Abstract
Evidence supports the role of temperament in the origins of psychiatric disorders. However, there are few data on associations between temperament and psychiatric disorders in early childhood. A community sample of 541 three-year old preschoolers participated in a laboratory temperament assessment, and caregivers were administered a structured diagnostic interview on preschool psychopathology. In bivariate analyses, temperamental dysphoria and low exuberance were associated with depression; fear, low exuberance, and low sociability were associated with anxiety disorders; and disinhibition and dysphoria were associated with oppositional defiant disorder. Although there were no bivariate associations between temperament and attention-deficit/hyperactivity disorder, disinhibition emerged as a unique predictor in multivariate analyses. Findings indicate that the pattern of relations between temperament and psychopathology in older youth and adults is evident as early as age 3.
Keywords: preschool, children, psychopathology, temperament, observation
There is growing interest in the area of developmental psychopathology on the role of temperament in the origins of psychiatric disorders (see Bijttebier & Roeyers, 2009; Frick, 2004). Temperament is generally defined as individual differences in emotional reactivity and regulation that appear early in life, are relatively stable, and are at least partly biologically based (Rothbart & Bates, 2006). Evidence supports the heritability and stability/continuity of temperamental traits, particularly from age three onward (Gagne, Vendlinski, & Goldsmith, 2009; Roberts & DelVecchio, 2000). While temperament refers to normal-range variations in emotion and behavior, psychopathology is characterized by pervasive and unregulated emotional and behavioral responses that occur in inappropriate contexts and lead to impairment (Goldsmith & Lemery, 2000).
There have been considerable advances in our understanding of the complex relations between temperament and psychopathology in youth (for reviews see Rothbart & Bates, 2006; Tackett, 2006). Nevertheless, a significant gap in the literature persists. Little work has examined associations between temperament traits and psychiatric disorders during early childhood. As individual differences in temperament are evident by the preschool period (Caspi & Shiner, 2006; Rothbart & Bates, 2006) and as growing evidence demonstrates that many psychiatric disorders can be identified in early childhood (Egger & Angold, 2006), it is important to determine whether temperament is associated with psychopathology in young children and if the pattern of associations is consistent with studies of older youth and adults.
Prior to addressing these questions, several conceptual and methodological issues must be considered. First, it is challenging to distinguish the constructs of temperament and psychopathology (Frick, 2004; Lahey, 2004), and this may pose particular difficulty in early childhood given the extensive and rapid changes in language, cognition, emotion, and social behavior during this period. These developmental changes often make it difficult to distinguish normative behaviors, including temperament traits, from clinically significant symptoms and disorders (Egger & Angold, 2006). Hence, developmentally appropriate research methods that are sensitive to the distinctions between temperament and psychopathology are needed to assess associations in early childhood.
Second, the majority of studies of younger children have used parent-report measures of both temperament and psychopathological symptoms, which may inflate associations by shared method variance. In addition, most parent-report temperament measures have items that overlap with measures of psychopathological symptoms (for more detail see Lemery, Essex, & Smider, 2002; Lengua, West, & Sadler, 1998), creating measurement confounds.1 While there have recently been important efforts to develop self-report measures of temperament that are distinct from psychiatric symptoms for older youth (Lahey et al., 2010), comparable measures for young children are not available.
Laboratory observational measures provide an alternative approach to assessing temperament in young children (Rothbart & Bates, 2006). Although more labor-intensive than parent-report measures, and limited to a single context and brief time-frame, laboratory observations of child temperament avoid the problem of shared method variance and reduce the overlap with measures of child psychopathology. Moreover, they offer an objective assessment of temperament by assessing behaviors of interest elicited by standardized, developmentally appropriate stimuli, facilitating comparisons with age-matched peers. The reliability, validity, and stability of laboratory observations suggest that they provide valid measures of child temperament (Durbin, Hayden, Klein, & Olino, 2007; Rothbart & Bates, 2006).
Third, it is only recently that structured diagnostic interviews for the assessment of psychopathology during early childhood have become available (e.g., Egger et al., 2006; Scheeringa & Haslett, 2010). Unlike symptom checklists, structured diagnostic interviews elicit the information necessary to make clinical diagnoses, which includes the nature, severity and duration of symptoms and subsequent impairment. Accumulating evidence supports the reliability and validity of structured diagnostic interviews in young children (e.g., Birmaher et al., 2008; Egger et al., 2006; Keenan et al., 1997; Lavigne et al., 2009; Luby et al., 2002).
In light of these considerations, our study assessed the associations between temperament and psychopathology in early childhood using independent methods designed to minimize overlap between constructs. Specifically, we examined the associations between observed temperament, assessed with a standardized, comprehensive laboratory-based battery, and psychopathology assessed with a structured diagnostic interview with parents and based on Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR; American Psychiatric Association, 2000) criteria in a large community sample of preschoolers.
Only a handful of cross-sectional (De Los Reyes et al., 2009; Luby et al., 2006; Scheeringa, Peebles, Cook, & Zeanah, 2001; Wakschlag et al., 2007) and longitudinal studies (Caspi et al., 1996; Hirshfeld-Becker et al., 2003) have examined temperament-psychopathology associations using observational measures of temperament-relevant behaviors and structured diagnostic interviews in young children. While these studies have made important contributions, several have not used standardized temperament measures, and most have focused on a single temperament dimension and/or a limited number of forms of psychopathology in clinic-referred or high-risk samples.
As part of an ongoing longitudinal study examining the role of temperament in risk for psychopathology, we assessed temperament traits in a large community sample of preschool-aged children using the Laboratory Temperament Assessment Battery (Lab-TAB; Goldsmith et al., 1995). The Lab-TAB is a comprehensive, developmentally appropriate observational assessment of temperament. Concurrent child psychopathology was assessed using a structured diagnostic interview with parents, the Preschool Age Psychiatric Assessment (PAPA; Egger, Ascher, & Angold, 1999). Like parent rating scales for temperament and psychopathology, diagnostic interviews can be biased by such factors as parents’ personality and psychopathology (Youngstrom, Izard, & Ackerman, 1999), parents’ lack of knowledge of developmental norms, and reliance on parents’ subjective judgments. However, the PAPA’s interviewer-based format aims to minimize such factors. Although the interviewer must adhere to the protocol and ask all required questions, s/he must also confirm the parent’s understanding of the question, elicit examples of relevant behaviors, and apply detailed guidelines for rating symptoms.
