Abstract
Cancer cachexia is a multifaceted syndrome characterized, among many symptoms, by extensive muscle wasting. Chronic systemic inflammation, partly triggered and sustained by cytokines, as well as increased oxidative stress contributes to the pathogenesis of this complex metabolic disorder. l-carnitine plays a central role in the metabolism of fatty acids and shows important antioxidant and anti-inflammatory properties. Systemic carnitine depletion has been described in several diseases, and it is characterized by fatigue, muscle weakness, and decreased tolerance to metabolic stress. In cachectic cancer patients, low serum carnitine levels have been reported, and this change has been suggested to play an important contributory role in the development of cachexia. Based on these data, carnitine supplementation has been tested in preliminary studies concerning human cachexia, resulting in improved fatigue and quality of life. We present here a review of clinical and experimental evidence regarding the use of carnitine supplementation in the management of cancer cachexia.
Keywords: l-carnitine, Cachexia, Cancer, Fatigue
Introduction
Cancer cachexia is a paraneoplastic syndrome present in 80% of terminally ill patients [1–3] and is markedly associated with adverse prognosis and shortened survival time [4, 5]. The symptoms include anorexia, weight loss, muscle loss, skeletal muscle atrophy, anemia, and alterations in carbohydrate, lipid, and protein metabolism [6]. Perhaps, one of the most relevant characteristics of cachexia is fatigue, which reflects the extensive muscle wasting associated with syndrome [5, 7, 8]. Actually, body protein depletion is one of the main trends of cachexia and involves not only skeletal muscle but also cardiac proteins, resulting in alterations in heart performance. This complex metabolic disorder is accompanied by an increase in local and systemic inflammatory mediators, such as proinflammatory cytokines [e.g., interleukin (IL)-6 and IL-8 and tumor necrosis factor-alpha (TNF-α)] [9, 10]. Another potential mediator is the imbalance of endogenous anabolic hormones (e.g., testosterone, insulin-like growth factor 1) and catabolic factors, such as glucocorticoids and myostatin [9, 11]. Moreover, tissue sensitivity to insulin is considerably reduced [12], and cellular prooxidant–antioxidant homeostasis is also disturbed with enhanced susceptibility to oxidant-induced stress [13].
Carnitine, a trimethylated amino acid roughly similar in structure to choline, facilitates the transfer of activated long-chain fatty acids from the cytoplasm to the mitochondria, where they are processed by oxidation to produce ATP [14]. It is involved in the transfer of the products of peroxisomal beta-oxidation to the mitochondria and in the removal of short-chain and medium-chain fatty acids from these organelles, in which it is responsible for maintaining coenzyme A levels. Carnitine thus plays a central role in the metabolism of fatty acids and energy by regulating the mitochondrial ratio of free coenzyme A to acyl-coenzyme A. Approximately 75% of carnitine in the organism is derived from dietary source [15], and red meat and dairy products are particularly rich in the amine, while 25% is synthesized in the liver and kidneys, from lysine and methionine [16]. The skeletal muscle and myocardium are carnitine-dependent, since they rely upon fatty acid oxidation as the main source of energy.
Patients with cancer are especially at risk for carnitine deficiency. They frequently present decreased caloric intake and increased metabolic requirements. In addition, pharmacological therapy interferes with carnitine absorption, synthesis, and excretion [17, 18]. The early studies by Winter et al. [19] reported carnitine deficiency in patients with chronic illness, including cancer. Recently, other studies have reported low serum levels of carnitine in cancer patients [20–25].
