Introduction
Over the last two decades methamphetamine use has escalated in the United States as well as around the world.1, 2 Methamphetamine abuse carries with it profound medical,3, 4 psychiatric,1, 3 legal5, and social1 problems. The increasing prevalence and adverse consequences of methamphetamine use highlight the importance of characterizing better the pharmacology of methamphetamine in order to develop promising treatment strategies for methamphetamine dependence.
The Diagnostic and Statistical Manual defines criteria for cocaine and amphetamine withdrawal syndromes6 and 87–97% of recently-abstinent amphetamine users are thought to experience withdrawal7, 8. Nevertheless, amphetamine withdrawal, much less methamphetamine withdrawal, has been studied on a very limited basis in humans7–9. The duration of amphetamine withdrawal is generally considered to be much longer than cocaine withdrawal,10 reportedly lasting from 5 days to more than 2 weeks7, 11. Acute withdrawal from chronic amphetamine use in humans has been associated with depression, fatigue, sleepiness12, aggression, agitation, anxiety, hyperphagia, hypersomnia, and psychomotor retardation13 14 and has also been linked with sleep abnormalities such as early onset of the first REM period, greatly increased total REM, and total sleep length that increased for several weeks15.
Given that the period of drug or substance withdrawal is often cited as time during which risk for relapse is very high16, 17, better characterizing the withdrawal syndrome associated with cessation of methamphetamine use would be of great importance for developing more efficacious treatment strategies. Therefore, we conducted this prospective observational pilot study to examine mood, anxiety, cognitive function and subjective measures of sleep over a 4-week period in patients entering residential treatment for methamphetamine dependence.
Methods
Subjects
Consecutive male and female treatment seeking volunteers were recruited from a local residential treatment facility between August 2006 and January 2008. Subjects between the ages of 18 and 65 were recruited by flyers and staff referrals at the treatment facility. Participants had to report methamphetamine as their primary drug problem with recent use verified by urine toxicology screen positive for methamphetamine. Subjects could not participate if they had an unstable medical condition requiring acute inpatient hospitalization, current diagnosis of other drug or alcohol physical dependence (other than tobacco), history of psychosis, schizophrenia or bipolar disorder, current suicidality, or current use of over-the-counter or prescription psychoactive drugs that may affect mood ratings. Women were not eligible if they were pregnant or lactating. Assessments were reviewed by a study physician prior to study entry to ensure these criteria were met. All participants gave written informed consent to participate in the study and were compensated monetarily for participation. This protocol was approved by the UAMS Institutional Review Board.
Setting
Participants were residing at the Recovery Centers of Arkansas (RCA), a licensed and accredited community-based provider of residential services for substance abuse and related disorders.
Research Design and Procedures
After informed consent, demographic data, drug use history, medical and psychiatric histories and a urine sample to test for recent methamphetamine use were obtained. Participants were then observed over a four-week period, during which time drug use, physiological, mood, sleep, cognitive and withdrawal assessments were obtained. The Methamphetamine Selective Severity Assessment (MSSA) was administered at baseline to determine severity of methamphetamine dependence11. Methamphetamine withdrawal symptoms were measured at baseline and thrice weekly using the Methamphetamine Withdrawal Assessment (MAWA) based on DSM-IV criteria for amphetamine withdrawal6. Thirteen items of amphetamine withdrawal symptoms were included in the MAWA. These items were: (i) drug craving; (ii) dysphoric mood; (iii) loss of pleasure; (iv) loss of interest in activities previously enjoyed; (v) anxiety; (vi) slowing in movement; (vii) agitation; (viii) decreased energy or fatigue; (ix) increased appetite or eating too much; (x) decreased appetite; (xi) vivid or unpleasant dreams; (xii) sleeping too much; and (xiii) insomnia. Each item was scored on a 0–4 scale (choices: `not at all', `a little, `moderately ', `quite a bit', and `extremely'). Hamilton Depression18 and Anxiety19 scales were administered at baseline and thrice weekly. Sleep quality and duration were assessed at baseline and thrice weekly utilizing items from the Sleep Inventory Questionnaire20. Domains assessed by this sleep questionnaire include overall quality of sleep rated on a 0–4 scale (choices: `very poor', `poor', `average', `good', `very good') and how refreshed the subject felt after awakening in the morning rated on a 0–4 scale (choices: `not at all', `a little', `moderately', `quite a bit', and `extremely'). Cognitive assessments were obtained at baseline, week 2 and 4 and included the Trail making Parts A and B21, the Digit symbol subtest of the Wechsler Adult Intelligence Scale-Revised22, and the Stroop Color Word Interference Test23. Heart rate and blood pressure (sitting and standing) were measured at baseline and thrice weekly. Body weight was measured at baseline and weekly.
