Abstract
BACKGROUND:
This study was conducted to evaluate the effect of a clinical pharmacist-led patient education program for type 2 diabetic patients at Isfahan Endocrine & Metabolism Research Center (IEMRC) from April 2008 to January 2009.
METHODS:
In a randomized controlled clinical trial, a total of 172 patients with uncontrolled type 2 diabetes were selected and randomly allocated into control and intervention groups. After taking informed written consent, the intervention group received an educational program about oral anti-hyperglycemic medications, adherence, diabetes dairy log and pill box usage. Patient's glycemic control in the intervention group was followed for three months through either telephone or face to face interviews with the pharmacist. Fasting blood glucose and HbA1c were measured at the start and end of the pharmacistled drug education program for both intervention and control groups.
RESULTS:
After a three months follow-up, mean fasting blood glucose and HbA1c of the patients in the intervention group decreased significantly compared to control group (p < 0.001).
CONCLUSIONS:
This study demonstrates an improvement in diabetes management of type 2 diabetics by involving a pharmacist in the multidisciplinary teams in the outpatient clinics. The results suggest the benefits of adding adherence education to the diabetic education programs.
Keywords: Diabetes Mellitus, Adherence, Medication, Self-Care, Clinical Pharmacist, HbA1c, Educational Activities
Because of high prevalence of diabetes and its complications, control of diabetes is one of the important components of health care system programs.1 The prevalence of diabetes was estimated to be 2.8% in 2000 and it is continuously increasing worldwide.2 Experts estimate that 7.7% of adults aged 25-64 years, or 2 million adults, suffered from diabetes in Iran in 2008.3
The management of diabetes is complicated and requires life-long therapy. Strict glycemic control has a main role in diabetes management.4 Although the medication therapy has a successful impact on glycemic control but adhering to the treatment and life style modifications are difficult for patients.5 At least 50% of patients are estimated to have inadequate adherence to medication regimens which may lead to suboptimal therapeutic goals and increased hospitalizations.6 Non-adherence to treatment among diabetic patients which may be related to passive role of patients in their care has been an ongoing problem for both patients and health care providers.7 Among different strategies for diabetes control, improving adherence plays a key role for optimizing metabolic control.6,8
Patient's education is a keystone of optimal therapy of diabetes and other chronic conditions. When patient's education is conducted effectively, this will lead to more involvement of patient in their care, better self management and improved adherence.6,8,9
Although patient's role has been determined to be a crucial factor in the management of diabetes, a multi-disciplinary approach to education has been suggested to be quite effective as well.10 As part of a multidisciplinary diabetes care team, pharmacists have a crucial role in providing care and education for patients.11 Patient's education by clinical pharmacists should be aimed for improving adherence, awareness of side effects and knowledge about the medication.12 Trustworthy relationship between patient and pharmacist can be used to improve diabetes care and outcomes.13 Some studies have revealed a range of successful methods by means of pharmacist's interventions in diabetes management.6,11,14
Although several educational programs have been developed for people with type 2 diabetes in Iran, but there is a need to improve the quality of these programs to enhance the knowledge and skills of patients in self management leading to improved adherence. To our knowledge, no study has been conducted to evaluate the effectiveness of a pharmacistled intervention in the management of diabetes in Iran. This paper presents a new model to incorporate pharmacists in the multidisciplinary teams for management of diabetes in Iran.
Methods
A randomized controlled trial was conducted in Isfahan Endocrine and Metabolism Research Center (IEMRC) to investigate the effect of pharmacistled education program on glycemic control from April 2008 to January 2009.
Inclusion-Exclusion Criteria
Patients with uncontrolled type 2 diabetes (HbA1c > 7%), who were able to read and write and were in a stable therapeutic condition, were eligible for the study. Patients excluded if they were confused, unwilling to participate or complete the study, unable to communicate verbally or reached HbA1c < 7% during the first month of the study.
