Abstract
The patient in this case report had two severe medical conditions that require oppositional treatment: prolactinoma and psychosis. A prolactinoma is a benign tumour of the pituitary gland that produces prolactin. Dopamine agonist medication is the first-line treatment in patients with prolactinoma. The psychotic symptoms started after a dosage increase of a dopamine D2-receptor agonist. Several antipsychotic medications were tried with and without the dopamine D2-receptor agonist, but severe command hallucinations remained. Cognitive behavioural therapy (CBT) was added which reduced the impact of the hallucinations to a great extent, indicating that CBT can have an additional positive effect in prolactinoma patients with psychosis that shows incomplete recovery after antipsychotic medication. Future research should be aimed at the severe and prolonged side effects of dopamine agonists in the treatment of prolactinoma patients with multiple risk factors for a psychotic decompensation.
Background
A prolactinoma is a benign tumour of the pituitary gland that produces prolactin. In men, the most common symptoms of hyperprolactinaemia are decreased libido, erectile dysfunction and infertility. In addition, macroprolactinomas by their very size may press on surrounding structures causing headaches or loss of vision (bitemporal hemianopsia) from pressure on the cross-over of the optic nerves. Dopamine normally inhibits prolactin secretion, so first-line treatment of patients with prolactinoma is a dopamine D2-receptor agonist.1 These drugs shrink the tumour and return prolactin levels to normal in approximately 80% of patients. However, standard treatment of prolactinoma increases dopaminergic activity and has the potential to exacerbate psychotic symptoms. Psychosis is associated with increased dopamine activity and is treated mainly with antipsychotic drugs that block dopamine D2 receptors. Thus, prolactinoma and psychosis require treatments that oppose each other.2
In some patients with prolactinoma and psychosis, it is difficult to achieve optimal balance between dopamine agonists and antagonists. In the present case report, we describe a psychotic patient with an inoperable prolactinoma who was treated with several antipsychotic agents without the desired effect on his debilitating auditory hallucinations. However, he did respond to additional cognitive behavioural therapy (CBT). This case report is the first to describe the option of additional CBT in the treatment of patients with prolactinoma and psychosis. Furthermore, the symptoms of this patient may provide some insight into the mechanisms underlying recurrent psychosis. Sensitisation may cause the enhancement or intensification of a specific response to a drug following prior exposure to the same (or functionally similar) drug. This patient used cannabis for a long period before his first psychotic symptoms appeared. Systemic administration of the psychoactive ingredient in cannabis, Δ-9-tetrahydrocannabinol, increases firing of dopaminergic neurons in the midbrain.3 4 In our patient, the dopamine agonist medication may have triggered an already sensitised dopamine system leading to recurrent psychosis.
Case presentation
A 33-year-old man was referred in 2008 to the Department of Early Psychosis of the Academic Medical Center in Amsterdam, the Netherlands. Four years earlier, a prolactinoma had been discovered (macroprolactinoma 4×5 cm). Quinagolide (a dopamine agonist) was started to lessen tumour growth, but liquor leakage developed due to destruction of the skull base by the prolactinoma and shrinkage of the prolactinoma. This was complicated by meningitis in 2005. Before the patient became ill he had been a computer programmer and had lived alone. He stopped working in 2006. He had used cannabis from before age 15 until age 32 (2007) on a daily basis. After a tumour debulking operation was performed in January 2007, quinagolide was restarted and slowly increased from 18.75 mg to 112.5 mg per day without liquor leakage. However, in March 2008 when the dose was increased to 112.5 mg, severe psychotic symptoms emerged for the first time. The patient heard voices that ordered him not to shower, not to get off the couch, etc. If he did not listen, they administered a stinging pain, after which he immediately obeyed their commands. In 2008 he started living with his mother because the voices ordered him not to go to his own house. Two months later he was admitted involuntarily to a psychiatric ward because he had threatened his mother and his nieces and nephews with a knife.
Investigations
A structural MRI scan showed a large prolactinoma (figure 1).
Figure 1.

MRI scan showing the large prolactinoma.
Differential diagnosis
-
▶
Schizophrenia
-
▶
Substance-induced psychotic disorder.