We anticipated that our findings would mirror the associations between temperament and psychopathology reported for older youth and adults. However, as the literature on young children is limited, we consider our hypotheses to be tentative and exploratory. Research on temperament and psychopathology in older youth and adults suggests that temperament traits related to sadness, fear/behavioral inhibition (BI), low exuberance, and low sociability are linked to internalizing disorders, and traits involving anger/frustration, high exuberance, and disinhibition are linked to externalizing disorders (for reviews see Nigg, 2006; Rothbart & Bates, 2006; Tackett, 2006). In terms of specific diagnoses, previous research suggests that high negative affect and low exuberance are associated with depression (e.g., Clark & Watson, 1991; Lonigan, Phillips, & Hooe, 2003); negative affect, specifically fear/BI, and low sociability are associated with anxiety disorders (Hirshfeld-Becker et al., 2003; Lonigan & Phillips, 2001); and high negative affect, specifically anger/frustration, high exuberance, and disinhibition are associated with the disruptive behavior disorders including oppositional defiant disorder (ODD) (Eisenberg et al., 2009; Stringaris, Maughan, & Goodman, 2010) and attention-deficit/hyperactivity disorder (ADHD) (Martel & Nigg, 2006). Hence, we tentatively hypothesized that we would find a similar pattern in our preschool-aged sample.
In addition, we explored the moderating role of gender on the relations between temperament and psychopathology. Although few sex differences in preschool psychopathology have been reported, other than possibly higher rates of disruptive behavior disorders in preschool boys than girls (Egger & Angold, 2006), there are well-documented gender differences emerging in later childhood and adolescence, including more externalizing disorders in boys and more internalizing disorders in adolescent girls, which may have their roots in early temperament-psychopathology associations. In addition, there are well-established gender differences in temperament traits: girls are better able to regulate and control their impulses than boys, and boys are slightly more exuberant and active and less shy, than girls (Else-Quest, Hyde, Goldsmith, & Van Hulle, 2006). It is possible that these sex differences influence early-emerging temperament-psychopathology associations. For example, the relation between control-related deficits and psychopathology may differ by gender (e.g., the relation between control-related deficits and internalizing disorders may be stronger for girls than for boys).
Method
Participants
A total of 559 three-year-old children (45.7% female) and their families participated in a study on temperament and risk for psychopathology, and parents of 541 children were interviewed with the PAPA. Respondents were primarily biological mothers (97.9%), and the remaining respondents were biological fathers, both parents, and a grandparent. Children’s mean age was 3.6 years (SD = 0.3). The mean ages of mothers and fathers were 35.9 years (SD = 4.4) and 38.3 years (SD = 5.4), respectively. Most parents were married (94.8%). Of the children, 86.9% were White/non-Hispanic and 9.1% were Hispanic. Of the families, 34.9% had one parent and 33.9% had two parents with college degrees.
Procedures
The Committees on Research Involving Human Subjects at Stony Brook University approved and oversaw the study procedures. Participants were recruited by calling families from commercial mailing lists. Families with a 3-year-old child living within 20 contiguous miles of Stony Brook, New York with at least one biological parent were eligible to participate. The primary caregiver was required to speak English, and children with significant medical disorders or developmental disabilities were excluded.. Written informed consent was obtained by parents after the procedures had been fully explained, and families were compensated $150.
Measures: Observations of Child Temperament
Laboratory Temperament Assessment Battery (Lab-TAB)
Each child and a parent visited the laboratory for a 2-hour observational assessment of temperament that included a standardized set of 12 episodes selected to elicit a range of temperament-relevant behaviors. Tasks were selected from the Lab-TAB (Goldsmith et al., 1995). Four subjects had incomplete data and were excluded from the analyses. To prevent carry-over effects, no episodes presumed to evoke similar affective responses occurred consecutively, and each episode was followed by a brief play break. The parent remained in the room with the child for all episodes except Stranger and Box Empty (see below), but was instructed not to interact with the child (except in Pop-Up Snakes). Each episode was videotaped and later coded. Experimenters/coders were unaware of all data on child psychopathology.
The episodes, in the order they occurred, were: (1) Risk Room. Child explored a set of novel and ambiguous stimuli, including a Halloween mask, balance beam, and black box; (2) Tower of Patience. Child and experimenter alternated turns in building a tower. The experimenter took increasing amounts of time before placing her block on the tower during each turn; (3) Arc of Toys. Child played independently with toys for five minutes before the experimenter asked the child to clean up the toys; (4) Stranger Approach. Child was left alone briefly in the room before a male accomplice entered, speaking to the child while slowly walking closer; (5) Make that Car Go. Child and experimenter raced remote-controlled cars; (6) Transparent Box. Experimenter locked an attractive toy in a transparent box, leaving the child alone with a set of non-working keys. After a few minutes, the experimenter returned and told the child that she had left the wrong set of keys. The child used the new keys to open the box and play with the toy; (7) Exploring New Objects. Child was given the opportunity to explore a set of novel and ambiguous stimuli, including a mechanical spider, a mechanical bird, and sticky soft gel balls; (8) Pop-up Snakes. Child and experimenter surprised the parent with a can of potato chips that actually contained coiled snakes; (9) Impossibly Perfect Green Circles. Experimenter repeatedly asked the child to draw a circle on a large piece of paper, mildly criticizing each attempt; (10) Popping Bubbles. Child and experimenter played with a bubble-shooting toy; (11) Snack Delay. Child was instructed to wait for the experimenter to ring a bell before eating a snack. The experimenter systematically increased the delay before ringing the bell; and (12) Box Empty. Child was given an elaborately wrapped box to open under the impression that a toy was inside.
Tape Coding Procedures
Coding procedures followed those reported in a previous study (Durbin, Klein, Hayden, Buckley, & Moerk, 2005). The scoring developed for these assessments has been related to home observations and demonstrated moderate stability over time in an independent sample (Durbin et al., 2007). The following temperament traits, emotional displays, and behaviors were rated: positive affect (PA), fear, sadness, anger, BI, inhibitory control, interest, activity, sociability, impulsivity, initiative, anticipatory PA, dominance, warmth, social interest, affiliation, assertiveness, clinginess, pushiness, hostility, noncompliance, avoidance, and social fear. Each variable was rated for all episodes except BI and inhibitory control.
