Abstract
Fibrous dysplasia (FD) and aneurysmal bone cyst (ABC) are uncommon benign intraosseous lesions. Simultaneous occurrence of both lesions is extremely rare. We present an example of concomitant FD and ABC in a 7 year-old with left eye blindness and discharge of one month duration. Physical examination revealed a proptotic left eye and bulging of the hard palate. CT and MRI are consistent with FD and ABC that involved the sphenoid and ethmoidal bones bilaterally. Incomplete combined endonasalcranial resection was performed. The patient presented five months postoperatively with a large recurrence and subsequent follow up was lost. Concomitant FD with ABC may occur in paranasal sinuses and may develop rapidly and exhibit locally aggressive behavior.
Introduction
Fibrous dysplasia (FD) consists of rare and benign osseous lesions of unknown etiology. They represent 2.5% of all bone tumors and 7% of benign bone tumors [1], in young, predominantly male patients [2,3]. The salient pathological feature of FD consists of the replacement of medullary bone by histologically benign fibro-osseous tissue [2]. FD may present as monostotic (70%), polystotic (30%), or as the main feature of McCune-Albright syndrome [4]. Craniofacial bones can be affected by monostotic (25%-30%) and polystatic (in 50%) lesions [5]. The most affected craniofacial bones are maxilla, mandible, frontal, sphenoid and temporal bones [6].
Aneurysmal bone cyst (ABC) is rare, benign vascular lesion, and considered secondary to certain pathological bone lesions [7]. ABC represents approximately 1.4% of all bone tumors, and only 3% among those are located in the cranium [8]. These lesions occur most commonly in patients under 20 years old of both genders [8]. Radiographs reveal an eccentric, lytic lesion typically with an expanded, remodeled "blown-out" or "ballooned" bony contour of the affected bone, with a delicate trabeculated appearance frequently. Fluid-filled spaces are common and may be seen on CT scans and MR images [7].
Concomitant FD and ABC are extremely rare with only 13 cases reported previously [9-12]. The clinical presentation of both FD and ABC depends on their location and the extent of involvement. The majority of reported cases are predominant in male children and young adults that are presented with symptomatic or asymptomatic mass. The development of ABC in FB may hastens the course of presentation [12]. In general, a complete excision of these lesions is recommended, and reports of aggressive behavior are occasionally found.
We report a rare example of concomitant FD and ABC of the skull base that presented with blindness and rapid local recurrence in a 7 year-old female patient. Also, we are presenting the multidisciplinary team approach of treating such cases.
Case report
A 7 year-old female, is presented at a local hospital with left eye blindness and discharge of one-month duration.
Physical examination showed a slightly proptotic left eye with no light perception, absence of direct pupil reflex and optic nerve atrophy in the left eye. In addition to, a slight hypertelorism. Otolaryngologic examination showed rhinorhea, bulging hard palate, and a left nasal mass (Figure 1).
Figure 1.
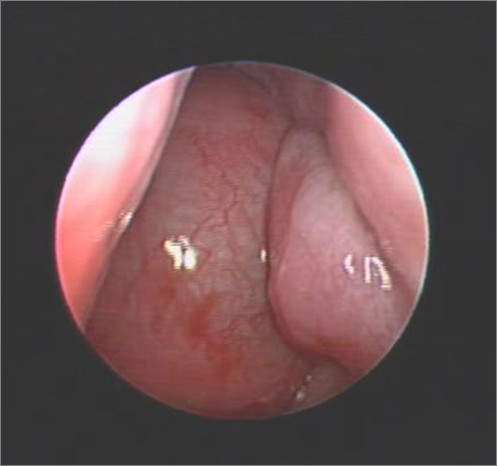
Endoscopic nasal view of left nostril, revealed huge nasal mass that occupied the whole cavity and reach to the level of inferior turbinate.
Preoperative CT findings (Figure 2, A) were consistent with fibrous dysplasia involving the sphenoid, ethmoidal sinuses, and posterior aspect of the nasal cavity as well as, the left maxillary sinus and the left optic foramen. Large expansible cystic spaces were also noticed in the lesion on preoperative MRI (Figure 3). Endoscopic biopsies revealed fibrous dysplasia with vascular component that were associated with significant and difficult to control bleeding.
