Abstract
Aim. To document population perceptions of well-being and predictors of self-assessed well-being.
Methods. National face-to-face interview survey of adults aged ≥16 years, conducted by the Office for National Statistics for their Omnibus Survey in Britain (response 58%; 1049 of 1823 eligible).
Results. People aged 65+ years were more likely than younger people to define well-being as being able to continue to do the things they had always done. Most men and women, in all age groups, rated their well-being and mental well-being positively. Self-rated health, mental health symptoms, long-standing illness and social support were the main drivers of overall well-being in all age groups. Mental health symptoms, long-standing illness and social support were the main drivers of mental well-being. For example, in reduced multivariable models, those who reported no long-standing illness had almost twice the odds of others, of good, rather than not good, overall well-being, and over three times the odds of good, rather than not good, mental well-being. The odds of good versus not good overall well-being were also multiplied by 1.002 for each additional available person for comfort and support and similarly by 1.073 in relation to mental well-being.
Conclusions. Understanding the drivers of well-being among adults, including older adults, is of high policy importance. Attention should be focused on improvements in population health and functioning and on encouraging younger and older people to develop and maintain social support networks and engagement in social activities.
Keywords: Ageing, health, social support, survey, well-being
Introduction
Positive perspectives in psychology view old age as a period of opportunity and well-being, with retention or potential development, of the psychological resources to cope with life’s challenges.1 It has been suggested that one of the ways of achieving greater well-being is adoption of psychological strategies, including promoting self-mastery and control and self-enhancing downward, not upward, comparisons with others.2 This coincides with worldwide public health interest in the promotion of well-being in older age and the compression of morbidity into fewer years of later life, driven by concerns about increasing health and social care expenditure in ageing societies. This is also reminiscent of the World Health Organization’s 1948 definition of health >50 years ago, which emphasized total mental, physical and social well-being.3
Well-being is a dynamic multifaceted concept. Subjective well-being consists of people’s own assessments of their overall lives, past and present, either cognitive (e.g. satisfaction) or affective (e.g. feelings of joy, pleasure, happiness),4–6 reflecting the influence of early Greek and 19th century utilitarian philosophy, with its focus on hedonism. Objective indicators (e.g. income) are generally, albeit weakly, associated with self-ratings of well-being and related indicators, including overall happiness, life satisfaction and quality of life (QoL).7–10 It has been argued, however, that once a certain level of human need has been met and a certain level of wealth has been achieved in society, material wealth contributes little to happiness.11
Although there is a current awareness that well-being has no clearly defined opposite, and it is more than the absence of ‘ill-being’, there are no agreed definitions, other than that it is a ‘good thing’, and much conceptual confusion.12,13 An agreed definition is needed; otherwise, its effective precursors will remain unidentified. But agreed by whom? Most existing models are discipline and culture specific. Rarely do definitions reach across disciplines and rarely are laypeople consulted about their views. The consequence is likely to be that any policy actions to improve well-being will be weakened by their lack of relevance to lay people. While lay perceptions of successful ageing, active ageing and QoL have been reported,14–16 there are few reports of lay definitions of well-being. One qualitative study17 reported that older men and women both identified family, health, activities, friendship, philosophy and jobs (in this order) were the most important to psychological well-being. While men were more likely than women to report that they would not change anything in their lives, women reported their desire to have had more friends and family.
Public health policy has focused mainly on promoting physical activity to maintain mental and physical functioning18 rather than on a multifaceted concept, which includes complex subjective, social and psychological dimensions. There are exceptions to reductionist views.19,20 NHS Scotland (2006)20 defined mental well-being in terms of wider well-being and as encompassing subjective feelings of life satisfaction, optimism, self-esteem, mastery and feeling in control, having a purpose in life, a sense of belonging and support. This is consistent with the long US tradition of social indicators research on general well-being.21 Promoting positive mental well-being is regarded as crucial in achieving a healthier nation, enabling older people to remain living in their own homes (www.communitycare.co.uk/.../Popps-and-prevention-for-elderly-people.htm; website accessed 05 September 2010) and having benefits to society. It is a current priority at national and local government levels (www.communities.gov.uk/localgovernment/…/wellbeingpower; website accessed 05 September 2010) and for health and social care commissioners.
Research is inconsistent on age–sex variations with life satisfaction, probably due to differing samples and measures used. Some have reported greater self-assessed well-being among younger, than older, people,22 although older men have also been found to have worse well-being than older women.23 A U-shaped relationship of well-being with age has been reported from survey research in the USA: from ages 50 to 85, people felt progressively better, with 85-year-olds reporting a greater sense of well-being than the 18-year-olds.24 Gender differences with well-being have been reported; marital status, health status and depression being predictive for well-being among men aged 60+ years, and self-rated health and depression only were predictive for women.25 Social contact and support have also been significant predictors.26,27 While promoting well-being is an issue for all ages, it is also pertinent in older age, given that there are more people aged in their 70s and 80s, and with increased life expectancy, than ever before. There is a policy concern about the potential costs of a more disabled population for public sector services and emphasis on the benefits of facilitating people to remain living in their own homes.