Each display of facial, bodily and vocal affect (PA, fear, sadness, anger) in each episode was rated on a three-point scale (low, moderate, high). Ratings were summed separately within each channel (facial, bodily, vocal) across the 12 episodes, standardized, and summed across the three channels to derive total scores for each affect domain. With the exception of BI and inhibitory control, the other variables were rated once per episode on a four-, five-, or ten-point scale, and summed across episodes. Coefficient alphas ranged from .50-.87 (median = .70), and intraclass coefficients (ICCs) for interrater reliability ranged from .40-.92 (median = .75; n = 35).
BI was coded only in the three episodes designed to assess this behavior: Risk Room, Stranger Approach, and Exploring New Objects. Specific behaviors, such as latency to touch objects, tentative play, gaze aversion, latency to vocalize, and approach to and avoidance of stranger were coded for each epoch, which spanned 20–30 seconds depending on the particular episode. Within each epoch, a maximum intensity rating of facial, bodily, and vocal fear was also coded. Except for latencies, behaviors were coded on three- or four-point scales. BI was computed as the average of the standardized ratings across epochs and episodes. Coefficient alpha for the BI scale was .80 and the interrater ICC was .88 (n = 35).
Inhibitory control was coded in two episodes designed to assess this behavior: Tower of Patience and Snack Delay. The coding system was adapted from Carlson (2005), which involved tallying the number of times a child failed to wait his or her turn during the episode. Tower of Patience consisted of 14 trials, and Snack Delay consisted of seven trials. The composite global inhibitory control variable (α = .70, interrater ICC = .98, n = 8) was constructed by adding the standardized scores for the two episodes.
Principal Components Analysis (PCA) of Lab-TAB variables
To reduce the number of temperament variables listed above, a PCA was conducted followed by an oblique rotation.2 Based on the eigenvalue > 1.0 rule and inspection of the scree plot, five components were extracted. Each component was easily interpretable and included several theoretically relevant variables with loadings greater than .40 and few cross-loadings on multiple factors (see Table 1). Unit-weighted scores were derived for each child to yield five temperament scales: sociability/assertiveness (α = .93); dysphoria (α = .80); fear (α = .71); exuberance (α = .88); and disinhibition (α = .70). Items were not double-counted on scales: in the few cases where there were cross-loadings, the item was added to the scale with the higher loading. Interrater ICCs were acceptable for all scales: sociability/assertiveness (.82); dysphoria (.88); fear (.82), exuberance (.92), and disinhibition (.83). Correlations between the temperament factors are presented in Table 1.
Table 1.
Principal Components Analysis of Lab-TAB Variables and Correlations among Scales
| Components | |||||
|---|---|---|---|---|---|
| Lab-TAB variables | Sociability/ assertiveness | Dysphoria | Fear | Exuberance | Disinhibition |
| Sociability | .84 | .05 | .12 | .19 | −.08 |
| Initiative | .82 | .17 | −.06 | .05 | .12 |
| Dominance | .81 | .26 | −.03 | .07 | .17 |
| Assertiveness | .77 | .32 | .05 | .04 | .10 |
| Social Interest | .74 | −.06 | .05 | .36 | −.15 |
| Social fear | −.72 | .05 | .14 | .21 | −.15 |
| Affiliation | .59 | −.09 | .06 | .44 | .34 |
| Avoidance | −.67 | .30 | .01 | −.08 | .08 |
| Sadness | −.03 | .79 | .23 | −.02 | −.20 |
| Anger | .16 | .80 | −.07 | −.03 | −.05 |
| Hostility | −.07 | .77 | −.12 | .09 | .11 |
| Pushiness | .15 | .62 | .02 | .01 | .39 |
| BI | −.09 | −.04 | .86 | .01 | −.01 |
| Fear | .24 | −.01 | .85 | −.03 | −.02 |
| Clinginess | −.21 | .09 | .60 | −.02 | .28 |
| PA | −.03 | .06 | .05 | .94 | .07 |
| Anticipatory PA | −.10 | .04 | −.03 | .92 | .07 |
| Interest | .27 | −.12 | −.21 | .64 | .11 |
| Warmth | .35 | −.33 | .00 | .56 | −.28 |
| Activity | .32 | .05 | −.16 | .54 | .35 |
| Impulsivity | .15 | .17 | −.07 | .32 | .68 |
| Noncompliance | −.09 | .40 | .08 | −.21 | .58 |
| Inhibitory Control | .02 | −.15 | .10 | .00 | −.80 |
|
Correlations between Lab-TAB temperament scales | |||||
| Sociability/ | .24*** | −.10* | .63*** | .26*** | |
| Assertiveness | |||||
| Dysphoria | .19*** | −.09* | .57*** | ||
| Fear | −.27*** | .16*** | |||
| Exuberance | .02 | ||||
Note. Component loadings >.40 that were unit-weighted to form the scales are in bold. Lab-TAB = Laboratory Temperament Assessment Battery; PA = positive affect; BI = behavioral inhibition; NA = negative affect.
p < .05;
p < .001.
Measures: Parent-reported Child Psychopathology
Preschool Age Psychiatric Assessment (PAPA; Version 1.4)
As parents remained with the child during the Lab-TAB, PAPA interviews were conducted with the primary caretaker by telephone within several weeks of the visit. The PAPA is a diagnostic interview that provides a comprehensive assessment of DSM-IV-TR diagnoses during the past three months in 2–5 year old children (Egger et al., 1999). As discussed above, it uses a structured format and an interviewer-based approach and includes a detailed glossary that provides guidelines for rating symptom severity, frequency, duration, and impairment. Diagnoses are derived by computer using algorithms for DSM-IV-TR criteria (Egger et al., 1999). Adequate test-retest reliability has been reported using independent interviews (Egger et al., 2006). The following diagnostic groups were employed in the analyses: Depressive Disorder (major depression, dysthymia, and depression not otherwise specified); Anxiety Disorder (specific phobia, separation anxiety, social phobia, generalized anxiety, agoraphobia, panic, and selective mutism); ODD; and ADHD (see Table 2 for the rates in this sample).
Table 2.