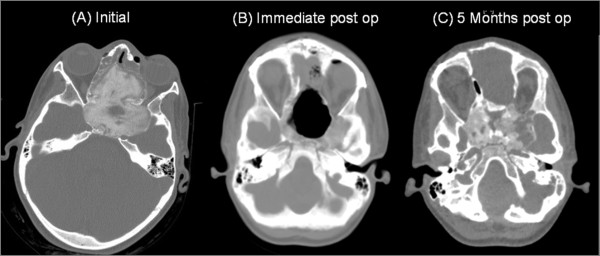
Figure 2.
Series CT scans of the tumor. (A) preoperative CT revealing ground glass appearance is consistent with fibrous dysplasia affecting of the sphenoid bone, ethmoidial bones, LT maxillary sinus, involving the optic foramen and harboring cystic expansible component. (B) Immediate post operative CT scan. (C) 5 months post operative follow up CT scan.
Figure 3.

Preoperative Axial T2 of the skull base revealed multiple fluid-fluid levels with hemorrhagic areas (white arrow) are consistent with associated aneurysmal bone cyst.
Surgical Excision
A combined endonasal-cranial approach to resect this lesion that entailed an extradural bi-coronal craniotomy (pericranium saving technique for closure) and medial bilateral orbitotomy was performed (Figure 2, B). The preoperative assessment of the tumor (using the neuronavigation system) revealed a volume of 88.67 cc, approximately 95% (84.17 cc) of the tumor was removed. 4.5 cc was left over the right optic nerve to preserve the vision on the unaffected eye. The intraoperative blood loss was estimated about 1700 cc. And the patient recovered without any appreciable complications, along with improvement of her proptosis. She was discharged with clinical and imaging follow up.
Histopathology
Histological evaluation revealed fibroblastic proliferation comprised of benign fibrous spindle areas with mature irregular bone formation (Figure 4). Cystic formation and hemorrhagic spaces lined by osteoclast-like multinucleated giant were also noted (Figure 5). The findings were consisted of fibrous dysplasia with aneurismal bone cyst-like features.
Figure 4.
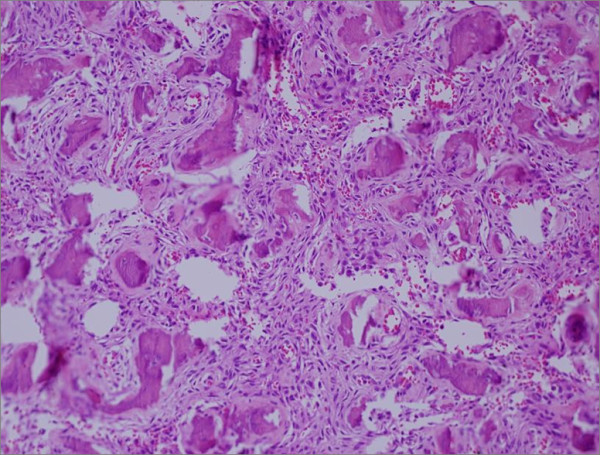
Fibrous dysplasia. Photomicrograph reveling spindle cells proliferation with islands of mature bone structure (with Chinese like characters). No mitosis or cellular features of malignancy are presented.
Figure 5.
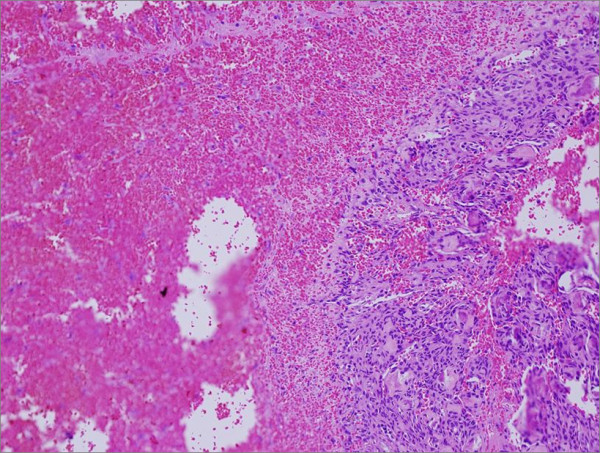
Aneurysmal bone cyst. Photomicrograph shows spindle cell proliferation with giant cell lining bloody cystic structure.
