Abstract
Study Design
Retrospective cohort study.
Objective
To evaluate the relationship between early physical therapy (PT) for acute low back pain and subsequent use of lumbosacral injections, lumbar surgery, and frequent physician office visits for low back pain.
Summary of Background Data
Wide practice variations exist in the treatment of acute low back pain. Physical Therapy (PT) has been advocated as an effective treatment in this setting though disagreement exists regarding its purported benefits.
Methods
A national 20% sample of the Centers for Medicare & Medicaid Services physician outpatient billing claims was analyzed. Patients were selected who received treatment for low back pain between 2003 and 2004 (n=439,195). To exclude chronic low back conditions, patients were excluded if they had a prior visit for back pain, lumbosacral injection, or lumbar surgery within the previous year. Main outcome measures were rates of lumbar surgery, lumbosacral injections, and frequent physician office visits for low back pain over the following year.
Results
Based on logistic regression analysis, the adjusted odds ratio for undergoing surgery in the group of enrollees that received PT in the acute phase (<4 weeks) compared to those receiving PT in the chronic phase (>3 months) was 0.38 (95% CI, 0.36 to 0.41), adjusting for age, gender, diagnosis, treating physician specialty, and comorbidity. The adjusted OR for receiving a lumbosacral injection in the group receiving PT in the acute phase was 0.46 (95% CI, 0.44 to 0.49), and the adjusted OR for frequent physician office usage in the group receiving PT in the acute phase was 0.47 (95% CI, 0.44 to 0.50).
Conclusions
There was a lower risk of subsequent medical service usage among patients who received PT early after an episode of acute low back pain relative to those who received PT at later times. Medical specialty variations exist regarding early use of PT, with potential underutilization among generalist specialties.
Keywords: Physical Therapy, Low Back Pain, Epidural Steroid Injection, Lumbar Surgery, Medicare, Epidemiology
Introduction
The lifetime prevalence of low back pain in adults is between 65% and 80%, and wide practice variations still exist in diagnosis and treatment of acute low back pain episodes. 1,2 Physical therapy (PT) has been advocated as an effective treatment for acute low back pain, 3,4 though disagreement exists regarding its benefits, and international guidelines contain conflicting recommendations for manipulation and exercise therapy. 5,6 While remaining active during an acute episode of low back pain has been shown to be more effective than bed rest, 7,8 evidence on the use of formal PT during an acute episode of low back pain is mixed. 3,4,6,9,10,11,12,13
The primary goal of this research was to evaluate the relationship between early PT use for acute low back pain and the use of other treatments for low back pain. Our hypothesis was that in the setting of acute low back pain, early PT use would be associated with decreases in the subsequent rates of lumbar surgery, lumbosacral spinal injections, and spine related physician encounters. We further sought to determine if use of early PT was substantially different across physician specialties.
Materials and Methods
Data Source
We examined a nationally representative, 20% sample of the Centers for Medicare & Medicaid Services (CMS) physician outpatient billing claims from 2002 through 2006, which allowed us to study episodes of care for the same patient over time. The dataset includes Current Procedural Technology (CPT) procedure codes, International Classification of Diseases, ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes, provider specialty, and date of service. Physician specialties were determined by the CMS Provider Specialty Code. Physician specialties associated with less than 2% of the total number of physician encounters for low back pain were grouped together as “Other Specialty”.
Patient Selection
In order to maintain consistency with previous studies on degenerative low back pain in the Medicare population, we limited our analysis to patients aged 66 or older who received treatment for low back pain between January 2003 and December 2004. Patients with back pain were identified using ICD-9-CM diagnosis codes (Appendix 1). Patients were selected if the primary diagnosis associated with the physician encounter corresponded to a low back pain diagnosis. We categorized these patients into seven groups, based on previously validated classifications 14: Nonspecific Backache; Probable Degenerative Changes; Spinal Stenosis; Herniated Disc; Possible Instability; Sciatica/Radiculitis; and Miscellaneous.
Appendix 1.
| Clinical Category | ICD-9 CM code | Diagnosis |
|---|---|---|
| Herniated Disc | 722.1 | Displacement of thoracic or lumbar disc without myelopathy |
| 722.10 | Displacement of lumbar disc without myelopathy | |
| 722.73 | Lumbar disc disorder with myelopathy | |
| Degenerative disc disease | 721.3 | Lumbosacral spondylosis without myelopathy |
| 721.5 | Baastrup’s disease | |
| 722.52 | Degeneration of lumbar or lumbosacral disc | |
| 722.93 | Other and unspecified lumbar disc disorder | |
| Spinal stenosis | 721.42 | Spondylogenic compression of lumbar spinal cord |
| 724.02 | Lumbar stenosis | |
| Possible Instability | 724.6 | Disorders of sacrum (including lumbosacral joint instability) |
| 738.4 | Acquired spondylolisthesis | |
| 756.11 | Spondylolysis, lumbosacral region | |
| 756.12 | Spondylolisthesis | |
| Nonspecific Backache | 307.89 | Psychogenic backache |
| 724.2 | Lumbago | |
| 724.5 | Backache, unspecified | |
| 846.0-9 | Sprains and strains, sacroiliac | |
| 847.2 | Sprains and strains, lumbar | |
| 847.3 | Sprains and strains, sacral | |
| Sciatica/Radiculitis | 724.3 | Sciatica |
| 724.4 | Thoracic or lumbosacral radiculitis | |
| Miscellaneous | 722.30 | Schmorl’s nodes, unspecified region |
| 722.32 | Lumbar Schmorl’s nodes | |
| 724.8 | Ossification of PLL | |
| 724.9 | Other unspecified back disorder | |
| 739.3 | Nonallopathic lesions, lumbar region | |
| 739.4 | Nonallopathic lesions, sacral region | |
| 756.10 | Anomaly of spine, unspecified |
The index visit for each patient was defined as the first physician office visit for a low back pain diagnosis within the study period. In order to select patient with acute rather than chronic low back pain, we excluded patients who had had a prior physician visit for low back pain, back surgery or a lumbar injection in the previous year. Patients were also excluded if their only PT visits were for postoperative rehabilitation.
