Abstract
Diffuse alveolar haemorrhage (DAH) is a rare complication of systemic lupus erythematosus (SLE), which can have a potentially lethal outcome. Conventional treatments of the condition include cyclophosphamide and intravenous immunoglobulins. Successful treatment with rituximab and plasmapheresis has also been described. The authors report the case of a woman recently diagnosed with SLE who developed DAH refractory to conventional treatment while on immunosuppressive treatment for class III lupus nephritis whose DAH responded to plasmapheresis.
Background
Pulmonary complications in systemic lupus erythematosus (SLE) are common. They include pleuritic chest pain, recurrent infections, pulmonary hypertension, shrinking lung syndrome, acute pneumonitis and pulmonary embolism (when associated with the anti-phospholipid syndrome).
Haemoptysis characterises a large number of conditions, including tuberculosis, bronchogenic carcinoma and mitral stenosis. Haemoptysis with diffuse alveolar haemorrhage (DAH) is a well-described, life-threatening complication of the anti-neutrophil cytoplasmic antibody associated vasculitides and anti-glomerular basement membrane disease, the so-called pulmonary-renal syndromes.
DAH is a rare and catastrophic complication of SLE occurring in approximately 1% of patients.1 The pathogenesis is poorly understood. Several treatment modalities have been used with varying degrees of success.
Case presentation
A 28-year-old Jamaican woman was diagnosed with SLE having been admitted to hospital with increasing malaise, weight loss, reduced appetite, arthralgia and low mood. Of note, her aunt suffered from SLE. She had no other past medical history. Her anti-DNA antibodies were >100 IU, C3 and C4 were low at 0.58 g/l (0.75–1.65) and 0.1 g/l (0.11–43), respectively, and antibodies to Ro, RNP and Sm were positive. She was thrombocytopenic with a platelet count of 46×109/l. Urine dipstick showed 3+ protein and 4+ blood and her creatinine was elevated at 424 μ/l. She underwent renal biopsy, which demonstrated class III glomerulonephritis with 39% active lesions and 11% crescents. The National Institutes of Health (NIH) activity score was 9/24 with a chronicity score of 2/12. She was started on steroids (three doses of intravenous methylprednisolone 500 mg followed by 40 mg prednisolone once a day on a tapering course) and mycophenolate mofetil at 2 g per day later increased to 3 g per day. Eighteen days after starting her induction treatment, she attended a routine outpatient appointment complaining of dyspnoea on minimal exertion and a possible small haemoptysis the previous day. At this stage, her prednisolone dose was 30 mg a day. Examination revealed minor chest signs, but chest x-ray (figure 1) showed new right middle and lower lobe consolidation. Her peripheral oxygen saturations were 100% with a PaO2 of 14 kPa breathing room air. However her saturations were noted to drop to 95% on minimal exertion.
Figure 1.
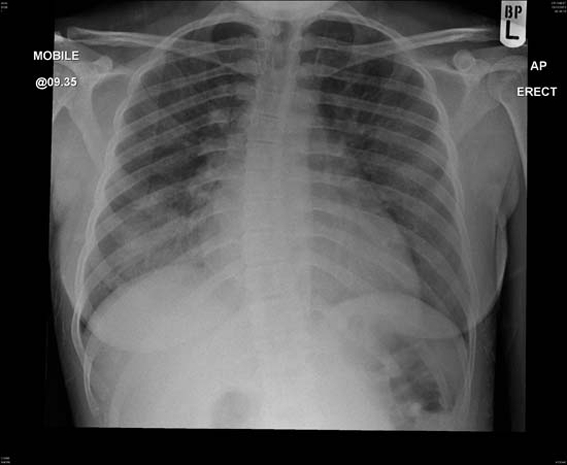
Evidence of diffuse alveolar haemorrhage in right middle and lower lobe.
Her creatinine had fallen to 216 μ/l since the start of induction treatment for lupus nephritis suggesting a response to treatment. However, her haemoglobin was 7.6 g/dl having been 8.9 g/dl a week earlier. Her platelet count remained low at 45. Her blood film showed no evidence of intravascular haemolysis and her thrombocytopenia was thought to be immune-mediated and related to her SLE.
Investigations
Urgent pulmonary function tests revealed a raised KCO 2.66 (predicted value 1.85). An urgent bronchoscopy showed fresh bleeding in the right lower lobe and did not show evidence of infection.