QoL is often regarded as an outcome indicator of well-being. Over three-quarters of people aged ≥65 years nationally report having a good QoL.28 However, for the remainder, negative influences on well-being, and thereby QoL, have been reported to include loneliness, low levels of social support and neighbourliness, poor physical functioning, poverty and lack of psychological resources.28–32 With older age, major life challenges are increasingly likely to occur, including declining health and functioning, with adverse effects on independence and social participation, social network losses due to illness and death of relatives, friends and neighbours and frailty or vulnerability to adverse outcomes.33 Each has potentially adverse repercussions for well-being. As Age Concern England and Help the Aged (2009)34 pointed out, these factors can blight the lives of millions of older people. Earlier research among ∼3000 people aged 65+ and 85+ years living at home reported that there were few improvements in psychological or physical well-being over 2.5 years of follow-up.35–39 Older people with higher levels of emotional, social and psychological well-being make less use of health and social services as, given their higher levels of self-esteem, they are more able to cope with problems in their daily lives, optimize opportunities and to have more active lifestyles.28 However, the influencing role of social support in promoting mental well-being is inconsistent.28,39 There is some evidence that also suggests that physical activity can prevent some aspects of mental illness in older people, such as depression, dementia and Alzheimer’s disease.40,41 The study presented here aims to document population perceptions of well-being and predictors of self-assessed well-being.
Methods
The data were derived from a national interview survey of adults aged ≥16 years, conducted by the Office for National Statistics (ONS) for their Omnibus Survey in Britain. The Omnibus Survey is conducted monthly and enables independent researchers (alongside government departments) to include a small number of questions in distinct topic modules. Although the questions were necessarily limited in number, inhibiting inclusion of a wider range of theoretically relevant variables and their measurement scales, the Omnibus Survey provides a valuable opportunity to reach a national random sample of adults.
The sampling frame used for the Omnibus Survey was the British postcode address file of ‘small users’. This file includes all private household addresses. A new sample of 67 postal sectors is selected each month. Postal sectors were selected with probability proportional to size, and stratified by region, and where the household reference person is in National Statistics Socio-Economic Classification (NS-SEC) 1-3 (employers in large organizations, higher managerial occupations and higher professional employees/self-employed) and the proportion of people aged >65 years.
Within each sector, 30 addresses (‘delivery points’) were selected randomly with a target sample size per survey of 1200 adults aged ≥16 years; one household within multioccupied address is sampled using a Kish Grid and one person per sampled household is selected for face-to-face interview using standard ONS procedures to randomly select one person. Because only one household member is interviewed per household, people in households containing few adults had a better chance of selection than those in households with many. A weighting factor is applied by ONS to correct for this unequal probability of selection, as well as for any differing rates of non-response for age group by sex.
Response rates
The survey interviews with Omnibus Survey sample respondents aged 16+ years took place, in their own homes in March 2010. The Omnibus survey response rate for completed interviews was 58% (1049) of 1823 eligible. Of the remainder, 31% (557) refused to participate and 9% (173) were not contactable during the interview period. For a further 2% (44), eligibility for inclusion was unknown.
This gave 1049 achieved interviews overall (adults of all ages). Although ONS does not collect information about non-responders, the sociodemographic characteristics of the sample were similar to those from mid-year population estimates for Great Britain (estimated from the 2001 census).
Measures
Well-being was measured by an unprompted open-ended survey question on perception of well-being (see Box 1). The open question was followed by common single-item survey questions: a 5-point Likert self-rating scale item of well-being overall, followed by mental well-being. In order to examine intercorrelations and overlap between indicators, additional items related to well-being were included (on the basis of literature equating well-being with these): self-ratings of life satisfaction, happiness and overall QoL; self-reported health status compared with others of the same age; physical functioning; reported long-standing illness, disability or infirmity and which limits activities; anxiety, nerves and depression; social participation and support28,42,43 and standard Omnibus Survey sociodemographic and socio-economic characteristics and classifications.
BOX 1.
Questionnaire items
| Please tell me, what does the term ‘well-being’ mean to you? You can mention as many things as you like including mental or psychological and/or physical health issues, social relationships and activities and anything else you think of. There are no right or wrong answers. Overall, would you say your own well-being was |
| [5-point response scale: very good–very bad] |
| Please rate your mental well-being, would you say your mental well-being was |
| [5-point response scale: very good–very bad] |
| In general, how satisfied are you with your life as a whole these days? |
| Please rate your satisfaction on a scale of 1-10, with 1 being low and 10 being high. |
| All things considered, how happy would you say you are |
| [4-point response scale: not at all happy–very happy] |
| Thinking about both the good and the bad things that make up your QoL, how would you rate the quality of your life as a whole? |
| [5-point response scale: very good–very bad] |
Responses were recorded verbatim. A thematic coding frame was designed by AB after reading all the transcripts, and the coding was then carried out by Corinne Ward, independently checked by AB.
Statistical methods
The main dependent variables of interest were self-rated well-being overall and mental well-being (both ranked very good, good, alright, bad and very bad). These were expressed as a ranked categorical variable. Univariate analyses were conducted to test associations between self-rated well-being overall and also mental well-being, with sociodemographic characteristics and social circumstances. Chi-square tests, means, independent samples t-tests, mixed design analysis of variance and Spearman’s rank order correlations were used.
