Abstract
A healthy 18-month-old girl presented with a history of intermittent hemifacial flushing when eating. Her symptom seemed to be exclusively triggered by chewing. Examination revealed cutaneous features of neurofibromatosis type 1 (NF1) and mild facial asymmetry. Imaging confirmed cerebral vacuolisation changes seen in NF1 and a left facial plexiform neurofibroma involving the parotid gland. This is the first reported case of Frey syndrome complicating NF1.
Background
Frey syndrome is not commonly encountered in the paediatric population but has been described in children following obstetric trauma and herpes zoster infection. This case serves as a reminder to consider Frey syndrome as a differential diagnosis in hemifacial flushing in children and expands the potential presenting profile for neurofibromatosis type 1 (NF1).
Case presentation
A previously healthy and developmentally normal 18-month-old girl presented with a history of intermittent hemifacial flushing when eating. Parents dated the flushing to when she started solids at 4–6 months. Left-sided facial flushing would begin within minutes of chewing and stop with cessation of eating. The area involved was bordered by the left pinna and extended to the midline across her forehead, down to her chin and along the line of her jaw (figure 1). The area involved was erythematous but dry. The episodes were seen daily, appeared to be exclusive to chewing and did not occur when drinking. There was no associated tearing, meiosis or sweating and she did not appear distressed by or even aware of the flushing. She was born by Caesarean section at full term and had no other medical history. There was no relevant family history.
Figure 1.
(A) The child before eating. (B) Left-sided facial flushing bordered by the left pinna and extended to the midline across the forehead, down to the chin and along the line of the jaw.
On examination, she had a mild facial asymmetry with some prominence of the left cheek and earlobe. Her head circumference measured 50.5 cm (98th centile) with a weight and height plotting on the 50th centile. She was found to have 10 cafe-au-lait patches measuring more than 5 mm. She also had freckles in her axillae and inguinal area. She had a mild right convex thoraco-lumbar scoliosis. Her neurological examination was normal. Ophthalmology assessment with slit lamp was normal.
Investigations
MRI of the brain (figure 2) revealed fluffy high signal lesions on T2-weighted and fluid attenuated inversion recovery (FLAIR) sequences in the cerebellum consistent with vacuolisation seen in NF1. MRI of the spine was normal. MRI with contrast of her face (figure 3) revealed an enhancing soft tissue mass centred on the left parotid gland, extending superiorly above the level of the external auditory meatus and consistent with a plexiform neurofibroma.
Figure 2.
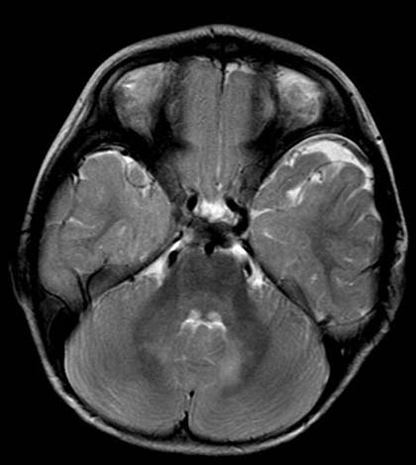
Axial T2-weighted sequence (Siemens Magnetom Avanto 1.5T) showing subtle increased signal in the cerebellar white matter a little more obvious on the left than the right side.
Figure 3.
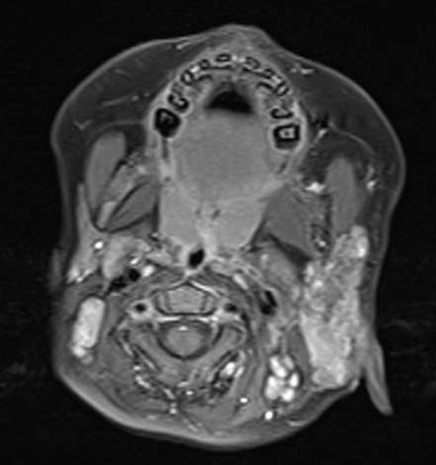
Axial T1-weighted fat saturated post -gadolinium image (Siemens Magnetom Avanto 1.5T) showing enlargement and diffuse enhancement of the left parotid gland.
Outcome and follow-up
We concluded that this child had NF1 complicated by Frey syndrome associated with a plexiform neurofibroma of her left parotid gland. At follow-up 18 months after presentation her hemifacial flushing has persisted but repeat imaging has shown no change in the size of her parotid lesion.
