Abstract
Objectives:
Increased central adiposity is associated with increased risk of cardiovascular disease (CVD) in youths. Since simple and inex-pensive but accurate diagnostic tools are required for general use in clinical practice, we examined body mass index (BMI), waist circumfe-rence (WC), waist-to-height ratio (WHtR) and skin-fold thickness (SFT) for their utility in predicting CVD risk factors in children.
Methods:
A representative sample of 3850 children (1981 males) aged, 3-11years, participated in this cross-sectional study. The association of CVD risk factors with BMI > 85th, WC > 90th, WHtR > 90th and SFT > 90th percentile was examined by multivariate logistic regression models. SPSS17was used for statistical analyses; P < 0.05 was considered statistically significant.
Results:
In studied children the prevalence of increased general adi-posity (BMI 4.1%) was considerably lower than the prevalence of high central adiposity (WC 11.8%, WHtR 9.5% and SFT sum 9.8%). Girls had more adverse lipid profiles and CVD risk factors than boys. Age-and gender- adjusted hypertension was significantly associated with adiposity (OR: 2.8) and increased skin-fold thickness (OR: 1.7). Among the four fat patterning variables WHtR > 90th percentile had the strongest association with increased LDL-C (OR: 2.0), Non HDL-C (OR: 2.1), LDL-C/HDL-C ratio (OR: 3.3), TG/HDL-C ratio (OR: 2.0) and risk factor clustering (OR: 1.7).
Conclusions:
Among the children studied, increased (WtHR) was the strongest predictor of traditional CDV risk factors, followed by in-creased skin-fold thickness and BMI.
Keywords: Anthropometric indices, prediction, cardiovascular risk factors, youth
INTRODUCTION
The prevalence of abdominal obesity defined by increased waist circumference (WC) or waist-to-height ratio (WHtR) has increased continuously among children and adolescents in the last two decades in USA and UK;1,2 whereas no significant trend is reported for high body mass index (BMI) during 1999 and 2004.3 This divergent development of general (BMI) and central (WC, WHtR) adiposity is of special concern since body fat distribution is one of the important determinants of cardiovascular disease (CVD) risk factors.4 Furthermore, CVD risk factor screening in children can predict CVD in young parents.5 This case finding strategy would improve general risk factor screening since only 38% of 8464 adolescents had a preventive care visit within 12 months and only 58% of medical care providers correctly identified weight status in some previous studies.6,7 After having shown that anthropometric indices assessment for CVD risk factors predicts CVD risk factors in adolescents,8 we examined whether fat patterning parameters like BMI > 85th percentile, WC > 90th percentile, WHtR > 90th percentile and skin fold thickness (SFT) > 90th percentile are able to predict traditional CVD risk factors in a large monoethnic community-based sample of children.
METHODS
Studied population
The Prevention Education Program (PEP) Family Heart Study is a prospective, communitybased family study of CVD risk factors and life-style behaviors in children and parents, which has been conducted since 1995 in the city of Nuremberg, Germany.8 Here we report the findings of 3850 German children who participated in yearly cross-sectional surveys from 2000 to 2007. Among them, 1981 were men and the mean (SD) age was 8.7 (1.7) years (age range; 3-11 years). Written informed consent, excluding assessment of the pubertal status, was obtained from all parents/guardians together with oral consent from children. PEP was approved according to the guidelines of the Helsinki Declaration by the Ethical Committee of the Medical Faculty of the Ludwig Maximilians University of Munich, the Bavarian Ministry of Science and Education, and the local school authorities. Exclusion criteria were non-European German ethnicity; incomplete datasets; apparent cardiovascular, metabolic, endocrine, or malignant diseases; and/or taking any medication.
Measurements
All measurements were performed by trained staff as described previously.8,9 Briefly, data composed of personal and familial medical history; socioeconomic data, medication, smoking habits, and physical activity were collected and assessed using interviewer-assisted question-naires. Physical examination included measurements of height and WC (to the nearest 0.1 cm), weight, SFT and blood pressure (BP); body mass index (BMI) as weight in kilograms divided by the square of height in meters, waist-to-height ratio (WHtR), the sum triceps, biceps and subscapular SFT and percent body fat (BF%) were calculated. Fasting veonous blood samples for lipid and glucose assessments were collected, processed and stored at -20ºC every year during November and December.
