Abstract
This report concerns a case of an 80-year-old man with progressive dysphagia and stridor. Patient's clinical and radiological evaluation revealed a mass of the hypopharynx and a large cervical osteophyte. Microlaryngoscopy under general anaesthesia demonstrated the presence of a hypopharynx abscess that was drained. A tracheotomy was performed in order to secure the airway, and 6 weeks later, the patient was decannulated and returned to full consistency diet.
Background
Anterior cervical osteophytes impinging upon the pharynx or oesophagus constitute a cause of dysphagia. Predominant among the pathological entities that can lead to the formation of osteophytes are diffuse idiopathic skeletal hyperostosis (DISH), degenerative diseases of the cervical spine and ankylosing spondylitis (AS). Although these patients are usually asymptomatic, there is documentation of patients presenting with upper aerodigestive tract symptoms. Moser in 1926 was the first to report dysphagia due to cervical spine osteophytes.1 Twenty-eight per cent of patients with cervical osteophytes complain of dysphagia.2 Although previous authors have described many cases of dysphagia due to cervical osteophytes, there was no reference to the literature of dysphagia and osteophytes combined with a hypopharynx abscess as we describe in our patient.
Case presentation
An 80-year-old man presented to our hospital complaining of progressive mild dysphagia, cough while eating for the last 10 days and stridor for 3 days. He reported no fever or odynophagia. Medical history included hypertension, arthritis and chronic obstructive airway disease. He also reported mild dysphagia to solid food in the past years. His nutritional status was good and no weight loss was reported.
Investigations
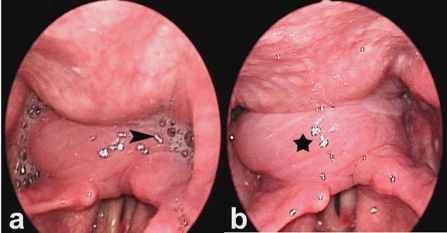
Indirect laryngoscopy with rigid endoscope revealed a mass in the postcricoid area plus impaired vocal cord mobility due to the pressure of the soft tissue mass. Vocal cords were lying in a paramedian position leaving a spindle-shaped gap during phonation. Saliva was retained in the pyriform sinuses (figure 1A,B). Evaluation of swallowing using flexible endoscope and food coloured with Evan's blue dye demonstrated presence of food in the pyriform sinuses and penetration into the larynx.
Figure 1.
Endoscopic evaluation before surgery. (A) Saliva retained in the pyriform sinuses (arrowhead) and (B) fluctuant mass of hypopharynx (asterisk).
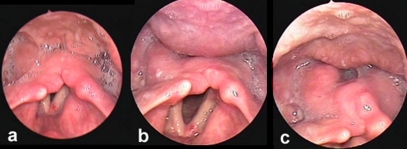
Radiological evaluation with plain radiographs revealed large anterior cervical osteophytes at the C4–C5 vertebra level, ossification of the anterior longitudinal ligament and a soft tissue mass impinging upon the postcricoid region (figure 2).
Figure 2.
Plain radiograph of the neck; soft tissue mass of hypopharynx (white arrow) and protruding osteophytes of C3–C4 vertebrae (black arrow).
Laboratory examinations were normal.
On physical examination, the patient was well oriented, with stable vital signs.
Differential diagnosis
The hypopharyngeal mass warranted urgent investigation by a head and neck surgeon to exclude malignancy. The mass could also be inflammatory, infective or of benign neoplastic origin. The patient had no coexisting known diseases that might affect swallowing function, such as lung cancer, oesophagus cancer, achalasia, stroke or Parkinson's disease.
Treatment
Microlaryngoscopy performed under general anaesthesia confirmed the existence of a fluctuant mass to the postcricoid area. Incision, drainage and marsupialisation of the mass were performed. The culture of the pus obtained showed staphylococcus. A tracheotomy was performed to provide secure airway and a nasogastric feeding tube was inserted for 5 days to ensure that the patient received adequate nutrition.
Patient was informed of the option of surgical excision of the osteophytes by the spinal cord surgeons but he strongly declined this alternative.
Postoperatively, the patient was treated with corticosteroids and non-steroid anti-inflammatory drugs.
