Abstract
Non-steroidal anti-inflammatory drug (NSAID)–induced enteropathy, comprising inflammation, ulceration, occult bleeding and subsequent healing with stricture formation in the small bowel, has become an established clinical entity. Recently, reports of similar pathological changes in the colon have led to increasing awareness of, what is termed, NSAID-induced colopathy. The authors here present a case of NSAID-induced colopathy with diaphragm formation in the colon. Diaphragms are thickened mucosal folds which can completely obliterate the bowel lumen. NSAID-induced colopathy can present with iron-deficiency anaemia, abdominal pain, weight loss, blood-positive stools or altered bowel habits, thus mimicking colon cancer. Acute presentation with bowel obstruction and/or perforation can also occur. Management involves withdrawal of the offending NSAID, excluding differential diagnoses such as inflammatory bowel disease and malignancy, and sometimes surgery with resection. With the increased use of coated and slow-release formulations of NSAIDs, increased awareness with regard to this clinical entity is relevant.
Background
We decided to write about this case because we think it is an important lesson to surgeons and clinicians that this benign illness is a relevant differential diagnosis when encountering a patient presenting with classical symptoms of colon cancer or inflammatory bowel disease. Furthermore, this was, to our knowledge, the first case of its sort in our department and has thus caused debate and increased awareness among our specialists.
Because of the increased use of coated and slow-release non-steroidal anti-inflammatory drugs (NSAIDs), we expect that surgeons worldwide will be presented with an increasing number of patients presenting with NSAID-induced colopathy and therefore believe it is important that our colleagues are aware of the condition and its management.
Case presentation
A 64-year-old woman presented with microcytic hypochromic anaemia (haemoglobin 3.3 mM (normal range 7.0–10.0)), 1½ months of loose stools, no subacute stenotic symptoms and abdominal pain located in the epigastria and lower right quadrant.
Medical history included osteoarthritis requiring two right-sided total hip replacements performed 13 and 3 years prior to this episode, respectively. The patient had, due to osteoarthritis, taken diclofenac 50 mg × 3 daily for 18 months prior to this incident, and had no family history of inflammatory bowel disease, colon cancer or other relevant disease.
Acute gastroscopy was performed, which identified a pyloric ulcer without bleeding stigmata along with mild gastritis. After gastroscopy, diclofenac was withdrawn.
Because no bleeding source was found by gastroscopy and due to pain in the lower right quadrant, a colonoscopy was performed 2 months later. This examination revealed, in an otherwise normal colon, a stenosis in the right transverse colon. The stenosis was not passable by scope. Biopsies were taken, which showed colonic mucosa with focal fibrosis; there were no signs of malignancy. The patient at this point reported unintended weight loss of 14 kg within the past few months. Stool for occult blood was not performed.
Due to the fibrosis, Crohn's disease was initially suspected and the patient was discussed at a multidisciplinary conference. At this conference, it was decided, because of the unintended weight loss, to consider the stenosis as potentially malignant. A CT-colography was performed, which showed a possible tumour in the ascending colon, thick-walled coecum and enlarged lymph nodes along the vasa mesenterica.
A laparoscopic right hemicolectomy was performed 5 months after the initial presentation and thus 5 months after NSAID cessation. The operation revealed an injected right colon with enlarged lymph nodes in the mesentery, no obvious tumour and no carcinosis. At macroscopic evaluation, two concentric strictures with thickened adjacent bowel wall were found. The stricture placed most anally had the pathognomonic appearance of a diaphragm with only a pinpoint central lumen. The more orally placed stricture was flatter and more broad-based with adjacent ulceration (figure 1). The patient was discharged a week later.
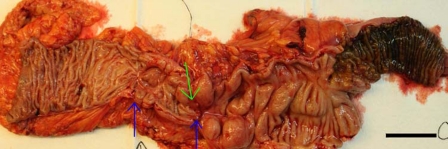
Figure 1.
Ascending colon containing two strictures (blue arrows), ulcer in relation to the oral stricture (green arrow) and dilated colon (right) oral to the stenoses (the bar represents 5 cm).
Microscopic examination of the specimen revealed the following: In the mucosa, crypt irregularity and mild inflammation were found. In the central part of the diaphragm, submucosal fibrosis with bundles of collagen aligned towards the apex of the diaphragm was identified. In relation to the ulcer, pronounced inflammation and, again, submucosal fibrosis were found (figure 2). The specimen showed no transmural inflammation or granulomata, which otherwise could indicate inflammatory bowel disease. The lymph nodes showed only inflammatory changes. There were no signs of malignancy.