Treatment
In May 2008, quinagolide was stopped for 6 weeks with little effect on the severity of hallucinations but with modest effect on persecutory delusions. Nonetheless, due to rising prolactin levels, quinagolide had to be restarted. The antipsychotic medication aripripazole 15 mg was started but discontinued after 2 months because of lack of effect on the psychotic symptoms. Antipsychotic medication was switched to quetiapine 800 mg and the commanding voices diminished to some extent but remained disturbingly present. The delusional beliefs remitted completely. The time line of (treatment) events and clinical severity of the positive symptoms is depicted in figure 2.
Figure 2.
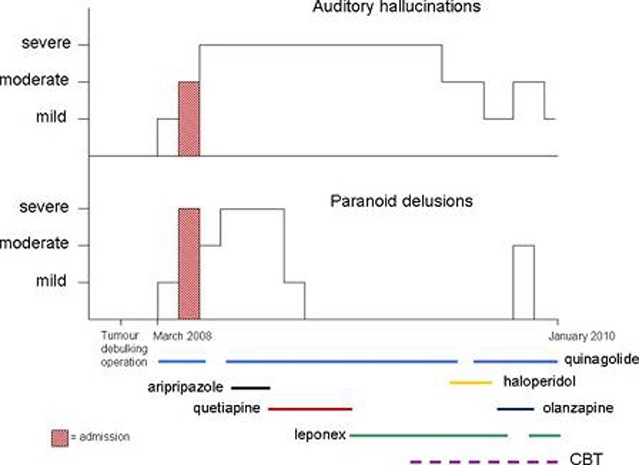
Time line of (treatment) events and clinical severity of positive symptoms.
Because the hallucinations persisted, antipsychotic medication was changed from quetiapine to leponex in February 2009 (up to 400 mg in April 2009, serum level of leponex was 0.50 mg/l). Later haloperidol (1 mg) was added but the voices remained even when the quinagolide was stopped for 4 weeks.
Cognitive therapy was started in May 2009. With command hallucinations, diminishing the power of the voices is important to lessen distress and decrease the likelihood of compliance.5–7 At the start of therapy, the patient rated each of the three voices he was hearing as having 100% control over him, where 0 is no power and 100 is complete power.
The methods of collaborative empiricism and Socratic dialogue were used to engage the patient in questioning, challenging and restructuring his power beliefs. Collaborative empiricism is a cognitive therapy procedure in which the therapist formulates a hypothesis and then helps the patient test the validity of the hypothesis. With Socratic dialogue, guided discovery is used not to change a patient's mind but to allow the patient to explore and reflect on his thoughts and behaviours. Subsequently, we used behavioural tests to help the patient put these beliefs to empirical test. We discussed the fact that reducing the power of the voices involved disobeying the voices and experiencing what would happen. A hierarchy of less to more difficult commands to disobey was constructed. The easiest command was to switch on the light with the hand he wanted to use and the most difficult was to live in his own house. The patient was afraid that the voices would cause him pain if he disobeyed them. In addition, to improve the self-esteem of the patient, competitive memory training (COMET)8 was employed. COMET is a technique that uses imagery of successful moments in life to counterbalance the negative emotions induced by voice content. Improved self-esteem can help the patient find the courage to disobey the voices in behavioural experiments.9
Starting with the least difficult command to disobey, the power of the voices was reduced after a few weeks from 100 to 70. Slowly the patient was able to stay for a few hours in his own house. To establish the lowest effective dose of antipsychotic medication with the least side effects, leponex was reduced to 200 mg and haloperidol was stopped without consequences in October 2009. Later on the patient also discussed professional training options with his job coach. He was able to sleep in his own house when his brother accompanied him. Because the patient insisted on trying one more antipsychotic to relieve him of the voices, medication was switched to olanzapine 10 mg in November 2009.
