Abstract
Objectives:
Non-alcoholic Steatohepatitis (NASH) is a cause of cirrhosis. Detecting its preventable causes could be useful in decreasing the disease and its complications. This study aimed to assess the prevalence of NASH in adult population living in Isfahan city as a sample of Iranian population.
Methods:
Blood samples of 2030 individuals referring to Dr. Shariati Hospital for routine health checkup were collected. All individuals with high liver enzymes [aspartate aminotransferase (AST) and/or Alanine aminotransferease (ALT)] were included in the study. Known causes of altered liver enzymes were excluded. Second blood samples were obtained 6 months later and those cases with persistent enzyme elevation were surveyed with ultrasonography.
Results:
In the first survey, 234 individuals (11.5 %) had ALT levels of more than 40 U/L. By rechecking samples after 6 months, 50% of all high serum ALT individuals remained at high level. After conducting complementary biochemical tests, 3.3% of the population was considered to have NASH; 20% of NASH cases did not have any abnormal findings in ultrasonography. Hypercholesterolemia was the most coexisting risk factor in NASH cases. We found a reverse correlation between ALT level and age (P = 0.02).
Conclusions:
The prevalence of NASH was comparable with other countries. According to the significantl correlation between ALT level and age, preventive interactions in younger individuals would decrease the incidence of NASH.
Keywords: Non-alcoholic steatohepatitis, Population-based study, Liver enzyme, Iran
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is a clinicopathologic syndrome that covers some clinical conditions ranging simple steatosis to steatohepatitis, fibrosis and end stage liver disease.1
Non-alcoholic steatohepatitis (NASH) is considered as a type of NAFLD with a prevalence of 2-3% in the general adult population. Obesity, diabetes, hyperlipidemia, insulin resistance and female sex are the major known risk factors for NASH; by increasing the incidence of these risk factors, we should expect its growing prevalence in the near future.2
Normally, NASH does not have any specific signs and symptoms and mild-to-moderate elevation of serum aminotransferase levels is the main laboratory finding.3,4
Liver biopsy is the gold standard for confirming the diagnosis and prognosis of NASH. The disease is confirmed by the hallmark histological features and exclusion of significant (more than 20 g/day) alcohol consumption. Other causes of chronic disease such as viral hepatitis (B and C), autoimmune disease, hemochromatosis, and Wilson disease must be also excluded.5
Among 25% of all NASH cases, the disease had a progressive condition. Spontaneous regression is reported in less than 15% of the patients.6
Alcohol use in Iran is less than Western countries because of the religious principles. Hence, it seems that the disorders of liver function tests should be mainly related to other causes such as NAFLD or NASH.
There are some limited studies on epidemic features of NAFLD among Iranian population as a group with specific culture, habits and also different patterns of risk factor prevalence. This study aimed to investigate some epidemiological aspects of NASH in a representative sample of Iranian adult population. Considering the complication s of NASH, this survey could be helpful in detecting its risk factors and high risk groups in deferent aspects. Future preventive programs and interventions can be considered on the results of such types of studies.
METHODS
In a cross-sectional study during fourmonth period, we collected data from the individuals referring to Dr. Shariati Hospital, a big general hospital in Isfahan Province, for routine health check up.
Target populations were adults, aged 17-70 years, with no history of alcohol consumption and also any kind of liver diseases such as hepatitis, liver metabolic disease; all consecutive 2030 individuals were selected.
Demographic information, as well as baseline characteristics like age, drug and disease history was collected for each individual by trained interviewers. Fasting venous blood samples were taken and analyzed for liver function enzymes with Hitachi 704 auto analyzer. Alanine aminotransferase (ALT and aspartate aminotransferase (AST) were measured.
Normal upper limit for ALT was considered 40 units per liter (U/L).4 Individuals with ALT equal or more than 40 U/L were rechecked 6 months later for detecting persistent liver enzyme elevation. For ruling out any other chronic liver disease and the rest of the baseline data, additional laboratory tests were conducted like hepatitis B surface antigen (Hbs Ag), hepatitis C antibody (HCV), hepatitis A antibody (HAV), anti nuclear antibody (ANA), anti mitochondrial antibody, anti smooth muscle antibody, anti liver-kidney microsome antibody (LKM), anti endomysial antibody, albumin, globulin, protein electrophoresis, cell blood count (CBC), fasting blood sugar (FBS), total cholesterol, triglycerides, low-density cholesterol (LDL-C) and high-density cholesterol (HDL-C).
The serological and biochemical measurements were done using Pars Azmoon kits (Pars Azmoon, Tehran, Iran, accredited by Bioactiva Dignostica, Germany) by Hitachi autoanalyser device (Hitachi 704, Tokyo, Japan).