Variables of interest
The primary variable of interest was time between an initial physician visit for low back pain and an outpatient PT visit, identified using CPT procedure codes. All PT visits were associated with a low back pain diagnosis code in order to exclude PT services provided for other diagnoses. Time to PT was measured as the number of days between the index physician visit and the initiation of physical therapy for low back pain and categorized into three groups, representing treatment in the acute, subacute, and chronic stage after diagnosis of low back pain. Based on previous definitions, 6,8,12,15,16,17 we defined the acute, subacute, and chronic treatment groups as those receiving PT in less than 4 weeks after the index visit, between 4 weeks and 3 months after the index visit, and between 3 months and 12 months after the index visit, respectively.
Outcomes
For each patient with a visit for low back pain, we counted episodes of surgery, lumbosacral injections, and back-related physician office visits that occurred subsequent to the initial physician visit for low back pain. Lumbosacral injections were identified using CPT procedure codes for caudal injections, interlaminar injections, transforaminal injections, facet joint injections, and sacroiliac injections. Lumbar surgery was identified using ICD-9 and CPT codes. We defined frequent physician office visit use as more than one standard deviation above the mean number of office visits for the population of enrollees. For patients who received any PT, the mean number of office visits related to low back pain in a year was 5 (standard deviation, 5.9). Heavy physician office visit use was therefore defined as 11 or more visits for a spine-related diagnosis within a year from the index visit.
Analysis
We used logistic regression models to examine the association between the timing of the initiation of PT and the likelihood of undergoing lumbar surgery or lumbar injection subsequent to the initial physician evaluation, after controlling for age, sex, primary diagnosis, physician specialty at initial visit, and comorbidity as calculated by the Charlson comorbidity index. 18 Comorbidity score and age were considered continuous variables in the regression analysis, while other variables were considered discrete categorical variable. To further determine any effects of age on the model given its potentially nonlinear relationship with health status, a secondary analysis was performed using age2 as a continuous variable in the regression model. Controlling for the same covariates, logistic regression models were also used to examine the relationship between PT initiation and frequent office visit usage. We tested each coefficient for significance using Wald tests. All data were analyzed with SPSS statistical software, version 16 with alpha level for hypothesis testing set at 0.05.
Results
Patient Demographics
431,195 enrollees were included in the analysis. The baseline characteristics of all patients are shown in Table 1, with comparisons among the three subgroups for PT as well as those enrollees who did not receive any PT. The largest subgroup of encounters was for nonspecific backache, which accounted for 63.6% of all physician encounters, followed by sciatica (14.5%), degenerative disc disease (10.5%), and spinal stenosis (6.2%). Diagnoses of herniated disc, instability, and miscellaneous low back pain diagnoses each accounted for less than 3% of all physician encounters for acute low back pain.
Table 1.
Patient characteristics
| All Patients (N=439,195) | Acute PT (N=29,169) | Subacute PT (N=10,138) | Chronic PT (N=16,800) | No PT (N=383,088) | |
|---|---|---|---|---|---|
| Mean Age - years | 76.0 | 75.1 | 75.2 | 75.3 | 76.2 |
| Charlson comorbidity score | 1.6 | 1.6 | 1.6 | 1.7 | 1.6 |
| Female | 67% | 64% | 67% | 68% | 67% |
| Diagnosis | |||||
| Nonspecific ache | 63.6% | 56.3% | 54.2% | 55.3% | 65.1% |
| Sciatica | 14.5% | 17.1% | 19.0% | 17.0% | 14.0% |
| Degenerative disc disease | 10.5% | 13.9% | 11.6% | 12.5% | 10.0% |
| Spinal stenosis | 6.2% | 6.2% | 8.7% | 9.0% | 5.9% |
| Herniated disc | 2.7% | 3.6% | 4.0% | 3.3% | 2.6% |
| Misc | 1.3% | 1.4% | 1.1% | 1.2% | 1.3% |
| Instability | 1.2% | 1.5% | 1.4% | 1.7% | 1.1% |
| 100.0% | 100.0% | 100.0% | 100.0% | 100.0% |
Among all patients who received PT, the mean time to initiation of PT was 86 days, with a range of 1 day to 365 days. Of patients receiving PT following initial physician encounter for low back pain, 52.0% received PT in the acute period, 18.1% received PT in the subacute period, between 31 days and 90 days, and 29.9% received PT in the chronic, or late period, between 91 days and 365 days.