l-Carnitine supplementation has been shown to improve the patient’s condition in several diseases, including senile dementia, metabolic neuropathies, HIV infection, myopathies, cardiomyopathies, and renal failure [26, 27]. In experimental cachexia, carnitine supplementation significantly lowered the tumor-induced rise in triacylglycerol, as well as cytokine production [28]. We have recently found that l-carnitine supplementation improves liver lipid metabolism of tumor-bearing rats (submitted data). The gene expression of microsomal triglyceride transfer protein, and carnitine palmitoiltransferase (CPT I) catalytic activity are reduced in the liver of cachectic rats, which also show increased liver (150%) and plasma (3.3-fold) triacylglycerol content. l-carnitine supplementation (1 g/Kg/d) was able to reverse the reduction of CPT I catalytic activity, recovering liver metabolic capacity. Based on these data, carnitine supplementation has been tested in preliminary studies on human cachexia. We present here a review on clinical and experimental evidence concerning the use of carnitine supplementation in the management of cancer cachexia.
Muscle atrophy and cancer cachexia
Chronic systemic inflammation, triggered and sustained by cytokines as well as increased oxidative stress, contribute to the pathogenesis of cachexia. Skeletal muscle loss represents a key feature of cachexia, and recently, the advances in the field of molecular biology have shed light on the pathogenesis of this symptom. Recent findings indicate that muscle-specific genes (i.e., myosin heavy chain) and their products must be targeted to initiate muscle wasting [29]. Muscle atrophy occurs at different levels, starting from repressed gene expression, ending with accelerated protein degradation. Myogenesis is severely compromised, and disruption of sarcomere architecture is associated with proteolysis of contractile apparatus [12]. Furthermore, the studies show that, besides myofibrilar protein loss, apoptosis is also present in skeletal muscle of cachectic tumor-bearing animals [30] and human patients with cancer cachexia [31].
When loss of skeletal muscle is grounded by chronic inflammatory disease or cancer, the level of inflammatory cytokines is markedly elevated [32, 33]. For long, it has been known that TNF-α is the most prominent among them [34, 35], and some authors have reported that TNF-α is able to induce muscle protein loss [36, 37] and skeletal myocyte apoptosis both in vivo and in vitro [38, 39]. Figueras et al. [40] showed that, during experimental cachexia, the contribution of muscle-derived TNF-α is decreased; however, significant changes were observed in relation to TNF-α receptors at the skeletal muscle level that could possibly be related with muscle wasting associated with tumor growth. Recently, it was shown that, in the skeletal muscle of cachectic patients, there is increased expression and activity of TNF-α-related pathways, including TNF-α mRNA, activation of TNFR1, and TNF-α associated to TNFR1, and increased oxidative stress [41].
Trophic effect of l-carnitine on skeletal muscle
The muscle is the most prominent carnitine depository since it stores about 95% of the total carnitine contained in the adult human body, showing a concentration 70-fold greater than that of the plasma. Carnitine is critical for normal skeletal muscle bioenergetics [42], and indeed, skeletal muscle is greatly affected in states of carnitine deficiency.
We investigated the influence of different doses (0.1, 1.0, and 2.0 g /kg/day) and time intervals (1, 14, or 28 days) of oral l-carnitine supplementation upon plasma and muscle l-carnitine concentration, as well as upon some aspects of lipid metabolism in rats (submitted data). The highest increase of plasma l-carnitine was found in the groups supplemented for 14 days with 1.0 and 2.0 g, compared with the controls. On the other hand, the highest alteration in muscle l-carnitine content was found in the groups supplemented for 28 days with 0.1, 1.0, and 2.0 g. These results indicate that no proportional relationship can be found between plasma and muscle l-carnitine concentration and that the lowest dose (0.1 g) supplemented for 28 days is already able to induce the maximal muscle concentration. Therefore, supplementation with higher doses is not necessary to enhance muscle content. Furthermore, even increases over 120% of muscle l-carnitine concentration were not able to modify long-chain fatty acid uptake, fat content, and carnitine palmitoyltransferase I and II (CPT I and II) activity in the skeletal muscle of control animals.