Setting
IEMRC outpatient clinic covers more than 90% of diabetic population of Isfahan and follows patients every three months for their disease management. Each patient in this clinic receives an educational program offered by a nurse. The education program covers five areas: 1) definition of diabetes mellitus, urine and blood glucose testing and foot care, 2) diet therapy, 3) controlling measures for diabetes, 4) symptoms and treatment approaches to hypoglycemia and uncontrolled hyperglycemia, and 5) diabetes complications including neuropathy, nephropathy, and retinopathy. All of the present patients either in intervention or control group participated in this program.
Sample Study
One hundred and seventy two patients were randomly selected among eligible patients who met inclusion-exclusion criteria and then allocated into two groups: intervention and control.
Pharmacist-Led Intervention
Patients in intervention group participated in two educational sessions offered by the primary author of this paper after giving informed consent. The first session was about different classifications of anti-hyperglycemic agents, dosages, mechanisms of action, indications, efficacy, adverse effects, medication safety issues, contraindications, warnings/precautions, drug interactions, pregnancy risk factors, lactation and storage. The topic of the second session was adherence and self-management which included definition of adherence, different aspects of adherence, role of adherence in diabetes management, different ways to improve adherence, self care management and different ways to improve it.
At the end of the second session, a diabetes diary log and pill box was given to each diabetic patient recruited in the study. The medication name, blood glucose levels and special events such as sick days and exercise were the type of information recorded in the diary log. The pharmacist also educated patients how to fill the diary log and use that information for selfglycemic control. A questionnaire containing patient demographics and lab results (HbA1c and fasting blood glucose) was filled by the pharmacist for each patient in the intervention group and advice was given according to her/his concerns about diabetes control. Each patient was followed for three months after second educational session by weekly telephone calls and appointments with the pharmacist in IEMRC for the glycemic control. In this educational program, pharmacist attempted to improve adherence by providing medication consultation service, creating an individualized patient schedule on administration times and dosage of each medication, educating the patient on the importance of medication adherence, dietary adherence and exercise on better glycemic control, giving advice on how to reduce adverse effects of medications, and also by teaching how to take medications in the holy month of Ramadan, and how to use pill boxes and diary logs to reduce forgetfulness. The intervention group participated in all education sessions whereas the control group only received the general education offered by the nursing staff.
Data Collection
HbA1c and FBS results of intervention group were collected pre and post intervention and of control group during the three month period of study. Demographic characteristics and laboratory test data of both groups were extracted from the patient charts at the beginning and end of the three month period.
Statistical Analysis
The student t test was used to compare differences in the mean of HbA1c and FBS in each group at baseline and after three months. In testing the effect of pharmacistled intervention on glycemic control, an unpaired t test was performed to compare means of HbA1c and FBS of the two groups. Descriptive statistics were used to summarize demographic characteristics. Frequencies were compared using the chi square test or Fisher's exact test. In order to determine the normal distribution of variables the Kolmogorov-Smirnov test was used. The non-parametric Kruskal-Wallis test was used to compare the distribution of ranks between the groups. The statistical analysis was carried out using SPSS for windows (Version 15). Significance was set at a two tailed probability value less than 0.05.
Sample Size
Based on the power of 80% with a 5% margin of error, sample size was calculated to be 172. The Institutional Review Board of Isfahan University of Medical Sciences approved the study protocol.
Results
Data analysis showed there were no significant differences in HbA1c and FBS means between control and intervention groups before intervention (p > 0.05), however, significant reductions in HbA1c and FBS (1.7 ± 1.4% and 30.8 ± 57.7 mg/dl respectively) were obtained in the intervention group at the end of the study period (Table 1). Also after three months follow up, 44.4% and 3.4% of patients in intervention and control groups, respectively, reached controlled HbA1c (HbA1c < 7%).
Table 1.
