Abstract
Background
Pericardial and intra-thoracic fat depots may represent novel risk factors for obesity-related cardiovascular disease. We sought to determine the prevalence, distribution and risk factor correlates of high pericardial and intra-thoracic fat deposits.
Methods and Results
Participants from the Framingham Heart Study (n=3312; mean age 52 years, 48% women) underwent multi-detector CT imaging in 2002–2005; high pericardial and high intra-thoracic fat were defined based on the sex-specific 90th percentile for these fat depots in a healthy reference sample. For men and women, the prevalence of high pericardial fat was 29.3% and 26.3%, respectively, and high intra-thoracic fat was 31.4% and 35.3%, respectively. Overall, 22.1% of the sample was discordant for pericardial and intra-thoracic fat depots: 8.3% had high pericardial but normal intra-thoracic fat, and 13.8% had high intra-thoracic but normal pericardial fat. Higher body mass index, higher waist circumference (WC) and increased prevalence of metabolic syndrome were more likely in participants with high intra-thoracic fat depots than with high pericardial fat (p<0.05 for all comparisons). High abdominal visceral adipose tissue was more frequent in participants with high intra-thoracic adipose tissue compared to those with high pericardial fat (p<0.001). Intra-thoracic fat, but not WC, was more highly correlated with VAT (r=0.76 and 0.78 in men and women, respectively; p<0.0001) than with SAT (r=0.46 and 0.54 in men and women, respectively; p<0.0001).
Conclusions
Although prevalence of pericardial fat and intra-thoracic fat were comparable at 30%, intra-thoracic fat correlated more closely with metabolic risk and visceral fat. Intra-thoracic fat may be a potential marker of metabolic risk and visceral fat on thoracic imaging.
Keywords: pericardial fat, obesity, epidemiology
Obesity, an important risk factor for cardiovascular disease, has been steadily rising in recent years.1 Visceral adipose tissue deposits mediate a significant part of the risk of obesity related vascular disease.2,3 Much of our understanding of the role of visceral adipose tissue has been derived from fat depots in the abdomen. However, emerging evidence suggests that thoracic visceral fat deposits, such as pericardial fat, may also have important cardiovascular effects that are locally mediated due to their proximity to cardiac structures.4–7 Pericardial fat deposits have been reported to be highly metabolically active and to secrete several vasoactive and inflammatory mediators.8 Increased pericardial fat has also been associated with measures of increased adiposity, adverse cardiovascular risk factor profiles and prevalent cardiovascular disease (CVD).6,7 Intra-thoracic fat does not appear to have the same local cardiovascular effects as pericardial fat, possibly due its lack of contiguity with cardiac structures. However, high levels of intra-thoracic fat may represent a marker for increased visceral adipose tissue. Due to the expanding cardiovascular indications for thoracic imaging, data on thoracic adipose tissue may be more readily available than abdominal visceral adipose tissue as a measure of cardiovascular and metabolic risk.
Despite the importance of pericardial fat and other intra-thoracic fat deposits as potential novel cardiovascular risk factors, the prevalence and age-distribution of pericardial and intra-thoracic fat have not been evaluated in a community-based sample. Furthermore, due to the highly correlated nature of pericardial, intra-thoracic and abdominal visceral fat, their respective contributions to metabolic risk have not been well established. We sought to estimate the prevalence and age distribution of these thoracic adipose deposits and to evaluate the metabolic risk factor profiles associated with different patterns of adipose tissue in the Framingham Offspring cohort, a middle aged community based sample.
Methods
Study Sample
The study sample consisted of participants from the Framingham Heart Study Offspring and Third Generation Cohorts who participated in the multi-detector CT (MDCT) sub-study between June 2002 and April 2005, as previously described.2,9,10 Of the 3529 participants in the MDCT sub-study, 3402 had interpretable values for both pericardial fat measures. An additional 55 participants were excluded for having previous CABG (which renders pericardial fat uninterpretable), 21 participants were excluded for a distant study visit, and 14 participants were excluded due to missing covariates, resulting in a total of 3312 individuals for the present investigation.
The study protocol was approved by the institutional review boards of the Boston University Medical Center and Massachusetts General Hospital. All subjects provided written informed consent.
MDCT Scan Protocol
Participants underwent 8-slice MDCT (LightSpeed Ultra, General Electric, Milwaukee, Wis) in the supine position with an average of 48 contiguous 2.5 mm slices of the heart using a prospectively ECG-triggered CT scanning protocol, as previously described.7 Participants also underwent a full thoracic scan after being briefly repositioned on the table. In addition, 25 × 5 mm thick slices (120 kVp, 400 mA, gantry rotation time 500 ms, table feed 3:1) were obtained spanning a 125-mm segment of the abdomen starting at the upper edge of S1.
Intrathoracic, Pericardial and Abdominal Fat Volume Measurements
Using a dedicated offline workstation (Aquarius 3D Workstation, TeraRecon Inc., San Mateo, CA) total thoracic and pericardial fat tissue volumes were measured. To determine the total thoracic and pericardial fat tissue volumes, a predefined image display setting based on Hounsfield units (HU) was used (window width −195 to −45 HU; window center −120 HU) which identified pixels that correspond with adipose tissue. Total thoracic and pericardial fat were quantified across the entire available imaging volume and were reported in cm3.