Independent associations with self-rated well-being and mental well-being were examined using classic logistic regression, with a binary dependent variable. The ranked categorical variables were dichotomized as ‘good’ (very good combined with good responses) 1 versus ‘not good’ (alright, bad, very bad responses) (0). The referent was 1. No correlation between the entered independent variables exceeded r = 0.550, and all satisfied the lower 0.70 univariate threshold for entry into a multivariable model. Those variables that were statistically significant in the initial full models were re-entered into reduced models, excluding non-significant items apart from age and sex in order to adjust for them. Both full and reduced models are shown.
Results
Characteristics of respondents
Table 1 shows that over half the sample comprised women; the mean age of women was 48.90 years and for men was 49.21 years. The majority were white, as would be expected in a random sample of the national population. Just over a third (36%) were in managerial/professional socio-economic categories. Table 1 shows the means and distributions by sex and by age.
Table 1.
Well-being survey: characteristics of responders, and by sex and age
| % (n) | |
| Age (years) | |
| 16–17 | 1 (15) |
| 18–19 | 1 (10) |
| 20–24 | 6 (63) |
| 25–29 | 6 (60) |
| 30–34 | 8 (81) |
| 35–39 | 9 (90) |
| 40–44 | 8 (88) |
| 45–49 | 8 (86) |
| 50–54 | 9 (92) |
| 55–64 | 18 (187) |
| 65–74 | 17 (171) |
| 75+ | 10 (106) |
| Total | 1049 |
| Mean ages by sex (SD) | |
| Female 48.90 (17.824) | |
| Male 49.21 (17.722) | |
| Two-tailed t-test: −0.281; P = 0.772 ns | |
| Sex | |
| Male | 44 (457) |
| Female | 56 (592) |
| Total | 1049 |
| Married/cohabiting | 55 (578) |
| Single | 20 (209) |
| Widowed | 12 (122) |
| Divorced/separated | 13 (136) |
| Same sex cohabitee | — (2) |
| Former/separated civil partner | — (2) |
| Total | 1049 |
| Married/cohabiting | |
| Female 62% (354) | |
| Male 69% (328) | |
| Chi-square 36.096, 6 df, P = 0.001 | |
| Age (years) | |
| 16–44 54% (231) | |
| 45–64 80% (316) | |
| 65+ 60% (136) | |
| Chi-square 340.036, 12 df, P = 0.001 | |
| Household size (adults and children) | |
| 1 | 28 (295) |
| 2 | 38 (396) |
| 3 | 15 (163) |
| 4 | 13 (137) |
| 5+ | 6 (58) |
| Total | 1049 |
| Mean (SD) | |
| Female 2.69 (1.345) | |
| Male 2.77 (1.366) | |
| Two-tailed t-test: −0.946; P = 0.207 ns | |
| Age (years) | |
| <65 3.00 (1.377) | |
| 65+ 1.74 (0.611) | |
| Two-tailed t-test: 13.338; P = 0.001 | |
| Number of adults in household (16+) | |
| 1 | 34 (352) |
| 2 | 52 (551) |
| 3 | 9 (92) |
| 4+ | 5 (54) |
| Total | 1049 |
| Mean (SD) | |
| Female 2.16 (0.949) | |
| Male 2.33 (1.036) | |
| Two-tailed t-test: 2.741; P = 0.012 | |
| Age (years) | |
| <65 2.38 (1.035) | |
| 65+ 1.73 (0.583) | |
| Two-tailed t-test: 9.003; P = 0.001 | |
| Housing tenure | |
| Owns outright | 35 (362) |
| Owns on mortgage | 34 (353) |
| Rents local authority/housing association | 18 (190) |
| Rents privately | 13 (141) |
| Total | 1049 |
| Rents LA/HA/privately | |
| Female 30% (169) | |
| Male 29% (136) | |
| Chi-square 3.621, 3 df, P = 0.305 ns | |
| Age (years) | |
| 16–44 32% (178) | |
| 45–64 18% (75) | |
| 65+ 23% (52) | |
| Chi-square 293.000, 6 df, P = 0.001 | |
| Car/van available for use in household | |
| Yes | 77 (809) |
| No | 23 (240) |
| Total | 1049 |
| Female 79% (450) | |
| Male 88% (419) | |
| Chi-square 15.384, 1 df, P = 0.001 | |
| Age (years) | |
| 16–44 84% (358) | |
| 45–64 88% (349) | |
| 65+ 72% (162) | |
| Chi-square 26.594, 2 df, P = 0.001 | |
| Done paid work in last 7 days as employee or self-employed | |
| Yes | 54 (563) |
| No | 46 (485) |
| Total | 1048 |
| Yes | |
| Female 49% (278) | |
| Male 60% (285) | |
| Chi-square 13.279, 1 df, P = 0.001 | |
| Age (years) | |
| 16–44 67% (288) | |
| 45–64 65% (256) | |
| 65+ 19% (8) | |
| Chi-square 236.897, 2 df, P = 0.001 | |
| NS-SEC five categories | |
| Managerial/professional occupations | 36 (378) |
| Intermediate occupations | 13 (139) |
| Small employers and own account workers | 7 (77) |
| Lower supervisory and technical occupations | 8 (85) |
| Semi-routine and routine occupations | 28 (291) |
| Not classified | 8 (79) |
| Total | 1049 |
| Managerial/professional | |
| Female 31% (178) | |
| Male 40% (190) | |
| Chi-square 66.972, 5 df, P = 0.001 | |
| Age (years) | |
| 16–44 31% (134) | |
| 45–64 40% (158) | |
| 65+ 34% (76) | |
| Chi-square 78.101, 10 df, P = 0.001 | |