Treating Physician Specialty
66 different physician specialties were associated with encounters for low back pain. The 10 most common specialties associated with a back-related physician visit, accounting for 93.5% of all cases, were Internal Medicine (27.8%), Family Medicine (24.7%), Orthopedics (16.1%), Emergency Medicine (6.0%), General Practice (3.9%), Physical Medicine & Rehabilitation (3.4%), Anesthesia (3.2%), Neurosurgery (3.1%), Neurology (3.1%), and Rheumatology (2.2%). The generalist specialties, including Internal Medicine, Family Practice, General Practice and Emergency Medicine, had the majority of encounters (62.4%). There were significant differences in diagnosis codes associated with various specialties as shown in Table 2. The generalist medical specialties were all associated with higher proportions of visits coded for nonspecific backache than the surgical subspecialties of Orthopedic Surgery and Neurosurgery as well as compared to other nonsurgical subspecialties. In contrast, the surgical subspecialties were associated with higher proportions of visits coded for spinal stenosis, herniated disc, potential instability, and degenerative disc disease.
Table 2.
Physician Specialty and Primary Diagnosis Code
| Diagnosis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Back ache | Degen Disc Disease | Herniated Disc | Instability | Misc | Sciatica | Spinal Stenosis | Total | |
| Specialty | ||||||||
| Generalist | ||||||||
| Internal Med | 78.3% | 3.5% | 1.6% | 0.2% | 1.1% | 13.3% | 2.0% | 100.0% |
| Family Practice | 78.4% | 4.2% | 1.4% | 0.3% | 1.7% | 12.7% | 1.2% | 100.0% |
| Emergency Med | 83.4% | 2.5% | 0.8% | 0.4% | 1.2% | 11.3% | 0.5% | 100.0% |
| General Practice | 72.7% | 6.9% | 2.3% | 0.4% | 3.1% | 12.5% | 2.1% | 100.0% |
| Surgical | ||||||||
| Orthopedics | 34.3% | 28.4% | 4.0% | 4.2% | 0.6% | 13.7% | 14.8% | 100.0% |
| Neurosurgery | 20.9% | 19.4% | 11.5% | 4.3% | 0.3% | 12.1% | 31.5% | 100.0% |
| Other Specialty | ||||||||
| PM&R | 40.4% | 17.6% | 4.0% | 1.5% | 1.5% | 22.6% | 12.5% | 100.0% |
| Anesthesia | 23.3% | 21.7% | 8.0% | 0.8% | 2.4% | 26.9% | 16.7% | 100.0% |
| Neurology | 27.9% | 6.8% | 5.7% | 0.6% | 0.9% | 45.4% | 12.8% | 100.0% |
| Rheumatology | 51.9% | 24.2% | 1.7% | 1.0% | 0.9% | 10.9% | 9.4% | 100.0% |
| Total | 63.6% | 10.5% | 2.7% | 1.2% | 1.3% | 14.5% | 6.2% | 100.0% |
Associated Treatments
Within 1 year from initial encounter for low back pain, 16.2% of enrollees received PT for low back pain, 11.9% received a lumbosacral injection, and 3.1% underwent lumbar surgery. Of all patients who underwent surgery, 35.1% had received at least one prior lumbosacral injection, and 27.5% had received prior physical therapy. Odds ratios for the outcomes of receiving lumbar surgery, lumbosacral injection, and heavy office use (≥ 11 office visits) based on the variables in the regression analysis are presented in Table 3.
Table 3.
Relationship between timing of PT and outcomes of surgery, lumbosacral injection, and physician office visits
| Odds Ratio for undergoing Lumbar Surgery | Odds Ratio for undergoing Lumbosacral Injection | Odds Ratio for Heavy Physician Office Visit usage for LBP (>11 per year) | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| PT group | |||
| Acute | 0.38 (0.36–0.41) | 0.46 (0.44–0.49) | 0.47 (0.44–0.50) |
| Subacute | 0.79 (0.73–0.86) | 0.90 (0.85–0.95) | 0.73 (0.68–0.79) |
| Chronic | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Age | 0.96 (0.95–0.96) | 1.01 (1.00–1.01) | 1.00 (0.99–1.00) |
| Comorbidity score | 0.92 (0.90–0.94) | 0.97 (0.96–0.99) | 1.03 (1.02–1.04) |
| Sex | |||
| Male | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Female | 0.69 (0.65–0.73) | 0.96 (0.92–1.01) | 1.21 (1.15–1.28) |
| Diagnosis | |||
| Backache | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Degen Disc Disease | 1.21 (1.09–1.35) | 1.30 (1.21–1.40) | 1.20 (1.11–1.31) |