Some studies have shown that l-carnitine may present an important role in the treatment of the myopathy induced by several etiologies. Long-term IV administration (12 months) of l-carnitine (2 g/day) to patients undergoing hemodialysis resulted in increased serum and muscle carnitine levels, together with hypertrophy and predominance of type I fibers [43] in the muscle. Another study [44] with uremic patients with some degree of muscular atrophy, reports that 24-week treatment with l-carnitine (2 g IV at the end of hemodialysis, or in dialysis solution, or per os twice daily) leads to an increase of about 7% in the diameter of type I and type IIa fibers, as well as to a reduction in atrophic fibers. No remarkable changes were documented in type IIb fibers [44]. These findings suggest a specific effect of l-carnitine on type I and IIa fibers, which are characterized by predominant oxidative metabolism and therefore require carnitine for fatty oxidation to produce energy.
Carnitine and oxidative stress
It has been widely shown that clinically significant oxidative stress takes place in patients with advanced cancer, as shown by augmented levels of reactive oxygen species (ROS) and decreased levels of glutathione peroxidase [45, 46]. Moreover, cancer-related anorexia/cachexia syndrome and oxidative stress alone or in combination are highly predictive of clinical outcome and survival [47, 48].
In skeletal muscle, ROS and nitrogen species are normally synthesized at low levels and are required for normal force production [49]. However, at high levels, they may suppress tissue antioxidant capacity, thus leading to oxidative stress. Oxidative imbalance is involved in several models of cancer-induced cachexia [50–52], and proteins are major targets of oxidative stress-derived effects on tissues [50, 53]. It was recently suggested that the ROS cascade regulates pathophysiologic signaling, leading to proteolysis and apoptosis, when these factors are present at high levels within myofibers [54]. Moreover, many studies suggest that cachexia is associated with a decrease in intracellular glutathione concentration in the muscle [55–57]. Decreased glutathione levels and increased glutathione disulphide/glutathione ratios have been observed in the skeletal muscle of weight-losing tumor-bearing mice [57]. l-carnitine treatment improved the tumor-induced decrease in muscular glutamate and glutathione levels and the increased plasma glutamate levels in tumor-bearing rodents [55].
Gramignano et al. [58] studied the efficacy of l-carnitine supplementation in a population of advanced cancer patients. l-carnitine administration (6 g/day for 4 weeks) led to a decreased ROS and increased glutathione peroxidase level, but not to a significant extent. However, other studies have demonstrated important effects of l-carnitine on oxidative stress, as in patients with renal disease [59], phenylketonuria [60], and nonalcoholic steatohepatitis [61], as well as on several experimental models of oxidative stress [62–64].
Carnitine and fatigue
Fatigue is the most common symptom experienced by patients with cancer [65]. Up to 80% to 96% of patients receiving chemotherapy and 60% to 93% of patients receiving radiation therapy report significant fatigue [66]. Only recently fatigue has been included among the most important symptoms in cancer patients, and its evaluation is still not routinely included among the symptoms attributable to the toxicity of chemotherapy [67]. There are multiple potential predisposing/etiologic factors, including cancer itself, treatment-related adverse effects, physiologic complications, impaired performance status, and psychological comorbidities, such as depression [65, 67]. Besides, tumor-induced cytokines and host-produced proinflammatory cytokines may represent a possible mechanism contributing to fatigue [68].
Recent research shows that some anticancer drugs interfere with carnitine network. An initial increase in plasma carnitine levels after initiation of chemotherapy and the development of carnitine deficiency during treatment with cisplatin, ifosfamide, or doxorubicin are reported [25]. The initial enhancement in plasma carnitine concentration may be associated with rapid tissue release into bloodstream to replace carnitine loss induced by chemotherapy [25]. Cisplatin causes reduction in glomerular filtration and tubular damage, and patients receiving this drug may have an increased loss of carnitine through the kidney [69]. The metabolic pathway of ifosfamide leads to formation of chloroacetyl-CoA, and the presence of chloroacetyl-carnitine is detected in urine [69]. This detoxification results in a secondary deficiency of carnitine in patients receiving ifosfamide. Doxorubicin also influences the carnitine system by decreasing heart concentration of free carnitine, free fatty acid oxidation, creatine phosphate, and oxygen uptake [70]. Additionally, anticancer therapy may affect the carnitine-dependent oxidation of fatty acids [17] and mitochondrial function [71–74].