Urine samples were obtained thrice-weekly and analyzed for the presence of methamphetamine (including metabolites) and other drugs using Hitachi 717 Automated Analyzers (Boehringer Mannheim Corp., Indianapolis, IN). A quantitative test was used to examine changes in urinary levels of methamphetamine over the course of participation in order to ensure that methamphetamine levels decreased over time as would be expected with abstinence.
Data analysis
Means and ranges were computed for continuous baseline characteristics. For longitudinal data, Proc GLIMMIX in SAS was used to fit a Mixed Model with Random Intercept. The GLIMMIX procedure in SAS allows for the generalization of the standard linear model (GLM) by allowing for the data to exhibit correlation and non-constant variability. Additionally, the random intercept allows the model to be fit separately for each individual, and then combined for the total model. This model was used initially to determine if there was a significant overall effect of time. Significant time point differences were identified utilizing post hoc Holm-Bonferroni corrections for multiple comparisons. For simplicity, a mean weekly score was calculated for measures that were obtained thrice weekly and these mean weekly scores are reported. For data with 5 time points (baseline and weeks 1 through 4), hypothesis tests were performed to test for differences between baseline and each subsequent time point as well as differences between each time point (e.g., baseline and week 1, week 1 and week 2, etc.). All tests performed were two-tailed and the level of α (to infer statistical significance) was set at 0.05.
Results
Baseline characteristics and treatment retention
Thirteen subjects (8 females and 5 males; 100% Caucasian) signed informed consent. Five were ineligible for the following reasons: baseline urine toxicology negative for methamphetamine (n=3), chronic cannabis use (n=1), and unstable hypertension (n=1). Six of the eight eligible participants (4 females, 2 males) completed the 4-week study. Study completers had a mean age of 32.7 yrs (range 25–39), 13.2 years (range 11–16) of education, reported first using methamphetamine at an average age of 16 (range 12–18), and reported using methamphetamine on average 23.8 (range 20–28) of the past 30 days. Five subjects had at least a high school education. Two participants used methamphetamine IV, while the other 4 smoked methamphetamine. Mean use of methamphetamine in any 24 hour use episode was approximately 0.9 grams (range 0.5–1.5). Participants reported using methamphetamine within 2 (n=5) or 3 (n=1) days prior to study entry. Mean baseline MSSA and MAWA scores were 48.2 (SD = 26.8) and 20.3 (SD = 12.5) respectively.
All study participants had urine screens negative for both licit and illicit substances and decreases in the amount of methamphetamine measured in quantitative urinalyses over the course of the study.
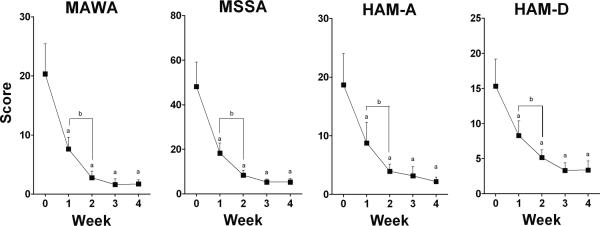
There were significant overall time effects for the MAWA (F=20.04, p<0.0001), MSSA (F=27.77, p<0.0001), HAM-D (F=19.61, p<0.0001), and the HAM-A (F=17.22, p<0.0001). Both the MAWA and MSSA scores decreased significantly between baseline and week 1 (MAWA: t= −5.38, p<0.001, MSSA: t= −6.54, p<0.001) as well as week 1 and week 2 (MAWA: t= −2.89, p=0.01, MSSA: t= −3.06, p<0.01) with no significant changes during the remaining two weeks of the study (Figure 1). For measures of depression and anxiety, a similar pattern of significant decreases during weeks 1 and 2 was observed for both the HAM-D (Wk1: t= −4.47, p<0.001, Wk2: t= −2.79, p=0.02) and HAM-A (Wk1: t= −4.34, p<0.001, Wk 2: t= −3.05, p=0.01) followed by no additional significant changes thereafter (Figure 1).