Follow-up
Five months after surgery, a recurrent large tumor was noticed, estimated to be 30.5 cc (Figure 2, C). The patient's parents declined any further treatment, and the patient was lost to follow up.
Discussion
We present a rare case of FD with ABC in the skull base of a female child with sudden blindness. The radiological and pathological findings were consistent with the diagnosis in this case. In contrast to previous reports, however, the present case progressed rapidly and led to bone destruction and extension to adjacent vital structures. Saito et al [12] presented a similar case involving the nasal cavity and the sphenoid sinus with symptoms that preceded the diagnosis by one year. In their case, complete excision was achieved with no recurrence after 3.5 years of follow up. Of the [11] concomitant FD and ABC that have been reported (Table 1[8-18]), [9,13,14,16-18], three occurred in the sinonasal cavity [8,12,13,15].
Table 1.
Clinical, radiological findings, and treatment of reported combined fibrous dysplasia and aneurysmal bone cyst of the skull
| Reference | Age (years) Gender | Site | Clinical presentation | Radiological findings | Treatment/Surgical approach | Follow-up |
|---|---|---|---|---|---|---|
| Składzień et al., 2008 [8] | 16/M | Rt Maxillary, orbital | Epistaxis and chronic rhinosinusitis | Large cystic lesion | En-bloc excision | 9 mo disease free |
| Rappaport, 1989 [9] | 25/M | Lt occipital | Painful mass | CT: pagetoid changes and hypodense lesion | Surgical excision | No f/u |
| Wojno and McCathy, 1994 [10] | 14/F | Rt temporal | Painless mass | CT: nonhomogeneous cystic lesion | Surgical excision | 2 yr disease free |
| Wojno and McCathy, 1994 [10] | 40/M | Lt frontal | Expanding mass Mass appear after head trauma |
CT: diffuse thickening of the calvarium, Lt frontal cyst | Surgical excision | No f/u |
| Haddad et al., 1998 [11] | 6.5/M | Rt temporal | Rt painless temporal mass | CT: nonhomogeneous cystic mass. | Frontotemporal excision | 4 yr disease free |
| Saito et al. 1998 [12] | 11/M | nasal cavity, sphenoid bone, and skull base | Nasal obstruction and headache for 1 yr | CT and MRI, irregular multilobulated tumor | Craniofacial excision | 3.5 yr disease free |
| Branch et al., 1986 [13] | 9/F | Lt parietal & fronto-temporal | Painful Lt and frontal parietal mass for 1 mo | CT: large cystic bone lesion in the parietal area | Surgical excision | No f/u |
| Branch et al., 1986 [13] | 19/M | Rt parietal | Painless mass k/c of FD for 15 yr |
CT: cystic expansion of the skull | Surgical excision | No f/u |
| Itshayek et al., 2002 [14] | 19/M | Lt occipital bone and clivus | Painless mass of the occipital area | CT: occipital cyst lesion | Selective embolization. Followed by surgical resection. | 1 yr disease free |
| Pasquini et al., 2002 [15] | 5/M | Rt maxillary sinus | Progressive and persistent Rt side epiphora and rhinosinusitis for 2 yr. | CT: Cyst-like lesion. | Transnasal endoscopic surgery | No f/u |
| Lin et al., 2004 [16] | 18/M | Lt frontal bone | Progressive enlargement of the mass with severe headache | CT: several expansile cystic spaces | Surgical resection | No f/u |
| Iseri et al., 2005 [17] | 35/F | Lt occipital bone | Progressive severe headache | FD of clivus, temporal, and occipital bones. | Unresectable | |
| Mattei et al., 2005 [18] | 19/M | Occipital bone | As SAH; severe headache and nuchal rigidity. | Hemmorage and cyst | Partial surgical resection | No f/u |
| Our case | 7/F | Sphenoidal and ethmoidal bones | Lt eye loss of vision Lt nasal obstruction |
Cystic expansible lesion | Endonasal - cranial resection | Recur after 5 mo |
FD; fibrous dysplasia. AG; angiogram. LPMA; Lt posterior meningeal artery. SAH; subarachnoid hemorrhage. ABC; aneurysmal bone cyst. f/u; follow up. k/c; known case.