Statistical analysis
Statistical analyses were performed using PASW 17.0 version for Windows (SPSS, Chicago, IL) according to a predefined analysis plan and program. Continuous variables are presented as the mean ± standard deviation (SD). Smoothed age- and gender-specific curves were constructed for WC, WHtR, SFT and BMI10 using the software package LMS Chart Maker Pro, version 2.3. The associations between anthropometric indices and CVD risk factors were evaluated by multivariate logistic regression using the backward Likelihood Quotient Model. All of the tests were 2-sided, and P values of < 0.05 were considered to be statistically significant.
RESULTS
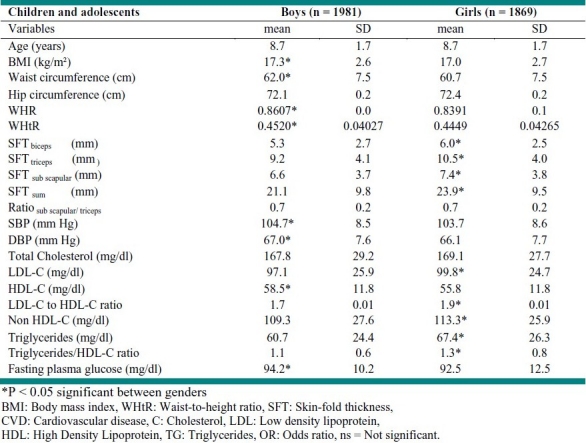
Anthropometric variables were significantly different among children. Boys had significantly higher mean values of BMI, WC, waist-to-hip ratio (WHR), WHtR, systolic blood pressure (SBP) and diastolic blood pressure (DBP) whereas SFT was significantly higher in girls (Table 1). Furthermore, girls had higher blood lipid levels except for HDL-C and fasting glucose, which were significantly higher in boys.
Table 1.
Characteristics of studied children
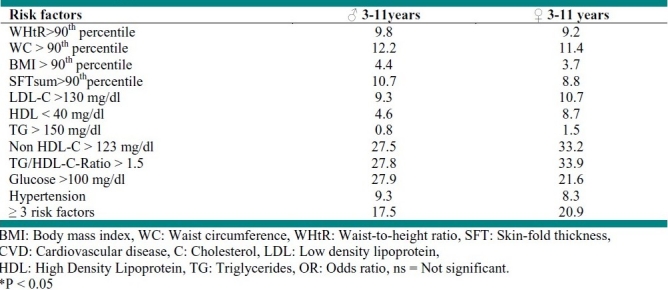
The prevalence of anthropometric risk factors was comparable in both genders. However, the prevalence of general adiposity, presented by BMI, (4.1%) in children was considerably lower than the prevalence of central adiposity (WC 11.8%, WHtR 9.5% and SFT sum 9.8%) (Table 2). Clustering of CVD risk factors was higher in girls who had also a more adverse lipid profile than boys. The prevalence of fasting hypergly-caemia was considerably higher in boys; hypertension was comparable in both genders.
Table 2.
Prevalence (%) of cardiovascular risk factors in studied children.
