Abstract
PURPOSE
To evaluate the repeatability of Fourier-domain optical coherence tomography (OCT) measurements of the thickness of femtosecond laser–created laser in situ keratomileusis (LASIK) flaps.
SETTING
Doheny Eye Institute, University of Southern California, Los Angeles, California, USA.
DESIGN
Case series, evaluation of diagnostic technology.
METHODS
In this consecutive series, Fourier-domain OCT (RTVue) was used to measure flap thickness 1 week after LASIK. Flaps were created with a Pulsion 60 kHz femtosecond laser programmed for 110 μm flap thickness. Each eye was scanned 2 times with a radial pachymetry pattern and 1 time with a horizontal line scan. Flap thicknesses were measured at 6 positions across the corneal flap (ie, ±0.5 mm, ±1.5 mm, and ±2.5 mm from the center on the horizontal and vertical meridians). The within-grader flap thickness repeatability and between-grader reproducibility were calculated by pooled standard deviations (SDs).
RESULTS
Twenty-one eyes were measured. The mean flap thickness measurements were highly predictable at all positions. Thickness SDs varied from 5.3 to 9.5 μm and uniformity, from 121.7 to 126.5 μm. The within-grader repeatability was 3.3 to 6.4 μm based on the same image measured at different times and 4.7 to 7.4 μm for different images. The between-grader reproducibility was 4.0 to 9.0 μm. There was no statistically significant asymmetry between the nasal side versus the temporal side, the superior side versus the inferior side, or the pericentral area versus the central area of the corneal flap.
CONCLUSIONS
The femtosecond laser created LASIK flaps with uniform and predictable thicknesses. Fourier-domain OCT gave highly repeatable flap-thickness measurements.
Laser in situ keratomileusis (LASIK) is the most popular refractive procedure for correcting myopia, hyperopia, and astigmatism.1 For these procedures and others, accurate corneal thickness measurements are important in pretreatment screening and surgical planning. Postoperative assessment of flap thickness and residual stromal bed (RSB) thickness is important for repeat laser treatment (also called enhancement) or for complication management. This knowledge is also valuable in characterizing the accuracy and repeatability of corneal flap creation with a microkeratome or a femtosecond laser.
Ultrasound pachymetry has been used to measure flap thickness by subtracting the stromal bed thickness measured intraoperatively from the preoperative corneal thickness.2,3 This method is associated with a risk for stromal bed contamination because it requires contact with the eye; therefore, it is not universally practiced. Optical coherence tomography (OCT), a noncontact technique, has been used as an alternative to evaluate the flap and RSB after LASIK.4,5 Recently, a new generation of Fourier-domain OCT instruments became available. These instruments can image the cornea with higher resolution and faster speed than older generation time-domain OCT instruments.6,7 In this study, we used anterior segment Fourier-domain OCT to evaluate the repeatability of measurements of the thickness of LASIK flaps created with a femtosecond laser system.
PATIENTS AND METHODS
This prospective observational study comprised patients seeking LASIK at Doheny Laser Vision Center, Doheny Eye Institute, University of Southern California. The LASIK flap was created with a 60 kHz femtosecond laser (Pulsion, IntraLase Corp.). All patients had a full preoperative workup including corneal topography, pupillometry, and pachymetry. No patient had corneal abnormalities or contraindications to LASIK. The Institutional Review Board, University of Southern California, approved the study protocol. The study was in accordance with the Declaration of Helsinki, and each patient provided informed consent.
The same surgeon (D.H.) performed all LASIK procedures. The femtosecond flap thickness was programmed to 110 μm with a diameter of 9.0 mm and a 70-degree angled side cut. All flaps had a superior hinge. The stromal ablations were performed with a scanning-spot excimer laser (Visx S4-IR, Abbott Medical Optics, Inc.).