Figure 2.
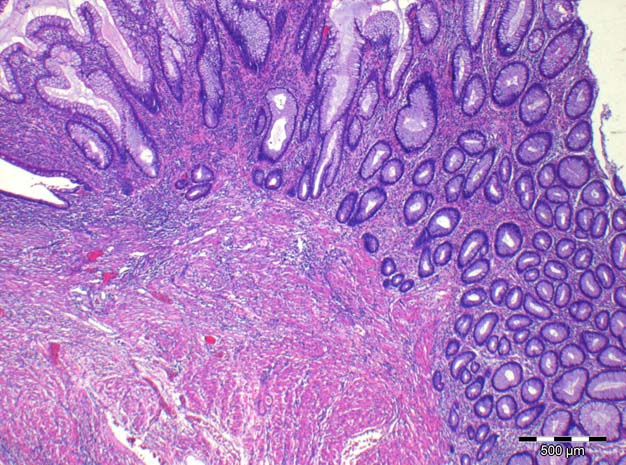
The anal stricture showing regenerative changes in the mucosa and submucosal inflammation and fibrosis (haematoxylin/eosin, 20×).
Investigations
-
▶
Gastroscopy – identifying a pyloric ulcer without bleeding stigmata along with mild gastritis.
-
▶
Colonoscopy with biopsies – identifying a stenosis just anal to the right flexure and biopsies revealing focal fibrosis in otherwise normal colonic mucosa.
-
▶
Microscopic evaluation of the operative specimen – revealing crypt irregularity and mild inflammation in the mucosa and submucosal fibrosis. The specimen showed no transmural inflammation or granulomata, which otherwise could indicate inflammatory bowel disease. No signs of malignancy.
Differential diagnosis
Colon cancer, inflammatory bowel disease (primarily Crohn's disease).
Treatment
-
▶
Withdrawal of NSAID
-
▶
Laparoscopic right hemicolectomy
Outcome and follow-up
The patient was seen in an outpatient clinic 1 month after the operation. At this point, all gastrointestinal (GI) symptoms had resolved and the patient was told not to use NSAIDs in the future.
Discussion
Adverse effects of the NSAIDs in the upper GI tract are well known to clinicians and physicians. NSAID-induced enteropathy, comprising inflammation, ulceration, occult bleeding and subsequent stricture formation in the small bowel, has become an established clinical entity.1 2 Recently, an increasing number of reports of similar pathological changes in the colon has led to increased awareness of, what is termed, NSAID-induced colopathy,3–6 although only around 100 cases have been presented in the literature.
NSAID-induced colopathy can present in various ways. Chronic symptoms such as iron-deficiency anaemia, abdominal pain, weight loss, blood-positive stools or altered bowel habits are the most common presenting features. However, acute presentation with bowel obstruction and/or perforation can occur. As in the case presented here, long-term NSAID use typically precedes the symptoms and the diagnosis, and most often the causative drug or drugs have been used for several years.6 7 There have also been reports, however, of short-term use causing severe colopathy with perforation.8
The diagnosis can be difficult. Biochemical levels are often unspecific, plain abdominal x-ray is not helpful and even CT-scans may not have the desired slice thickness to identify the colonic diaphragms.9 The diagnosis is most easily established with colonoscopy.6 However, awareness of the condition is cornerstone to its diagnosis.
Primary management is simple and includes withdrawal of the offending NSAID. This simple step often alleviates symptoms, since inflammation and ulceration are stopped. Already formed diaphragms, however, do not disappear when the NSAID is withdrawn. These diaphragm strictures can sometimes be handled with balloon dilatation.10 Surgery is reserved for the cases presenting more acutely and for those with severe obstruction.11
An important part of the management is to exclude other possible causes of large bowel obstruction. Inflammatory bowel disease and, most importantly, malignant disease must be ruled out before making the diagnosis. Sometimes, as in the case presented here, the diagnosis can only be made after surgical resection.