| Herniated Disc | 1.94 (1.68–2.25) | 1.88 (1.68–2.09) | 1.21 (1.06–1.39) |
| Instability | 2.18 (1.77–2.68) | 1.46 (1.24–1.73) | 1.12 (0.90–1.38) |
| Miscellaneous | 0.72 (0.49–1.04) | 0.72 (0.57–0.91) | 1.001 (0.80–1.27) |
| Sciatica | 1.49 (1.36–1.63) | 1.77 (1.67–1.88) | 1.01 (0.94–1.09) |
| Spinal Stenosis | 2.70 (2.43–3.00) | 2.06 (1.90–2.23) | 1.35 (1.22–1.48) |
| Physician Specialty | |||
| Internal Medicine | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Anesthesia | 1.41 (1.19–1.68) | 6.35 (5.66–7.12) | 1.79 (1.57–2.05) |
| Emergency Medicine | 1.30 (1.08–1.55) | 1.31 (1.16–1.49) | 1.02 (0.88–1.19) |
| Family Practice | 1.07 (0.96–1.18) | 0.93 (0.87–1.00) | 1.03 (0.95–1.12) |
| General Practice | 0.83 (0.68–1.01) | 0.76 (0.66–0.87) | 1.21 (1.06–1.38) |
| Neurology | 1.08 (0.90–1.29) | 0.98 (0.86–1.11) | 1.41 (1.23–1.62) |
| Neurosurgery | 3.21 (2.79–3.69) | 1.26 (1.11–1.43) | 1.04 (0.89–1.21) |
| Orthopedics | 1.34 (1.21–1.48) | 1.70 (1.59–1.82) | 0.99 (0.91–1.07) |
| PM&R | 0.79 (0.67–0.93) | 1.60 (1.46–1.75) | 1.47 (1.33–1.64) |
| Rheumatology | 0.80 (0.62–1.03) | 1.11 (0.95–1.29) | 1.40 (1.19–1.65) |
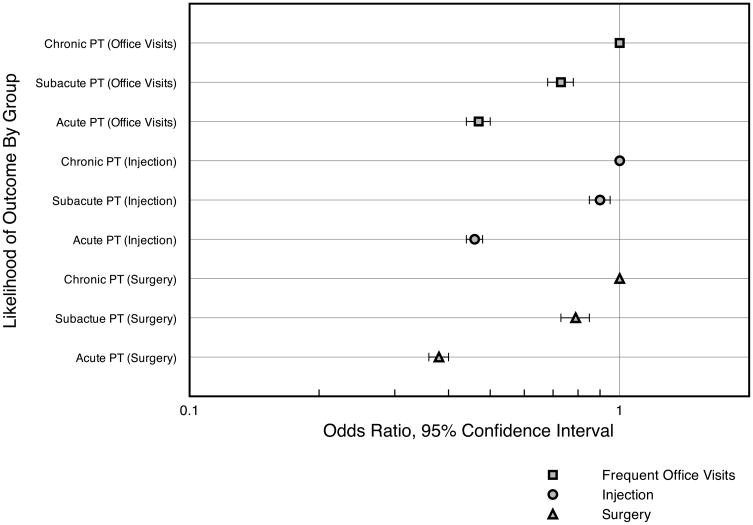
There was a significant reduction in the likelihood of undergoing subsequent surgery in the group of patients who received PT in either the acute or subacute phase, as compared with those receiving PT in the chronic phase (Figure 1). The odds ratio for undergoing surgery in the group of enrollees that received PT in the acute phase, compared to those receiving PT in the chronic phase was 0.38 (95% confidence interval, 0.36 to 0.41), after adjusting for age, gender, diagnosis, treating physician specialty, and comorbidity. The adjusted odds ratio for undergoing surgery in those receiving PT in the subacute phase when compared to those receiving PT in the chronic phase was 0.79 (95% confidence interval, 0.73 to 0.86).
Figure 1.
Odds Ratio for Undergoing Lumbar Surgery, Spinal Injection, or Heavily Using Subsequent Office Visits for Low Back Pain
The risk for lumbosacral injection among enrollees receiving PT in the acute or subacute phase was lower than that of patients receiving PT in the chronic phase. While 17% of all enrollees who received PT also received a lumbosacral injection, the adjusted odds ratio for receiving an injection in the group receiving PT in the acute phase as compared to the chronic phase was 0.46 (95% confidence interval, 0.44 to 0.49). The adjusted odds ratio for receiving a lumbosacral injection in those receiving PT in the subacute phase was 0.90 (95% confidence interval, 0.85 to 0.95).
A reduction in frequent use of physician office visits for low back pain was also noted in the group of patients receiving PT in the acute phase or subacute phase. The adjusted odds ratio for frequent physician office visits was 0.47 (95% confidence interval, 0.44 to 0.50) for acute PT patients and 0.73 (95% confidence interval 0.68 to 0.79) for subacute PT patients.
Medical Specialty Variations
Patterns of enrollees’ physical therapy use were different based on physician specialty at initial diagnosis (Table 4). Among the 10 medical specialties that evaluated patients with low back pain most often, patients who were initially evaluated by generalist specialists were least likely to receive physical therapy within 1 year, while those evaluated by physiatrists (PM&R) were most likely to receive physical therapy within 1 year from evaluation and also most likely to receive physical therapy in the acute setting. More than thirty percent of patients initially evaluated by a physiatrist received subsequent PT, compared to less than 10% of those initially evaluated by an emergency room specialist, 13% of those initially evaluated by a family practitioner and 14% of those initially evaluated by an internist.
Table 4.