The cornea was imaged using a Fourier-domain OCT system (RTVue, software version 4.0, Optovue, Inc.) with a corneal adaptor module. The system operates at 830 nm wavelength and has a scan rate of 26 000 axial scans per second. The depth resolution is 5 μm (full-width, half-maximum) in tissue. The corneal adaptor module produces telecentric scanning for anterior segment imaging using a wide-angle (long lens) or high-magnification (short lens) adapter lens. This study used the wide-angle lens, which has a scan width of 6.0 mm and a transverse resolution (focused spot size) of 15 μm.8
A 6.0 mm diameter pachymetry scan pattern consisting of 8 high-definition meridional scans acquired in 0.32 seconds was used to image the central cornea. The cornea was also imaged with a 6.0 mm long line scan pattern along the horizontal meridian. The line scan acquires 16 consecutive frames for each scan.
Two pachymetry scans were obtained from each eye preoperatively and 1 week after the surgery. In addition, 1 horizontal line scan was obtained from each eye at the 1-week postoperative visit. All scans were performed with the patient seated. The patient’s head was stabilized by a chin and forehead rest, and the gaze of the eye was stabilized by an internal fixation target. There was no physical contact between the scanning module and the eye. The OCT and video camera images were displayed in real time to aid alignment. The patient was repositioned after each scan.
The Fourier-domain OCT system’s corneal adaptor module software automatically detects the anterior and posterior corneal boundaries, performs dewarping to correct image distortion due to refractive index mismatch between the air and cornea, and maps the corneal thickness.8 For line scans, the software performs automatic registration to remove the corneal motion between the consecutive frames and provides the user with an averaged image.
A manual flap computer caliper tool was used to measure the LASIK flap thickness. The flap was distinguished from the stromal bed by its increased internal reflectivity and interface signal peak (Figure 1). The flap thickness was measured along the horizontal and vertical cross-sections of the pachymetry scan ±0.5 mm, ±1.5 mm, and ±2.5 mm away from the center. Flap thickness was also measured at these 6 positions along the averaged horizontal line scan. Three graders (C.S., M.T., Y.L.) measured the flap thickness independently in randomized order. All patient information was masked. One grader (C.S.) performed the measurement twice with a 1-month separation between measurements.
Figure 1.
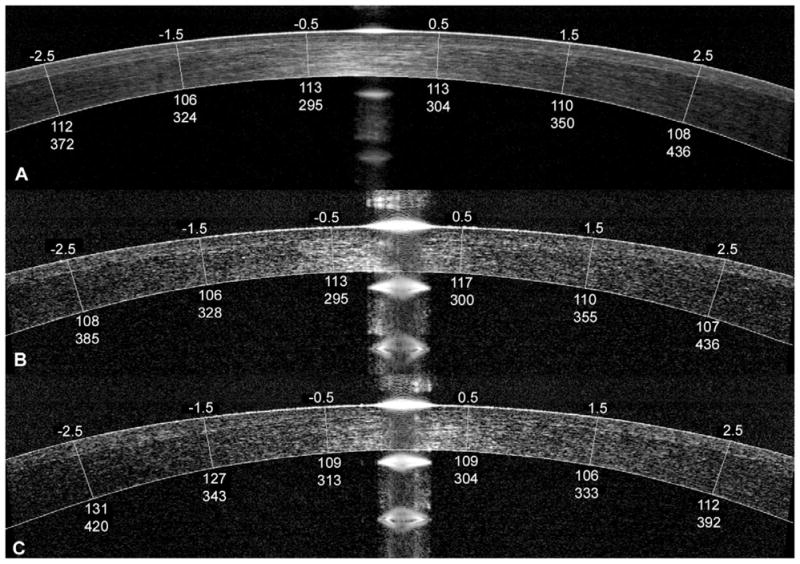
Corneal Fourier-domain OCT images overlapped with flap thicknesses measured with a manual flap computer caliper tool. A: Frame-averaged horizontal line scan. B: Horizontal single frame cross-sectional image from a pachymetry scan. C: Vertical single frame cross-sectional image from the pachymetry scan. For each image, the upper numbers represent distances from the central cornea (mm). The lower numbers represent flap thickness and RSB (μm), respectively.
To determine the uniformity of the femtosecond laser–created flap, the flap measurements along the nasal, temporal, superior, and inferior semimeridians were grouped (Figure 2) and the mean flap thickness was calculated for each group. Moreover, the flap measurements at the ±0.5 mm positions were grouped to calculate the mean central flap thickness. Similarly, the flap measurements at the ±1.5 mm and ±2.5 mm positions were grouped to calculate the mean pericentral flap thickness. Statistical tests based on the generalized estimating function were performed to evaluate the flap thickness asymmetry nasally versus temporally, superiorly versus inferiorly, and centrally versus pericentrally.9
Figure 2.