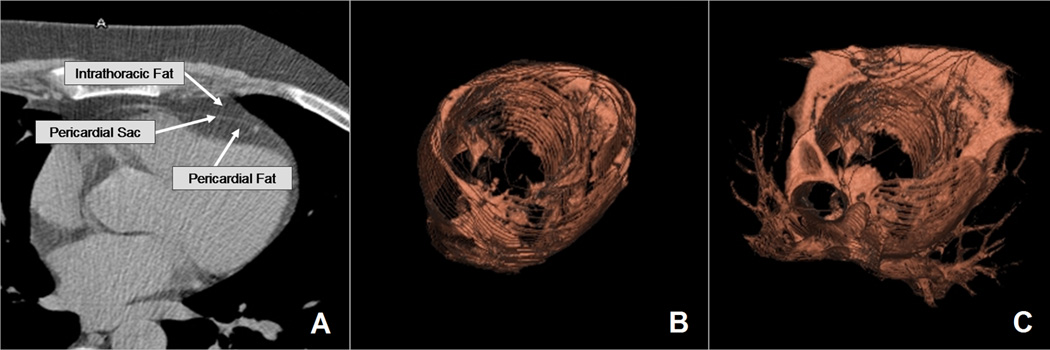
Using a semi-automatic segmentation technique, both total thoracic and pericardial fat volumes were determined as previously described.7,11 (Figure 1) Total thoracic fat volume was defined as total adipose tissue located within the lower two-thirds of the thorax (i.e. comprising the volume delimited by the level of the right pulmonary artery to the diaphragm and the chest wall to the descending aorta). Pericardial fat volume was defined as total adipose tissue measured within the pericardial sac. Intra-thoracic fat was derived as the difference between total thoracic fat and pericardial fat. Segmentation of the overall volume was automatically interpolated using the manually-defined tracings. When necessary, the reader made manual adjustments through the scan volumes to account for interpolating errors. On a random sample of 100 participants, intra- and inter-reader reproducibility was excellent for total thoracic fat and pericardial fat, as previously reported.7,12
Figure 1.
(A) Axial representation of pericardial fat and intrathoracic fat demonstrating pericardial fat borders and (B) three-dimensional reconstruction of pericardial fat (C) and total thoracic fat. (Reprinted from permission for the European Heart Journal6).
Visceral adipose tissue volumes (VAT) were assessed, as previously described,12 using the same image display windows as above (Aquarius 3D Workstation, TeraRecon Inc., San Mateo, CA). Intra- and inter-reader reproducibility was excellent for visceral abdominal fat, as previously reported.7,12
Risk Factor Assessment
Risk factors and covariates were measured at the seventh examination (1998 –2001) and at the first examination (2002–2005) for members of the Framingham Offspring and Third Generation Cohorts, respectively. Hypertension was defined as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or treatment with an antihypertensive agent. Total and high-density lipoprotein (HDL) cholesterol, serum triglycerides, and fasting plasma glucose were measured on fasting morning samples. Elevated triglycerides were defined as ≥150 mg/dL or treatment with a lipid-lowering agent. Low HDL was defined as <40 mg/dL (men) and <50 mg/dL (women). Diabetes mellitus was defined as fasting plasma glucose ≥126 mg/dL or treatment with a hypoglycemic agent and/or insulin; impaired fasting glucose was defined as fasting plasma glucose from 100 to 125 mg/dL in the absence of treatment for diabetes mellitus. Metabolic syndrome (MetS) was defined based on the Modified National Cholesterol Education Program Adult Treatment Panel III criteria.13 BMI was defined as weight (in kilograms) divided by the square of height (in meters) and WC was measured at the level of the umbilicus. Prevalent CVD included any prior coronary heart disease (including myocardial infarction, angina pectoris, or coronary insufficiency), stroke (thromboembolic or hemorrhagic infarction or transient ischaemic attack), intermittent claudication (defined as exertional calf discomfort relieved with rest), and congestive heart failure (according to the Framingham Heart Study CHF criteria14). All CVD events were adjudicated by a panel of three Framingham investigators after review of all available medical records and Framingham Heart Study examination records including examining physician notes.
Statistical Analysis
Fat volumes were estimated for the 5th, 10th, 25th, 50th, 75th, 90th and 95th percentiles stratified by age and sex. To determine the prevalence of high pericardial and intra-thoracic fat, a healthy referent sample was created by hierarchical exclusion of participants with the following covariates: BMI ≥ 30 kg/m2 (n=901); presence of hypertension (or use of anti-hypertensive medications), triglycerides ≥ 150 mg/dl or lipid treatment, low HDL cholesterol (<40 mg/dL in men and <50 mg/dL in women), IFG, diabetes or use of hypoglycemic medications (n=1515); prevalent CVD (n=3); current tobacco smoking (n=117); BMI < 18.5 kg/m2 (n=12), resulting in 285 men and 479 women in the healthy referent sample. We defined high pericardial and intra-thoracic fat based on fat volumes greater than the 90th percentile (sex-specific) from the healthy referent sample; participants with volumes equal or less than the 90th percentile were deemed to have “normal” volumes of pericardial or intra-thoracic fat. The 90th percentile was chosen to ensure adequate sample size in the healthy referent sample in order to provide statistically robust estimates for the fat volume cut-off values. Prevalence estimates of high pericardial or high intra-thoracic fat were stratified by sex and the following age categories: 35–44, 45–54, 55–64, 65–74, and 75–84.
To evaluate whether pericardial or intrathoracic fat was a better marker for indices of obesity and cardiometabolic risk factors, we examined sex-specific correlations between fat volumes and waist circumference, visceral abdominal fat volume and cardiometabolic risk factors. Furthermore, to establish the risk factor profiles associated with different patterns of thoracic adipose tissue, we stratified our sample into four mutually exclusive categories based on pericardial and intra-thoracic fat volumes: normal pericardial and intra-thoracic fat, high pericardial fat/normal intra-thoracic fat, normal pericardial fat/ high intra-thoracic fat, and high pericardial and intra-thoracic fat. We used a stratified analysis by category of fat distribution to evaluate the association between prevalence of cardiometabolic risk factors and each fat deposit due to the high degree of collinearity between the different regional fat deposits which frequently lead to unstable estimates of association with standard linear regression models. Differences across the four categories and between the discordant categories (high pericardial/normal intra-thoracic fat and normal pericardial/high intra-thoracic fat categories) were assessed by sex-specific age-adjusted logistic regression using the Wald Chi-square contrast approach in SAS PROC LOGISTIC for dichotomous covariates, and sex-specific age-adjusted analysis of variance using tests of effect for general contrasts in SAS PROG GLM for continuous covariates. We also evaluated the contributions of high pericardial and high intra-thoracic fat in the context of visceral abdominal fat using the same methods. Similar analyses were conducted using generalized estimating equation logistic regression and analysis of variance (using SAS PROC GENMOD for each analytical method) to account for the correlation within family, assuming the within-family correlation followed the compound symmetry structure. Results from GEE models (not shown) were virtually the same as the results presented here.