Associations between Observed Child Temperament [M (Sd)]and Diagnostic Categories
| Depression | Anxiety | ODD | ADHD | |||||
|---|---|---|---|---|---|---|---|---|
| Present | Absent | Present | Absent | Present | Absent | Present | Absent | |
| Sociability/Assertiveness | −1.81(3.49) | .04(4.41) | −1.38(4.10) | .34(4.42) | .09(3.36) | .00(4.51) | −.03(2.51) | .01(4.44) |
| t(539) = −1.32 | t(539) = −3.65*** | t(539) = .14 | t(539) = −.03 | |||||
| Dysphoria | 2.12(6.55) | −.04(3.07) | .38(3.52) | −.09(3.08) | .89(3.61) | −.09(3.11) | −1.05(2.04) | .02(3.19) |
| t(539) = 2.13* | t(539) = 1.37 | t(539) = 2.11* | t(539) = −1.12 | |||||
| Fear | −.29(1.57) | .01(2.40) | .60(2.57) | −.15(2.32) | −.15(2.35) | .02(2.39) | −.28(2.14) | .01(2.39) |
| t(539) = −.39 | t(539) = 2.90** | t(539) = −.49 | t(539) = −.39 | |||||
| Exuberance | −3.26(4.42) | .05(4.14) | −1.70(4.63) | .40(3.94) | −.39(3.66) | .03(4.22) | .37(3.98) | −.02(4.17) |
| t(539) = −2.50* | t(539) = −4.72*** | t(539) = −.68 | t(539) = .31 | |||||
| Disinhibition | −.48(2.95) | .01(2.37) | −.04(2.50) | .01(2.36) | 1.15(2.23) | −.11(2.37) | 1.04(1.34) | −.02(2.39) |
| t(539) = −.65 | t(539) = −.192 | t(539) = 3.64*** | t(539) = 1.46 | |||||
| Rate of Disorder | ||||||||
| % (n) | 1.8 (10) | 19.6 (106) | 9.4 (51) | 2.0 (11) | ||||
p < .05;
p < .01;
p < .001;
Significant associations are in bold. Note: PAPA = Preschool Age Psychiatric Assessment; ODD = oppositional defiant disorder; ADHD = attention deficit/hyperactivity disorder.
Interviews were conducted by advanced graduate students in clinical psychology who received training on the administration of the PAPA from a member of the PAPA development team. Raters were unaware of all temperament data. Interviews generally lasted 1–2 hours. To examine interrater reliability, a second rater independently rated audiotapes of 21 PAPA interviews. Kappas were 1.00 for all diagnostic categories.
Early Childhood Inventory-4 (ECI-4)
The ECI-4 is a parent rating scale used to screen DSM-IV emotional and behavioral disorders in 3- to 6-year olds (Gadow & Sprafkin, 2000). Parents completed the ADHD and ODD sections of the inventory. The overall correct classification rates for ADHD and ODD with respect to chart diagnoses were 60% and 74%, respectively (Sprafkin, Volpe, Gadow, Nolan, & Kelly, 2002). In the present sample, coefficient alphas for the ECI-4 were .79 (ADHD-Inattention), .82 (ADHD-Hyperactivity/Impulsivity), and .85 (ODD).
To reduce administration time, for the first 60% of the sample (n = 324) the interviewer used the ECI-4 ADHD and ODD scales as a screen to help determine whether to complete the ADHD and ODD sections of the PAPA. The interviewer also confirmed the absence of the cardinal ADHD and ODD symptoms with the parent. If evidence from the screener and these queries indicated the child was very unlikely to meet diagnostic criteria, then the section(s) was skipped. In the remaining 40% of the sample (n = 217), the full PAPA ADHD and ODD sections were administered to all caregivers. Results were similar when analyses were limited to the 40% of the sample who received the complete PAPA.
Results
Associations with Demographic Variables
First, we examined associations between the five temperament scales and demographic variables, including child sex, race/ethnicity, and parental education level. Girls (M = .30, SD = 2.42) displayed more fear than boys (M = −.25, SD = 2.33), t(539) = −2.72, p < .01. In contrast, boys (M = .58, SD = 2.45) exhibited more disinhibition than girls (M = −.68, SD = 2.10), t(539) = 6.34, p < .001; boys (M = .26, SD = 3.46) also exhibited more dysphoria than girls (M = −.30, SD = 2.77), t(539) = 2.03, p < .05. Temperament was not associated with child race/ethnicity. Children with at least one parent who graduated from college showed less dysphoria (M = −.20, SD = 2.87) than children who did not have a parent who graduated college (M = .44, SD = 3.70), t(539) = −2.23, p < .05.
Diagnoses were not associated with child sex and race/ethnicity. Of the families where neither parent graduated college, a larger percentage of children had an anxiety disorder (25.1%, 44/175) than children of families where at least one parent graduated college (16.9%, 62/366), χ2 (1, N = 541) = 5.06, p < .05. As parental education was associated with both child dysphoria and anxiety disorders, analyses involving these two variables were repeated controlling for parental education. The results were identical to analyses that did not control for parental education.
Associations between Child Temperament and Diagnoses
Table 2 shows the associations between the five temperament scales and the four diagnostic categories. Higher levels of dysphoria (Cohen d = .18) and lower levels of exuberance (d = .22) were significantly associated with a depression diagnosis. Higher levels of fear (d = .25) and lower levels of sociability (d = .31) and exuberance (d = .41) were significantly associated with an anxiety disorder diagnosis. Higher levels of dysphoria (d = .18) and disinhibition (d = .31) were significantly associated with an ODD diagnosis. No temperament traits were significantly associated with an ADHD diagnosis.
Next, a series of logistic regression analyses were conducted to examine the unique associations between the temperament variables and each diagnostic category. The five temperament scales were entered simultaneously as independent variables (IVs) in each model. Dysphoria was uniquely associated with a depression diagnosis, Odds Ratio (OR) = 1.24, 95% confidence interval (CI) = 1.02–1.50, p < .05. Low exuberance was associated with an anxiety disorder diagnosis at a trend level, OR = .94, CI = .88–.1.01, p = .07. Disinhibition was uniquely associated with an ODD diagnosis, OR = 1.24, CI = 1.08–1.42, p < .01. Lastly, disinhibition was uniquely associated with an ADHD diagnosis, OR = 1.42, CI = 1.10–1.85, p < .01, and low dysphoria was associated with ADHD at a trend level, OR = .70, CI = .49–1.01, p = .06.
