603–614. doi: 10.1016/j.ccl.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Peix A, Garcia EJ, Valiente J, et al. Ischemia in women with angina and normal coronary angiograms. Coron Artery Dis. 2007;18:361–366. doi: 10.1097/MCA.0b013e3281689a3f. [DOI] [PubMed] [Google Scholar]
- 7.Coats AJS. Ethical authorship and publishing. International Journal of Cardiology. 2009;131:149–150. doi: 10.1016/j.ijcard.2008.11.048. [DOI] [PubMed] [Google Scholar]