In general, 234 individuals (11.5%) had ALT level higher than 40 U/L. They were invited to come for rechecking of ALT after 6 months. Totally, 55 of 96 participants who agreed to continue the study were diagnosed to have persistent elevated ALT level.
Complementary tests were conducted for these 55 individuals; 14 of them did not perform these tests and 7 individuals had positive autoimmune tests. Complementary tests were normal in 34 persons postulated as NASH cases after ultrasonography confirmation. Nine patients were female (26.5%) and 25 (73.5%) were male.
For managing missing data in this phase, we selected a random sample from missing individuals (10% of them) and compared their data with available cases. We did not find any significant difference between them (One-way ANOVA: P = 0.4).
Liver ultrasound was done by an expert radiologist in all cases with persistent high level of ALT in order to detect fatty liver changes. Ultra-sound is useful in detecting NAFLD but cannot detect small amounts of hepatic steatosis and cannot establish the diagnosis of NASH or stage of hepatic fibrosis.7 Fatty changes are singed with a hypo echo zone in liver. Fatty Infiltration graded to three degrees as follows: mild: minimal increasing hepatic echogenicity and normal view of diaphragm and border of intrahepatic vessels, moderate: a little impairment of intrahepatic vessels and diaphragm view, and severe: a noticeable increasing in hepatic echogenicity, poor penetration of the posterior segment of the right lobe and nonvisualization of the hepatic vessels and diaphragm.8
Persistent liver enzyme elevation and sonographic findings implying to fatty liver changes besides ruling out of any other chronic liver disorders, as well as absence of alcohol consumption was considered as probable NASH in this study. For ethical issues, we did not perform liver biopsy. Statistical analysis was done by SPSS software (version 13:0; SPSS Inc., Chicago, IL) using t, one-way analysis of variance (ANOVA) and Spearman tests.
RESULTS
From 2030 participants, 63.8% were men. The prevalence of high blood pressure, hypercholesterolemia and diabetes mellitus was 24.2, 36.1 and 7.6 percent, respectively. The mean age of study population was 47.3 ± 16.6 years. The mean level of ALT was 25.01 ± 22.7 U/L with significant difference between two genders (22.4 ± 21.2 in women and 29.5 ± 24.4 in men; t-test: P < 0.001). ALT level declined with increasing age (Spearman test: r = -0.1, P = 0.002).
In general, 234 individuals (11.5%) had ALT level higher than 40 U/L. They were invited to come for rechecking of ALT after 6 months. Totally, 55 of 96 participants who accepted our invitation were diagnosed to have persistent elevated ALT level.
In NASH cases, the mean age was 43.4 ± 13.8 years and the mean levels of tests were as follows: triglycerides: 174.2 ± 88.3 mg/dl; total cholesterol: 215.7 ± 53.5 mg/dl; LDL-C: 123.8 ± 32.7 mg/dl; and HDL-C: 46.2 ± 8.7 mg/dl; FBS: 110.2 ± 38.5 mg/dl; ALT: 56.8 ± 23.2 U/L; AST: 37.3 ± 20.3 U/L; and ALT/AST ratio: 0.65 ± 0.14.
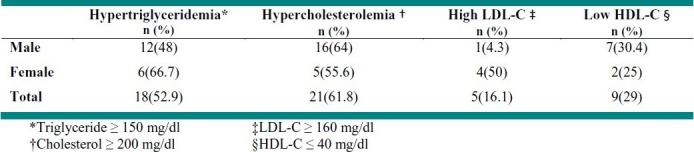
Hypercholesterolemia was the most frequent findings among NASH cases (Table 1).
Table 1.
Dyslipidemia among non-alcoholic steatohepatitis patients
Positive history of diabetes mellitus was found in 17.6% of the patients. 15.2% of those known as NASH had FBS more than 126 mg/dl; 14.7% of NASH cases had high blood pressure.
Ultrasound findings showed 58.8% with mild, 20.6% with moderate, and 2.9% with severe fatty liver changes.
DISCUSSION
In this study, the prevalence of NASH was estimated 3.3% among adult population which was similar to many other studies.9–12
ALT level correlated inversely with age. This conducted us to define normal ALT level based on age. The prevalence of diabetes mellitus in NASH cases (15.2%) was less than the findings (21-55%) of many other studies;9–11 in some other countries, the prevalence of diabetes mellitus in NASH cases is more than twice.13
The prevalence of other risk factors such as hypercholesterolemia and hypertension between NASH cases was similar to previous studies.9–14
Liver ultrasound showed fatty liver changes in more than 82% of NASH cases which is similar to some other studies.15,16
It seems that NASH is a major cause of per-sistent elevation of serum aminotransferase levels in our study population.
