Description
Intracardiac tumours move both with breathing and with the cardiac cycle; they therefore pose unique problems for radiotherapy delivery. Conventional radiotherapy must encompass the tumour with a margin to account for this motion, and the prescription is limited by myocardial radiation tolerance. The greater accuracy of radiosurgery allows higher radiation-dose deposition, with relative myocardial sparing.
A 67-year-old male underwent surgical resection of a right-ventricular metastatic adenocarcinoma in March 2009, followed by postoperative conventional radiotherapy close to myocardial tolerance (40 Gy in 20 fractions). Six months later the tumour regrew, obstructing the ventricle and leading to heart failure, with a prognosis of days. Further surgery was not possible. He was treated with fractionated radiosurgery (25 Gy in five fractions) using the CyberKnife system (Accuray, Sunnyvale, California, USA) (figure 1).
Figure 1.

Picture of the CyberKnife system components. A compact linear accelerator is mounted on a six-joint robotic arm, which can move freely around the patient. Two kilovoltage x-ray sources are positioned orthogonally for near ‘real-time’ target imaging. The infrared Synchrony camera can monitor chest-wall movement via light-emitting diodes placed on the patient's chest.
Implanted pericardial fiducial markers allowed near real-time x-ray monitoring of the tumour and heart position with breathing. The integrated Synchrony system correlated fiducial position with real-time monitoring of chest-wall movement, enabling the radiation beam to track the moving tumour continuously. Cardiac cycle motion was accounted for by outlining the tumour position on three different phases of a cardiac-gated CT scan, fused with the radiotherapy planning CT (figure 2).
Figure 2.
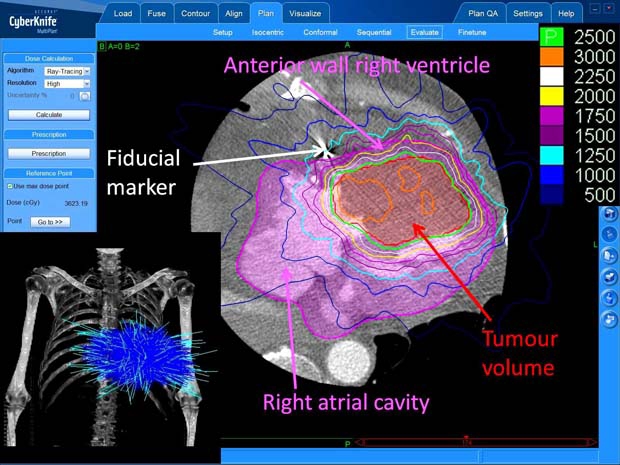
Axial slice from cardiac-gated CT scan used to assist treatment planning. The tumour volume is shown in red overlay, and whole heart volume in pink overlay. The radiation isodose arrangement is superimposed, with the isodose key shown top right (doses are in centigray, where 100 centigray=1 gray (Gy)). The radiotherapy beam arrangement is shown on the skeleton view (bottom left). One hundred and ninety eight individual beams of radiation (light blue) converge on the target to give the optimum dose distribution.
Echocardiography showed a 27% reduction in cross-sectional tumour area at 1 week following treatment, and cardiac function improved with symptomatic improvement. The patient died 6 months after treatment. The case demonstrates that radiosurgery is a feasible and effective treatment for intracardiac tumours, either with (as in this case) or without previous radiotherapy.
Footnotes
Competing interests Dr Martin and Dr Plowman have received honoraria from Accuray, Sunnyvale, California, USA, for educational presentations related to the use of CyberKnife.
Patient consent Obtained.