Outcome and follow-up
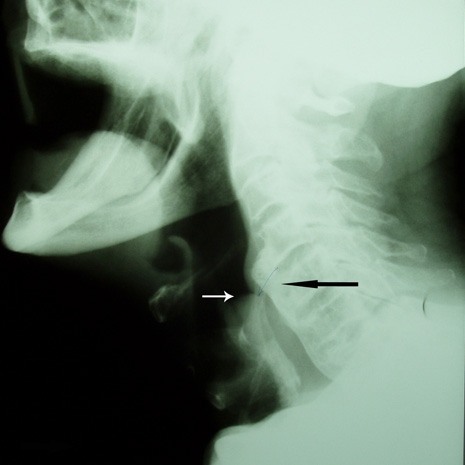
The postoperative period was uneventful. Weekly postoperative endoscopic evaluation of swallowing revealed food aspiration, which resolved 6 weeks later and the patient was decannulated (figure 3A–C). The patient remained free of swallowing problems on a full consistency diet 1.5 years after surgery.
Figure 3.
(A) Four weeks after surgery, the patient remains cannulated; obvious regression of the mass is seen and the saliva retains in the pyriform sinuses with episodes of aspiration. (B) Six weeks after surgery, the patient is decannulated, with no episodes of aspiration. (C) Six weeks after surgery, there is total regression of the mass without any blockage to the lumen of hypopharynx/postcricoid area.
Discussion
Cervical osteophytes affect proximally 20–30% of the population, especially middle aged and older people.3 Cervical bony outgrowths are common and have a vast differential diagnosis, which includes DISH, AS, acromegaly, hypoparathyroidism and trauma. Among these, the most common causes of cervical anterior osteophytes are DISH and AS.4
Cervical osteophytes may cause several clinical manifestations. Symptoms involved with the spine are rigidity, decreased mobility and spinal column pain.5 Cervical osteophytes can also cause respiratory symptoms such as dyspnoea,6 aspiration pneumonia4 and sleep apnoea.7 The most common symptom is progressive difficulty with solid foods and eventually liquids. Dysphagia may be accompanied by foreign body sensation or odynophagia.8
There are many mechanisms explaining dysphagia caused by osteophytes, including (1) direct impingement by large osteophytes, (2) obstruction by local periosteophyte oedema and inflammation, (3) spasm of the adjacent cricopharyngeal musculature, (4) smaller osteophytes may cause dysphagia if they are located opposite to a fixed point such as the cricoid cartilage, (5) fibrosis and adhesions from tissue reaction near the protruding mass that fixes the oesophagus and prevents normal mobility and (6) interference with epiglottis movement.9–11
The most frequent level related to dysphagia is C5–C6 followed by C4–C5.12 The bolus is passing through a severely restricted cricopharyngeal opening, because of the presence of the osteophytes. The bolus may traumatise the mucosa, cause erosions and ulcers at the point of pressure between the cricoid cartilage and the protruding osteophytes10 and can rarely result in perforation of the pharynx.13 These ulcers could allow microorganisms to penetrate the mucosa and lead to inflammation and abscess formation. This hypothesis could be an explanation for the development of the abscess that complicated the coexisting mild osteophytic dysphagia in our patient.
Radioimaging – spinal x-ray or CT scan – is the gold standard investigation for DISH, having an advantage over MRI for demonstration of bone architecture.
Over the past four decades, various diagnostic criteria have been proposed, but the model suggested by Resnick and Niwayama is the most widely accepted. Their criteria are (1) flowing calcification of paraspinal longitudinal ligaments affecting at least four consecutive levels of vertebral bodies; (2) absence of signs suggestive of disc degeneration; and (3) absence of any other degenerative disease of the spinal joints.
For patients presented with respiratory or digestive symptoms, videofluoroscopy and laryngoscopy are important for evaluation of tracheal and oesophageal pathology.14 Endoscopy with rigid endoscope of the upper gastrointestinal system, when needed, should be performed cautiously because of the risk of oesophageal perforation.4
Treatment can be either conservative or surgical. Conservative management includes modification of diet, non-steroidal inflammatory medications, corticosteroids and muscle relaxants.15 The first-line treatment for patients presenting with dysphagia is diet modification and advice about mastication and deglutition by a speech therapist. Persistence or progression of the symptoms indicates that surgical excision of the cervical osteophytes, osteophytectomy, may be necessary. Surgical approaches used for cervical osteophytectomy are the transcervical anterolateral approach, posterolateral approach and transoral approach. Surgical interventions carry the risk of complications including oesophageal injury, recurrent laryngeal nerve injury, Horner's syndrome, cervical instability, persistent symptoms and recurrence.14
Cervical osteophytes should be considered in the differential diagnosis of dysphagia in older people especially when thorough evaluation reveals no other cause of dysphagia such as functional and mobility disorders, structural lesions, neurologic diseases or neoplasms.16 Early diagnosis will contribute to the appropriate treatment, reduce the possibility of complications and add to the quality of life.