| Highest level of education | |
| Degree or equivalent | 19 (198) |
| Below degree level | 44 (463) |
| Other | 14 (149) |
| None (no qualifications) | 23 (239) |
| Total | 1049 |
| No qualifications | |
| Female 23% (132) | |
| Male 18% (87) | |
| Chi-square 5.264, 3 df, P = 0.153 ns | |
| Age (years) | |
| 16–44 11% (47) | |
| 45–64 18% (73) | |
| 65+ 44% (99) | |
| Chi-square 121.928, 6 df, P = 0.001 | |
| Annual gross income | |
| Up to £8319 | 28 (243) |
| £8320–£14 559 | 24 (210) |
| £14 560–£23 399 | 20 (175) |
| ≥£23 400 | 29 (250) |
| Total | 878 |
| Mean (SD) | |
| Female 17.3477 (8.159) | |
| Male 23.456 (9.514) | |
| Two-tailed t-test: −10.240; P = 0.0001 | |
| Age (years) | |
| <65 21.214 (9.659) | |
| 65+ 16.395 (6.738) | |
| Two-tailed t-test: 6.431; P = 0.001 | |
| Ethnicity | |
| White British | 89 (931) |
| White other | 5 (51) |
| Other | 6 (66) |
| Total | 1048 |
| Region | |
| North East | 4 (48) |
| North West | 13 (137) |
| Yorkshire and Humber | 10 (102) |
| East Midlands | 9 (94) |
| West Midlands | 10 (102) |
| East of England | 8 (81) |
| London | 9 (91) |
| South East | 14 (152) |
| South West | 9 (100) |
| Wales | 6 (58) |
| Scotland | 8 6(83) |
| Total | 1049 |
| Number of respondents | |
ns, not statistically significant at least at the 0.05 level. Due to sample weighting numbers do not necessarily = 100%, t-tests were for independent samples, two-tailed tests; t-tests could only be performed on ranked or continuous variables (and with age dichotomized); for other variables, chi-square tests were performed and on three-category age groups.
Perceptions of well-being and how it can be improved
Open-coded responses to the first question on perceptions of well-being are shown in Table 2. The most common response related to being in good health (67% = 705), followed by life satisfaction (21% = 220), positive outlook (19% = 20), financial security (19% = 201) and mental functioning (13% = 133). There were few associations with age, sex or income.
TABLE 2.
What does the term ‘well-being’ mean to you?
| Having/being in good health/physical functioning, physically fit, strong, having energy, feeling well, retaining senses—sight, hearing and not being bed bound | 67 (705) |
| Life satisfaction, enjoyment, enjoying life, happiness and being happy not depressed | 21 (20) |
| Positive thinking, outlook/good/attitude to life/state of mind, keeping sense of humour, staying focused, not worrying, self-confidence, less stress, get up and do it, think positive, have a purpose in life, taking on challenges and being in control | 19 (20) |
| Financial security, independence, adequate/sufficient income/pension (including for food, bills and transport) and no money worries/problems | 19 (201) |
You can mention as many things as you like including mental or psychological and/or physical health issues, social relationships and activities and anything else you think of. There are no right or wrong answers.
Fewer people aged 65+ years defined well-being in terms of life satisfaction (10% = 22 compared with 22% = 85 of those aged 45–64 years and 26% = 113 of those aged 16–44 years; chi-square 24.683, 2 d.f., P = 0.001). However, people aged 65+ years were more likely than younger people to define well-being as being able to continue to do the things they had always done: 14% = 31 compared with 6% = 22 of people aged 45–64 years and 4% = 18 of those aged 16–44 years (chi-square 24.815, 4 d.f., P = 0.001).
More of those on higher than lower incomes mentioned positive thinking: 26% = 64 of those earning £23 400+ mentioned this compared with 23% = 40 of those earning £14 560–£23 399, 14% = 29 of those on £8320–£14 559 and 17% = 42 of those earning less than this (chi-square 11.971, 3 d.f., P = 0.007). They were also more likely to mention financial security than those on lower incomes: 30% = 30 compared with 17 = 30, 16% = 34 and 14% = 35, respectively (chi-square 26.713, 6 d.f., P = 0.001).
The main responses are shown in Table 2. Supplementary Table 1 (available at Family Practice online) shows the full responses. The most common response to the next open-ended question on how the well-being of older people can be improved, related to having better access to services (28% = 298), followed by more social support (22% = 233), more social activities (17% = 179) and having more money (14% = 146) (see supplementary Table 2, available at Family Practice online).