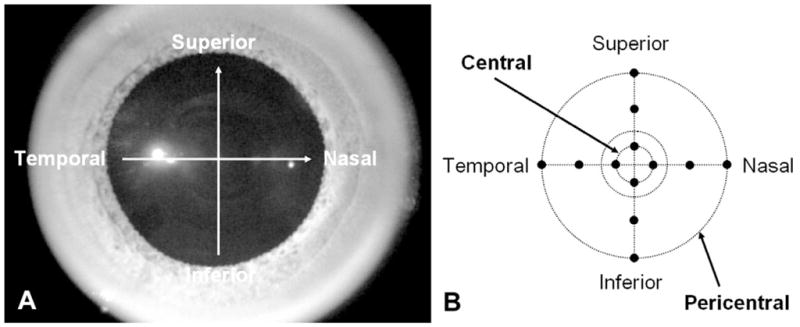
A: Pupil image showing horizontal and vertical meridional scans from the pachymetry scan pattern. B: Flap thickness was measured ±0.5 mm, ±1.5 mm, and ±2.5 mm from the center of the cornea.
The within-grader repeatability and between-grader reproducibility of the flap thickness measurements were determined. The within-grader repeatability was calculated by the pooled standard deviation (SD) of the measurements made by a single grader on repeated scans and on the same image but graded 1 month after the original measurements were made. The between-grader reproducibility was calculated by the pooled SD of the measurements made by different graders on the same images.
For statistical tests that involved both eyes of the same patients, the generalized estimating function method was used to account for the correlation between eyes. All statistical analyses, including mean and SDs, were performed using SAS software (version 9.1.3, SAS Institute, Inc.). The significance level was set at 0.05.
RESULTS
Twenty-one eyes of 12 patients (6 men, 6 women) were scanned 1 week after LASIK. The mean age of the patients was 42.8 years (range 29 to 60 years). The mean preoperative manifest spherical equivalent (SE) was −2.78 diopters (D) ± 2.33 (SD) (range −8.00 to +2.25 D). The mean preoperative central corneal thickness by Fourier-domain OCT was 538.2 ± 21.8 μm.
Femtosecond laser-created LASIK flaps were visible in all OCT scans obtained 1 week postoperatively. In OCT images, the contrast between the flap and corneal stroma was best seen in the midperiphery, more than 3 mm in diameter, and was worst in the central and pericentral area, less than 3 mm in diameter.
The range of mean flap thicknesses at the ±0.5 mm, ±1.5 mm, and ±2.5 mm positions was from 121.7 μm to 126.5 μm (Table 1). The SD of the flap thickness varied from 5.3 to 9.5 μm at different measurement positions. There was no statistically significant flap thickness asymmetry detected for the nasal versus temporal side (P = .7), the superior versus inferior side (P = .21), or the pericentral versus central side (P = .43) of the corneal flap. Similarly, there was no significant difference between the flap thicknesses measured from the horizontal single frame and the horizontal averaged frame (P = .37).
Table 1.
Flap thicknesses measured by OCT at various distances from center
| Distance from Center | ||||||
|---|---|---|---|---|---|---|
| Measurement (μm) | −2.5 mm | −1.5 mm | −0.5 mm | +0.5 mm | +1.5 mm | +2.5 mm |
| Mean horizontal averaged frame | 125.4 ± 9.4 | 125.2 ± 8.7 | 125.9 ± 8.9 | 126.2 ± 8.1 | 125.6 ± 7.6 | 125.7 ± 9.5 |
| Mean horizontal single frame | 124.5 ± 5.3 | 124.6 ± 5.8 | 124.9 ± 7.5 | 126.5 ± 5.5 | 124.2 ± 6.7 | 124.6 ± 8.6 |
| Mean vertical single frame | 123.6 ± 7.0 | 125.5 ± 6.5 | 123.2 ± 6.6 | 123.0 ± 5.4 | 122.5 ± 6.4 | 121.7 ± 7.3 |
Means ± SD
The within-grader repeatability of the flap thickness was 3.3 to 6.4 μm if the grader performed the measurements on the same image at different times (Table 2). It was 4.7 to 7.4 μm if the grader performed the measurements on repeated OCT scans. The between-grader reproducibility of the flap thickness measurement was 4.0 to 9.0 μm (Table 3).