Taken together, these data suggest that chemotherapy-induced damage of carnitine system and secondary deficiency of the molecule may cause fatigue due to impaired energy metabolism. Indeed, it is reasonable to hypothesize that carnitine repletion might be an effective strategy for the treatment of fatigue in this population.
A preliminary analysis to determine the effects of 1 week of l-carnitine supplementation in cancer patients with fatigue and carnitine deficiency showed a significant improvement on fatigue, depression, and sleep disruption [22]. A phase I/II open-label trial of l-carnitine supplementation in adult carnitine-deficient patients with advanced cancer reported similar results, since most of the patients who received l-carnitine experienced improved fatigue, mood, and sleep [75]. In another study, patients with advanced cancer receiving chemotherapy and presenting low levels of serum carnitine were treated with oral l-carnitine (4 g daily for 7 days) [21]. Fatigue was improved in the majority of patients, with the concomitant normalization of serum carnitine levels. In addition to these previously fatigue-related reported effects, an increase of lean body mass and appetite were also reported, which may explain the improvement of symptoms with respect to fatigue and quality of life [58]. Significant improvements in fatigue were also observed in a randomized phase III clinical trial, in which l-carnitine (4 g/day) was orally given to patients with advanced cancer [76].
Anti-inflammatory effects of l-carnitine
As previously reported, TNF-α have been implicated on the muscle protein loss in cancer cachexia [32–34]. Steffen, Lees, and Booth [77] reported that the administration of either soluble TNF receptor-1 or the general inhibitor of TNF-α production, pentoxifylline, attenuated losses in both body and skeletal muscle mass, and also reduced increases in ubiquitin proteasome pathway transcripts in an animal model of cardiac cachexia.
Some findings support the hypothesis that administration of l-carnitine attenuates the inflammatory process in pathological conditions; however, there are no data on cancer cachexia. In hypertense animals, l-carnitine supplementation was able to counteract the enhancement of IL-1β, IL-6, and TNF-α in the plasma and heart tissue [78]. Oral administration of l-carnitine (6 g/day for 2 weeks) to AIDS patients led to a significant decrease in serum TNF-α [79]. Moreover, studies report that l-carnitine decreases C-reactive protein, a positive acute phase protein that is increased in inflammation, in hemodialysis patients [80, 81]. l-carnitine treatment also was able to restore the age-related changes in the functions of inflammatory cells, and presented a protective role in the tissue destruction in inflammation by decreasing the superoxide anion production [82].
Furthermore, an interesting study showed that l-carnitine can transactivate glucocorticoid-responsive promoters in vitro, in a way similar to dexamethasone [83], suppressing the release of TNF-α and IL-2 by IFN-γ primed and/or LPS-stimulated human primary monocytes. The authors suggest that the immunomodulatory effects of l-carnitine may, at least in part, be mediated by activation of glucocorticoid receptor-α.
Safety
In most studies, a dose between 2 and 6 g of l-carnitine/day was adopted; however, little is known about the amin’s safety and tolerability in cancer patients. Cruciani et al. [75] reported that l-carnitine may be safely administered orally at doses up to 3,000 mg/day. Mild gastrointestinal effects (nausea and vomiting) may occur. Besides, the investigations indicate that although responses are variable, blood levels can be restored within only 1 week of supplementation, but it is unlikely that skeletal muscle levels are fully restored by the end of this period [22, 75].