In secondary analyses, we further excluded all individuals from the healthy referent group that were overweight (BMI >=25 kg/m2) to create a lean healthy referent sample (n = 134 men and 337 women) to provide the distribution of pericardial and intra-thoracic fat volumes in healthy lean individuals. The thoracic fat volumes derived from this lean healthy reference sample may represent a better estimate of the normal physiological amounts of pericardial fat, but due to the small sample used to derive these cut-offs, these estimates may be less statistically robust and subject to more random error.
SAS version 9.1 was used to perform all computations; a two-tailed p-value <0.05 was considered significant. No adjustment was made for multiple comparisons due to the exploratory nature of this study.
Results
There were a total of 3312 participants, including 1707 men and 1605 women, eligible for this analysis. The clinical characteristics of the overall sample are described in Table 1.
Table 1.
Clinical Characteristics of Overall Sample
| Men | Women | |
|---|---|---|
| N | 1707 | 1605 |
| Age (years) | 49.4 ± 10.5 | 52.05 ± 9.9 |
| BMI (kg/m2) | 28.4 ± 4.6 | 27.08 ± 5.9 |
| Waist Circumference (cm) | 100.8 ± 11.9 | 93.2 ± 15.7 |
| Low HDL cholesterol (%) | 32.2 | 25.2 |
| Elevated triglycerides (%) | 43.1 | 26.7 |
| Hypertension (%) | 30.7 | 26.2 |
| Impaired fasting glucose (%) | 40.0 | 19.3 |
| Diabetes (%) | 7.2 | 4.9 |
| Metabolic Syndrome (%) | 37.2 | 27.3 |
| Current Smoking (%) | 13.7 | 12.5 |
| Hypertension treatment (%) | 18.3 | 18.2 |
| Lipid treatment (%) | 16.6 | 10.2 |
| Diabetes treatment (%) | 3.3 | 2.6 |
| Prevalent CVD, n (%) | 94 (5.7) | 56 (3.8) |
| Fat Volumes (cm3) | ||
| Pericardial Fat | 124.4 ± 46.2 | 100.4 ± 38.8 |
| Intra-thoracic Fat | 128.7± 64.4 | 66.3 ± 40.3 |
| Visceral abdominal Fat | 2211.6 ± 1010.8 | 1354.9 ± 829.2 |
Continuous variables expressed as mean±standard deviation. All values represent percentages (with absolute numbers in parentheses) except where specified otherwise.
BMI- Body mass index; HDL –High density lipoprotein; CVD – Cardiovascular Disease
Distribution of Pericardial and Intrathoracic Fat in the Community
The age- and sex-specific distribution for pericardial and intra-thoracic fat volumes are presented in Table 2. Both pericardial and intra-thoracic fat volumes increased with age into the 7th decade for all percentiles of fat. For the overall sample, the median values for pericardial fat volumes in men and women were 117.5 cm3 and 93.9 cm3, respectively, and for intra-thoracic fat volumes they were 117.7 cm3 and 58.4 cm3.
Table 2.
Volumes of Pericardial and Intra-thoracic fat by percentiles within age groups in men and women in the overall sample
| Pericardial fat Volumes (cm3) | ||||||||
|---|---|---|---|---|---|---|---|---|
| N | 5th | 10th | 25th | 50th | 75th | 90th | 95th | |
| Men | ||||||||
| 35–44 | 608 | 62.5 | 69.8 | 83.6 | 105.7 | 132.8 | 156.4 | 173.3 |
| 45–54 | 502 | 68.4 | 78.0 | 94.5 | 114.5 | 142.3 | 178.6 | 200.2 |
| 55–64 | 289 | 69.4 | 81.2 | 105.0 | 125.3 | 155.3 | 206.6 | 220.5 |
| 65–74 | 186 | 77.5 | 90.1 | 115.8 | 144.5 | 194.7 | 227.2 | 275.5 |
| 75–84 | 85 | 62.9 | 89.7 | 104.1 | 133.8 | 167.5 | 215.3 | 253.9 |
| Women | ||||||||
| 35–44 | 430 | 48.5 | 52.7 | 63.6 | 80.3 | 96.6 | 130.5 | 149.8 |
| 45–54 | 495 | 52.9 | 57.3 | 71.4 | 89.6 | 113.6 | 141.2 | 159.7 |
| 55–64 | 364 | 57.5 | 64.3 | 80.5 | 98.7 | 127.1 | 155.7 | 170.6 |
| 65–74 | 213 | 63.4 | 70.4 | 90.3 | 113.5 | 146.0 | 177.4 | 199.7 |
| 75–84 | 94 | 66.0 | 73.5 | 91.7 | 115.2 | 154.8 | 194.8 | 206.3 |
| Intra-thoracic Fat Volumes (cm3) | ||||||||
| N | 5th | 10th | 25th | 50th | 75th | 90th | 95th | |
| Men | ||||||||
| 35–44 | 608 | 35.6 | 46.2 | 67.2 | 95.8 | 136.4 | 186.2 | 219.9 |
| 45–54 | 502 | 51.9 | 63.8 | 82.3 | 114.5 | 161.0 | 217.4 | 249.9 |
| 55–64 | 289 | 61.4 | 70.5 | 105.4 | 134.6 | 180.1 | 231.0 | 263.0 |
| 65–74 | 186 | 77.1 | 89.6 | 120.6 | 158.6 | 204.8 | 252.5 | 278.7 |
| 75–84 | 85 | 55.3 | 81.4 | 116.0 | 145.7 | 190.2 | 232.8 | 266.4 |
| Women | ||||||||
| 35–44 | 430 | 17.9 | 20.6 | 27.0 | 39.0 | 56.0 | 83.9 | 98.2 |
| 45–54 | 495 | 21.1 | 24.5 | 33.1 | 47.5 | 73.8 | 109.7 | 130.1 |
| 55–64 | 364 | 30.3 | 36.0 | 50.9 | 73.0 | 97.1 | 136.1 | 155.9 |
| 65–74 | 213 | 38.0 | 47.3 | 66.1 | 86.8 | 117.6 | 157.4 | 177.0 |
| 75–84 | 94 | 34.5 | 44.7 | 65.8 | 84.3 | 107.5 | 138.9 | 157.0 |
Prevalence of high pericardial fat and high Intra-thoracic fat
Based on the age- and sex-specific 90th percentile cut-off for pericardial fat and intra-thoracic fat volumes, we defined a group of participants with high pericardial and intra-thoracic fat, respectively. The prevalence of high pericardial and high intra-thoracic fat stratified by age are reported in Table 3. The overall prevalence for pericardial fat was 29.3% (men) and 26.3% (women), and for intra-thoracic fat it was 31.4% (men) and 35.3% (women). A general trend of increasing prevalence of high pericardial and intra-thoracic fat deposits was also noted with increasing age. For both men and women, the prevalence of high thoracic depots peaked in the 65–74 age group, except for intra-thoracic fat in women which peaked in the 55–64 age group. A trend towards decreased prevalence of high intra-thoracic and pericardial deposits beyond the 7th decade was also observed.