Fig 1.
Methamphetamine Withdrawal and Mood Rating Scores Over Time
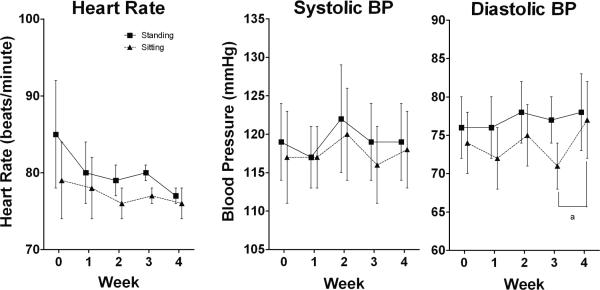
There was no significant overall time effect for standing (F=1.69, p=0.16) or sitting systolic blood pressure (F= 1.04, p=0.39) or standing diastolic blood pressure (F=0.36, p=0.84). (Figure 2). There was an overall significant time effect for sitting diastolic blood pressure (F=2.57, p<.05). Sitting DBP increased significantly between weeks 3 and 4 (t=2.80, p=0.03). No significant change over time in either sitting (F=0.51, p=0.73) or standing HR (F=1.21, p=0.31) was observed. There was an overall significant time effect for weight (F=4.95, p=0.007). Body weight increased significantly between baseline and week 2 (t=2.99, p<0.05), 3 (t=2.98, p=0.04) and 4 (t= 4.08, p=0.004).
Fig 2.
Changes in Vitals Over Time
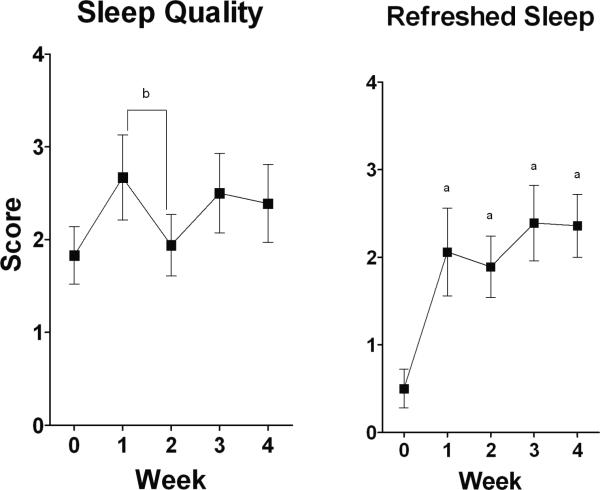
Significant overall time effects for both sleep quality (F=2.80, p=0.03) and refreshed sleep (F=6.96, p<0.0001) were observed. Relative to baseline, a significant improvement in refreshed sleep (t=−2.80, p=0.03) occurred during the first week of the residential stay, while a significant decrease in sleep quality was found between weeks one and two (t=−2.80, p=0.02) (Figure 3).
Fig 3.
Quality and Refreshed Sleep Scores Over Time
Performance on the Stroop Color-Word test, the Trials A and B tests and the Digit symbol sub-test portion of the Wechsler Adult Intelligence Scale- Revised did not change significantly over the course of the study (see table 1).
Table 1.
