Abstract
Purpose
The aim of this report is to present a previously unreported causative organism associated with brown-pigmented hypopyon in a patient with endophthalmitis.
Methods
This is a retrospective case report which includes clinicopathologic correlations.
Results
Vitreous cultures demonstrated Streptococcus bovis infection resulting in a brown-pigmented hypopyon, with uveal pigment found intra- and extracellularly on pathologic examination of the pupillary membrane.
Conclusions
S. bovis endophthalmitis may be a cause of dark hypopyon, especially in patients with a history of liver disease, and, when identified, warrants colonoscopy and cardiac workup.
Keywords: Streptococcus bovis, Brown/dark hypopyon, Endophthalmitis, Colon cancer, Endocarditis
Introduction
The presence of brown pigment within a hypopyon is a useful diagnostic clue and has been reported in the setting of necrotic intraocular melanoma as well as Listeria monocytogenes and Serratia marcescens endogenous endophthalmitis [1, 2].
We report a patient that presented with brown hypopyon in the setting of Streptococcus bovis endogenous endophthalmitis, thereby expanding the differential diagnosis for this clinical clue. This report also discusses the systemic associations, especially colon cancer and endocarditis [3].
Case report
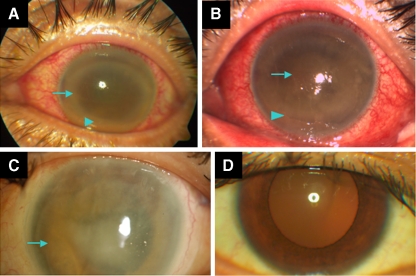
A 47-year-old Asian man with a history of cirrhosis and alcoholism was referred with a red, painful left eye of 3-days duration. On examination, visual acuity was 20/70 in the right eye and light perception in the left eye. Pressures were 15 and 20 in the right and left eyes, respectively. Examination of the left eye demonstrated a corneal ring infiltrate, brown hypopyon (Fig. 1a), and a dark pupillary membrane. B-scan ultrasonography demonstrated dense vitreous opacities, and a presumptive diagnosis of endogenous endophthalmitis was made. The patient underwent vitreous tap and intravitreal injection of vancomycin 1 mg/0.1 mL, ceftazidime 2.25 mg/0.1 mL, and voriconazole 100 mcg/0.1 mL.
Fig. 1.
a–d External photographs. a Left eye, at presentation, dark corneal ring infiltrate (arrow), and brown hypopyon (arrowhead). b Four days later, progression of dark hypopyon (blue arrowhead) and development of a brown papillary membrane (arrow). c Left eye, postoperative corneal edema and significant iris heterochromia (arrow). d Right eye, showing the patient's original iris color, obtained at a similar time point as c
Blood cultures were drawn and the patient was started on intravenous penicillin 3 million units/4 h and cefotaxime 1 gm/8 h for probable bacteremia. Abdominal ultrasound and CT showed evidence of cirrhosis, and transthoracic echocardiography was normal. Vitreous and blood cultures revealed S. bovis. The patient underwent colonoscopy, which ruled out colon cancer.
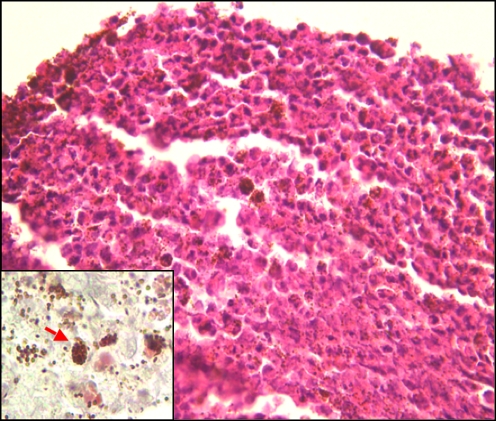
The left eye did not improve (Fig. 1b); on day 5 he underwent a second tap and injection with vancomycin, ceftazidime, and dexamethasone. Vitreous cultures remained positive for S. bovis (vancomycin sensitive), therefore, the patient underwent pars plana vitrectomy, lensectomy, pupillary membranectomy, and intravitreal vancomycin on day 9. The vitreous specimen was positive for S. bovis, while the pupillary membrane showed extensive uveal pigment, both extracellularly and within necrotic leukocytes (Fig. 2).