Table 3.
Prevalence of High Pericardial Fat and Intra-Thoracic Fat by Age and Sex
| 35–44 | 45–54 | 55–64 | 65–74 | 75–84 | Overall | |
|---|---|---|---|---|---|---|
| Pericardial Fat | ||||||
| Women (%) | 13.3 | 19.8 | 32.4 | 49.8 | 42.6 | 26.3 |
| Men (%) | 17.8 | 27.3 | 37.0 | 53.8 | 43.5 | 29.3 |
| Intra-thoracic Fat | ||||||
| Women (%) | 12.8 | 22.5 | 31.7 | 24.8 | 11.2 | 35.3 |
| Men (%) | 20.0 | 29.5 | 38.4 | 54.8 | 48.2 | 31.4 |
High pericardial or intra-thoracic fat deposit defined as >90th percentile for fat volume in a healthy reference sample.
In a secondary analysis, we created a lean, healthy reference sample by further excluding overweight subjects. Using the 90th percentile cut-offs derived from this reference sample, the overall prevalence for pericardial fat was 43.8% (men) and 30.3% (women), and for intra-thoracic fat was 48.9% (men) and 46.6% (women).
Correlations between fat depots, waist circumference and metabolic risk factors
Waist circumference consistently had higher correlations with most cardiometabolic risk factors as compared to intra-thoracic, visceral abdominal or pericardial fat (Supplementary Table 1A and B). Both intra-thoracic fat and waist circumference were similarly associated with visceral abdominal fat (r= 0.76 and 0.72 for intra-thoracic fat and waist circumference, respectively, in men and r=0.72 and 0.72 for intra-thoracic fat and waist circumference, respectively, in women). More importantly, we found that intra-thoracic fat was more strongly correlated with visceral abdominal fat than with subcutaneous fat, whereas waist circumference was highly correlated with both visceral abdominal and subcutaneous fat.