Physician Specialty and Referral to PT
| PT subgroup | ||||
|---|---|---|---|---|
| Any PT | Acute | Subacute | Chronic | |
| Specialty | ||||
| Generalist | ||||
| Internal Med | 14.4% | 38.3% | 14.3% | 47.5% |
| Family Practice | 13.3% | 41.4% | 14.6% | 44.0% |
| Emergency Med | 9.8% | 35.5% | 17.3% | 47.2% |
| General Practice | 17.3% | 45.7% | 13.3% | 41.0% |
| Surgical | ||||
| Orthopedics | 22.4% | 45.9% | 13.6% | 40.6% |
| Neurosurgery | 17.1% | 29.2% | 17.2% | 53.6% |
| Other Specialty | ||||
| PM&R | 32.0% | 59.6% | 10.6% | 29.8% |
| Anesthesia | 16.4% | 21.3% | 15.4% | 63.3% |
| Neurology | 18.9% | 32.8% | 15.9% | 51.3% |
| Rheumatology | 17.7% | 31.7% | 14.5% | 53.8% |
| Total | 16.2% | 40.9% | 14.2% | 44.8% |
Discussion
Among Medicare beneficiaries evaluated for low back pain, we found a strong association between the utilization of early PT and a decrease in the likelihood of subsequent lumbar surgery, lumbosacral injection, and frequent back pain related physician visits in the year following initial evaluation. In addition, there appeared to be a “dose-response” relationship between the time until initiating treatment with PT and the reduced risk of undergoing additional interventions. That is, the risk was lower in the group of patients receiving PT in the acute phase compared with those receiving PT in the subacute phase. Finally, although generalist medical specialties had the highest proportion of the visits for acute back pain, they were associated with the lowest rates of subsequent PT visits.
Early Physical Therapy Use
Early physical therapy was strongly associated with decreased use of lumbosacral injections, physician office visits for low back pain, and lumbar surgery, when compared with PT that occurred at later times. This finding is consistent with a recent case-control study of active PT care for acute low back pain that reported an association between active PT within 90 days of onset of acute low back pain and decreased use of various healthcare resources including prescription medication, MRI imaging, and epidural injections in the year following discharge from PT. 13 Other studies have demonstrated that physical therapy initiated within the first six weeks following diagnosis of low back pain leads to a wide range of improvements in disability, general health, social function, anxiety, depressive symptoms, mental health and vitality, when compared to advice on staying active. 4 However, other systematic reviews and meta-analyses have reported inconclusive or limited benefits for PT in the setting of acute low back pain. 19,20 Indeed, these discrepancies may form the basis for the difference in national and international guidelines in recommending PT as an early intervention in acute low back pain. Guidelines from Australia and the Netherlands recommend no formal physical interventions in the treatment of acute low back pain in the first 6 weeks, while guidelines from the USA, UK, New Zealand, Denmark and Sweden all recommend various forms of early physical intervention, and guidelines from Israel, Germany, and Finland are equivocal. 5 This study provides additional support for a beneficial effect of early PT.
Dose-response relationship
There are a number of potential explanations for the dose-response relationship we found. First, early formal PT may substantially increase patients’ level of overall activity in the acute stage of low back pain, the effect of which has been shown in a number of studies to be superior to inactivity. 4,7,12,21,22 Second, physical therapists may provide continued patient education and reassurance about the expected course of back pain; in primary care settings, the rates of patient education by physicians about the benign course of back pain has been found to be as low as 23%, 23 though this represents a key component of many clinical practice guidelines. 6 Finally, the physical therapy interventions themselves may have a beneficial effect on outcomes, though this study did not examine the specific types of interventions performed at each visit. Indeed, debate continues regarding the most appropriate types of therapy to deliver within a PT session and whether subgroups of patients may be identified who would benefit differentially from alternate types of treatment, whether focused on passive modalities, manipulation, stretching, or active strengthening of particular muscle groups. 3 It is clear that PT encounters may represent a number of contrasting treatments; this study does not differentiate between them, but nevertheless suggests an overall benefit for a heterogeneous set of treatments.
Provider specialty
More than sixty medical specialties were found to be involved in initial evaluation and treatment of patients with acute low back pain in this Medicare population. The largest proportion of these medical providers represented primary care providers. Nearly two-thirds of all patients were initially evaluated by a generalist specialty, including Internal Medicine, Family Practice, Emergency Medicine or General Practice. This is similar to prior epidemiological data from the National Ambulatory Medical Care Survey (NAMCS) which is a general physician survey intended to represent practicing office based physicians. In that study, 56% of all back pain visits were evaluated by a generalist specialty, 2 and the rates of evaluation by neurologists (4.0%), neurosurgeons (7.1%), and orthopedic surgeons (25%) were higher than those reported here. However, that may reflect differences in specialty referrals as well as a different patient population, as the NAMCS data includes patients of all ages as well as all visits for low back pain rather than the initial physician office visit as we report here.