Cognitive Performance over Time N=6
| Measure | Mean (SD) | F value | P |
|---|---|---|---|
| Trails A | Time in seconds | 3.43 | 0.07 |
| Baseline | 28.5 (13.8) | ||
| Week 2 | 23.3 (6.7) | ||
| Week 4 | 19.2 (4.5) | ||
| Trails B | Time in seconds | 0.66 | 0.54 |
| Baseline | 56.0 (25.6) | ||
| Week 2 | 54.7 (13.4) | ||
| Week 4 | 49.5 (13.1) | ||
| Color Word Interference | T-score | 0.18 | 0.84 |
| Baseline | 62.3 (11.2) | ||
| Week 2 | 57.5 (11.5) | ||
| Week 4 | 60.2 (19.6) | ||
| Digit Symbol Subtest | Number correct | 1.84 | 0.21 |
| Baseline | 52.8 (8.4) | ||
| Week 2 | 53.8 (12.1) | ||
| Week 4 | 59.8 (9.2) |
Trails A and B: A lower score indicates a better performance.
Color Word Interference and Digit Symbol Subtest: A higher score indicates a better performance.
Discussion
Overall, self-reported measures of depression, anxiety and methamphetamine withdrawal symptoms decreased significantly during the first two weeks of the residential stay with the most dramatic reduction occurring during the first week. These results differ somewhat from those of a previous study by McGregor and colleagues11, which demonstrated a decline in methamphetamine withdrawal severity approaching control levels within one week. The reason for this is unclear, but may be due to the fact that several patients in the McGregor study received low dose benzodiazepines, which may have affected measures of methamphetamine withdrawal. Additionally, participants in the current study were older and had used methamphetamine longer. These differences may have contributed to the longer duration of withdrawal symptoms in the current study, suggesting that the duration of methamphetamine withdrawal-related symptoms may be longer than previously reported.
Although sitting diastolic blood pressure did increase significantly between weeks 3 and 4, values were never outside of clinically acceptable normal ranges. These findings are consistent with results from those of McGregor, et. al.11, in that radial pulse and blood pressure did not change significantly and stayed within normal limits for the duration of the 3 week study. Be that as it may, the clinical utility of these measures are unclear in monitoring methamphetamine withdrawal during early treatment.
Self-report measures of refreshed sleep improved significantly during the first week in treatment; however, although this improvement persisted for refreshed sleep, quality of sleep significantly worsened during the second week of the residential stay. This would seem to indicate that, although the amount of sleep in abstinent methamphetamine users may stabilize fairly quickly as demonstrated in the previous study by McGregor et. al.11, sleep quality may be a complex phenomenon that does not stabilize as rapidly. It is also somewhat unclear why seemingly related measures of refreshed sleep and quality of sleep don't follow a similar pattern. These somewhat inconsistent findings suggest that a closer examination of sleep to include more objective measures of sleep, such as actigraphic monitoring, is warranted.
Cognitive testing did not reveal significant changes during the course of the study, although performance did appear to decline during the second week of treatment. This is in contrast to previous studies that have demonstrated significant problems in cognitive function in non-treatment seeking, recently abstinent methamphetamine dependent individuals25, 26. The previous studies are difficult to compare to the current study as these previous studies were in non-treatment seeking methamphetamine dependent individuals and all results were based on comparisons to controls. It should be noted, however, that the negative results of the present study may be due to the small sample size, which is less than 33% of that for previous studies25, 26. Thus, these negative results may be due to a lack of power as well as differences in sample populations. These findings also suggest that subjective ratings are much more robust than cognitive measures in detecting changes following abrupt termination of amphetamine administration.