Cardiovascular risk factor profiles by patterns of intra-thoracic and pericardial fat distribution
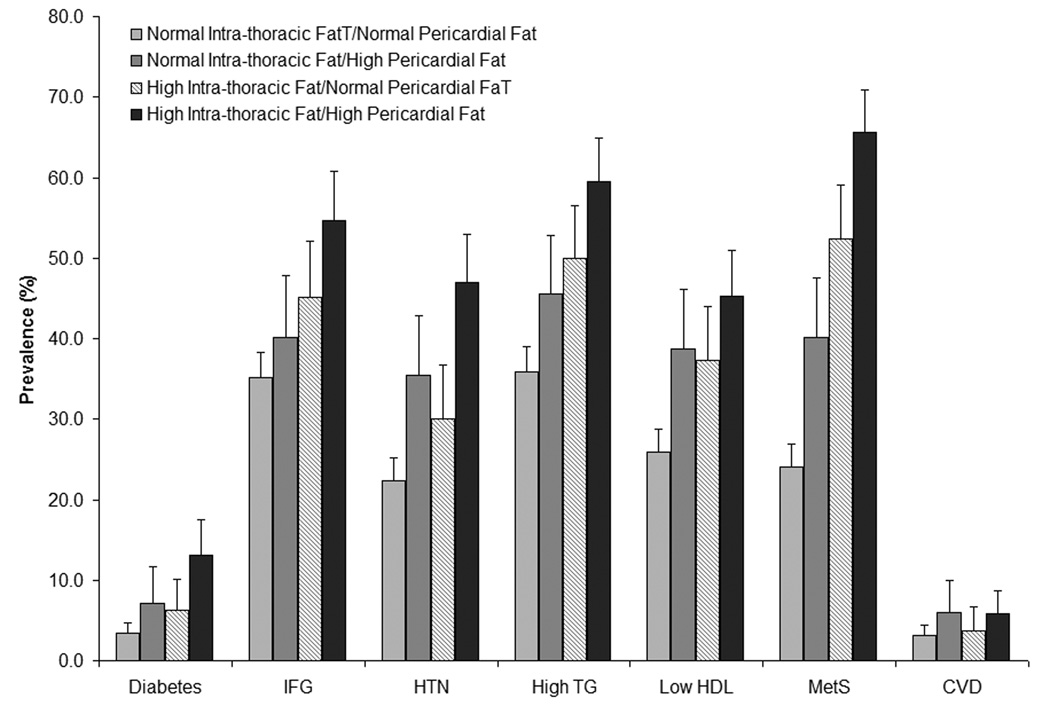
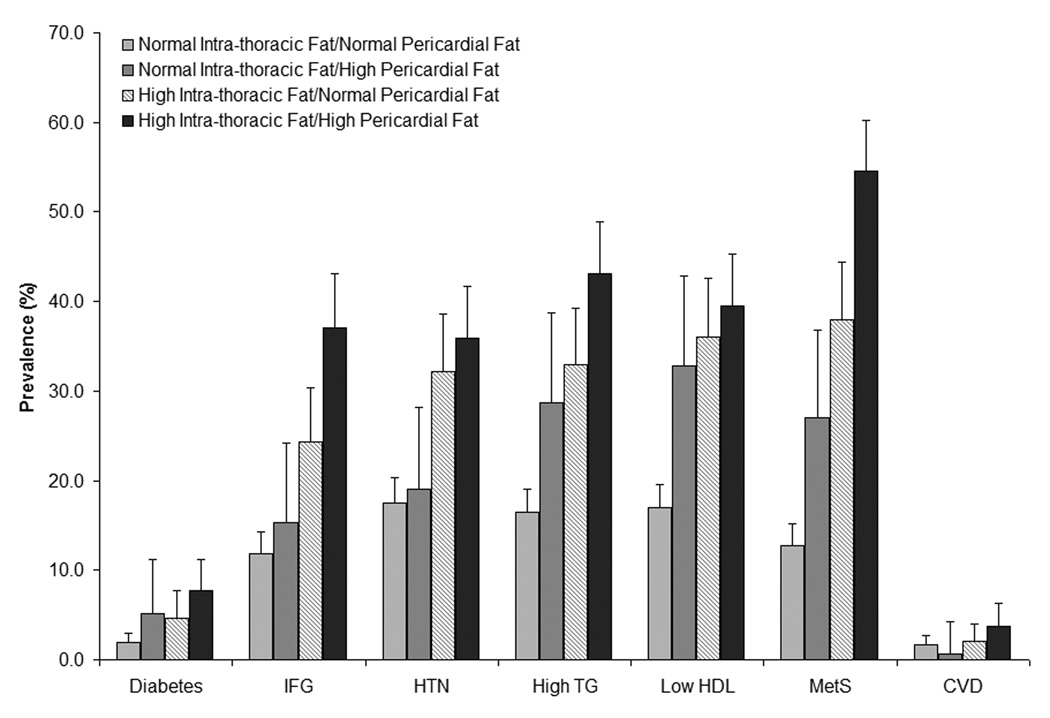
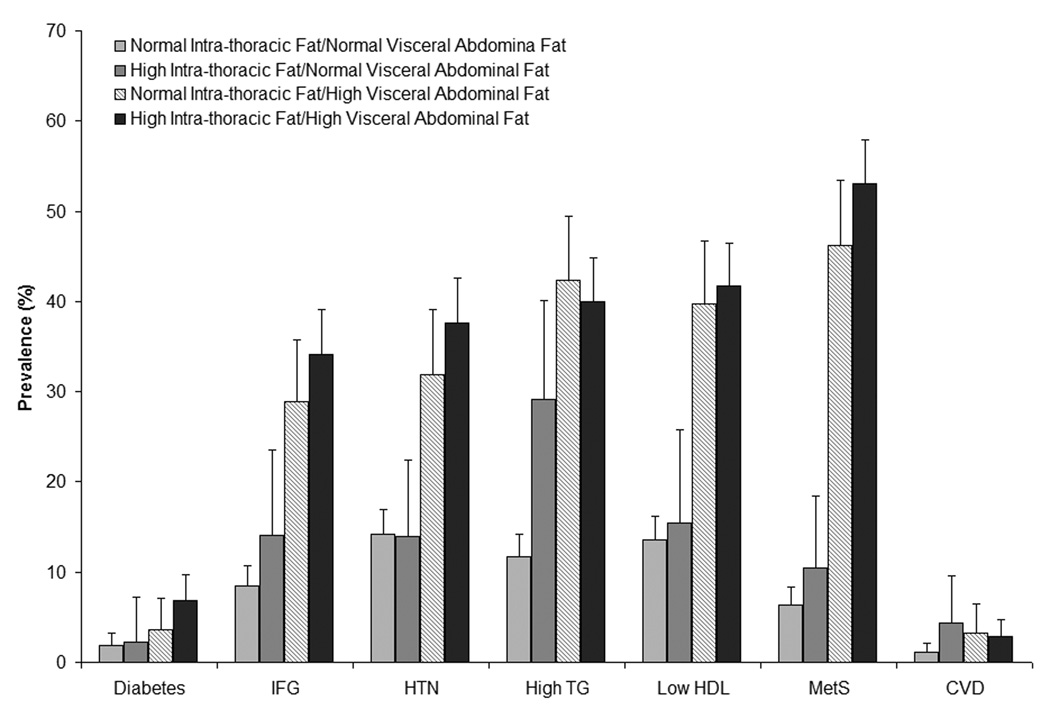
To evaluate the unique contributions of each regional fat depot to prevalent cardiovascular risk profiles, we examined risk factors across different patterns of fat distribution and specifically across groups discordant for thoracic fat deposits (Table 4 and Figure 1). In our sample, 23.1% of men and 20.9% of men were discordant for pericardial and intra-thoracic fat depots: 10.6% of men and 5.9% of women had high pericardial but normal intra-thoracic fat, and 12.5% of men and 15.0% of women had high intra-thoracic but normal pericardial fat. In both men and women, we observed a trend toward a higher prevalence for all cardiovascular risk factors, including diabetes, low HDL, hypertension and metabolic syndrome across categories of high intra-thoracic and pericardial fat deposits (p<0.001 for trend) (Figure 2). Prevalence of CVD also increased similarly, in both sexes, across categories of high intra-thoracic and high pericardial fat (p=0.04 and 0.02 for trend, in men and women, respectively). Measures of adiposity followed a similar trend with increased BMI, waist circumference and visceral abdominal fat volume across categories of high intra-thoracic and high pericardial fat deposits (Table 4).
Table 4.