Treatment
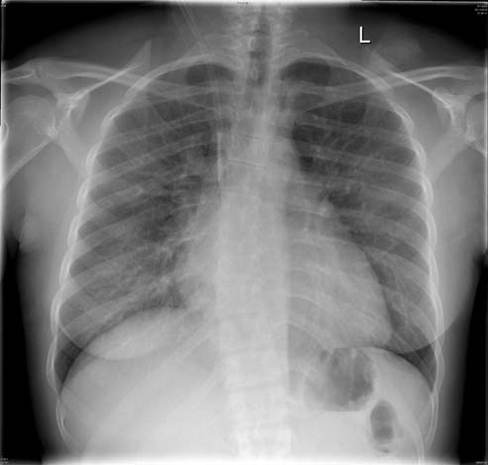
The patient was treated with intravenous cyclophosphamide 500 mg , mycophenolate mofetil was stopped and her prednisolone was increased to 60 mg a day. In view of her thrombocytopenia she was also given intravenous immunoglobulins (Ig) 1 mg/kg. Her haemoglobin dropped further to 6.2 g/dl and she required 2 units of packed red cell transfusion. However, she continued to deteriorate and 72 h after initiation of treatment she had ongoing haemoptysis. Chest x-ray (figure 2) showed worsening of the changes in the right middle and lower lobe and continuing decrement in her haemoglobin indicating ongoing bleeding. She was transferred to the critical care unit care for close monitoring where she received a further dose of intravenous Ig at 1 mg/kg and five plasma exchanges at 60 ml/kg.
Figure 2.

Worsening changes 24 h later.
Outcome and follow-up
Fortunately, soon after the initiation of plasmapheresis she improved with resolution of the radiological changes (figure 3). She did not require ventilatory support. She was discharged home 8 days after presentation.
Figure 3.
Resolution of the changes 48 h following initiation of plasmapheresis.
She is currently receiving fortnightly pulsed intravenous cyclophosphamide and continues on a reducing regimen of steroids. Her haemoglobin is currently 10.1 g/dl and her creatinine is 166 μ/l. She has to date had no further relapse.
Discussion
Pulmonary haemorrhage is rarely associated with SLE but should be considered in patients with abnormalities on chest radiography even in the absence of haemoptysis or without a significant fall in haemoglobin.1 It is unclear whether any specific features predispose a particular group of SLE patients to suffer DAH though the majority of patients also have co-existent lupus nephritis.2 No consensus guidance on treatment of DAH in SLE exists primarily because of the rarity of the condition. The combination of cyclophosphamide and methylprednisolone has been shown in some studies to result in lower mortality rates.3 Rituximab and plasma exchange have also been successfully used.4 5 Our patient had haemoptysis and DAH, which occurred soon after starting a course of induction treatment with corticosteroids and mycophenolate mofetil for lupus nephritis and in the context of immune-mediated thrombocytopenia. It was refractory to initial treatment with cyclophosphamide, increased corticosteroids and intravenous Ig. The temporal association of her clinical improvement can be attributed to the initiation of plasmapheresis. However, it should also be noted that her deterioration was associated with administration of intravenous Ig. Although the chest x-ray did not show pulmonary oedema, the fluid load required in order to give the intravenous Ig may well have exacerbated the pulmonary haemorrhage. This is an important consideration, as in one series intravenous Ig was given to 10 of 29 patients with SLE and DAH.1 Mortality is high in DAH due to lupus.5 Therefore, we suggest that plasmapheresis should be considered as treatment in SLE associated DAH in the context of active disease where conventional treatment has failed to induce a rapid response. Where DAH is life-threatening, the threshold for initiating plasma exchange should be low. In addition, a treatment such as intravenous Ig that requires a significant fluid load should be used with caution.
Learning points.
-
▶
DAH is a rare but potentially catastrophic complication of SLE.
-
▶
Case reports have suggested benefit with various treatments such as cyclophosphamide, intravenous Ig and rituximab.
-
▶
Large fluid loads can exacerbate DAH and, thus, treatments that require a significant fluid load should be used with caution.
-
▶
Early use of plasmapheresis as a rescue treatment may be of benefit and should be considered at an early stage in refractory cases of DAH complicating SLE.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Shen M, Zeng X, Tian X, et al. Diffuse alveolar hemorrhage in systemic lupus erythematosus: a retrospective study in China. Lupus 2010;19:1326–30 [DOI] [PubMed] [Google Scholar]
- 2.Lee JG, Joo KW, Chung WK, et al. Diffuse alveolar hemorrhage in lupus nephritis. Clin Nephrol 2001;55:282–8 [PubMed] [Google Scholar]
- 3.Zamora MR, Warner ML, Tuder R, et al. Diffuse alveolar hemorrhage and systemic lupus erythematosus. Clinical presentation, histology, survival, and outcome. Medicine (Baltimore) 1997;76:192–202 [DOI] [PubMed] [Google Scholar]
- 4.Narshi CB, Haider S, Ford CM, et al. Rituximab as early therapy for pulmonary haemorrhage in systemic lupus erythematosus. Rheumatology (Oxford) 2010;49:392–4 [DOI] [PubMed] [Google Scholar]
- 5.Erickson RW, Franklin WA, Emlen W. Treatment of hemorrhagic lupus pneumonitis with plasmapheresis. Semin Arthritis Rheum 1994;24:114–23 [DOI] [PubMed] [Google Scholar]