CONCLUSION
Because of the importance of NASH and its complications and its risk factors of NASH in various populations, more studies should be carried out about this disease especially in the countries with less alcohol consumption. Because of the significant correlation between ALT level and age, considering preventive measures in younger individuals would decrease the incidence of NASH.
Footnotes
Conflict of interest statement: All authors declare that they have no conflict of interest.
Source of funding: The study was funded by researchers.
REFERENCES
- 1.Grant LM, Lisker-Melman M. Nonalcoholic fatty liver disease. Ann Hepatol. 2004;3(3):93–9. [PubMed] [Google Scholar]
- 2.Bernal Reyes B, Saen labra A, Bernardo-Escualero R. Prevalence of nonalcoholic steatohepatitis (NASH) with comparative diabetic Stadium. Rev Coustroentrol Mex. 2000;65(2):58–62. [PubMed] [Google Scholar]
- 3.Alba LM, Lindor K. Review article: Non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2003;17(8):977–86. doi: 10.1046/j.1365-2036.2003.01493.x. [DOI] [PubMed] [Google Scholar]
- 4.Diehl AK, Poordad F. Sleisenger and Fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/ management. In: Feldman M, Friedman LS, Sleisenger MH, editors. Nonalcoholic fatty liver disease. Philadelphia: W.B. Saunders Company; 2002. pp. 1393–403. [Google Scholar]
- 5.Lindor KD. New York: American Liver Foundation; 2002. What is NAFLD/NASH? (Nonalcoholic Fatty Liver Disease/Nonalcoholic Steatohepatitis) Available from: URL: http://www.liverfoundation.org . [Google Scholar]
- 6.Das K, Kar P. Non-alcoholic steatohepatitis. J Assoc Physicians India. 2005;53:195–9. [PubMed] [Google Scholar]
- 7.Mishra P, Younossi ZM. Abdominal ultrasound for diagnosis of nonalcoholic fatty liver disease (NAFLD) Am J Gastroenterol. 2007;102(12):2716–7. doi: 10.1111/j.1572-0241.2007.01520.x. [DOI] [PubMed] [Google Scholar]
- 8.Scatarige JC, Scott WW, Donovan PJ, Siegelman SS, Sanders RC. Fatty infiltration of the liver.Ultra-sonographic and computetomographic correlation. J Ultrasound Med. 1984;3(1):9–14. doi: 10.7863/jum.1984.3.1.9. [DOI] [PubMed] [Google Scholar]
- 9.Sheth SG, Gordon FD, Chopra S. Nonalcoholic steato-hepatitis. Ann Intern Med. 1997;126(2):137–45. doi: 10.7326/0003-4819-126-2-199701150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Pourshams A, Malekzadeh R, Monavvari A, Akbari MR, Mohamadkhani A, Yarahmadi S, et al. Prevalence and etiology of persistently elevated alanine aminotransferase levels in healthy Iranian blood donors. J Gastroenterol Hepatol. 2005;20(2):229–33. doi: 10.1111/j.1440-1746.2004.03511.x. [DOI] [PubMed] [Google Scholar]
- 11.Wanless IR, Shiota K. The pathogenesis of nonalcoholic steatohepatitis and other fatty liver diseases: a four-step model including the role of lipid release and hepatic venular obstruction in the progression to cirrhosis. Semin Liver Dis. 2004;24(1):99–106. doi: 10.1055/s-2004-823104. [DOI] [PubMed] [Google Scholar]
- 12.Neuschwander-Tetri BA. Nonalcoholic steatohepatitis and the metabolic syndrome. Am J Med Sci. 2005;330(6):326–35. doi: 10.1097/00000441-200512000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein SG, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: an emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131(1):90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 14.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413–9. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 15.Ataseven H, Yildirim MH, Yalniz M, Bahcecioglu IH, Celebi S, Ozercan IH. The value of ultrasonography and computerized tomography in estimating the histopathological severity of nonalcoholic steatohepatitis. Acta Gastroenterol Belg. 2005;68(2):221–5. [PubMed] [Google Scholar]
- 16.Oliva MR, Mortele KJ, Segatto E, Glickman JN, Erturk SM, Ros PR, et al. Computed tomography features of nonalcoholic steatohepatitis with histopathologic correlation. J Comput Assist Tomogr. 2006;30(1):37–43. doi: 10.1097/01.rct.0000193818.31749.84. [DOI] [PubMed] [Google Scholar]