Respondents on higher incomes of ≥£23 400 were more likely to mention having more money (23% = 57) compared with those on £14 560–£23 399 (10% = 18) and £8320–£14 559 (14% = 30) and those on less than this (£11% = 27) (chi-square 19.912, 3 d.f., P = 0.001). Women were more likely than men to mention more social activities (21% = 117 versus 13% = 62; chi-square 10.313, 1 d.f., P = 0.001). Younger people, aged 16–44 years, were more likely to mention more social support (26% = 10 compared with 24% = 93 of those aged 45–64 years and 14% = 32 of those aged 65+ years; chi-square 11.448, 2 d.f., P = 0.003).
In addition, respondents were asked a structured question how older people could be helped to remain in their own homes, given the importance of this to people.29 Table 3 shows that the most common response given was provision of help with personal care needs, followed by help with household tasks, nursing care, visitors to check they are alright or to prevent loneliness and help with home repairs. They were also asked an open-ended question about anything else that could help them. Home adaptations were most commonly mentioned.
TABLE 3.
Population views of how older people can be helped to remain at homea
| % (n) | |
| Help with personal care needs | 58 (613) |
| Help with household tasks | 57 (598) |
| Help with nursing care needs | 44 (462) |
| Visitors to check people are alright at home | 42 (438) |
| Visitors for social contact and to prevent loneliness | 37 (385) |
| Help with household repairs/maintenance | 32 (333) |
| Support to get out of the house | 30 (317) |
| Number of respondents | 1049 |
Totals do not equal 100% as respondents could mention more than one theme; each theme coded once per respondent.
Additional areas people mentioned (open-ended) here were financial help and support/grants (6%/66); more carers/community and nursing care/24-hour support at home (5%/55), family support (4%/45), home adaptations/equipment (4%/45), medical care (2%/19); emergency care/buzzers/alarms (2%/17); mobile shops/internet access for shopping (1%/5).
Self-assessed well-being and correlates
Most respondents rated their well-being, mental well-being, happiness, life satisfaction and QoL positively: 78% (802) rated their well-being overall as very good or good, as did 80% (826) in relation to their mental well-being; 66% (679) rated their life satisfaction on the top three points of a 1–10 scale (indicating high life satisfaction); 46% (472) rated themselves as very happy and 79% (826) rated their QoL as a whole as very good or good. The detailed responses, health and social circumstances and means for age and sex are shown in supplementary Table 3 (available at Family Practice online).
As would be expected, there were differences in mean health and functioning by age and sex, with women and older people having worse scores. Women were more likely to have undertaken exercise activities, and younger people were most likely to have gone to a cinema etc., while people in middle age groups were least likely to have gone to clubs. While there was no sex difference with available help with practical chores, men were more likely than women to have someone available for comfort, as were younger people. Older people were more likely to have available practical help, perhaps reflecting their greater needs. Consistent with this, as would be expected, they were more likely to report a long-standing illness and, as were women, difficulties with physical functioning. As expected, women were also most likely to report anxiety/nerves/depression. There were no age or sex differences in ratings of future chances of going into care (asked of people aged 65+ years only).
Supplementary Table 4 (available at Family Practice online) shows means for the indicators of well-being by age and sex. Mixed design analysis of variance showed that there were no significant differences (F1,121 not significant 0.339).
The intercorrelations (Spearman’s rho) between related concepts were all highly statistically significant, with moderately high correlations: self-rated well-being, self-rated mental well-being, life satisfaction rating, happiness and QoL. No correlation was >0.663, confirming that these indicators are related but do not completely overlap, retaining their conceptual distinctions (Table 4).
TABLE 4.
Spearman’s rank correlations between indicators of well-being
| Self-rated well-being overall | Self-rated mental well-being | Life satisfaction rating | Happy rating | Self-rated quality of life | |
| Self-rated well-being overall | — | 0.663** | −0.565** | 0.485** | 0.580** |
| Self-rated mental well-being | 0.663** | — | −0.501** | 0.457** | 0.488** |
| Life satisfaction rating | −0.565** | −0.501** | — | −0.639** | −0.636** |
| Happy rating | 0.485** | 0.457** | −0.639** | — | 0.579** |
| Self-rated QoL | 0.580** | 0.488** | −0.636** | 0.579** | — |
P < 0.05; ** P < 0.01 inverse correlations reflect different directions of coding.
Health, functioning, social participation and support, assessed chances of entering care, household size and indicators of socio-economic status (SES) were all significantly correlated with self-rated well-being overall and mental well-being (supplementary Table 5 is available at Family Practice online). Age and sex were not (and see earlier).
Significant independent variables were entered into a multivariable analyses for well-being and mental well-being, adjusting for age, sex, household size and indicators of SES. None of the sociodemographic or economic indicators achieved significance for overall or mental well-being.
The full model for overall well-being (see Table 5, Exp B) shows that those who ranked their health more negatively, who had difficulty with mobility and problems with anxiety, nerves and depression had significantly reduced odds of rating their well-being as good rather than not good. Those with no reported long-standing illness had almost four times the odds of those with long-standing illness of good rather than not good, overall well-being. Those who had more people available for comfort and support had increased odds of good rather than not good well-being.