Table 2.
Within-grader flap thickness measurement repeatability, same image.*
| Distance from Center | ||||||
|---|---|---|---|---|---|---|
| Measurement (μm) | −2.5 mm | −1.5 mm | −0.5 mm | +0.5 mm | +1.5 mm | +2.5 mm |
| Horizontal averaged frame | 3.6 | 4.1 | 4.2 | 4.2 | 3.3 | 3.8 |
| Horizontal single frame | 5.6 | 5.0 | 6.2 | 5.5 | 6.0 | 6.4 |
| Vertical single Frame | 6.0 | 4.5 | 5.3 | 4.7 | 3.4 | 5.1 |
| Different Images† | ||||||
| Horizontal Single Frame | 5.8 | 7.4 | 5.9 | 6.5 | 6.4 | 5.3 |
| Vertical Single Frame | 6.5 | 4.7 | 4.9 | 6.0 | 7.2 | 6.2 |
The same image was measured by the same investigator 1 month later.
Table 3.
Between-grader flap thickness measurement reproducibility
| Distance from Center | ||||||
|---|---|---|---|---|---|---|
| Measurement (μm) | −2.5 mm | −1.5 mm | −0.5 mm | +0.5 mm | +1.5 mm | +2.5 mm |
| Horizontal averaged frame | 4.0 | 4.0 | 6.2 | 6.7 | 5.2 | 5.5 |
| Horizontal single frame | 5.1 | 5.8 | 9.0 | 7.7 | 6.7 | 7.9 |
| Vertical single frame | 4.9 | 5.8 | 5.3 | 7.2 | 6.2 | 5.6 |
DISCUSSION
Advantages of bladeless femtosecond lasers over mechanical microkeratomes in the creation of corneal flaps include more reliable flap thickness, more control over flap diameter, independence of corneal contour and diameter, and less risk for free and buttonhole caps.10 Several studies have evaluated femtosecond laser–created LASIK flaps. Binder11 reports that flaps intended to be 110 μm thick were actually 125 ± 12 μm thick. In contrast, Rosa et al.10 found that a femtosecond laser setting of 120 μm resulted in thinner flaps (115 ± 12.5 μm). Von Jagow and Kohnen12 measured flap thicknesses ±0.5, ±1.0, ±2.0, and ±3.0 mm from the corneal vertex. For an intended 100 μm flap thickness setting, the mean femtosecond laser flap thickness was measured to be 108 to 124 μm with up to 16 μm SD at different locations.
Our results are consistent with findings in other studies. We found that the femtosecond laser–created LASIK flap was highly predictable and uniform. The measured mean flap thicknesses (121.7 to 126.5 μm) were slightly thicker than the nominal laser setting of 110 μm. This bias may be related to the calibration of the femtosecond laser system used. Another contributor to this bias is the central epithelial hyperplasia that occurs after myopic LASIK.5,13 The variation in flap thickness was small, having a SD less than 9.5 μm at all measurement positions. No statistically significant asymmetry was detected nasally versus temporally, superiorly versus inferiorly, or pericentrally versus centrally. A uniform flap may contribute to more predictable refractive and wavefront outcomes.14,15
The flap measurement within-grader reproducibility was best (4.0 to 7.9 μm) in the pericentral area 1.5 mm and 2.5 mm from the center. It worsened toward the center (5.3 to 9.3 μm). This decrease in reproducibility was expected because the flap was best visualized in the pericentral zone, where the stromal bed signal was low and the contrast in the flap reflectivity was high. The contrast was poor near the corneal vertex, where both flap reflectivity and stromal bed internal reflectivity were high. These contrast variations are introduced by the variation in incidence angle as the OCT beam is scanned across the corneal dome. Due to the corneal geometry, this is an intrinsic limitation for OCT flap measurement.