Conclusions and future perspectives
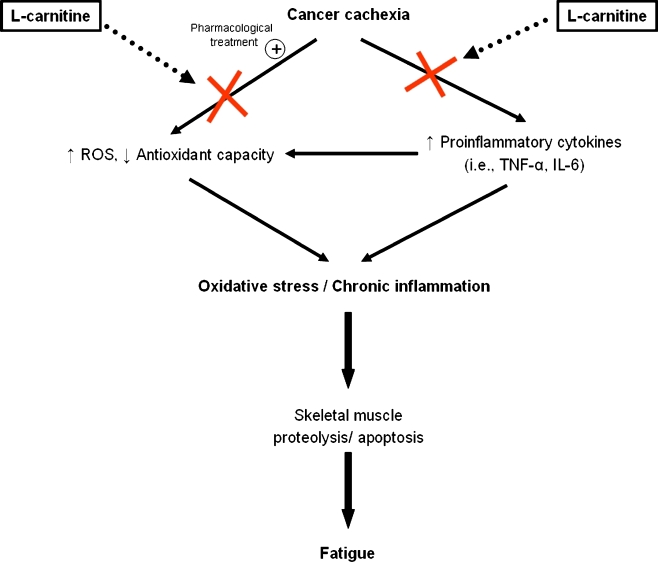
Since the levels of inflammatory cytokines as well as increased oxidative stress are related to cachexia, therapeutic strategies to ameliorate such conditions may be extremely important to counteract these deleterious effects. There is evidence that l-carnitine is able to reduce chronic inflammation and oxidative stress in cancer patients (Fig. 1). Considering the positive results supported by studies, l-carnitine appears a very interesting agent in the treatment of cancer cachexia. However, more clinical trials are needed to define the optimal use of l-carnitine as therapeutic agent to improve cachexia symptoms, as muscle atrophy, fatigue, and inflammatory/oxidative profile on cancer patients.
Fig. 1.
Action mechanism of l-carnitine on cancer cachexia
On the other hand, at the basic research level, it is important to comprehensively address the molecular pathways involved in the effect of l-carnitine supplementation and to extend the knowledge regarding the response of other organs and tissues, beyond the liver and muscle. We have shown, for instance, that the white adipose tissue, whose morphophysiology is severely affected by cachexia, is an important contributor to systemic inflammation during paraneoplastic syndrome and other mild chronic inflammatory diseases [84–87]. Therefore, it should be interesting to examine the effect of l-carnitine supplementation upon adipokines, which are not only mediators of inflammation, but are also involved in the regulation of oxidative balance, along with important metabolic effects.
There may also be potential beneficial effects of l-carnitine supplementation in regard to the central nervous system. Hypothalamic carnitine palmitoyltransferase is involved, along with fatty acid synthase in the regulation of the melanocortin system, and since many factors including TNF-α and IL-1 inhibit fatty acid oxidation [88, 89], it is conceivable that l-carnitine supplementation may affect energy intake in cachectic patients.
Taken together, the data available in the literature indicate that l-carnitine supplementation appears as a very interesting complementary therapy for cancer patients and that the study of the mechanisms underlying its effects should be carefully examined.
Acknowledgments
Conflict of interest
None.
The authors of this manuscript certify that they comply with the Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [90].