Table 5.
Adjusted a logistic regression showing independent associations [odds ratios (OR), 95% confidence intervals (CI)] with predictors of self-rated well-being and self-rated mental well-being
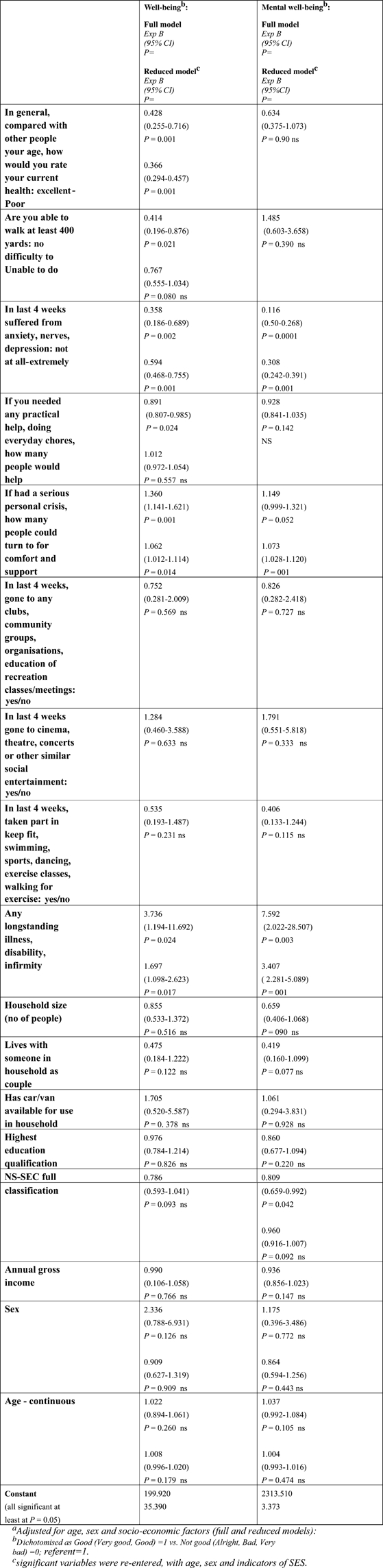 |
Health status, long-standing illness, anxiety, nerves, depression and number of available supporters retained significance when entered into the reduced model. People with less than good health status had less than half the odds of those with good health of rating their overall well-being as good rather than not good. Those who reported no long-standing illness had almost twice the odds of those with a long-standing illness, of good, rather than not good, overall well-being. Those reporting anxiety, nerves and depression were about half as likely as those without these symptoms to report their well-being as good rather than not good. Number of people available for practical support did not retain significance, while the odds of good versus not good well-being were multiplied by 1.002 for each additional available person for comfort and support.
The table also shows the models for mental well-being. Again, those with no problems with anxiety, nerves or depression had significantly reduced odds of rating their mental well-being as good rather than not good in the full and reduced models. Those who reported no long-standing illness had over seven times the odds of good rather than not good, mental well-being in the full model, and over three times the odds in the reduced model (but there were no significant associations with health status and mobility). Number of available practical helpers was not significant in the full model. As number of available supporters just missed significance at the 0.05 level in the full model, it was included in the reduced model, where it was highly significant. The odds of good versus not good mental well-being were multiplied by 1.073 for each additional available person for comfort and support.
Discussion
Current health policy aims to promote well-being and mental well-being in populations, including among older people. A systematic review of interventions to promote mental well-being in older age concluded that most evidence supported exercise, followed by psychological interventions, although definitive research is still needed.41 There is some conceptual confusion in the policy and academic literature with interchangeable use of concepts, including well-being, life satisfaction, happiness and QoL. None of the correlations between these variables exceeded r = 0.663, confirming that these indicators are related but do not completely overlap, retaining their conceptual distinctiveness. Thus, care needs to be taken when defining variables of interest and their outcome indicators.
The strength of this study was that it was a national population survey of adults aged >16 years. The weakness was the response rate of 58%, although response rates of <60% are increasingly usual for population surveys. However, the data were weighted by ONS, based on population estimates derived from the last census, to compensate for any response bias. In this study, most men and women, in all age groups, rated their well-being and mental well-being positively. The study findings were consistent with Waddell and Jacobs–Lawson’s analyses:25 sociodemographic and economic variables had no significant impact on well-being or mental well-being when considered in multivariable models. Self-rated health, mental health symptoms, long-standing illness and social support were the main drivers of overall well-being. Mental health symptoms, long-standing illness and social support were the main drivers of mental well-being.