We also examined the relation between temperament and comorbidity, as indexed by the interaction between pairs of diagnoses. There was only one significant interaction between a pair of diagnoses and a temperament dimension: ODD and depression with dysphoria, β = −.14, t(540) = −2.54, p < .05. Posthoc LSD pairwise comparisons showed higher levels of dysphoria were found in children with depression only (M = 3.78, SD = 8.29) than in children with ODD only (M = 1.00, SD = 3.74), children with comorbid ODD and depression (M = −.38, SD = .57), and children with neither diagnosis (M = −.14, SD = 2.99), p < .05; children with ODD only exhibited significantly more dysphoria than children with neither diagnosis, p < .05. Finally, we examined interactions between each pair of temperament scales with each of the four diagnostic groups: none of the temperament trait by temperament trait interactions was significant.
Relations among Child Temperament, Sex, and Diagnosis
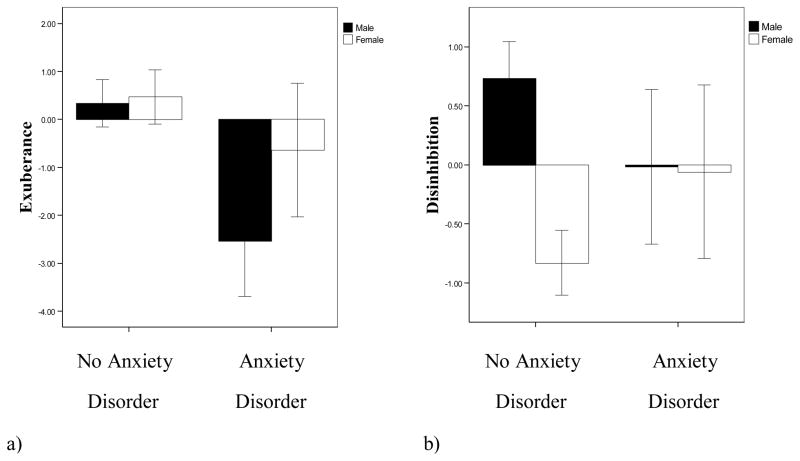
To examine whether child sex influences the relation between temperament and psychopathology, logistic regression analyses were conducted with the temperament scales, sex, and the temperament by sex interaction terms entered as IVs and each diagnosis as the dependent variable. Sex significantly moderated the associations of two temperament scales with an anxiety disorder diagnosis (see Figure 1).
Figure 1.
Associations between temperamental (a) exuberance and (b) disinhibition and preschoolers’ anxiety disorder diagnosis by child sex: boys with an anxiety disorder (n = 59); boys without an anxiety disorder (n = 235); girls with an anxiety disorder (n = 47); girls without anxiety (n = 200).
First, there was a significant exuberance by sex interaction, OR = 1.12, CI = 1.01–1.24, p < .05. LSD pairwise comparisons revealed that boys with an anxiety disorder showed significantly less exuberance (M = −2.54, SD = 4.42) than boys without an anxiety disorder (M = .33, SD = 3.86), and girls with (M = −.64, SD = 4.73) and without an anxiety disorder (M = .47, SD = 4.05).
Second, sex moderated the association of disinhibition with an anxiety disorder, OR = 1.35, CI = 1.11–1.63, p < .01. LSD pairwise comparisons indicated that boys without (M = .73, SD = 2.42) an anxiety disorder were significantly more disinhibited than boys with (M = −.02, SD = 2.51) an anxiety disorder, and girls with (M = −.06, SD = 2.50) and without (M = −.82, SD = 1.97) an anxiety disorder. In addition, boys with an anxiety disorder were significantly more disinhibited than girls without an anxiety disorder, and girls with an anxiety disorder were significantly more disinhibited than girls without an anxiety disorder.3
Discussion
The goal of this study was to examine associations between temperament and psychiatric disorders in early childhood. We assessed the relations between a range of temperament dimensions using a comprehensive laboratory-based measure and a range of psychiatric disorders using a structured diagnostic interview in a large sample of non-referred preschoolers. Preschoolers’ observed temperament traits demonstrated small-medium sized associations with parents’ reports of their children’s psychopathology.
The pattern of these associations was generally consistent with prior research in older youth and adults and studies largely relying on parent-report checklists of temperament and symptomatology. Our findings extend this work to younger children and to other approaches of assessing temperament and psychopathology. It has been hypothesized that high NE, low approach-related behaviors, and high withdrawal-related behaviors are associated with internalizing disorders (Clark & Watson, 1991; Tackett, 2006). In particular, low-approach behaviors, such as low exuberance, have been linked to depressive disorders, and behavioral inhibition/shyness has been linked to anxiety disorders; nevertheless, there is some overlap among these associations (Anderson & Hope, 2008). Our findings are generally, but not entirely, consistent with this pattern. We found that dysphoria and low exuberance were associated with depressive disorders, and fear/inhibition, low sociability, and low exuberance were associated with anxiety disorders in bivariate analyses. Contrary to the majority of findings in older youth and adults using inventories, our bivariate analyses indicated that low exuberance, rather than high dysphoria, was common to both depression and anxiety. More research is needed to elucidate associations between low exuberance, or low PA, and anxiety disorders and whether associations may reflect developmental factors or measurement differences. Moreover, associations between low exuberance and both depression and anxiety in early childhood may provide insight into the origins of the developmental pathways between anxiety and depression (Copeland, Shanahan, Egger, & Angold, 2009) and the high comorbidity between the two disorders (Shankman & Klein, 2003).
With respect to externalizing disorders, past research has reported negative associations between behavioral control/constraint, or effortful control, and children’s disruptive behavior disorders, including conduct problems (Eisenberg et al., 2009) and ADHD (Martel, 2009). Our findings are consistent with this work as ODD was correlated with disinhibition, which tapped low inhibitory control, impulsivity, and noncompliance. In addition, both ODD and ADHD were uniquely associated with disinhibition in the multivariate analyses. ODD was also characterized by higher dysphoria, which is consistent with findings linking anger/irritability to oppositional behavior problems (De Pauw & Mervielde, 2010), and growing evidence for the role of negative emotionality and emotion dysregulation in the development and course of ODD (Stringaris et al., 2010). The trend association between low dysphoria and ADHD in the multivariate analyses was unexpected, as ADHD has generally been linked to higher NE (Martel, 2009). We are reluctant to interpret this finding, as it did not emerge in the bivariate analyses and could reflect a weak suppression effect of another temperament trait.