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Puccio M, Nathanson L. The cancer cachexia syndrome. Semin Oncol. 1997;24:277–287. [PubMed] [Google Scholar]
- 2.Nelson KA. The cancer anorexia–cachexia syndrome. Semin Oncol. 2000;27:64–68. [PubMed] [Google Scholar]
- 3.Davis MP, Dickerson D. Cachexia and anorexia: cancer’s covert killer. Support Care Cancer. 2000;8:180–187. doi: 10.1007/s005200050282. [DOI] [PubMed] [Google Scholar]
- 4.Barber MD, Ross JA, Fearon KC. Cancer cachexia. Surg Oncol. 1999;8:133–141. doi: 10.1016/S0960-7404(99)00045-6. [DOI] [PubMed] [Google Scholar]
- 5.von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle. 2010;1:1–5. doi: 10.1007/s13539-010-0002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Argilés JM, Alvarez B, López-Soriano FJ. The metabolic basis of cancer cachexia. Med Res Ver. 1997;17:477–498. doi: 10.1002/(sici)1098-1128(199709)17:5<477::aid-med3>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 7.von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1:129–133. doi: 10.1007/s13539-010-0014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Argilés JM, Garcia-Martínez C, Llovera M, López-Soriano FJ. The role of cytokines in muscle wasting: its relation with cancer cachexia. Med Res Rev. 1992;12:637–652. doi: 10.1002/med.2610120605. [DOI] [PubMed] [Google Scholar]
- 9.Tisdale MJ. Mechanisms of cancer cachexia. Physiol Rev. 2009;89:381–410. doi: 10.1152/physrev.00016.2008. [DOI] [PubMed] [Google Scholar]
- 10.Durham WJ, Dillon EL, Sheffield-Moore M. Inflammatory burden and amino acid metabolism in cancer cachexia. Curr Opin Clin Nutr Metab Care. 2009;12:72–77. doi: 10.1097/MCO.0b013e32831cef61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morley JE, Thomas DR, Wilson MM. Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr. 2006;83:735–743. doi: 10.1093/ajcn/83.4.735. [DOI] [PubMed] [Google Scholar]
- 12.Pajak B, Orzechowska S, Pijet B, Pijet M, Pogorzelska A, Gajkowska B, et al. Crossroads of cytokine signaling—the chase to stop muscle cachexia. J Physiol Pharmacol. 2008;59:251–264. [PubMed] [Google Scholar]
- 13.Orzechowski A, Ostaszewski P, Brodnicka A, et al. Excess of glucocorticoids impairs whole body antioxidant status in young rats. Relation to the effect of dexamethasone in soleus muscle and spleen. Horm Metab Res. 2000;32:174–180. doi: 10.1055/s-2007-978617. [DOI] [PubMed] [Google Scholar]
- 14.Bremer J. Carnitine—metabolism and functions. Physiol Rev. 1983;63:1420–1480. doi: 10.1152/physrev.1983.63.4.1420. [DOI] [PubMed] [Google Scholar]
- 15.Rebouche CJ. Quantitative estimation of absorption and degradation of a carnitine supplement by human adults. Metabolism. 1991;40:1305–1310. doi: 10.1016/0026-0495(91)90033-S. [DOI] [PubMed] [Google Scholar]
- 16.Mitwalli AH, Al-Wakeel JS, Alam A, Tarif N, Abu-Aisha H, Rashed M, et al. L-carnitine supplementation in hemodialysis patients. Saudi J Kidney Dis Transplant. 2005;16:17–22. [PubMed] [Google Scholar]
- 17.Visarius TN, Stucki JW, Lauterburg BH. Inhibition and stimulation of long-chain fatty acid oxidation by chloroacetaldehyde and methylene blue in rats. J Pharmacol Exp Ther. 1999;289:820–824. [PubMed] [Google Scholar]
- 18.Lancaster CS, Hu C, Franke RM, Filipski KK, Orwick SJ, Chen Z, et al. Cisplatin-induced downregulation of OCTN2 affects carnitine wasting. Clin Cancer Res. 2010;16:4789–4799. doi: 10.1158/1078-0432.CCR-10-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winter SC, Szabo-Aczel S, Curry CJ, Hutchinson HT, Hogue R, Shug A. Plasma carnitine deficiency. Clinical observations in 51 pediatric patients. Am J Dis Child. 1987;141:660–665. doi: 10.1001/archpedi.1987.04460060076039. [DOI] [PubMed] [Google Scholar]