Fig. 2.
Histopathological aspect of pupillary membrane, displaying necrotic leukocytes admixed with a large amount of uveal pigment, both extra- and intracellularly (hematoxylin-eosin, original magnification ×400). Gram stain was negative for bacteria (inset, original magnification ×1,000). Note intracellular pigment granules (inset, arrow)
On day 19, the patient underwent repeat vitreous cultures and intravitreal injection of vancomycin and dexamethasone. Cultures were negative, however the final visual acuity was light perception and the eye developed significant iris heterochromia (Fig. 1c and d).
Discussion
This report expands the causes of dark hypopyon to include S. bovis, a Gram (+) cocci occasionally isolated from the human digestive tract and known to cause endocarditis, and morez rarely, urinary infections and neonatal septicemia and meningitis. Although rarely associated with ocular infections, S. bovis has been reported in cases of endogenous endophthalmitis, although the authors did not comment on the color of the hypopyon [4].
An important association between S. bovis and colon cancer has been demonstrated, although the exact mechanism remains elusive [2]. A change in colonic flora secondary to hepatic dysfunction was hypothesized to explain S. bovis translocating from the intestinal mucosa into the blood stream [5]. Our patient had longstanding liver dysfunction, which likely contributed to his bacteremia; he did not, however, develop colon cancer during 4 years of follow up.
Pink hypopyon has been associated with both S. marcescens due to necrosis and bleeding and Klebsiella pneumonia due to red pigment prodigiosin [6, 7]. L. monocytogenes endophthalmitis presents with brown hypopyon, profound vision loss, and no identifiable extraocular focus of infection [2]. In contrast to our patient, Listeria is associated with significant glaucoma, which, similar to the dark hypopyon, is ascribed to pigment dispersion. While our patient had normal IOP, pigment dispersion (Fig. 2) and eventual iris heterochromia (Fig. 1d) suggest a similar mechanism.
Conclusion
In summary, S. bovis endophthalmitis may present with brown hypopyon, and should be suspected in patients with a history of liver disease. Once S. bovis is cultured, colonoscopy and cardiac workup should be performed.
Acknowledgements
Supported in part by an unrestricted grant to the Department of Ophthalmology from Research to Prevent Blindness Inc., New York, NY; grant from the Fletcher Jones Foundation.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
No authors have any financial/conflicting interests to disclose.
References
- 1.Eliott D, OBrien TP, Green WR, et al. Elevated intraocular pressure, pigment dispersion and dark hypopyon in endogenous endophthalmitis from Listeria monocytogenes. Surv Ophthalmol. 1992;37(2):117–124. doi: 10.1016/0039-6257(92)90074-4. [DOI] [PubMed] [Google Scholar]
- 2.Equi R, Green R. Endogenous Serratia marcescens endophthalmitis with dark hypopyon: a case report and review. Surv Ophthalmol. 2001;46(3):259–268. doi: 10.1016/S0039-6257(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 3.Klein RS, Recco RA, Catalano MT, et al. Association of Streptococcus bovis and carcinoma of the colon. N Engl J Med. 1977;297(15):800–802. doi: 10.1056/NEJM197710132971503. [DOI] [PubMed] [Google Scholar]
- 4.Bleibel W, D’Silva K, Elhorr A, Bleibel S, Dhanjal U. Streptococcus bovis endophthalmitis: a unique presentation of colon cancer. Dig Dis Sci. 2007;52(9):2336–2339. doi: 10.1007/s10620-006-9287-x. [DOI] [PubMed] [Google Scholar]
- 5.Zarkin BA, Lillemoe KD, Cameron JL, et al. The triad of Streptococcus bovis bacteremia, colonic pathology, and liver disease. Ann Surg. 1990;211(6):190–191. doi: 10.1097/00000658-199006000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chao AN, Chao A, Wang NC, et al. Pink hypopyon caused by Klebsiella pneumonia. Eye(Lond) 2010;24(5):929–931. doi: 10.1038/eye.2009.202. [DOI] [PubMed] [Google Scholar]
- 7.al Hazzaa SA, Tabbara KF, Gammon JA. Pink hypopyon: a sign of Serratia marcescens enophthalmitis. Br J Ophthalmol. 1992;76(12):764–765. doi: 10.1136/bjo.76.12.764. [DOI] [PMC free article] [PubMed] [Google Scholar]