Comparison of HbA1c and fasting plasma glucose before and after education
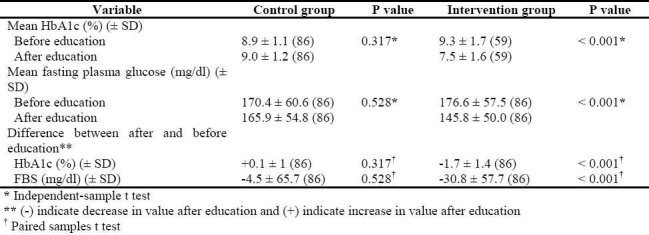
A significant relationship emerged between reduction of HbA1c and first measured HbA1c level in the intervention group (p < 0.001).
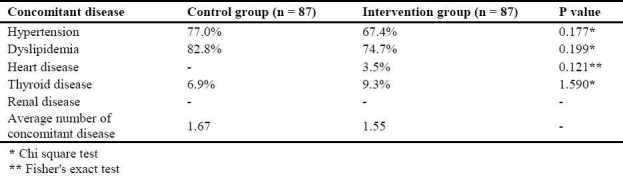
Control and intervention groups were compared for demographic characteristics (age, gender, duration of DM, and level of education), concomitant disease, type and number of medications taken by the study population and the first laboratory data (HbA1c and FBS) before education program and no significant differences were detected (Tables 2–4).
Table 2.
Comparison of demographic characteristics of patients in both groups
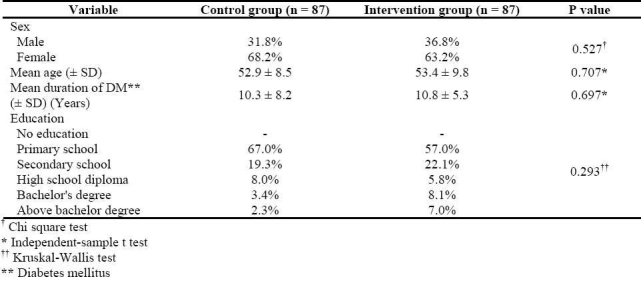
Table 4.
Comparison of the type and number of medications taken by patients in both groups
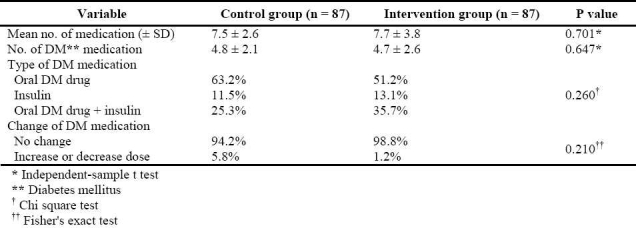
Table 3.
Comparison of concomitant diseases of patients in both groups
Discussion
The present study shows that better glycemic control was obtained in the intervention group and that the pharmacist education sessions, pill box, use of diary logs and follow up calls and appointments proved beneficial in reducing mean FBS and HbA1cs significantly.
To our knowledge, this type of intervention is first of its kind to be reported in Iran and shows that pharmacists could have added value in diabetes care management. However, since an aggregate of techniques was utilized in current intervention, it is difficult to show whether each individual component would have different impact on the final outcomes of the study.
Although there are educational programs in diabetes centers in Iran but the innovation used in this study was educating patients about importance of adherence and different approaches to improve it by utilizing a pharmacist in addition to a pill box, diary log and follow-up calls.
In this educational program, pharmacist tried to increase knowledge and motivation of the patients for better glycemic control. It seems that this educational program may have more effect on motivation and knowledge of patients with higher HbA1c than patients with lower HbA1c. It may be because patients with better glycemic control may be more familiar with the ways to control diabetes than patients with higher HbA1c, before educational program.
Other published studies showed similar results to the present study.5,8,10 In the current study patients were given advice for their glycemic control by a pharmacist every week; this continuous follow up may develop a trustable relationship between the pharmacist and patients. This close professional relationship as a part of this educational program might have contributed to a better diabetes control in the study. Suppapitiporn et al revealed that consulting with pharmacist in each visit improve the efficacy of glycemic control program.14
Provision of a pill box and daily diabetes record for each patient in the intervention group might have contributed to their medication taking behavior. Maier et al showed that using a simple pill box caused a significance decrease in HbA1c.5
Companions of patients during three months, close relationship existed between patients and pharmacist, acceptance of pharmacist orders for diabetes control by patients and better glycemic control of patients in the intervention group show the acceptance of pharmacist by patients.