Discussion
Frey syndrome was first described by Duphenix in 1757 but rediscovered by Frey in 19231. It is also known as the auriculotemporal nerve syndrome. The auriculotemporal nerve is a distal branch of the mandibular nerve that originates from the trigeminal nerve and passes laterally to the neck of the mandible where it gives off secretomotor fibres to the parotid and ascends to the superficial temporal region where it is somatosensory and supplies the auricle, external acoustic meatus, outer side of the tympanic membrane and the skin in the temporal region.2 Disruption of the nerve is thought to lead to aberrant regeneration of parasympathetic fibres with secretomotor function to the parotid gland to local cutaneous arterioles.
Frey syndrome was first reported following parotid surgery when the majority of post-parotidectomy patients will experience cutaneous flushing and sweating with eating to some degree. In some, the effect can be quite debilitating.3 It has also been reported following radical neck dissection, carotid endarterectomy, submandibular gland excision, mandibular fracture and surgical approaches to the mandible.4
In children, obstetrics forceps trauma and herpes zoster infection are recognised causes of auriculotemporal nerve syndrome. An article in the Archives of Dermatology described eight children who developed symptoms in infancy.5 They developed localised facial flushing within seconds to minutes after taking solid foods. Similar to our case, the children did not exhibit sweating over the affected area of skin. The author noted that six of the eight children were born via forceps assisted delivery and in most the condition followed a benign course with diminished flushing over time.
An earlier case report described localised gustatory flushing and sweating in a child who suffered unilateral facial herpes zoster6 and it has been suggested that this syndrome can be mistaken for food allergy.7 An individual with NF1 is reported to have had unilateral hyperhidrosis involving an upper limb without obvious explanation.8 Histopathological examination of a skin biopsy from the hyperhidrotic area in this case revealed no increase or abnormality of eccrine glands compared to a section of normal skin.
Intra-parotid plexiform neurofibromas are uncommon but have been described in association with NF1.9
Learning points.
-
▶
This is the first reported case of Frey syndrome associated with a plexiform neurofibroma in a child.
-
▶
In a child presenting with unexplained hemifacial flushing a diagnosis of NF1 should be considered.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Frey L. Le syndrome de nerf auriculotemporal. Rev Neurol 1923;2:97–9 [Google Scholar]
- 2.Moore KL, Agur AMR. Essential Clinical Anatomy. Third Edition Baltimore, MD: Lippincott Williams & Wilkins; 2007:691 [Google Scholar]
- 3.Luna Ortiz K, Rascon Ortiz M, Sansón Riofrio JA, et al. Control of Frey’s Syndrome in Patients Treated with Botulinum Type A. Med Oral Patol Oral Cir Bucal 2007;12:E79–84 [PubMed] [Google Scholar]
- 4.O’Neill JP, Condron C, Curran A, et al. Lucja Frey–historical relevance and syndrome review. Surgeon 2008;6:178–81 [DOI] [PubMed] [Google Scholar]
- 5.Dizon MV, Fischer G, Jopp-McKay A, et al. Localized facial flushing in infancy. Auriculotemporal nerve (Frey) syndrome. Arch Dermatol 1997;133:1143–5 [PubMed] [Google Scholar]
- 6.Drummond PD, Boyce GM, Lance JW. Postherpetic gustatory flushing and sweating. Ann Neurol 1987;71:16–25 [DOI] [PubMed] [Google Scholar]
- 7.Kaddu S, Smolle J, Komericki P, et al. Auriculotemporal (Frey) syndrome in late childhood: an unusual variant presenting as gustatory flushing mimicking food allergy. Pediatr Dermatol 2000;17:126–8 [DOI] [PubMed] [Google Scholar]
- 8.Baskan EB, Karli N, Baykara M, et al. Localized unilateral hyperhidrosis and neurofibromatosis type 1: case report of a new association. Dermatology (Basel) 2005;211:286–9 [DOI] [PubMed] [Google Scholar]
- 9.Fadda MT, Verdino G, Mustazza MC, et al. Intra-parotid facial nerve multiple plexiform neurofibroma in patient with NF1. Int J Pediatr Otorhinolaryngol 2008;72:553–7 [DOI] [PubMed] [Google Scholar]