The flap interface was better visualized in registered and averaged OCT image frames in which the background and speckle noises were suppressed. Therefore, flap measurements made with averaged frames (4.0 to 6.7 μm) were more reproducible than those of single frames (4.9 to 9.0 μm). The use of frame averaging may be particularly helpful in cases in which the LASIK flap interface is faint.
A limitation of the current technique is that the flap and stromal bed thicknesses are measured postoperatively, not intraoperatively. Thus, the method does not replace the utility of intraoperative ultrasound pachymetry in obtaining real-time measurements of bed thickness before excimer laser ablation in primary LASIK. However, the high repeatability of femtosecond laser–cut flap thickness suggests that the statistical range of flap thickness measured by OCT may be adequate for primary LASIK planning in most cases. For LASIK retreatment, OCT bed measurement is clinically useful because it can be performed without relifting the flap, unlike intraoperative ultrasound pachymetry.
Two other imaging modalities, very-high-frequency ultrasound16,17 and in vivo confocal microscopy,18,19 have been used to measure LASIK flap thickness postoperatively without lifting the flap. Although very-high-frequency ultrasound can visualize the flap for a long time after LASIK, it requires contact or immersion. Confocal microscopy has excellent resolution, but its field of view is limited. Therefore, OCT is a more practical technology because it can image the flap with high resolution and it is a noncontact method. A limitation of the current RTVue-CAM OCT software is that it only allows up to a 6.0 mm scan width while imaging the cornea. A separate scan covering the peripheral cornea has to be made to measure the flap thickness outside the central 6.0 mm zone.
In summary, this study showed that femtosecond laser–created LASIK flaps were predictable and uniform. The flap thickness measured with Fourier-domain OCT was highly repeatable and reliable; however, further prospective studies with a larger population may be needed to show the greater flap measurement precision of Fourier-domain OCT compared with that of other techniques. We recommend routine measurement of LASIK flap thicknesses 1 week postoperatively, when early hydration changes have resolved and the flap interface remains highly visible.
Acknowledgments
Supported by NIH grant R01 EY018184, a research grant from Optovue, Inc., a Charles C. Manger III, MD Chair in Corneal Laser Surgery endowment, and an unrestricted grant from Research to Prevent Blindness, Inc., New York, New York, USA.
Footnotes
Presented in part at the annual meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, Florida, USA, May 2009.
Financial Disclosure: Drs. Rosas Salaroli, Zhang, Branco Ramos, and Allemann have no financial or proprietary interest in any material or method mentioned.
Additional financial disclosures: Drs. Huang, Li, and Tang received research grant support from Optovue, Inc. Dr. Huang received patent royalty, stock options, and travel support from Optovue, Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stulting RD, Lahners WJ, Carr JD. Advances in refractive surgery; 1975 to the present. Cornea. 2000;19:741–753. doi: 10.1097/00003226-200009000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Durairaj VD, Balentine J, Kouyoumdjian G, Tooze JA, Young D, Spivack L, Taravella MJ. The predictability of corneal flap thickness and tissue laser ablation in laser in situ keratomileusis. Ophthalmology. 2000;107:2140–2143. doi: 10.1016/s0161-6420(00)00407-3. [DOI] [PubMed] [Google Scholar]
- 3.Miranda D, Smith SD, Krueger RR. Comparison of flap thickness reproducibility using microkeratomes with a second motor for advancement. Ophthalmology. 2003;110:1931–1934. doi: 10.1016/S0161-6420(03)00786-3. [DOI] [PubMed] [Google Scholar]
- 4.Maldonado MJ, Ruiz-Oblitas L, Munuera JM, Aliseda D, García-Layana A, Moreno-Montañés J. Optical coherence tomography evaluation of the corneal cap and stromal bed features after laser in situ keratomileusis for high myopia and astigmatism. Ophthalmology. 2000;107:81–87. doi: 10.1016/s0161-6420(99)00022-6. discussion by DR Hardten, 88. [DOI] [PubMed] [Google Scholar]
- 5.Li Y, Netto MV, Shekhar R, Krueger RR, Huang D. A longitudinal study of LASIK flap and stromal thickness with high-speed optical coherence tomography. Ophthalmology. 2007;114:1124–1132. doi: 10.1016/j.ophtha.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 6.Rosas Salaroli CH, Li Y, Huang D. High-resolution optical coherence tomography visualization of LASIK flap displacement. J Cataract Refract Surg. 2009;35:1640–1642. doi: 10.1016/j.jcrs.2009.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarunic MV, Asrani S, Izatt JA. Imaging the ocular anterior segment with real-time, full-range Fourier-domain optical coherence tomography. Arch Ophthalmol. 2008;126:537–542. doi: 10.1001/archopht.126.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Tang M, Zhang X, Salaroli CH, Ramos JL, Huang D. Pachymetric mapping with Fourier-domain optical coherence tomography. J Cataract Refract Surg. 2010;36:826–831. doi: 10.1016/j.jcrs.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. [Accessed November 26, 2010];Biometrika. 1986 73:13–22. Available at: http://www.biostat.jhsph.edu/~fdominic/teaching/bio655/references/extra/liang.bka.1986.pdf.