We also explored whether these relations varied as a function of other disorders and other temperament traits. There was no evidence for interactions between temperament dimensions in the associations with diagnoses. Moreover, only one significant interaction involving temperament and pairs of disorders emerged. We found that children with depression only showed higher levels of dysphoria than children with comorbid ODD and depression, children with ODD only, and children with neither diagnosis; children with ODD only showed more dysphoria than children with neither diagnosis. Our findings suggest that dysphoria is more strongly associated with depression than ODD and that the presence of comorbid ODD is associated with less dysphoria in depressed preschoolers. It appears that comorbid depression and ODD may be more similar to pure ODD than pure depression, which is consistent with longitudinal findings demonstrating that depressed children comorbid with conduct problems were at lower risk for depression in adulthood than depressed children without conduct problems (Harrington, Fudge, Rutter, Pickles, & Hill, 1991).
We also investigated whether gender moderated temperament-psychopathology associations in preschoolers. Two significant findings emerged. Boys who were reported by their parents to have an anxiety disorder demonstrated more behavioral manifestations of low approach and high control. Specifically, boys with an anxiety disorder showed less exuberance compared to boys without an anxiety disorder and girls with and without an anxiety disorder. Boys with an anxiety disorder also showed lower levels of disinhibition than boys without an anxiety disorder. In contrast to boys, girls with an anxiety disorder demonstrated greater disinhibition than girls without an anxiety disorder. However, boys and girls with anxiety disorders exhibited similar levels of disinhibition.
These findings suggest that there may be sex-specific links between temperament and anxiety disorders. For boys, low exuberance and high control may predispose to anxiety disorders, or reflect a “shutting down”, or emotionally constricted/behaviorally overcontrolled, pattern of coping with anxiety. In contrast, for girls disinhibition may predispose to anxiety disorders, perhaps through effects on emotion regulation deficits. Girls with anxiety disorders may have difficulty disengaging attention from threatening stimuli, which may maintain and further exacerbate anxious and negative affective states (Lonigan, Vasey, Phillips, & Hazen, 2004). This is consistent with findings in older youth demonstrating associations between lower levels of control-related processes, such as effortful or attentional control, and anxiety (e.g., Meesters, Muris, & van Rooijen, 2007). Alternatively, it is possible that parents may be more likely to recognize and report anxiety in young boys and girls with these gender-specific patterns of behavior.
The distinction between temperament and psychopathology is a challenging conceptual and methodological problem (Frick, 2004; Lahey, 2004; Tackett, 2006). However, efforts are being made to address these challenges. For instance, Rapee and Coplan (2010) recently reviewed evidence supporting the distinction between fearful temperament and anxiety disorder, including the finding that many highly fearful children and adults do not meet criteria for an anxiety disorder and that psychological interventions may have stronger effects on anxiety disorders than fearful temperaments.
Our findings, along with previous research in older youth (e.g., Lahey et al, 2010; Lemery et al., 2002; Lengua et al., 1998), suggest that there are systematic associations between the domains of temperament and psychopathology even after significant efforts are made to remove methodological confounds. However, some degree of overlap is inherent in the nature of the constructs. For instance, our observational assessment of temperament included positive affect, fear, sadness, anger, noncompliance, and impulsivity, all of which coincide somewhat with various psychopathological symptoms. Our diagnostic interview aimed to minimize this overlap by assessing whether symptomatic variants of these emotions and behaviors are present in multiple contexts, are intrusive/distressing, and cause impairment. Nevertheless, defining the boundaries between the constructs continues to be a problem that will not be easily resolved.
It is also important to consider that the associations between traits and disorders may vary depending on sample characteristics. For example, in treatment seeking samples of preschoolers with observed high levels of BI, studies have reported that as many as 90–100% met criteria for an anxiety disorder (Kennedy et al., 2009; Rapee et al., 2005). However, using similar observational methods in our community sample, we found small to moderate correlations between our factors capturing aspects of BI (low sociability and high fear) and an anxiety disorder diagnosis. This is consistent with research demonstrating that trait-psychopathology relations may differ depending on clinic referred vs. non-referred samples and may be stronger in referred samples (Van Leeuwen, Mervielde, De Clercq, & Fruyt, 2007). Thus, more work on the relations between temperament and psychopathology is needed in both clinical and nonclinical samples across development.
Our study had several important strengths. We used independent methods to assess both temperament and psychiatric disorders in preschoolers. In addition, we used both a comprehensive laboratory-based assessment of temperament and a comprehensive diagnostic interview. The size of the sample was also much larger than most previous studies, allowing us to examine interactions between disorders and traits and with gender.
However, the study also had several limitations. First, laboratory observations of children’s temperament rely on a single occasion and setting, which precludes an assessment of traits across contexts and over time. However, findings have supported the validity of similar observational approaches in predicting behavior in naturalistic settings and at later points in development (Caspi, 2000; Durbin et al., 2007). Second, the taxonomy of temperament during early childhood remains unclear, which poses difficulties in comparing findings across studies. In this study, a PCA yielded five factors, which overlapped with the factors identified in previous reviews of the structure of personality and temperament in youth (Caspi & Shiner, 2006; De Pauw & Mervielde, 2010; Rothbart & Bates, 2006). Third, the classification of psychopathology in young children is also a nascent area, and the diagnostic instruments used to assess preschoolers’ problem behaviors are fairly new and still being investigated. Fourth, the sample was largely white and middle class. Future studies should examine these associations in more diverse samples. Fifth, despite having a fairly large number of participants, the number of cases with some disorders was small owing to the use of a non-referred sample. Sixth, the study was cross-sectional and cannot untangle the direction of associations. Finally, given the limited literature on temperament and psychopathology in young children, the study was somewhat exploratory, and future research would benefit from a more theoretically driven approach.
Implications for Research, Policy, and Practice
Understanding the relations between temperament and psychopathology in young children is critical, as temperament appears to directly and indirectly influence social development, may contribute to the development and course of psychiatric disorders, and could be useful in treatment planning (Rothbart & Bates, 2006; Tackett, 2006; Zinbarg, Uliaszek, & Adker, 2008). Moreover, greater understanding of these associations may be useful in identifying at-risk populations, guiding the development of preventive and early interventions, and elucidating the distinct and shared etiological factors between disorders and within the same disorder. For instance, research on temperament-psychopathology associations may elucidate the heterogeneity within disorders, which may allow us to develop more tailored interventions. Lastly, our findings suggest that the pattern of associations between temperament and psychopathology that has been reported in older youth and adults is also evident in early childhood, indicating that these relations may have considerable continuity over time.