Lindenmeyer et al in the review of five studies revealed a potential benefit of diabetes care interventions by pharmacists to improve medication adherence, especially in providing patient education. These studies focused on taking medications using a system of reminder and packaging and pharmacistled integrated management to improve adherence and glycated hemoglobin.6
Other studies have shown that application of self care management principles and adherence program and integration of pharmacist in education program are useful for chronic disease management such as diabetes control.1,6,9
Adherence to medication is an important part of glycemic control program.15 Outpatient health care centers encounter patients with poor adherence to medication which has a great effect on economic, quality of life and physical, mental and social functions of patients.16,17 Most type 2 diabetic patients are managed by several anti-hyperglycemic drugs. In the present study type 2 diabetic patients took different medications (7.5-7.7 pills per patient) which revealed the presence of concomitant diseases in the study population (1.55-1.67 concomitant diseases per patient).
Several studies revealed that adherence to medication was significantly associated with better clinical outcomes.18–20 One of the important aspects of this educational program was about adherence, so this educational program may help patients to be more adherent to their medications. According to this concept this educational program will be more efficient for patients with lower adherent or higher HbA1c level.
The association between HbA1c level before education and decrease in HbA1c level after education reveals that this education program was more useful for patients with higher HbA1c level who may have worse adherence.
Because of the major burden of three months follow up on the pharmacist, this study suggests that the clinical pharmacist team is necessary for diabetes management and follow up toward self care in outpatient setting.
This study supports the idea of integration of pharmacist in multidisciplinary health care team and also addition of this intervention in diabetic education curriculum for better glycemic control.
Future studies might be performed to evaluate the effect of community pharmacist on glycemic control by giving a brief advice for adherence, diabetes dairy log, pill box and anti-hyperglymic medications.
Limitations
Because patients were followed up for their clinical result data, the study was conducted in special population of type 2 diabetic patients who had a documented medical record in IEMRC. This population was familiar with educational programs and every three months visits to their physician, consequently they might be more motivated than other diabetic patients for participating in the pharmacist educational sessions and follow up period so further studies may be required to evaluate the efficacy of this educational program on the other diabetic populations.
Conclusions
This study suggests an improvement in diabetes management by the integration of pharmacist in to multidisciplinary team in the outpatient clinics. The results show the benefit of this type of intervention in diabetes management in Iran.
Conflict of Interests
Authors have no conflict of interests.
Authors’ Contributions
SF provided assistance in the design and coordination of the study, carried out all the experiments and prepared the first draft of the manuscript. AMS and AHZ provided assistance in the coordination of the study and participated in manuscript preparation. MA coordinated all experiments and provided assistance for all experiments. All authors have read and approved the content of the manuscript.
Acknowledgments
The authors acknowledge the help of Mr. Akbar Hassanzadeh, MS of Epidemiology and Biostatistics, with the statistical calculation. We would also like to thank the staff of the Isfahan Endocrine and Metabolism Center where this study was conducted. This study was funded from Isfahan University of Medical Sciences. (Grant no. 387311).