- 10.Rosa AM, Neto Murta J, Quadrado MJ, Tavares C, Lobo C, Van Velze R, Castanheira-Dinis A. Femtosecond laser versus mechanical microkeratomes for flap creation in laser in situ keratomileusis and effect of postoperative measurement interval on estimated femtosecond flap thickness. J Cataract Refract Surg. 2009;35:833–838. doi: 10.1016/j.jcrs.2008.12.038. [DOI] [PubMed] [Google Scholar]
- 11.Binder PS. Flap dimensions created with the IntraLase FS laser. J Cataract Refract Surg. 2004;30:26–32. doi: 10.1016/S0886-3350(03)00578-9. [DOI] [PubMed] [Google Scholar]
- 12.von Jagow B, Kohnen T. Corneal architecture of femtosecond laser and microkeratome flaps imaged by anterior segment optical coherence tomography. J Cataract Refract Surg. 2009;35:35–41. doi: 10.1016/j.jcrs.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Lohmann CP, Güell JL. Regression after LASIK for the treatment of myopia: the role of the corneal epithelium. Semin Ophthalmol. 1998;13:79–82. doi: 10.3109/08820539809059822. [DOI] [PubMed] [Google Scholar]
- 14.Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:804–811. doi: 10.1016/j.jcrs.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 15.Nordan LT, Slade SG, Baker RN, Suarez C, Juhasz T, Kurtz R. Femtosecond laser flap creation for laser in situ keratomileusis: six-month follow-up of initial U.S. clinical series. J Refract Surg. 2003;19:8–14. doi: 10.3928/1081-597X-20030101-03. [DOI] [PubMed] [Google Scholar]
- 16.Alió JL, Piñero DP. Very high-frequency digital ultrasound measurement of the LASIK flap thickness profile using the IntraLase femtosecond laser and M2 and Carriazo-Pendular microkeratomes. J Refract Surg. 2008;24:12–23. doi: 10.3928/1081597X-20080101-03. [DOI] [PubMed] [Google Scholar]
- 17.Reinstein DZ, Silverman RH, Sutton HFS, Coleman DJ. Very high-frequency ultrasound corneal analysis identifies anatomic correlates of optical complications of lamellar refractive surgery; anatomic diagnosis in lamellar surgery. Ophthalmology. 1999;106:474–482. doi: 10.1016/S0161-6420(99)90105-7. [DOI] [PubMed] [Google Scholar]
- 18.Erie JC, Patel SV, McLaren JW, Ramirez M, Hodge DO, Maguire LJ, Bourne WM. Effect of myopic laser in situ keratomileusis on epithelial and stromal thickness; a confocal microscopy study. Ophthalmology. 2002;109:1447–1452. doi: 10.1016/s0161-6420(02)01106-5. [DOI] [PubMed] [Google Scholar]
- 19.Gokmen F, Jester JV, Petroll WM, McCulley JP, Cavanagh HD. In vivo confocal microscopy through-focusing to measure corneal flap thickness after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:962–970. doi: 10.1016/s0886-3350(02)01275-0. [DOI] [PubMed] [Google Scholar]