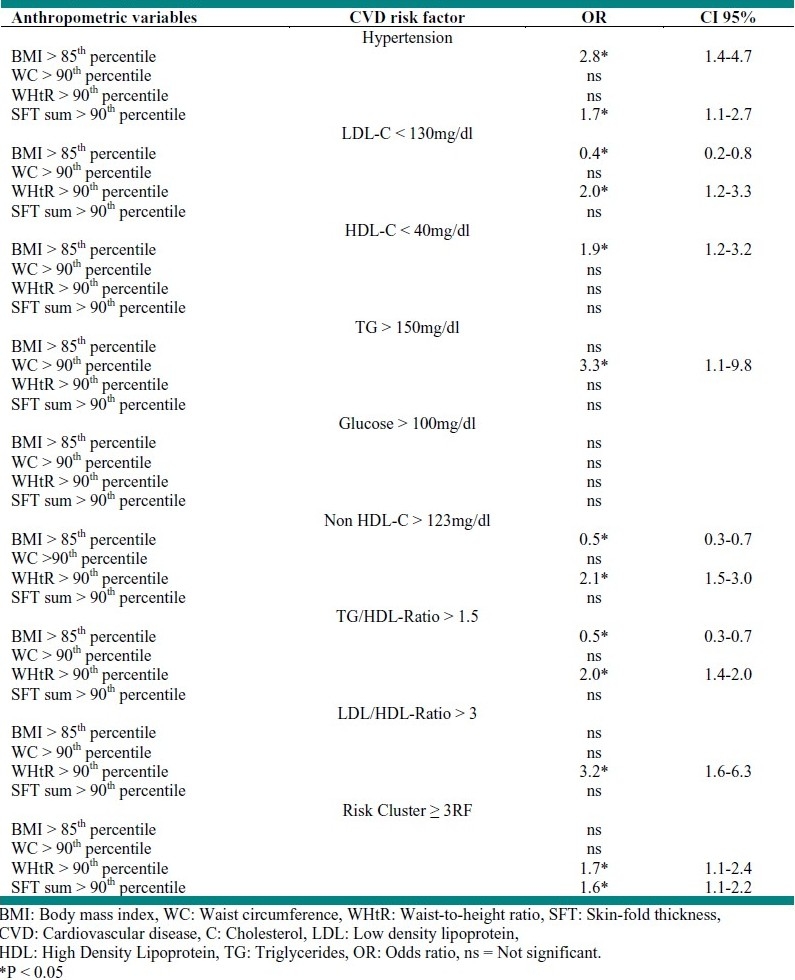
As shown in table 3, age and gender adjusted hypertension is significantly associated with adiposity (OR: 2.8) and increased skin-fold thickness (OR: 1.7). However, among the four different fat patterns, WHtR > 90th percentile was the strongest predictor of increased LDL-C (OR: 2.0), non HDL-C (OR: 2.1), LDL-C/HDL-C ratio (OR: 3.3), TG/HDL-C ratio (OR: 2.0) and risk factor clustering (OR: 1.7), whereas increased BMI and SFT could predict the risk of two parameters. Increased WC only, hypertriglyceridemia (OR: 3.3) and fasting hyperglycaemia were not associated with fat patterning.
Table 3.
Age-and gender-adjusted associations between 3 anthropometric indices and cardiovascular risk factors
DISCUSSION
The present study demonstrates that different fat patterns would predict CVD risk factors in children. WHtR > 90th percentile was the strongest anthropometric index detecting 4 out of 8 risk factors together with risk factor clustering. This is consistent with the study of 10-14-year-old children from Cyprus showing that WC and WHtR were better predictors of CVD risk factors than BMI.11 Another study evaluating 9-13-year-old Japanese children indicated that WHtR was the most significant predictor among the anthropometric indices for CVD risk factor clustering, and dyslipoproteinemia.12 Maffeis et al showed that 3-11-year-old Italian children with WC > 90th percentile were more likely to have multiple risk factors of CVD/and a strong association existed with triceps and sub-scapular SFT.13 In Hong Kong Chinese children, aged 6-12 years, WC correlated slightly more than BMI with CVD risk factors especially with elevated TG, decreased HDL-C and high BP but poorly with elevated LDL-C and impaired blood glucose; the latter is also consistent with our findings.14 The Bogalusa Heart Study demonstrated that WHtR had a slightly stronger association with impaired lipid levels than BMI and that BMI-for-age was slightly more associated with BMI.
In overweight children, the association of WHtR with adverse CVD risk factors was stronger than of BMI and SFT.15,16 The comparison between the PEP Family Heart Study and the Bogalusa Heart Study might be biased by age (3-11 years vs. and 5-17 years) and race (German children vs. biracial youths).
Strengths of this observational study were the homogeneous urban population of German children without co-morbidities, its large gender-balanced size, constancy of staff and methods over seven years in this monocentric study and the use of simple, wellestablished surrogate methods permitting easy and inexpensive application in clinical practice. Limitations were the cross-sectional design of the study which does not allow any decision about casual relationships of the associations and the lack of internationally agreed cutoff values of WHtR, WC, and SFT.
CONCLUSION
In our study, increased WHtR was the strongest predictor of CVD risk factors in 3-11-year-old children, together with increased SFT and BMI additionally predicting high BP, hypertriglyceridemia and low HDL-C.
Acknowledgments
The PEP Family Heart Study is a joint effort of many investigators and staff members whose efforts are gratefully acknowledged. We especially thank the study participants for their continuous engagement for many years.