People perceived well-being differently, depending on their age and level of income. People on higher incomes were more likely to mention the need for positive thinking and financial security for achieving well-being; those on lower incomes being least likely to mention these. Thus, having more money appeared to make people value it more. This is consistent with earlier research on people’s perceptions of influences on QoL, where those in the higher income groups were more likely than those on lower incomes to mention having adequate finances.14
People aged 65+ years were more likely than younger people to define well-being as being able to continue to do the things they had always done and less likely to mention life satisfaction. Understanding the drivers of well-being among adults, including older adults, is of high policy importance. Greater understanding means that policy can be better informed and guided about what to target in order to promote it. These analyses suggest that attention should be focused, not only on improvements in population health and functioning, and access to services, but on encouraging people to develop and maintain their social support networks and engagement in social activities. This is supported by respondents’ emphasis on the need for visitors to check they are alright or to prevent loneliness, as one of the ways of enabling people to remain living at home rather than care homes. The promotion of mental and physical health is directly relevant to clinical practice. The important of informing the public about the wider benefits of maintaining social support and participation is a health promotion message that public policy needs to place greater emphasis on. However, large scale randomized trials are still required to support the most cost-effective interventions.
Supplementary material
Supplementary Tables 1–5 are available at Family Practice online.
Declaration
Funding: self-funded.
Ethical approval: Office for National Statistics Omnibus Survey Ethics Committee.
Conflict of interest: none.
Acknowledgments
Thanks are due to ONS Omnibus Survey staff for mounting the module and processing the data. Material from the ONS Omnibus Survey, made available through ONS, has been used with the permission of the Controller of The Stationery Office. We also thank members of the study advisory group and Ms Corinne Ward for her coding. Members of ONS Omnibus Survey who carried out the original analysis and collection of the data hold no responsibility for the further analysis and interpretation of them.
References
- 1.Baltes PB, Baltes MM, editors. Successful Aging. Perspectives from the Behavioral Sciences. New York, NY: Cambridge University Press; 1990a. [Google Scholar]
- 2.Ryff C. Psychology and aging. In: Hazzard W, Blass J, Ettinger W, Halter J, Ouslander J, editors. Principles of Geriatric Medicine and Gerontology4nd edn. New York: McGraw-Hill; 1999. [Google Scholar]
- 3.World Health Organization. Constitution of the World Health Organization. Geneva, Switzerland: World Health Organization; 1947. [Google Scholar]
- 4.Diener E, Lucas RE. Subjective emotional well being. In: Lewis M, Haviland JM, editors. Handbook of Emotions, 2nd edn. New York, NY: Guilford; 2000. [Google Scholar]
- 5.Andrews FM. Social indicators of perceived life quality. Soc Indic Res. 1974;1:279–99. [Google Scholar]
- 6.Andrews FM, Withey SB. Social Indicators of Well-Being: American’s Perceptions of Life Quality. New York, NY: Plenum Press; 1976. [Google Scholar]
- 7.Bowling A, Windsor J. Towards the good life. A population survey of dimensions of quality of life. J Happiness Stud. 2001;2:55–81. [Google Scholar]
- 8.Bowling A, Gabriel Z. An integrational model of quality of life in older age. A comparison of analytic and lay models of quality of life. Soc Indic Res. 2004;69:1–36. [Google Scholar]
- 9.Veenhoven R. Is happiness relative? Soc Indic Res. 1991;24:1–34. [Google Scholar]
- 10.Heylighten F, Bernheim J. Global progress I: empirical evidence for ongoing increase in quality of life. J Happiness Stud. 2000;I:323–49. [Google Scholar]
- 11.James O. Affluenza. London, UK: Vermillion; 2007. [Google Scholar]
- 12.Ereant G, Whiting R. Research report DCSF–RWO 73. London, UK: Department of Children, Schools and Families; 2008. What do we mean by wellbeing? And why does it matter? Linguistic landscapes. [Google Scholar]
- 13.Huppert FA. Mental Capital and Well-Being: Making the Most of Ourselves in the 21st Century. State-of-Science Review. Psychological Well-Being: Evidence Regarding its Causes and Consequences. SR-X2. London, UK: Government Office for Science Foresight project, 2008. [Google Scholar]
- 14.Bowling A, Gabriel Z, Dykes J, et al. Let’s ask them: a national survey of definitions of quality of life and its enhancement among people aged 65 and over. Int J Aging Hum Dev. 2003;56:269–306. doi: 10.2190/BF8G-5J8L-YTRF-6404. [DOI] [PubMed] [Google Scholar]
- 15.Bowling A, Dieppe P. What is successful ageing and who should define it? Br Med J. 2005;331:1548–51. doi: 10.1136/bmj.331.7531.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowling A. Perceptions of active ageing in Britain: divergences between minority ethnic and whole population samples. Age Ageing. 2009;38:703–10. doi: 10.1093/ageing/afp175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryff CD. In the eye of the beholder: views of psychological well-being among middle-aged and older adults. Psychol Aging. 1989;4:195–210. doi: 10.1037//0882-7974.4.2.195. [DOI] [PubMed] [Google Scholar]