Meanwhile, the endocrinologist slowly increased quinagolide to 150 mg because his prolactin level was still too high. Psychotic symptoms increased. The patient also started hearing a fourth voice that told him to stop smoking or otherwise the voice would give him a heart attack. With the restart of leponex in December 2009, the additional psychotic symptoms swiftly disappeared but the fourth voice remained. The patient indicated that he did not want to and could not stop smoking and that he experienced intense fear and stress because of this voice. We therefore planned a behavioural experiment to test the credibility of the fourth voice. The patient scored the credibility of the threat at 30 on a scale of 0 (no credibility) to 100 (no doubt). If the patient had a heart attack within a month, this would prove that the voice was able to give the patient a heart attack. If the patient did not have a heart attack, then the voice had no power to do as it claimed. After 2 weeks of smoking and no heart attack, the credibility of the voice was reduced to 20 and after a month to 1. At the end of 15 CBT sessions, the patient was able to stay in his own house alone and to work on his computer programs. The voices continued to be present but the patient was able to disregard their commands. Such an outcome is typical of that reported by Trower et al5: reduced motivation to comply with voices leads to reduced distress and impact, but without changing the fundamental topography of the voices (frequency, content, etc).
Outcome and follow-up
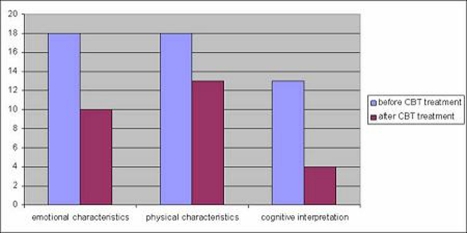
The Psychotic Symptom Rating Scales (PSYRATS)10 was used to assess hallucinations before and after CBT treatment. Haddock et al10 distinguished three factors on the PSYRATS auditory hallucinations rating scale: an emotional characteristics factor (amount and degree of negative content of the voices, amount and intensity of distress), a physical characteristics factor (frequency, duration, location and loudness of the voices) and a cognitive interpretation factor (beliefs about voices, disruption of daily life and control). The scores on all three factors were decreased after treatment, with the strongest decrease in the cognitive interpretation factor score (figure 3).
Figure 3.
Psychotic Symptom Rating Scale auditory hallucinations rating scale factor scores before and after additional cognitive behavioural therapy.
At 6-month follow-up, the patient was still doing well. He was living in his own house and had started his own business writing computer programs. In addition, he was able to lose the weight he had gained as a side effect of the antipsychotic medication and to reduce his smoking habit.
Discussion
The patient in this case report had two severe medical conditions that require oppositional treatment: prolactinoma and psychosis. The psychotic symptoms started after an increase in the dosage of a dopamine D2-receptor agonist. It is not sure whether this medication was the sole cause of the psychotic disorder, since some symptoms were still present after a wash-out period of 6 weeks. However, the symptoms appeared quickly after the dosage of the dopamine D2-receptor agonist was increased and some persecutory beliefs became less severe during wash-out of the agonist. Nonetheless, the commanding auditory hallucinations remained although several antipsychotic medications were tried with adequate dosage and duration.
There have been a few case reports of iatrogenic psychosis in patients treated with dopamine agonist therapies for a prolactinoma.11–13 An increase in dopaminergic activity in the mesolimbic area of the brain due to these medications has been suggested as the aetiology of such cases of psychosis. Several case reports have been published describing patients with a prolactinoma and schizophrenia, delineating the dilemma between treating the prolactinoma and treating the psychosis. Aripripazole has been suggested as the treatment of choice because of its effectiveness in treating the symptoms of schizophrenia while allowing the patient to maintain a normal prolactin level in the presence of a functional prolactinoma without the need for additional medications that could complicate treatment of the patient's psychosis.14 However, in our patient aripripazole was discontinued because of lack of effect on his psychotic symptoms.
We have to take into consideration that (1) the patient started using cannabis before age 15 and continued to use it on a daily basis until age 32 (cannabis abuse before age 15 is a known risk factor for schizophrenia15); (2) the patient had multiple insults to his brain starting with a large prolactinoma extending to his frontal cortex, followed by meningitis and then neurosurgery. The dopamine D2-receptor agonist may have been the tipping point in the dopamine disturbances already present prior to use of this medicine.
The reduced impact of the auditory hallucinations during CBT is supported by the revised dopamine hypothesis of Howes and Kapur.16 They propose that the locus of dopamine dysregulation is primarily at the presynaptic dopaminergic control level and that this dysregulation is the ‘final common pathway’ to psychosis. The abnormal release of dopamine leads to an aberrant assignment of salience to innocuous stimuli. It is argued that psychotic symptoms emerge over time as the individual's own explanation of the experience of aberrant salience. Psychosis is, therefore, aberrant salience driven by dopamine and filtered through the individual's existing cognitive and sociocultural schemas, thus allowing the same chemical (dopamine) to have different clinical manifestations in different cultures and different individuals.16
Learning points.