Clinical Characteristics by Intra-thoracic and Pericardial Fat Categories
| P-values | ||||||
|---|---|---|---|---|---|---|
| Risk Factor | Normal Intra-thoracic Fat Normal Pericardial Fat |
Normal Intra-thoracic Fat High Pericardial Fat |
High Intra-thoracic Fat Normal Pericardial Fat |
High Intra-thoracic Fat High Pericardial Fat |
Between Discordant Categories |
Across All Categories |
| Men | ||||||
| N (%) | 998 (58.5) | 181 (10.6) | 215 (12.5) | 313 (18.3) | ||
| Age (yrs) | 47.0 | 50.5 | 50.6 | 55.54 | 0.95 | <0.0001 |
| BMI (kg/m2) | 26.7 | 29.1 | 30.2 | 32.28 | 0.01 | <0.0001 |
| WC (cm) | 96.0 | 103.4 | 105.7 | 111.09 | 0.03 | <0.0001 |
| Fat Volume (cm3) | ||||||
| Intra-thoracic | 90.5 | 118.3 | 190.4 | 214.2 | <0.0001 | <0.0001 |
| Pericardial | 99.1 | 162.1 | 116.8 | 188.55 | <0.0001 | <0.0001 |
| Visceral abdominal | 1726.5 | 2295.0 | 2759.8 | 3322.83 | <0.0001 | <0.0001 |
| Women | ||||||
| N (%) | 944 (58.8) | 95 (5.9) | 241 (15.1) | 325 (20.2) | ||
| Age (yrs) | 48.8 | 52.9 | 56.8 | 57.65 | 0.0004 | <0.0001 |
| BMI (kg/m2) | 24.6 | 27.4 | 30.0 | 32.15 | <0.0001 | <0.0001 |
| WC (cm) | 86.5 | 95.1 | 100.8 | 106.66 | 0.0003 | <0.0001 |
| Fat Volume (cm3) | ||||||
| Intra-thoracic | 43.2 | 56.0 | 94.3 | 117.24 | <0.0001 | <0.0001 |
| Pericardial | 78.8 | 138.6 | 96.0 | 154.96 | <0.0001 | <0.0001 |
| Visceral abdominal | 916.0 | 1336.3 | 1821.5 | 2293.7 | <0.0001 | <0.0001 |
BMI – body mass index; WC – waist circumference
Figure 2.
Prevalence of Cardiometabolic Risk Factors, Metabolic Syndrome and CVD by Intra-thoracic and Pericardial Fat Distribution Pattern in (A) Men and (B) Women. Age-adjusted p<0.001 for trend across categories of fat distribution for all covariates (except CVD where p=0.04 and 0.02 for trend, in men and women, respectively). *denotes p<0.05 for comparisons between discordant categories for high thoracic fat. Errors bars denote upper of the 95% confidence interval limit. IFG – Impaired fasting glucose; HTN – hypertension; TG – Triglycerides; HDL – High density lipoprotein; MetSyn – Metabolic Syndrome
In discordant subjects, with high intra-thoracic fat compared to those with high pericardial fat, the prevalence of metabolic syndrome was significantly higher in men (p<0.05), whereas hypertension, low HDL and metabolic syndrome were significantly higher in women (p<0.05 for all) (Figure 2). There was no statistically significant difference in the prevalence of CVD across discordant categories of pericardial and intra-thoracic fat. In both men and women, BMI, waist circumference, metabolic syndrome and visceral adipose tissue volumes were significantly higher in individuals with high intra-thoracic fat as compared to individuals with high pericardial fat (p<0.001 for all comparisons) (Table 4).
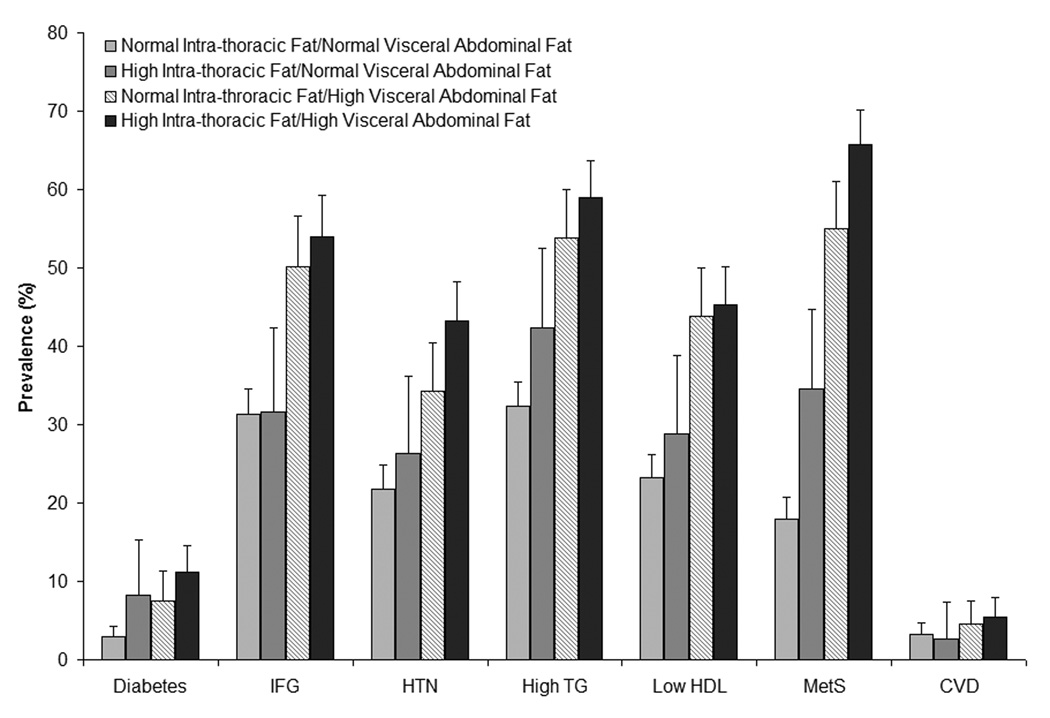
Cardiovascular risk factor profiles by patterns of intra-thoracic, pericardial and abdominal fat distribution
To further evaluate the contributions of intra-thoracic fat deposits on cardiovascular risk factor profiles in the context of abdominal visceral fat, we evaluated the prevalence of risk factors across different patterns of intra-thoracic and abdominal visceral fat distributions (Figure 3). We found evidence for a trend towards increasing prevalence of cardiac risk factors and metabolic syndrome across categories of high intra-thoracic fat and high visceral fat (p≤0.001 for trend). When individuals discordant for high intra-thoracic fat and high visceral abdominal fat were compared, a higher prevalence of high triglycerides, low HDL and metabolic syndrome was observed (p<0.001 for all) among individuals with high visceral fat compared to high intra-thoracic fat. A higher BMI and increased waist circumference was also identified for individuals with high visceral abdominal fat as compared to high intra-thoracic fat (p<0.001 for both). Similar results were also observed in sex-specific comparisons, except that hypertension was found to be more frequent in women, but not men, with high visceral abdominal fat as compared to high intra-thoracic fat.
Figure 3.
Prevalence of Cardiometabolic Risk Factors, Metabolic Syndrome and CVD by Intra-thoracic and Visceral Abdominal Fat Distribution Pattern in (A) Men and (B) Women.