Footnotes
Conflict of interest statement: All authors declare that they have no conflict of interest.
Source of funding: Foundation for the Prevention of Atherosclerosis, Nuremberg, Germany; Ludwig Maximilian University, Munich, Germany; Bavarian Ministry of Health, Munich; City of Nuremberg.
REFERENCES
- 1.Li C, Ford ES, Mokdad AH, Cook S. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics. 2006;118(5):e1390–8. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message--‘keep your waist circumference to less than half your height’. Int J Obes (Lond) 2006;30(6):988–92. doi: 10.1038/sj.ijo.0803226. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299(20):2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 4.Daniels SR, Morrison JA, Sprecher DL, Khoury P, Kimball TR. Association of body fat distribution and cardiovascular risk factors in children and adolescents. Circulation. 1999;99(4):541–5. doi: 10.1161/01.cir.99.4.541. [DOI] [PubMed] [Google Scholar]
- 5.Schwandt P, Bischoff-Ferrari HA, Staehelin HB, Haas GM. Cardiovascular risk screening in school children predicts risk in parents. Atherosclerosis. 2009;205(2):626–31. doi: 10.1016/j.atherosclerosis.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Irwin CE, Jr, Adams SH, Park MJ. Newacheck PW.Preventive care for adolescents: few get visits and fewer get services. Pediatrics. 2009;123(4):e565–72. doi: 10.1542/peds.2008-2601. [DOI] [PubMed] [Google Scholar]
- 7.Huang JS, Donohue M, Golnari G, Fernandez S, Walker-Gallego E, Galvan K, et al. Pediatricians′ weight assessment and obesity management practices. BMC Pediatr. 2009;9:19. doi: 10.1186/1471-2431-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwandt P, Bertsch T, Haas GM. Anthropometric screening for silent cardiovascular risk factors in adolescents: The PEP Family Heart Study. Atherosclerosis. 2010;211(2):667–71. doi: 10.1016/j.atherosclerosis.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 9.Schwandt P, Geiss HC, Ritter MM, Ublacker C, Parhofer KG, Otto C, et al. The prevention education program (PEP).A prospective study of the efficacy of family-oriented life style modification in the reduc-tion of cardiovascular risk and disease: design and baseline data. J Clin Epidemiol. 1999;52(8):791–800. doi: 10.1016/s0895-4356(99)00068-2. [DOI] [PubMed] [Google Scholar]
- 10.Schwandt P, Kelishadi R, Haas GM. First reference curves of waist circumference for German children in comparison to international values: the PEP Family Heart Study. World J Pediatr. 2008;4(4):259–66. doi: 10.1007/s12519-008-0048-0. [DOI] [PubMed] [Google Scholar]
- 11.Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord. 2000;24(11):1453–8. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]
- 12.Hara M, Saitou E, Iwata F, Okada T, Harada K. Waist-to-height ratio is the best predictor of cardiovascular disease risk factors in Japanese school-children. J Atheroscler Thromb. 2002;9(3):127–32. doi: 10.5551/jat.9.127. [DOI] [PubMed] [Google Scholar]
- 13.Maffeis C, Pietrobelli A, Grezzani A, Provera S, Tato L. Waist circumference and cardiovascular risk factors in prepubertal children. Obes Res. 2001;9(3):179–87. doi: 10.1038/oby.2001.19. [DOI] [PubMed] [Google Scholar]
- 14.Sung RY, Yu CC, Choi KC, McManus A, Li AM, Xu SL, et al. Waist circumference and body mass index in Chinese children: cutoff values for predicting cardiovascular risk factors. Int J Obes (Lond) 2007;31(3):550–8. doi: 10.1038/sj.ijo.0803452. [DOI] [PubMed] [Google Scholar]
- 15.Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, et al. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr. 2007;86(1):33–40. doi: 10.1093/ajcn/86.1.33. [DOI] [PubMed] [Google Scholar]
- 16.Freedman DS, Katzmarzyk PT, Dietz WH, Srinivasan SR, Berenson GS. Relation of body mass index and skinfold thicknesses to cardiovascular disease risk factors in children: the Bogalusa Heart Study. Am J Clin Nutr. 2009;90(1):210–6. doi: 10.3945/ajcn.2009.27525. [DOI] [PMC free article] [PubMed] [Google Scholar]