Acknowledgments
This work was supported by NIMH RO1-MH069942 (DNK) and GCRC Grant M01-RR10710 to Stony Brook University from the National Center for Research Resources.
Footnotes
We do not wish to disparage parent report measures of child temperament in general, as they have a number of significant strengths, including time-efficiency, low cost, and capitalizing on the parent’s knowledge of the child’s behavior across contexts and over time. Our point is simply that parent report measures have limitations in addressing the specific question of the association between temperament and psychopathology in young children.
The structure of personality using observational methods is largely unexplored (Zentner & Bates, 2008), and there continue to be inconsistencies in the literature on the structure of temperament in early childhood using parent-reports (De Pauw, Mervielde & Leeuwan, 2009; De Pauw & Mervielde, 2010). Therefore, we employed an exploratory, rather than confirmatory, approach to reduce the number of observed temperament indicators (i.e., PCA).
Given the lack of clear boundaries for determining clinical diagnoses in preschoolers (Egger & Angold, 2006), we examined temperament-psychopathology associations using both DSM-IV-TR diagnoses and symptom scale scores based on the PAPA. Findings were relatively consistent across approaches.
The authors have no conflicts of interest to disclose.
References
- Anderson ER, Hope DA. A review of the tripartite model for understanding the link between anxiety and depression in youth. Clinical Psychology Review. 2008;28:275–287. doi: 10.1016/j.cpr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Press; 2000. text revision. [Google Scholar]
- Bijttebier P, Roeyers H. Temperament and vulnerability to psychopathology: Introduction to the special section. Journal of Abnormal Child Psychology. 2009;37:305–308. doi: 10.1007/s10802-009-9308-2. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, et al. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children–A preliminary psychometric study. Journal of Psychiatric Research. 2008;43:680–686. doi: 10.1016/j.jpsychires.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson SM. Developmentally sensitive measures of executive function in preschool children. Developmental Neuropsychology. 2005;28:595–616. doi: 10.1207/s15326942dn2802_3. [DOI] [PubMed] [Google Scholar]
- Caspi A. The child is father of the man: Personality continuities from childhood to adulthood. Journal of Personality and Social Psychology. 2000;78:158–172. doi: 10.1037//0022-3514.78.1.158. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Caspi A, Shiner RL. Personality development. In: Damon W, Lerner R, Eisenberg N, editors. Handbook of child psychology, sixth edition: Social, emotional, and personality development. Vol. 3. New York: John Wiley; 2006. pp. 300–365. [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shahan L, Costello J, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Henry DB, Tolan PH, Wakschlag LS. Linking informant discrepancies to observed variations in young children’s disruptive behavior. Journal of Abnormal Child Psychology. 2009;37:637–652. doi: 10.1007/s10802-009-9307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Pauw SSW, Mervielde I. Temperament, personality, and developmental psychopathology: A review based on the conceptual dimensions underlying childhood traits. Child Psychiatry and Human Development. 2010;41:313–329. doi: 10.1007/s10578-009-0171-8. [DOI] [PubMed] [Google Scholar]
- De Pauw SSW, Mervielde I, Van Leeuwen KG. How are traits related to problem behavior in preschoolers? Similarities and contrasts between temperament and personality. Journal of Abnormal Child Psychology. 2009;37:309–325. doi: 10.1007/s10802-008-9290-0. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, Moerk KC. Temperamental emotionality in preschoolers and parental mood disorders. Journal of Abnormal Psychology. 2005;114:28–37. doi: 10.1037/0021-843X.114.1.28. [DOI] [PubMed] [Google Scholar]
- Durbin CE, Hayden EP, Klein DN, Olino TM. Stability of laboratory-assessed temperamental emotionality traits from ages 3 to 7. Emotion. 2007;7:388–399. doi: 10.1037/1528-3542.7.2.388. [DOI] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Egger HL, Ascher BH, Angold A. The Preschool Age Psychiatric Assessment: Version 1.1. Durham, NC: Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center; 1999. [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Valiente C, Spinrad TA, Cumberland A, Liew J, Reiser M, et al. Longitudinal relations of children’s effortful control, impulsivity, and negative emotionality to their externalizing, internalizing and co-occurring behavior problems. Developmental Psychology. 2009;45:988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Else-Quest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperament: A Meta-Analysis. Psychological Bulletin. 2006;132:33–72. doi: 10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Special section: Temperament and childhood psychopathology. Integrating research on temperament and childhood psychopathology: Its pitfalls and promise. Journal of Clinical Child and Adolescent Psychology. 2004;33:2–7. doi: 10.1207/S15374424JCCP3301_1. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Early Childhood Inventory - 4: Screening Manual. Stony Brook, NY: Checkmate Plus; 2000. [Google Scholar]
- Gagne JR, Vendlinski MK, Goldsmith HH. The genetics of childhood temperament. In: Kim Y-K, editor. Handbook of behavior genetics. New York, NY: Springer; 2009. pp. 251–267. [Google Scholar]
- Goldsmith HH, Lemery KS. Linking temperamental fearfulness and anxiety symptoms: A behavior-genetic perspective. Biological Psychiatry. 2000;48:1199–1209. doi: 10.1016/s0006-3223(00)01003-9. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Reilly J, Lemery KS, Longley S, Prescott A. Laboratory Temperament Assessment Battery: Preschool version. Unpublished manuscript 1995 [Google Scholar]
- Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of childhood and adolescent depression: II. Links with antisocial disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:434–439. doi: 10.1097/00004583-199105000-00013. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Biederman J, Calltharp S, Rosenbaum ED, Rosenbaum JF. Behavioral inhibition and disinhibition as hypothesized precursors to psychopathology: Implications for pediatric bipolar disorder. Biological Psychiatry. 2003;53:985–999. doi: 10.1016/s0006-3223(03)00316-0. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannelli J. DSM-III-R disorders in preschool children from low-income families. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:620–627. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Kennedy SJ, Rapee RM, Edwards SL. A selective intervention program for inhibited preschool-aged children of parents with an anxiety disorder: Effects on current anxiety disorders and temperament. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:602–609. doi: 10.1097/CHI.0b013e31819f6fa9. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Commentary: Role of temperament in developmental models of psychopathology. Journal of Child and Adolescent Clinical Psychology. 2004;33:88–93. doi: 10.1207/S15374424JCCP3301_9. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Tackett JL, Waldman ID. Psychometrics of a self-report version of the child and adolescent dispositions scale. Journal of Clinical Child & Adolescent Psychology. 2010;39:351–361. doi: 10.1080/15374411003691784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavigne JV, LeBailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, Depression, and Anxiety in a community sample of 4-year-olds. Journal of Clinical Child & Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Lemery KS, Essex MJ, Smider NA. Revealing the relation between temperament and behavior problem symptoms by eliminating measurement confounding: Expert ratings and factor analyses. Child Development. 2002;73:867–882. doi: 10.1111/1467-8624.00444. [DOI] [PubMed] [Google Scholar]
- Lengua LJ, West SG, Sandler IN. Temperament as a predictor of symptomatology in children: Addressing contamination of measures. Child Development. 1998;69:164–181. [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM. Temperamental basis of anxiety disorders in children. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. Oxford University Press; 2001. pp. 60–91. [Google Scholar]
- Lonigan CJ, Phillips BM, Hooe ES. Tripartite model of anxiety and depression in children: evidence from a latent variable longitudinal study. Journal of Consulting and Clinical Psychology. 2003;71:465–481. doi: 10.1037/0022-006x.71.3.465. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW, Phillips BM, Hazen RA. Temperament, anxiety, and the processing of threat-relevant stimuli. Journal of Clinical Child and Adolescent Psychology. 2004;33:8–20. doi: 10.1207/S15374424JCCP3301_2. [DOI] [PubMed] [Google Scholar]
- Luby JL, Heffelfinger AK, Mrakotsky C, Hessler MJ, Brown KM, Hildebrand T. Preschool major depressive disorder: Preliminary validation for developmentally modified DSM-IV criteria. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Luby JL, Sullivan J, Belden A, Stalets M, Blankenship S, Spitznagel E. An observational analysis of behavior in depressed preschoolers: Further validation of early-onset depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:203–212. doi: 10.1097/01.chi.0000188894.54713.ee. [DOI] [PubMed] [Google Scholar]
- Martel MM. Research review: A new perspective on attention-deficit/hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry. 2009;50:1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT. Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. Journal of Child Psychology and Psychiatry. 2006;47:1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- Meesters C, Muris P, can Rooijen B. Relations of neuroticism and attentional control with symptoms of anxiety and aggression in non-clinical children. Journal of Psychopathology and Behavioral Assessment. 2007;29:149–158. [Google Scholar]
- Nigg JT. Temperament and developmental psychopathology. Journal of Child Psychology and Psychiatry. 2006;47:395–422. doi: 10.1111/j.1469-7610.2006.01612.x. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy S, Ingram M, Edwards S, Sweeney L. Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology. 2005;73:488–497. doi: 10.1037/0022-006X.73.3.488. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Coplan RJ. Conceptual relations between anxiety disorder and fearful temperament. In: Gazelle H, Rubin KH, editors. Social anxiety in childhood: Bridging developmental and clinical perspectives. New Directions for Child and Adolescent Development. Vol. 127. San Francisco: Josey-Bass; 2010. pp. 17–31. [DOI] [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Bates JE. Temperament in children’s development. In: Damon W, Lerner R, Eisenberg N, editors. Handbook of child psychology, sixth edition: Social, emotional, and personality development. Vol. 3. New York: John Wiley; 2006. pp. 99–166. [Google Scholar]
- Scheeringa MS, Haslett N. The Reliability and Criterion Validity of the Diagnostic Infant and Preschool Assessment: A New Diagnostic Instrument for Young Children. Child Psychiatry and Human Development. 2010;41:299–312. doi: 10.1007/s10578-009-0169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Peebles CD, Cook CA, Zeanah CH. Toward establishing procedural, criterion, and discriminant validity for PTSD in early childhood. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:52–60. doi: 10.1097/00004583-200101000-00016. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Klein DN. The relation between depression and anxiety: An evaluation of the tripartite, approach-withdrawal and valence-arousal models. Clinical Psychology Review. 2003;23:605–637. doi: 10.1016/s0272-7358(03)00038-2. [DOI] [PubMed] [Google Scholar]
- Sprafkin J, Volpe RJ, Gadow KD, Nolan EE, Kelly K. A DSM-IV-referenced screening instrument for preschool children: The Early Childhood Inventory-4. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:604–612. doi: 10.1097/00004583-200205000-00018. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B, Goodman R. What’s a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: Findings from the Avon longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:474–483. doi: 10.1097/00004583-201005000-00008. [DOI] [PubMed] [Google Scholar]
- Tackett JL. Evaluating models of the personality-psychopathology relationship in children and adolescents. Clinical Psychology Review. 2006;26:584–599. doi: 10.1016/j.cpr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Van Leeuwen KG, Mervielde I, De Clercq BJ, De Fruyt F. Extending the spectrum idea: Child personality, parenting and psychopathology. European Journal of Personality. 2007;21:63–89. [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Carter AS, Hill C, Danis B, Keenan K, et al. A developmental framework for distinguishing disruptive behavior from normative misbehavior in preschool children. Journal of Child Psychology and Psychiatry. 2007;48:976–987. doi: 10.1111/j.1469-7610.2007.01786.x. [DOI] [PubMed] [Google Scholar]
- Youngstrom E, Izard C, Ackerman B. Dysphoria-related bias in maternal ratings of children. Journal of Consulting and Clinical Psychology. 1999;67:905–916. doi: 10.1037//0022-006x.67.6.905. [DOI] [PubMed] [Google Scholar]
- Zentner M, Bates JE. Child temperament: An integrative review of concepts, research programs and measures. European Journal of Developmental Science. 2008;2:7–37. [Google Scholar]
- Zinbarg RE, Uliaszek AA, Adler JM. The role of personality in psychotherapy for anxiety and depression. Journal of Personality. 2008;76:1649–1688. doi: 10.1111/j.1467-6494.2008.00534.x. [DOI] [PubMed] [Google Scholar]