Practice pattern variations between medical specialties have been shown to exist in the diagnostic labeling and treatment of low back pain 24,25 as well as in multiple other settings where different specialties overlap in evaluation and treatment of a particular disease or disorder. 26,27,28 Outcome variations between specialties have been noted as well, especially in the surgical literature. 29,30,31 Indeed, in this study, we found that there were significant differences in patients’ use of PT based on the physician specialty at initial patient evaluation for acute low back pain. Patients initially evaluated by physiatrists were much more likely than those initially treated by other medical specialties to receive any PT as well as to receive PT at the earliest time point. Referral patterns may represent a difference in medical training or treatment bias between specialties; economic factors may also be important in referral to PT, as providers may have a financial relationship with a PT practice. Given the potential benefits of early PT discussed here, our finding that generalist practitioners are associated with the lowest rates of physical therapy visits among patients suggests that efforts directed at increasing appropriate PT referrals among this group of physicians may be beneficial in decreasing overall medical service use for low back pain complaints in this group of patients. However, further cost analyses are needed to fully evaluate the overall medical utilization costs in this setting, as the direct costs of formal physical therapy are significant and may approach or exceed the costs of the other outcomes measured in this study.
Percentage of patients receiving PT
Of all patients evaluated for acute low back pain, only a minority (16.2%) received PT within one year. In other published population based studies of patients with low back pain, the percentage of patients receiving PT has been higher. Two studies 2,32 have used the National Ambulatory Medical Care Service (NAMCS) database to evaluate population based patterns of resource use in patients with low back pain. These have shown PT referrals made in 21% to 27% of cases. An even larger percentage of patients (38%) received PT referrals in a cohort of patients evaluated at US Spine centers 33, and in a German cohort of primary care patients (49%) 34. These differences may be partially explained by the younger age groups evaluated in these studies; older patients with low back pain have been shown to be less likely to receive referral to PT than younger patients with similar diagnoses. 33
While the majority of acute low back pain resolves within seven weeks, the natural history of low back pain tends to include episodic exacerbations and remissions of symptoms, though the rate of recurrence has been found to be variable in different populations, as well as with varied definitions of recurrence. 1,35,36 In analyzing treatment that occurred in the subacute or chronic time periods after initial physician evaluation, it is therefore possible that these interventions represent responses to symptomatic exacerbations rather than responses to a continuation of the original episode of low back pain.
Limitations
Important limitations in the use of Medicare databases in outcomes research have been previously reported 37 and include potentially inaccurate coding, the inherent vagueness of the ICD-9 taxonomy, and difficulty in determining the severity of the disease in question. Certainly, patients with more significant disease or disability are more likely to receive additional evaluation and treatment compared to those with mild symptoms. Our finding that 2.7% of enrollees who did not receive any PT progressed to eventual lumbar surgery compared with 5.3% of those who did receive PT likely reflects this difference in disease severity. The patients without any PT visits likely represent cases of mild back pain, for which further evaluation or treatment was felt to be contraindicated. However, we had no direct method of gauging disease severity with billing diagnosis codes alone.
A number of proxies for measuring disease severity have been proposed, though none have been validated in the setting of low back pain. The number of diagnoses included on a billing claim have been found to have some explanatory power in measuring disease severity in different settings, 38,39 though this measure alone is inadequate at explaining the variance in disease severity unless another source of clinical information can be incorporated to supplement claims data. In our study, the number of spine-related diagnosis codes included in the billing claim did capture some of the variance in disease severity. For example, those patients with one diagnosis code corresponding to a back pain diagnosis had an overall rate of lumbar surgery of 3.1%, those with two back pain diagnoses had an overall rate of lumbar surgery of 6.2%, those with three low back pain diagnoses had a rate of lumbar surgery of 9.2%, and those with four diagnoses had an overall lumbar surgery rate of 12.9%. The inclusion of this variable in the regression analysis did not significantly change the overall odds ratios reported above, suggesting that disease severity may play less of a role in our findings.
An additional limitation is that the Medicare Part B billing claims we used to capture PT visits are associated only with outpatient facilities. Hospital-based PT services are associated with Medicare Part A claims, which were not available for this analysis. However, hospital-based PT likely represents a small minority of PT services delivered. In fact, in one study evaluating PT use in acute low back pain using the Medicare Part A claims data, PT use was reported in only 0.2% of all patients with nonspecific low back pain, 40 suggesting that the Part A claims data represents only a small minority of the billing claims for total physical therapy delivered. Thus our study probably underestimates the true usage of PT following physician visits for acute low back pain to a small degree.
The distribution of diseases represented in this study may be different than in a group of younger patients, especially with respect to spinal stenosis, and variations in diagnosis may also represent diagnostic ambiguity or practitioner convention. 37 The results from this Medicare population may also not be generalized to a younger group of patients. The effect of patient expectations and preferences in the treatment of back pain was not able to be examined in this study. Patient expectations are likely to influence patient preference for surgical versus nonoperative treatment41 and this may drive provider decision regarding recommendations for physical therapy as well as overall therapy utilization rates. Finally, while we report outcomes related to the use of PT, this intervention is not a discrete and homogenous entity. Rather, a number of different types of physical therapy are available and in common practice, and this study does not differentiate specifically between them. A number of studies have proposed differential benefits for specific physical therapy interventions corresponding to specific patient populations, based either on diagnosis, specific exam maneuvers that elicit symptoms, or other criteria. 3,4,11,22
Conclusions
We have demonstrated a decreased usage of medical services in patients who receive PT early after an episode of acute low back pain. Our large cohort size suggests this is a robust finding. The medical specialty variations reported regarding PT usage in patients seen by generalists, surgeons, and other specialists, suggests that efforts to modify treatment practice be directed at those who are potentially underutilizing PT in this setting, namely those in the generalist specialties. This is especially important since those providers are also responsible for evaluating the largest proportion of patients with acute low back pain.