The small sample size (N=6) is a significant limitation of the current study and does limit generalizability for the overall population of methamphetamine dependent patients entering inpatient treatment. The lower than expected recruitment of eligible methamphetamine users over an 18-month time frame occurred due to several factors: staff did not always remember to refer potential participants, RCA contacts were recommending potential patients to be abstinent prior to their admission to the facility, which was an exclusion criterion, and comorbidity and/or use of psychoactive medications was prevalent in these patients. These factors highlight the difficulties with conducting studies like this in real world situations. Although interpretation of findings was sometimes difficult because the power to detect significant differences may have been too low, that significant changes in some sleep, withdrawal and anxiety/mood measures occurred indicate that these symptoms may be the result of a pharmacological effect associated with cessation of methamphetamine use. . An alternate explanation is that the declines in these measures are not due to resolving drug withdrawal per se, but rather reflect an improvement in anxiety and mood symptoms as patients settle into the supportive treatment milieu, engage in therapy, and consequently report fewer subjective symptoms of withdrawal. A placebo controlled, double-blind study is necessary to more closely examine the potential contribution of treatment milieu effects relative to the pharmacological effects associated with methamphetamine cessation as well as the effects of methamphetamine withdrawal on relapse and treatment retention. Although medications that reduce symptoms associated with withdrawal may be extremely valuable in promoting engagement and retention in behavioral and psychosocial treatment27, 28, future studies need to more closely examine the impact of these withdrawal symptoms on treatment outcome. The small number of study participants also likely limited our ability to find significant changes in cognitive functioning that have previously been demonstrated25, 26.
Another major limitation of the study is that it was uncontrolled; that is, there was no control for the abstinent condition. However, these findings will aid the development of a double-blind, placebo-controlled withdrawal paradigm to control for expectancy and define more precisely the severity and time-course of methamphetamine withdrawal as well as examine the efficacy of potential pharmacotherapies for alleviating these symptoms.
Conclusion
Despite the limitations cited, this study extends the literature by pointing toward a methamphetamine withdrawal syndrome that includes alterations in measures of sleep quality and refreshed sleep, early improvement in depression and anxiety symptoms, most striking during the first week, but persisting into the second week. The findings of the present and prior studies highlight the need for a double-blind, placebo-controlled methamphetamine withdrawal paradigm in humans, currently underway, where changes in sleep, cognitive function and withdrawal measures can be explored more fully.
Acknowledgments
This research was supported by NIH awards RR020146, P50-DA12762 and the Arkansas Biosciences Institute.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Murray J. Psychophysiological aspects of amphetamine-methamphetamine abuse. Journal Psychology. 1998;132:227–237. doi: 10.1080/00223989809599162. [DOI] [PubMed] [Google Scholar]
- 2.Rawson RA, Anglin MD, Ling W. Will the methamphetamine problem go away? Journal of Addictive Diseases. 2002;21:5–19. doi: 10.1300/j069v21n01_02. [DOI] [PubMed] [Google Scholar]
- 3.Kosten TR. Neurobiology of abused drugs. Opioids and stimulants. J Nerv Ment Dis. 1990;178:217–227. doi: 10.1097/00005053-199004000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Albertson TE, Derlet RW, Van Hoozen BE. Methamphetamine and the expanding complications of amphetamines. West J Med. 1999;170:214–219. [PMC free article] [PubMed] [Google Scholar]
- 5.NACO The Meth Epidemic in America. The National Association of Counties. 2005 [Google Scholar]
- 6.APA, APA . Diagnostic and Statistical Manual for Mental Disorders 2000. Washington DC: 2000. [Google Scholar]