PNS; paranasal sinuses.
The presentation of these lesions, as in our case, depends on the location, rate of growth and site of involvement. Symptoms may include painless mass, pressure symptoms, nasal obstruction, headache and loss of vision. Acute hemorrhage into the cyst(s) may causes pain, rapid enlargement and/or rupture and subarachnoid hemorrhage [18]. All reported cases were treated surgically with generally good outcomes.
ABC in distal tibia has been treated by high-energy, low-dose radiation on one patient and was successful, with no recurrence during the five years follow up [19]. However, radiation for ABC of skull base or concomitant ABC with FD residual tumors has not been reported. The aggressive nature of the present case and others suggests that adjuvant therapy may be required in some cases.
Conclusion
Our case represents a rapid developing fibrous dysplasia with aneurismal bone cyst at the skull base leading to unilateral blindness. Awareness of such cases may lead to early detection and diagnosis for effective therapy.
A multidisciplinary team is needed for both diagnosis (clinical, radiological, and histopathological) and management (otolaryngology, neurosurgery, and neuronavigation) in this kind of diseases.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AST: writer, alignment and drafted the manuscript. KHQ: surgen, writer. EB: radiological diagnosis, writer. LS: neuronavigation, writer. ABM: pathological diagnosis, writer. AJS: surgen, writer. All authors read and approved the final manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Contributor Information
Abdullah Sulieman Terkawi, Email: abdullahast@hotmail.com.
Khalid H Al-Qahtani, Email: k_qahtani2001@yahoo.com.
Eman Baksh, Email: emanbakhsh2000@hotmail.com.
Lahbib Soualmi, Email: lsoualmi@yahoo.ca.
Asim El-Bagir Mohamed, Email: asimelbagir@hotmail.com.
Abdulrahman J Sabbagh, Email: abdulrahman.sabbagh@gmail.com.
Acknowledgements
We are grateful to Dr. Adel El-Naggar for his great influence in reviewing this manuscript, Dr. Suhail Maqbool for his helpful guidance in writing the manuscript and patient management, and Dr. Mahmoud Al-Yamany for helping in innovating and performing the skull base approach.
References
- Edgerton MT, Persing JA, Jane JA. The surgical treatment of fibrous dysplasia with emphasis on recent contributions from cranio-maxillo-facial surgery. Ann Surg. 1985;202:459–479. doi: 10.1097/00000658-198510000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman MD, Rao VM, Lowry LD, Kelly M. Fibrous dysplasia of the paranasal sinuses. Otolaryngol Head Neck Surg. 1986;95:222–225. doi: 10.1177/019459988609500217. [DOI] [PubMed] [Google Scholar]
- Harrison DFN. In: Cancer of head and neck. Suen JY, Myers EN, editor. Churchill-Livingstone, New York; 1981. Unusual tumors; pp. 829–876. [Google Scholar]
- Albright F, Butler AM, Hampton AO, Smith PH. Syndrome characterized by osteitis fibrosa disseminata, areas of pigmentation and endocrine dysfunction, with precocious puberty in females: report of five cases. N Engl J Med. 1937;216:727–746. doi: 10.1056/NEJM193704292161701. [DOI] [Google Scholar]
- Ham DW, Pitman KT, Lassen LF. Fibrous dysplasia of the clivus and sphenoid sinus. Military Med. 1998;163:186–189. [PubMed] [Google Scholar]