References
- 1.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2008;31(Suppl 1):S97–104. doi: 10.2337/dc10-S097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, et al. Prevalence of diabetes and im-paired fasting glucose in the adult population of Iran: national survey of risk factors for non-communicable diseases of Iran. Diabetes Care. 2008;31(1):96–8. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 4.Kitabchi AE, Freire AX, Umpierrez GE. Evidence for strict inpatient blood glucose control: time to revise glycemic goals in hospitalized patients. Metabolism. 2008;57(1):116–20. doi: 10.1016/j.metabol.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Maier C, Mustapic D, Schuster E, Luger A, Eher R. Effect of a pocket-size tablet-dispensing device on glycaemic control in type 2 diabetic patients. Diabet Med. 2006;23(1):40–5. doi: 10.1111/j.1464-5491.2005.01721.x. [DOI] [PubMed] [Google Scholar]
- 6.Lindenmeyer A, Hearnshaw H, Vermeire E, Van Royen P, Wens J, Biot Y. Interventions to improve adherence to medication in people with type 2 diabetes mellitus: a review of the literature on the role of pharmacists. J Clin Pharm Ther. 2006;31(5):409–19. doi: 10.1111/j.1365-2710.2006.00759.x. [DOI] [PubMed] [Google Scholar]
- 7.Morgan CL, Currie CJ, Peters JR. Relationship between diabetes and mortality: a population study using record lin-kage. Diabetes Care. 2000;23(8):1103–7. doi: 10.2337/diacare.23.8.1103. [DOI] [PubMed] [Google Scholar]
- 8.Albano MG, Crozet C, d′Ivernois JF. Analysis of the 2004-2007 literature on therapeutic patient education in diabetes: results and trends. Acta Diabetol. 2008;45(4):211–9. doi: 10.1007/s00592-008-0044-9. [DOI] [PubMed] [Google Scholar]
- 9.Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336(7642):491–5. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wermeille J, Bennie M, Brown I, McKnight J. Pharmaceutical care model for patients with type 2 diabetes: integration of the community pharmacist into the diabetes team--a pilot study. Pharm World Sci. 2004;26(1):18–25. doi: 10.1023/b:phar.0000013465.24857.a8. [DOI] [PubMed] [Google Scholar]
- 11.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28(4):421–36. doi: 10.1592/phco.28.4.421. [DOI] [PubMed] [Google Scholar]
- 12.Sisson E, Kuhn C. Pharmacist roles in the management of patients with type 2 diabetes. J Am Pharm Assoc 2003. 2009;49(Suppl 1):S41–5. doi: 10.1331/JAPhA.2009.09075. [DOI] [PubMed] [Google Scholar]
- 13.Padmaja Kumari R, Raman R, Sharma T. Physicians, pharmacists, and people with diabetes in India. Pharm World Sci. 2008;30(6):750–2. doi: 10.1007/s11096-008-9225-4. [DOI] [PubMed] [Google Scholar]
- 14.Suppapitiporn S, Chindavijak B, Onsanit S. Effect of diabetes drug counseling by pharmacist, diabetic disease booklet and special medication containers on glycemic control of type 2 diabetes mellitus: a randomized controlled trial. J Med Assoc Thai. 2005;88(Suppl 4):S134–41. [PubMed] [Google Scholar]
- 15.Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27(5):1218–24. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- 16.Balkrishnan R, Rajagopalan R, Camacho FT, Huston SA, Murray FT, Anderson RT. Predictors of medication ad-herence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003;25(11):2958–71. doi: 10.1016/s0149-2918(03)80347-8. [DOI] [PubMed] [Google Scholar]
- 17.Hepke KL, Martus MT, Share DA. Costs and utilization associated with pharmaceutical adherence in a diabetic population. Am J Manag Care. 2004;10(2 Pt 2):144–51. [PubMed] [Google Scholar]
- 18.Rozenfeld Y, Hunt JS, Plauschinat C, Wong KS. Oral antidiabetic medication adherence and glycemic control in managed care. Am J Manag Care. 2008;14(2):71–5. [PubMed] [Google Scholar]
- 19.Walker E, Molitch M, Kramer M, Kahn S, Ma Y, Edelstein S, et al. Adherence to preventive medications: predictors and outcomes in the Diabetes Prevention Program. Diabetes Care. 2006;29(9):1997–2002. doi: 10.2337/dc06-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant R, Adams AS, Trinacty CM, Zhang F, Kleinman K, Soumerai SB, et al. Relationship between patient medication adherence and subsequent clinical inertia in type 2 diabetes glycemic management. Diabetes Care. 2007;30(4):807–12. doi: 10.2337/dc06-2170. [DOI] [PubMed] [Google Scholar]