Learning points.
-
▶
Cervical osteophytes should be considered in the differential diagnosis of dysphagia.
-
▶
Lateral cervical radiography is important for diagnosis in patients with DISH and/or cervical osteophyte-induced dysphagia.
-
▶
Dysphagia caused by cervical osteophytes may be treated conservatively or surgically.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Mosher H. Exostoses of the cervical vertebrae as a cause of the difficulty in swallowing. Laryngoscope 1926;36:181–2 [Google Scholar]
- 2.Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology 1976;119:559–68 [DOI] [PubMed] [Google Scholar]
- 3.Bone RC, Nahum AM, Harris AS. Evaluation and correction of dysphagia-producing cervical osteophytosis. Laryngoscope 1974;84:2045–50 [DOI] [PubMed] [Google Scholar]
- 4.De Jesus-Monge WE, Cruz-Cuevas EI. Dysphagia and lung aspiration secondary to anterior cervical osteophytes: a case report and review of the literature. Ethn Dis 2008;18(2 Suppl 2):S2–137–40 [PMC free article] [PubMed] [Google Scholar]
- 5.Cammisa M, De Serio A, Guglielmi G. Diffuse idiopathic skeletal hyperostosis. Eur J Radiol 1998;27(Suppl 1):S7–11 [DOI] [PubMed] [Google Scholar]
- 6.Caminos CB, Cenoz IZ, Louis CJ, et al. Forestier disease: an unusual cause of upper airway obstruction. Am J Emerg Med 2008;26:1072.e1–3 [DOI] [PubMed] [Google Scholar]
- 7.Ando E, Ogawa T, Shigeta Y, et al. A case of obstructive sleep apnoea with anterior cervical osteophytes. J Oral Rehabil 2009;36:776–80 [DOI] [PubMed] [Google Scholar]
- 8.Mader R. Clinical manifestations of diffuse idiopathic skeletal hyperostosis of the cervical spine. Semin Arthritis Rheum 2002;32:130–5 [DOI] [PubMed] [Google Scholar]
- 9.Di Vito J., Jr Cervical osteophytic dysphagia: single and combined mechanisms. Dysphagia 1998;13:58–61 [DOI] [PubMed] [Google Scholar]
- 10.Constantoyannis C, Papadas T, Konstantinou D. Diffuse idiopathic skeletal hyperostosis as a cause of progressive dysphagia: a case report. Cases J 2008;1:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Granville LJ, Musson N, Altman R, et al. Anterior cervical osteophytes as a cause of pharyngeal stage dysphagia. J Am Geriatr Soc 1998;46:1003–7 [DOI] [PubMed] [Google Scholar]
- 12.Hilding DA, Tachdjian MO. Dysphagia and hypertrophic spurring of the cervical spine. N Engl J Med 1960;263:11–14 [DOI] [PubMed] [Google Scholar]
- 13.Fuerderer S, Eysel-Gosepath K, Schröder U, et al. Retro-pharyngeal obstruction in association with osteophytes of the cervical spine. J Bone Joint Surg Br 2004;86:837–40 [DOI] [PubMed] [Google Scholar]
- 14.Goh PY, Dobson M, Iseli T, et al. Forestier's disease presenting with dysphagia and dysphonia. J Clin Neurosci 2010;17:1336–8 [DOI] [PubMed] [Google Scholar]
- 15.Srivastava S, Ciapryna N, Bovill I. Diffuse idiopathic skeletal hyperostosis as an overlooked cause of dysphagia: a case report. J Med Case Reports 2008;2:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Valadka AB, Kubal WS, Smith MM. Updated management strategy for patients with cervical osteophytic dysphagia. Dysphagia 1995;10:167–71 [DOI] [PubMed] [Google Scholar]