Key points
In patients who received physical therapy within 30 days after initial physician visit for low back pain, there was a decreased likelihood of receiving subsequent surgery or epidural steroid injections in the following year compared with those who received PT after 90 days.
The use of frequent office visits was significantly lower among patients who received PT within 30 days relative to those who received PT late.
Wide variation exists between medical specialties regarding the use of PT, with patients seen by generalist medical specialties receiving PT least often.
Acknowledgments
This research was supported by the NIH Intramural Research Program.
References
- 1.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb 1;344:363–370. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 2.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995 Jan 1;20:11–19. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003 Jul 1;28:1363–1371. doi: 10.1097/01.BRS.0000067115.61673.FF. [DOI] [PubMed] [Google Scholar]
- 4.Wand BM, Bird C, McAuley JH, Dore CJ, MacDowell M, De Souza LH. Early intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine. 2004 Nov 1;29:2350–2356. doi: 10.1097/01.brs.0000143619.34308.b4. [DOI] [PubMed] [Google Scholar]
- 5.Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine. 2001 Nov 15;26:2504–2513. doi: 10.1097/00007632-200111150-00022. [DOI] [PubMed] [Google Scholar]
- 6.Chou R, Qaseem A, Snow V, Casey D, Cross JTJ, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007 Oct 2;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 7.Malmivaara A, Hakkinen U, Aro T, Heinrichs ML, Koskenniemi L, Kuosma E, Lappi S, Paloheimo R, Servo C, Vaaranen V. The treatment of acute low back pain--bed rest, exercises, or ordinary activity? N Engl J Med. 1995 Feb 9;332:351–355. doi: 10.1056/NEJM199502093320602. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Diehl AK, Rosenthal M. How many days of bed rest for acute low back pain? A randomized clinical trial. N Engl J Med. 1986 Oct 23;315:1064–1070. doi: 10.1056/NEJM198610233151705. [DOI] [PubMed] [Google Scholar]
- 9.Skargren EI, Carlsson PG, Oberg BE. One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Subgroup analysis, recurrence, and additional health care utilization. Spine. 1998 Sep 1;23:1875–1883. doi: 10.1097/00007632-199809010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Pinnington MA, Miller J, Stanley I. An evaluation of prompt access to physiotherapy in the management of low back pain in primary care. Fam Pract. 2004 Aug;21:372–380. doi: 10.1093/fampra/cmh406. [DOI] [PubMed] [Google Scholar]
- 11.Fritz JM, Cleland JA, Brennan GP. Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists? Med Care. 2007 Oct;45:973–980. doi: 10.1097/MLR.0b013e318070c6cd. [DOI] [PubMed] [Google Scholar]
- 12.Pengel LHM, Refshauge KM, Maher CG, Nicholas MK, Herbert RD, McNair P. Physiotherapist-directed exercise, advice, or both for subacute low back pain: a randomized trial. Ann Intern Med. 2007 Jun 5;146:787–796. doi: 10.7326/0003-4819-146-11-200706050-00007. [DOI] [PubMed] [Google Scholar]
- 13.Fritz JM, Cleland JA, Speckman M, Brennan GP, Hunter SJ. Physical therapy for acute low back pain: associations with subsequent healthcare costs. Spine. 2008 Jul 15;33:1800–1805. doi: 10.1097/BRS.0b013e31817bd853. [DOI] [PubMed] [Google Scholar]
- 14.Cherkin DC, Deyo RA, Volinn E, Loeser JD. Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases. Spine. 1992 Jul;17:817–825. doi: 10.1097/00007632-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Carragee EJ. Clinical practice. Persistent low back pain. N Engl J Med. 2005 May 5;352:1891–1898. doi: 10.1056/NEJMcp042054. [DOI] [PubMed] [Google Scholar]
- 16.Staal JB, de Bie R, de Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. 2008:CD001824. doi: 10.1002/14651858.CD001824.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol. 2006 Apr 15;163:754–761. doi: 10.1093/aje/kwj100. [DOI] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Haigh R, Clarke AK. Effectiveness of rehabilitation for spinal pain. Clin Rehabil. 1999;13(Suppl 1):63–81. doi: 10.1191/026921599678132587. [DOI] [PubMed] [Google Scholar]
- 20.van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine. 1997 Sep 15;22:2128–2156. doi: 10.1097/00007632-199709150-00012. [DOI] [PubMed] [Google Scholar]
- 21.Tygiel PP, Anaya S, Porter A. A randomized trial of exercise therapy in patients with acute low back pain--efficacy on sickness absence. Spine. 1996 Feb 15;21:529–530. doi: 10.1097/00007632-199602150-00029. [DOI] [PubMed] [Google Scholar]