Due to increasing awareness of the upper GI side effects of NSAIDs,12 enteric-coated and slow-release formulations have been introduced. Thus, with these formulations intestinal mucosa in the lower GI tract is subjected to the NSAIDs directly. Although the pathogenesis of the small and large bowel lesions has not been fully established, and controversy remains whether the lesions arise in response to a direct or systemic toxic effect,6 7 13 the increased number of reports of colonic damage parallel to the introduction of the slow-release drugs support the hypothesis concerning a direct toxic effect. The fact that the lesions have only been described in the right colon, where the coecum acts as a reservoir and the mucosa, thus, is subjected to the NSAIDs for a long time, supports this hypothesis further.14
As described, the presentation of these patients can be unspecific, and other more common causes of entero- or colopathy are primarily sought. However, the pathognomonic endoscopic findings supported by histology with ulceration, submucosal fibrosis and inflammation may give the diagnosis.
In conclusion, with an ageing population, prolonged treatment of chronic illnesses and the increased use of enteric-coated or slow-release NSAIDs, the number of patients presenting with NSAID-induced colopathy has presumably not yet peaked. Thus, the general surgeon, as well as other physicians, should consider this diagnosis, when assessing patients with the relevant symptoms and a history of NSAID use.
Learning points.
-
▶
NSAID-induced colopathy is a relevant differential diagnosis to colon cancer and inflammatory bowel disease.
-
▶
Withdrawal of the offending NSAID most often alleviates the symptoms.
-
▶
Diaphragms causing stenosis can be identified by colonoscopy and managed by balloon dilatation.
-
▶
Surgery is reserved for cases presenting acutely and for those with severe obstruction.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Lang J, Price AB, Levi AJ, et al. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol 1988;41:516–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao B, Sanati S, Eltorky M. Diaphragm disease: complete small bowel obstruction after long-term nonsteroidal anti-inflammatory drugs use. Ann Diagn Pathol 2005;9:169–73 [DOI] [PubMed] [Google Scholar]
- 3.El Hajj I, Hawchar M, Sharara A. NSAID-induced colopathy: case report and review of the literature. J Med Liban 2009;57:274–6 [PubMed] [Google Scholar]
- 4.Margolius DM, Cataldo TE. Nonsteroidal anti-inflammatory drug colopathy mimicking malignant masses of the colon: a report of three cases and review of the literature. Am Surg 2010;76:1282–6 [PubMed] [Google Scholar]
- 5.Aftab AR, Donnellan F, Zeb F, et al. NSAID-induced colopathy. A case series. J Gastrointestin Liver Dis 2010;19:89–91 [PubMed] [Google Scholar]
- 6.Byrne MF, McGuinness J, Smyth CM, et al. Nonsteroidal anti-inflammatory drug-induced diaphragms and ulceration in the colon. Eur J Gastroenterol Hepatol 2002;14:1265–9 [DOI] [PubMed] [Google Scholar]
- 7.Masannat YA, Harron M, Harinath G. Nonsteroidal anti-inflammatory drugs-associated colopathy. ANZ J Surg 2010;80:96–9 [DOI] [PubMed] [Google Scholar]
- 8.Bjarnason I, Hayllar J, MacPherson AJ, et al. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology 1993;104:1832–47 [DOI] [PubMed] [Google Scholar]
- 9.Pilgrim S, Velchuru V, Waters G, et al. Diaphragm disease and small bowel enteropathy due to non-steroidal anti-inflammatory drugs: a surgical perspective. Colorectal Dis 2009 [DOI] [PubMed] [Google Scholar]
- 10.Smith JA, Pineau BC. Endoscopic therapy of NSAID-induced colonic diaphragm disease: two cases and a review of published reports. Gastrointest Endosc 2000;52:120–5 [DOI] [PubMed] [Google Scholar]
- 11.Gargot D, Chaussade S, d'Alteroche L, et al. Nonsteroidal anti-inflammatory drug-induced colonic strictures: two cases and literature review. Am J Gastroenterol 1995;90:2035–8 [PubMed] [Google Scholar]
- 12.García Rodríguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet 1994;343:769–72 [DOI] [PubMed] [Google Scholar]
- 13.Hooker GD, Gregor JC, Ponich TP, et al. Diaphragm-like strictures of the right colon induced by indomethacin suppositories: evidence of a systemic effect. Gastrointest Endosc 1996;44:199–202 [DOI] [PubMed] [Google Scholar]
- 14.Halter F, Weber B, Huber T, et al. Diaphragm disease of the ascending colon. Association with sustained-release diclofenac. J Clin Gastroenterol 1993;16:74–80 [DOI] [PubMed] [Google Scholar]