Age-adjusted p<0.001 for trend across all categories of fat distribution for all covariates (except CVD where p=0.16 and 0.02 for trend, in men and women, respectively). *denotes p<0.05 for comparisons between discordant categories for high thoracic fat. Errors bars denote upper of the 95% confidence interval limit. IFG – Impaired fasting glucose; HTN – hypertension; TG – Triglycerides; HDL – High density lipoprotein; MetSyn – Metabolic Syndrome
When individuals discordant for high pericardial fat and high visceral abdominal fat were compared, all risk factors and measures of adiposity were higher among individuals with high abdominal visceral fat compared to high pericardial fat (Supplementary Table 2). None of the metabolic risk factors or measures of adiposity we examined tracked more closely with a thoracic fat depot (intra-thoracic or pericardial fat) as compared to visceral abdominal fat.
Discussion
In this community-based sample of more than three thousand middle-aged individuals, nearly one-third have high pericardial fat and high intra-thoracic fat volumes. When we further excluded overweight individuals from the healthy referent sample, the prevalence of high pericardial fat and high intra-thoracic fat was as high as ~40% and ~50%, respectively. By the 7th decade of life, nearly half of individuals in the community have increased pericardial and intrathoraic fat. We show that high intra-thoracic fat deposits are cross-sectionally associated with increased prevalence of cardiometabolic risk factors. Participants with both high pericardial fat and high intra-thoracic fat or those with both high intra-thoracic fat and high visceral abdominal fat were both found to have a more adverse cardiometabolic profiles compared to individuals with ≤1 high regional fat deposit.
To evaluate the contribution of each thoracic deposit to cardiometabolic risk, we examined participants discordant for pericardial and intra-thoracic fat deposits. Higher BMI, higher waist circumference and prevalent metabolic syndrome were more likely to track with high intra-thoracic fat than with high pericardial fat. Ultimately, we show that these risk factors track more closely with visceral abdominal fat than with either thoracic fat deposit, which underscores the importance of the abdominal visceral fat compartment as a marker of cardiometabolic risk. However, because visceral abdominal fat is not frequently available during cardiac imaging, we evaluated whether thoracic fat depots could be used as a proxy for visceral abdominal fat. We found that intra-thoracic fat was a better proxy for visceral abdominal fat than pericardial fat. More importantly, we also show that intra-thoracic fat is better able to discriminate between visceral abdominal fat and subcutaneous abdominal fat, as compared to waist circumference. This suggests that intra-thoracic fat may be a useful marker of visceral abdominal fat on thoracic imaging.
In the Context of the Current Literature
To our knowledge, there are no prior reports of the prevalence or distribution of thoracic fat deposits in the community. We present a comprehensive age- and sex-specific description of the distribution of such fat deposits in the community. Our estimates of prevalence of high pericardial and high intra-thoracic fat are consistent with current estimates of obesity in the US population of 32.2% 1 and the prevalence of high volumes of other regional adipose deposits such as high subcutaneous fat (30%) and high visceral abdominal fat (30%), which we have reported previously.15 High intra-thoracic fat in the context of high visceral abdominal fat may also be a marker of increased obesity-related cardiometabolic risk given the more adverse risk factor profile observed among patients with high levels of both abdominal and thoracic fat. Similar observations have also been reported for other regional fat deposits.7,15
Several studies have previously reported associations between pericardial fat, cardiometabolic risk factors and measures of adiposity.7,16–18 Iacobellis et al have reported that pericardial fat thickness, as measured by echocardiography, was associated with waist circumference, diastolic blood pressure and fasting insulin levels.17 We have shown that increased pericardial fat is associated with cardiovascular disease risk factors, prevalent CVD and coronary calcium.6,7 We and others have also reported that pericardial fat is highly correlated with visceral abdominal fat.7,16–18 We now extend these findings by demonstrating similar associations with intra-thoracic fat and cardiovascular risk factors. More importantly, we show that high intra-thoracic fat is more closely associated with an adverse cardiovascular risk factor profiles than high pericardial fat. Intra-thoracic fat, but not pericardial fat, also tracked more closely with increased measures of central adiposity and prevalent metabolic syndrome.
Our findings that intra-thoracic fat more closely relates to cardiometabolic risk factors than pericardial fat may also explain why pericardial fat, but not intrathoracic fat, has been independently associated with prevalent CVD6 and coronary artery calcium7. Our results indicate that the association between pericardial fat and CVD is unlikely mediated via conventional cardiometabolic risk factors, whereas the weak association between intra-thoracic fat and CVD may be mediated via these risk factors.
Potential Mechanisms
Visceral fat is emerging as a potentially important cardiovascular and metabolic risk factor. Given the highly collinear relationships between different fat deposits, the unique contributions of these thoracic fat deposits have previously remained largely unexplored. Due to the shared embryological origin between pericardial fat and visceral abdominal fat it has been hypothesized that pericardial fat could act as the regional depot for visceral fat accumulation in the chest.19 Our results suggest that intra-thoracic fat may, in fact, represent a better proxy for visceral fat accumulation in the thorax than pericardial fat.
Our findings that metabolic syndrome tracked with high intra-thoracic fat is likely due to the confounding effects of elevated levels of BMI, waist circumference and visceral adipose tissue observed among individuals with high intra-thoracic fat and not due to any specific properties of intra-thoracic fat. However, the association of increased measures of adiposity, visceral abdominal fat and prevalent metabolic syndrome with high intra-thoracic fat suggest that measures of intra-thoracic fat volumes could represent a potential marker for increased metabolic risk, particularly when volumetric data on visceral abdominal fat is unavailable.
Implications for Further Research
Given the expanding cardiovascular uses of thoracic CT imaging, intra-thoracic and pericardial fat volumes will be increasingly available in both clinical and research settings and could be used as a marker for increased metabolic risk. In the present paper, we have provided age- and sex-specific cut-points for volumes of thoracic fat deposits based on a healthy (including a lean healthy) reference sample derived from a community based cohort which could be used as a nomogram for future studies evaluating pericardial and intra-thoracic fat. It has been suggested that pericardial fat may be a modifiable risk factor as this fat deposit has been shown to decrease with exercise and diet.20,21 Our nomogram of thoracic fat volumes could be used to evaluate whether changes across percentiles lead to meaningful improvements in cardiovascular risk. Determining the specific fat volume cut-points associated with increased cardiometabolic risk longitudinally would significantly enhance our current nomogram and may be the subject of future research.