- 22.Machado LAC, de Souza MvS, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine. 2006 Apr 20;31:E254–62. doi: 10.1097/01.brs.0000214884.18502.93. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez-Urzelai V, Palacio-Elua L, Lopez-de-Munain J. Routine primary care management of acute low back pain: adherence to clinical guidelines. Eur Spine J. 2003 Dec;12:589–594. doi: 10.1007/s00586-003-0567-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bogefeldt J, Grunnesjo M, Svardsudd K, Blomberg S. Diagnostic differences between general practitioners and orthopaedic surgeons in low back pain patients. Ups J Med Sci. 2007;112:199–212. doi: 10.3109/2000-1967-194. [DOI] [PubMed] [Google Scholar]
- 25.Carey TS, Garrett J. Patterns of ordering diagnostic tests for patients with acute low back pain. The North Carolina Back Pain Project. Ann Intern Med. 1996 Nov 15;125:807–814. doi: 10.7326/0003-4819-125-10-199611150-00004. [DOI] [PubMed] [Google Scholar]
- 26.Wong WM, Lim P, Wong BCY. Clinical practice pattern of gastroenterologists, primary care physicians, and otolaryngologists for the management of GERD in the Asia-Pacific region: the FAST survey. J Gastroenterol Hepatol. 2004 Sep;19(Suppl 3):S54–60. doi: 10.1111/j.1440-1746.2004.03590.x. [DOI] [PubMed] [Google Scholar]
- 27.O’Neill L, Kuder J. Explaining variation in physician practice patterns and their propensities to recommend services. Med Care Res Rev. 2005 Jun;62:339–357. doi: 10.1177/1077558705275424. [DOI] [PubMed] [Google Scholar]
- 28.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007 Dec 20;357:2589–2600. doi: 10.1056/NEJMsa067735. [DOI] [PubMed] [Google Scholar]
- 29.Hannan EL, Popp AJ, Feustel P, Halm E, Bernardini G, Waldman J, Shah D, Chassin MR. Association of surgical specialty and processes of care with patient outcomes for carotid endarterectomy. Stroke. 2001 Dec 1;32:2890–2897. doi: 10.1161/hs1201.099637. [DOI] [PubMed] [Google Scholar]
- 30.Goodney PP, Lucas FL, Stukel TA, Birkmeyer JD. Surgeon specialty and operative mortality with lung resection. Ann Surg. 2005 Jan;241:179–184. doi: 10.1097/01.sla.0000149428.17238.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dimick JB, Goodney PP, Orringer MB, Birkmeyer JD. Specialty training and mortality after esophageal cancer resection. Ann Thorac Surg. 2005 Jul;80:282–286. doi: 10.1016/j.athoracsur.2005.01.044. [DOI] [PubMed] [Google Scholar]
- 32.Jackson JL, Browning R. Impact of national low back pain guidelines on clinical practice. South Med J. 2005 Feb;98:139–143. doi: 10.1097/01.SMJ.0000136261.21711.85. [DOI] [PubMed] [Google Scholar]
- 33.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J. 2005 Sep–Oct;5:530–541. doi: 10.1016/j.spinee.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 34.Chenot JF, Leonhardt C, Keller S, Scherer M, Donner-Banzhoff N, Pfingsten M, Basler HD, Baum E, Kochen MM, Becker A. The impact of specialist care for low back pain on health service utilization in primary care patients: a prospective cohort study. Eur J Pain. 2008 Apr;12:275–283. doi: 10.1016/j.ejpain.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 35.Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine. 2008;33:2923–2928. doi: 10.1097/BRS.0b013e31818a3167. [DOI] [PubMed] [Google Scholar]
- 36.Marras WS, Ferguson SA, Burr D, Schabo P, Maronitis A. Low back pain recurrence in occupational environments. Spine. 2007;32:2387–2397. doi: 10.1097/BRS.0b013e3181557be9. [DOI] [PubMed] [Google Scholar]
- 37.Chan L, Houck P, Prela CM, MacLehose RF. Using medicare databases for outcomes research in rehabilitation medicine. Am J Phys Med Rehabil. 2001 Jun;80:474–480. doi: 10.1097/00002060-200106000-00018. [DOI] [PubMed] [Google Scholar]
- 38.Melfi C, Holleman E, Arthur D, Katz B. Selecting a patient characteristics index for the prediction of medical outcomes using administrative claims data. J Clin Epidemiol. 1995 Jul;48:917–926. doi: 10.1016/0895-4356(94)00202-2. [DOI] [PubMed] [Google Scholar]
- 39.Wang PS, Walker A, Tsuang M, Orav EJ, Levin R, Avorn J. Strategies for improving comorbidity measures based on Medicare and Medicaid claims data. J Clin Epidemiol. 2000 Jun;53:571–578. doi: 10.1016/s0895-4356(00)00222-5. [DOI] [PubMed] [Google Scholar]
- 40.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006 Mar–Apr;7:143–150. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 41.Lurie JD, Berven SH, Gibson-Chambers J, Tosteson T, Tosteson A, Hu SS, Weinstein JN. Patient preferences and expectations for care: determinants in patients with lumbar intervertebral disc herniation. Spine. 2008;33:2663–2668. doi: 10.1097/BRS.0b013e31818cb0db. [DOI] [PMC free article] [PubMed] [Google Scholar]