- 7.Cantwell B, McBride AJ. Self-detoxification by amphetamine dependent patients: a pilot study. Drug Alcohol Dependence. 1998;49:157–163. doi: 10.1016/s0376-8716(97)00160-9. [DOI] [PubMed] [Google Scholar]
- 8.Gossop MR, Bradley BP, Brewis RK. Amphetamine withdrawal and sleep disturbances. Drug and Alcohol Dependence. 1982;10:177–183. doi: 10.1016/0376-8716(82)90010-2. [DOI] [PubMed] [Google Scholar]
- 9.Shoptaw SJ, Kao U, Heinzerling K, Ling W. Treatment for amphetamine withdrawal. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD003021.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srisurapanont M, Jarusuraisin N, Kittirattanapaiboon P. Treatment of amphetamine withdrawal. The Cochrane Library. 2005;2 doi: 10.1002/14651858.CD003021. [DOI] [PubMed] [Google Scholar]
- 11.McGregor C, Srisurapanont M, Jittiwutikarn J, Laobhripatr S, Wongtan T, White JM. The nature, time course and severity of methamphetamine withdrawal. Addiction. 2005;100:1320–1329. doi: 10.1111/j.1360-0443.2005.01160.x. [DOI] [PubMed] [Google Scholar]
- 12.Monroe RR, Drell HZ. Oral use of stimulants obtained from inhalers. Journal of the American Medical Association. 1947;135:909–915. doi: 10.1001/jama.1947.02890140029007. [DOI] [PubMed] [Google Scholar]
- 13.Hawks D, Mitcheson M, Ogborne A, Edwards G. Abuse of methylamphetamine. British Medical Journal. 1969;21:715–721. doi: 10.1136/bmj.2.5659.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angrist B, Sudilovsky A. Central nervous system stimulants: Historical aspects and clinical effects. In: Iversen, LI SD, Snyder SH, editors. Handbook of psychopharmacology Vol11: Stimulants. Plenum Press; New York, NY: 1978. [Google Scholar]
- 15.Kales A, Heuser G, Kales JD, Rickles WH, Jr., Rubin RT, Scharf MB, Ungerleider JT, Winters WD. Drug dependency. Investigations of stimulants and depressants. Annals of Internal Medicine. 1969;70:591–614. doi: 10.7326/0003-4819-70-3-591. [DOI] [PubMed] [Google Scholar]
- 16.Trevisan LA, Boutros N, Petrakis IL, Krystal JH. Complications of alcohol withdrawal: pathophysiological insights. Alcohol Health Res World. 1998;22:61–66. [PMC free article] [PubMed] [Google Scholar]
- 17.Koob GF. Neurobiology of Addiction: Toward the Development of New Therapies. Annals of the New York Academy of Sciences. 2000;909:170–185. doi: 10.1111/j.1749-6632.2000.tb06682.x. [DOI] [PubMed] [Google Scholar]
- 18.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton M. The assessment of anxiety states by rating. British J Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 20.Carskadon MA, DW, Mitler MM, Guilleminault C, Zarcone VP, Spiegel R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. Am J Psychiatry. 1976;133:1382–1388. doi: 10.1176/ajp.133.12.1382. [DOI] [PubMed] [Google Scholar]
- 21.Reitan KM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955;19:393–4. doi: 10.1037/h0044509. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan E, Fein D, Morris R, Delis DC. WAIS-R as a Neuropsychological Instrument. Harcourt Brace Jovanovich, Inc.; Toronto: 1991. [Google Scholar]
- 23.Golden CJ. Stroop color and word test. Stoelting Co.; Wood Dale, IL: 1978. [Google Scholar]
- 24.Cruickshank CC, Dyer KR. A review of the clinical pharmacology of methamphetamine. Addiction. 2009;104:1085–1099. doi: 10.1111/j.1360-0443.2009.02564.x. [DOI] [PubMed] [Google Scholar]
- 25.Kalechstein AD, Newton TF, Green M. Methamphetamine dependence is associated with neurocognitive impairment in the initial phases of abstinence. Journal of Neuropsychiatry and Clinical Neurosciences. 2003;15:215–220. doi: 10.1176/jnp.15.2.215. [DOI] [PubMed] [Google Scholar]
- 26.Monterosso JR, Aron AR, Cordova X, Xu J, London ED. Deficits in response inhibition associated with chronic methamphetamine abuse. Drug and Alcohol Dependence. 2005;79:273–277. doi: 10.1016/j.drugalcdep.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Rawson R, Gonzales R, Brethen P. Treatment of methamphetamine use disorders: an update. Journal of SubstanceAbuse Treatment. 2002;23:145–50. doi: 10.1016/s0740-5472(02)00256-8. [DOI] [PubMed] [Google Scholar]
- 28.Vocci F. Presented to the Methamphetamine Advisory Group to Attorney General Reno. Washington, DC: May, 1998. Medication development for methamphetamine-related disorders. [Google Scholar]