Strengths and Limitations
The major strengths of our study were the relatively large sample drawn from a community based cohort, which limited referral bias, and provided adequate power for a stratified analysis by regional fat distribution. We also used a highly reproducible CT volumetric assessment of fat deposits which represents the gold standard for fat quantification. Our study also had several limitations that deserve further comment. Our sample was derived from a primarily white community of European descent, therefore our results may not be generalizable to other ethnicities. Furthermore, our observational study used prevalent data to provide cross-sectional associations, and therefore we can not infer causality.
Conclusions
We have shown that approximately one third of a community-based sample have high pericardial and high intra-thoracic fat, potential novel cardiovascular and metabolic risk factors. Although visceral abdominal fat was most closely related to metabolic risk than any other fat depot, intra-thoracic fat was more highly correlated with cardiometabolic risk factors than pericardial fat. Intra-thoracic fat may represent a useful marker for increased metabolic risk and visceral fat on thoracic imaging.
Supplementary Material
Acknowledgments
Sources of Funding
Dr. Thanassoulis is supported by a Research Fellowship from the Canadian Institute of Health Research and the Fonds de Recherche en Santé du Québec. The Framingham Heart Study is supported by NIH Contract # N01-HC-25195. Dr. Vasan was supported in part by R01-DK-080739.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Subject codes: [8] Epidemiology; [30] CT and MRI; [135] Risk Factors; [150] Imaging
Disclosures: None
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB, Sr, O'Donnell CJ. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007;116:39–48. doi: 10.1161/CIRCULATIONAHA.106.675355. [DOI] [PubMed] [Google Scholar]
- 3.Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, Nevitt M, Holvoet P, Newman AB. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005;165:777–783. doi: 10.1001/archinte.165.7.777. [DOI] [PubMed] [Google Scholar]
- 4.Iacobellis G, Leonetti F, Singh N, M Sharma A. Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. International Journal of Cardiology. 2007;115:272–273. doi: 10.1016/j.ijcard.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. The American Journal of Cardiology. 2004;94:1084–1087. doi: 10.1016/j.amjcard.2004.06.075. [DOI] [PubMed] [Google Scholar]
- 6.Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, O'Donnell CJ, Fox CS, Hoffmann U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J. 2009;30:850–856. doi: 10.1093/eurheartj/ehn573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, O'Donnell CJ, Fox CS. Pericardial Fat, Visceral Abdominal Fat, Cardiovascular Disease Risk Factors, and Vascular Calcification in a Community-Based Sample: The Framingham Heart Study. Circulation. 2008;117:605–613. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 8.Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O'Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y. Human Epicardial Adipose Tissue Is a Source of Inflammatory Mediators. Circulation. 2003;108:2460–2466. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 9.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963;107:539–556. doi: 10.1111/j.1749-6632.1963.tb13299.x. [DOI] [PubMed] [Google Scholar]
- 10.Splansky GL, Corey D, Yang Q, Atwood LD, Cupples LA, Benjamin EJ, D'Agostino RB, Sr, Fox CS, Larson MG, Murabito JM, O'Donnell CJ, Vasan RS, Wolf PA, Levy D. The Third Generation Cohort of the National Heart, Lung, and Blood Institute's Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol. 2007;165:1328–1335. doi: 10.1093/aje/kwm021. [DOI] [PubMed] [Google Scholar]
- 11.Fox CS, Gona P, Hoffmann U, Porter SA, Salton CJ, Massaro JM, Levy D, Larson MG, D'Agostino RB, Sr, O'Donnell CJ, Manning WJ. Pericardial Fat, Intrathoracic Fat, and Measures of Left Ventricular Structure and Function: The Framingham Heart Study. Circulation. 2009;119:1586–1591. doi: 10.1161/CIRCULATIONAHA.108.828970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maurovich-Horvat P, Massaro J, Fox CS, Moselewski F, O'Donnell CJ, Hoffmann U. Comparison of anthropometric, area- and volume-based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi-detector computed tomography. Int J Obes (Lond) 2007;31:500–506. doi: 10.1038/sj.ijo.0803454. [DOI] [PubMed] [Google Scholar]
- 13.Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 14.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol. 1993;22:6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 15.Pou KM, Massaro JM, Hoffmann U, Lieb K, Vasan RS, O'Donnell CJ, Fox CS. Patterns of abdominal fat distribution: the Framingham Heart Study. Diabetes Care. 2009;32:481–485. doi: 10.2337/dc08-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fluchter S, Haghi D, Dinter D, Heberlein W, Kuhl HP, Neff W, Sueselbeck T, Borggrefe M, Papavassiliu T. Volumetric assessment of epicardial adipose tissue with cardiovascular magnetic resonance imaging. Obesity (Silver Spring) 2007;15:870–878. doi: 10.1038/oby.2007.591. [DOI] [PubMed] [Google Scholar]
- 17.Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, Di Mario U, Leonetti F. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003;88:5163–5168. doi: 10.1210/jc.2003-030698. [DOI] [PubMed] [Google Scholar]
- 18.Taguchi R, Takasu J, Itani Y, Yamamoto R, okoyama K, Watanabe S, Masuda Y. Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis. 2001;157:203–209. doi: 10.1016/s0021-9150(00)00709-7. [DOI] [PubMed] [Google Scholar]
- 19.Ho E, Shimada Y. Formation of the epicardium studied with the scanning electron microscope. Dev Biol. 1978;66:579–585. doi: 10.1016/0012-1606(78)90263-4. [DOI] [PubMed] [Google Scholar]
- 20.Iacobellis G, Singh N, Wharton S, Sharma AM. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity (Silver Spring) 2008;16:1693–1697. doi: 10.1038/oby.2008.251. [DOI] [PubMed] [Google Scholar]
- 21.Kim MK, Tomita T, Kim MJ, Sasai H, Maeda S, Tanaka K. Aerobic exercise training reduces epicardial fat in obese men. J Appl Physiol. 2009;106:5–11. doi: 10.1152/japplphysiol.90756.2008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.