- Bibby K, McFadzean R. Fibrous dysplasia of the orbit. Br J Ophthalmol. 1994;78:266–270. doi: 10.1136/bjo.78.4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation and imaging. AJR. 1995;164:573–580. doi: 10.2214/ajr.164.3.7863874. [DOI] [PubMed] [Google Scholar]
- Składzień J, Oleś K, Zagólski O, Moskała M, Sztuka M, Strek P, Wierzchowski W, Tomik J. A giant cranial aneurysmal bone cyst associated with fibrous dysplasia. B-ENT. 2008;4:29–33. [PubMed] [Google Scholar]
- Rappaport ZH. Aneurysmal bone cyst associated with fibrous dysplasia of the skull. Neurochirurgia. 1989;32:192–194. doi: 10.1055/s-2008-1054037. [DOI] [PubMed] [Google Scholar]
- Wojno KJ, McCarthy EF. Fibro-osseous lesions of the face and skull with aneurysmal bone cyst formation. Skeletal Radiol. 1994;23:15–18. doi: 10.1007/BF00203695. [DOI] [PubMed] [Google Scholar]
- Georges F Haddad, Hambali Fadi, Mufarrij Amjad, Nassar Anis, Fuad S Haddad. Concomitant Fibrous Dysplasia and Aneurysmal Bone Cyst of the Skull Base. Pediatr Neurosurg. 1998;28:147–153. doi: 10.1159/000028639. [DOI] [PubMed] [Google Scholar]
- Saito Kiyoshi, Fukuta Keizo, Takahashi Masakatsu, Yukio Seki, Youshida Jun. Benign fibroosseous lesions involving the skull base, paranasal sinuses, and nasal cavity. Report of two cases. J Neurosurg. 1998;88:1116–1119. doi: 10.3171/jns.1998.88.6.1116. [DOI] [PubMed] [Google Scholar]
- Branch CL, Challa VR, Kelly DL. Aneurysmal bone cyst with fibrous dysplasia of the parietal bone. Report of two cases. J Neurosurg. 1986;64:331–335. doi: 10.3171/jns.1986.64.2.0331. [DOI] [PubMed] [Google Scholar]
- Itshayek Eyal, Spector Sergey, Gomori Moshe, Ricardo Segal. Fibrous dysplasia in combination with aneurysmal bone cyst of the occipital bone and the clivus: case report and review of the literature. Neurosurgery. 2002;51:815–818. doi: 10.1097/00006123-200209000-00040. [DOI] [PubMed] [Google Scholar]
- Pasquini Ernesto, Compadretti Giacomo Ceroni, Sciarretta Vittorio, Ippolito Antonio. Transnasal endoscopic surgery for the treatment of fibrous dysplasia of maxillary sinus associated to aneurysmal bone cyst in a 5-year-old child. Int J Pediatr Otorhinolaryngol. 2002;62:59–62. doi: 10.1016/S0165-5876(01)00593-6. [DOI] [PubMed] [Google Scholar]
- Wen-Chiung Lin, Wu Hung-Ta Hondar, Chao-Jung Wei, Chang Cheng-Yen. Aneurysmal bone cyst arising from fibrous dysplasia of the frontal bone (2004:2b) Eur Radiol. 2004;14:930–932. doi: 10.1007/s00330-003-2181-4. [DOI] [PubMed] [Google Scholar]
- Pervin K Iseri, Efendi Husnu, Demirci Ali, Komsuoglu Sezer. Fibrous Dysplasia of the Cranial Bones: A Case Report and Review of the Literature. Yale Journal of Biology and Medicine. 2005;78:139–143. [PMC free article] [PubMed] [Google Scholar]
- Mattei TA, Mattei JA, Ramina R, Aguiar PH. Fibrous dysplasia in combination with aneurysmal bone cyst presenting as a subarachnoid haemorrhage. Neurol Sci. 2005;26:178–181. doi: 10.1007/s10072-005-0458-x. [DOI] [PubMed] [Google Scholar]
- Kamikonya N, Hishikawa Y, Kurisu K, Taniguchi M, Miura T. Aneurysmal bone cyst treated by high-energy, low-dose radiation therapy: a case report. Radiat Med. 1991;9(2):54–6. [PubMed] [Google Scholar]