- 18.National Institute for Health and Clinical Excellence. Mental Wellbeing and Older People. Guidance for Occupational Therapy Activity Interventions to Improve the Mental Wellbeing of Older People. London, NICE Public Health Guidance 16. London, UK: NICE; 2008. [Google Scholar]
- 19.Department of Health. Confident Communities, Brighter Futures. A Framework for Developing Well-Being. London, UK: New Horizons, Department of Health; 2010. [Google Scholar]
- 20.NHS Scotland. Mental Health Improvement Programme, Background and Policy Context. NHS Scotland; 2006. www.wellscotland.info/mentalhealth/national-programme.html. Updated 2010 (accessed on 15 April 2010) [Google Scholar]
- 21.Noll HH. Social indicators and quality of life research. Background, achievements and current trends. In: Genov N, editor. Advances in Sociological Knowledge Over Half a Century. Wiesbaden, Germany: VS Verlag für Sozialwissenschaften; 2004. pp. 151–81. [Google Scholar]
- 22.Lampinen P, Heikkinen RL, Kauppinen M, Heikkinen E. Activity as a predictor of mental well-being among older adults. Aging Ment Health. 2006;10:454–66. doi: 10.1080/13607860600640962. [DOI] [PubMed] [Google Scholar]
- 23.Carmel S, Bernstein JH. Gender differences in physical health and psychosocial well being among four age-groups of elderly people in Israel. Int J Aging Hum Dev. 2003;56:113–31. doi: 10.2190/87YH-45QN-48TY-9HN8. [DOI] [PubMed] [Google Scholar]
- 24.Stone AA, Schwartza JE, Brodericka JE, Deaton A. A Snapshot of the Age Distribution of Psychological Well-being in the United States. National Academy of Sciences, USA; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Waddell EL, Jacobs-Lawson JM. Predicting positive well-being in older men and women. Int J Aging Hum Dev. 2010;70:181–97. doi: 10.2190/AG.70.3.a. [DOI] [PubMed] [Google Scholar]
- 26.Warr P, Butcher V, Robertson I, Callinan M. Older people’s well-being as a function of employment, retirement, environmental characteristics, and role preference. Br J Psychol. 2004;95:297–324. doi: 10.1348/0007126041528095. [DOI] [PubMed] [Google Scholar]
- 27.Li LW, Lang J. Social exchanges and subjective well-being among older Chinese: does age make a difference? Psychol Aging. 2007;22:386–91. doi: 10.1037/0882-7974.22.2.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bowling A. Ageing Well. Quality of Life in Old Age. Maidenhead, UK: Open University Press; 2005. [Google Scholar]
- 29.Victor C, Scambler S, Bond B, Bowling A. Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol. 2000;10:407–17. [Google Scholar]
- 30.Victor C, Scambler S, Bond J, Bowling A. The prevalence of, and risk factors for, loneliness in later life. Ageing Soc. 2005;25:357–76. [Google Scholar]
- 31.Allen J. Older People and Well-Being. London, UK: Institute for Policy Studies; 2008. [Google Scholar]
- 32.Bowling A, Banister D, Sutton S, Evans O, Windsor J. A multidimensional model of the quality of life in older age. Aging Ment Health. 2002;6:355–71. doi: 10.1080/1360786021000006983. [DOI] [PubMed] [Google Scholar]
- 33.Lepeleire J, Iliffe S, Mann E, Degryse JM. Frailty: an emerging concept for general practice. Br J Gen Pract. 2009;59:e177–82. doi: 10.3399/bjgp09X420653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Age Concern England and Help the Aged. One Voice. Shaping Our Ageing Society. London, UK: Age Concern England and Help the Aged; 2009. [citing Principal Population Projections, 2006 base, Government Actuary Department] [Google Scholar]
- 35.Bowling A, Browne P. Social networks, health and emotional well-being among the oldest old living in London. J Gerontol. 1991;46:S20–32. doi: 10.1093/geronj/46.1.s20. [DOI] [PubMed] [Google Scholar]
- 36.Bowling A, Farquhar M. The health and well-being of Jewish people aged 65 to 85 years living at home in the East End of London. Aging Soc. 1993;13:213–44. [Google Scholar]
- 37.Bowling A, Farquhar M, Grundy E, Formby J. Psychiatric morbidity among people aged 85+ in 1987. A follow-up study at two and a half years: associations with changes in psychiatric morbidity. Int J Geriatr Psychiatry. 1992;5:307–21. [Google Scholar]
- 38.Bowling A, Farquhar M, Grundy E, Formby J. Changes in life satisfaction over a two and a half year period among very elderly people living in London. Soc Sci Med. 1993;36:641–55. doi: 10.1016/0277-9536(93)90061-8. [DOI] [PubMed] [Google Scholar]
- 39.Bowling A. Social networks and social support among older people and implications for emotional well-being and psychiatric morbidity. Int Rev Psychiatry. 1994;9:447–59. [Google Scholar]
- 40.Burns T, Knapp M, Catty J, et al. Home treatment for mental health problems: a systematic review. Health Technol Assess. 2001;5:15. doi: 10.3310/hta5150. [DOI] [PubMed] [Google Scholar]
- 41.Windle G, Hughes D, Linck P, et al. Public Health Interventions to Promote Mental Well-Being in People Aged 65 and Over: Systematic Review of Effectiveness and Cost-Effectiveness. Bangor, UK: University of Wales; 2007. [Google Scholar]
- 42.Bowling A. Research Methods in Health. Investigating Health and Health Services. 3rd edn. Maidenhead, UK: Open University Press; 2009. [Google Scholar]
- 43.Bowling A. Just one question: if one question works why ask several? Editorial. J Epidemiol Community Health. 2005;59:342–5. doi: 10.1136/jech.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