-
▶
Cognitive behavioural therapy can have an additional positive effect when other treatment options have proven to be insufficient to reduce command hallucinations in patients with a prolactinoma during treatment with a dopamine D2-receptor agonist.
-
▶
Our results support the hypothesis of Howes and Kapur that altering the existing cognitive schemas in a patient with dopamine dysregulation can have beneficial effects on psychosis.
-
▶
Future research should be aimed at the severe and prolonged side effects of dopamine agonists in the treatment of prolactinoma patients with multiple risk factors for a psychotic decompensation.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf) 2006;65:265–73 [DOI] [PubMed] [Google Scholar]
- 2.Konopelska S, Quinkler M, Strasburger CJ, et al. Difficulties in the medical treatment of prolactinoma in a patient with schizophrenia–a case report with a review of the literature. J Clin Psychopharmacol 2008;28:120–2 [DOI] [PubMed] [Google Scholar]
- 3.Diana M, Melis M, Gessa GL. Increase in meso-prefrontal dopaminergic activity after stimulation of CB1 receptors by cannabinoids. Eur J Neurosci 1998;10:2825–30 [DOI] [PubMed] [Google Scholar]
- 4.French ED, Dillon K, Wu X. Cannabinoids excite dopamine neurons in the ventral tegmentum and substantia nigra. Neuroreport 1997;8:649–52 [DOI] [PubMed] [Google Scholar]
- 5.Trower P, Birchwood M, Meaden A, et al. Cognitive therapy for command hallucinations: randomised controlled trial. Br J Psychiatry 2004;184:312–20 [DOI] [PubMed] [Google Scholar]
- 6.Birchwood M, Meaden A, Trower P, et al. The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med 2000;30:337–44 [DOI] [PubMed] [Google Scholar]
- 7.Hacker D, Birchwood M, Tudway J, et al. Acting on voices: Omnipotence, sources of threat, and safety-seeking behaviours. Br J Clin Psychol 2008;47(Pt 2):201–13 [DOI] [PubMed] [Google Scholar]
- 8.Korrelboom K, de Jong M, Huijbrechts I, et al. Competitive memory training (COMET) for treating low self-esteem in patients with eating disorders: A randomized clinical trial. J Consult Clin Psychol 2009;77:974–80 [DOI] [PubMed] [Google Scholar]
- 9.Birchwood M, Gilbert P, Gilbert J, et al. Interpersonal and role-related schema influence the relationship with the dominant ‘voice’ in schizophrenia: a comparison of three models. Psychol Med 2004;34:1571–80 [DOI] [PubMed] [Google Scholar]
- 10.Haddock G, McCarron J, Tarrier N, et al. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med 1999;29:879–89 [DOI] [PubMed] [Google Scholar]
- 11.Al-Semaan YM, Clay HA, Meltzer HY. Clozapine in treatment of bromocriptine-induced psychosis. J Clin Psychopharmacol 1997;17:126–8 [DOI] [PubMed] [Google Scholar]
- 12.Peter SA, Autz A, Jean-Simon ML. Bromocriptine-induced schizophrenia. J Natl Med Assoc 1993;85:700–1 [PMC free article] [PubMed] [Google Scholar]
- 13.Cabeza GA, Flores LF, Iñiguez IE, et al. Acute psychosis secondary to bromocriptine treatment in a patient with a prolactinoma. Rev Invest Clin 1984;36:147–9 [PubMed] [Google Scholar]
- 14.Freeman B, Levy W, Gorman JM. Successful monotherapy treatment with aripiprazole in a patient with schizophrenia and prolactinoma. J Psychiatr Pract 2007;13:120–4 [DOI] [PubMed] [Google Scholar]
- 15.Henquet C, Murray R, Linszen D, et al. The environment and schizophrenia: the role of cannabis use. Schizophr Bull 2005;31:608–12 [DOI] [PubMed] [Google Scholar]
- 16.Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull 2009;35:549–62 [DOI] [PMC free article] [PubMed] [Google Scholar]