- 20.Dodson WL, Sachan DS, Krauss S, Hanna W. Alterations of serum and urinary carnitine profiles in cancer patients: hypothesis of possible significance. J Am Coll Nutr. 1989;8:133–142. doi: 10.1080/07315724.1989.10720288. [DOI] [PubMed] [Google Scholar]
- 21.Graziano F, Bisonni R, Catalano V, Silva R, Rovidati S, Mencarini E, et al. Potential role of levocarnitine supplementation for the treatment of chemotherapy-induced fatigue in non-anaemic cancer patients. Br J Cancer. 2002;86:1854–1857. doi: 10.1038/sj.bjc.6600413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cruciani RA, Dvorkin E, Homel P, Culliney B, Malamud S, Shaiova L, et al. L-carnitine supplementation for the treatment of fatigue and depressed mood in cancer patients with carnitine deficiency: a preliminary analysis. Ann NY Acad Sci. 2004;1033:168–176. doi: 10.1196/annals.1320.016. [DOI] [PubMed] [Google Scholar]
- 23.Vinci E, Rampello E, Zanoli L, Oreste G, Pistone G, Malaguarnera M. Serum carnitine levels in patients with tumoral cachexia. Eur J Intern Med. 2005;16:419–423. doi: 10.1016/j.ejim.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Malaguarnera M, Risino C, Gargante MP, Oreste G, Barone G, Tomasello AV, et al. Decrease of serum carnitine levels in patients with or without gastrointestinal cancer cachexia. World J Gastroenterol. 2006;12:4541–4545. doi: 10.3748/wjg.v12.i28.4541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hockenberry MJ, Hooke MC, Gregurich M, McCarthy K. Carnitine plasma levels and fatigue in children/adolescents receiving cisplatin, ifosfamide, or doxorubicin. J Pediatr Hematol Oncol. 2009;31:664–669. doi: 10.1097/MPH.0b013e3181b259a7. [DOI] [PubMed] [Google Scholar]
- 26.Evangeliou A, Vlassopoulos D. Carnitine metabolism and deficit—when supplementation is necessary? Curr Pharm Biotechnol. 2003;4:211–219. doi: 10.2174/1389201033489829. [DOI] [PubMed] [Google Scholar]
- 27.Laviano A, Meguid MM, Guijarro A, Muscarioti M, Cascino A, Preziosa I, et al. Antimyopathic effects of carnitine and nicotine. Curr Opin Clin Nutr Metab Care. 2006;9:442–448. doi: 10.1097/01.mco.0000232905.89662.60. [DOI] [PubMed] [Google Scholar]
- 28.Winter BK, Fiskum G, Gallo LL. Effects of L-carnitine on serum triglyceride and cytokine levels in rat models of cachexia and septic shock. Br J Cancer. 1995;72:1173–1179. doi: 10.1038/bjc.1995.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y-P, Schwartz RJ. TNF-α regulates early differentiation of C2C12 myoblasts in an autocrine fashion. FASEB J. 2001;15:1413–1415. doi: 10.1096/fj.00-0632fje. [DOI] [PubMed] [Google Scholar]
- 30.van Royen M, Carbó N, Busquets S, Alvarez B, Quinn LS, López-Soriano FJ, et al. DNA fragmentation occurs in skeletal muscle during tumor growth: A link with cancer cachexia? Biochem Biophys Res Commun. 2000;270:533–537. doi: 10.1006/bbrc.2000.2462. [DOI] [PubMed] [Google Scholar]
- 31.Busquets S, Deans C, Figueras M, Moore-Carrasco R, López-Soriano FJ, Fearon KC, et al. Apoptosis is present in skeletal muscle of cachectic gastro-intestinal cancer patients. Clin Nutr. 2007;26:614–618. doi: 10.1016/j.clnu.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 32.Nakashima J, Tachibana M, Ueno M, Miyajima A, Baba S, Murai M. Association between tumor necrosis factor in serum and cachexia in patients with prostate cancer. Clin Cancer Res. 1998;4:1743–1748. [PubMed] [Google Scholar]
- 33.Karayiannakis AJ, Syrigos KN, Polychronidis A, Pitiakoudis M, Bounovas A, Simopoulos K. Serum levels of tumor necrosis factor-alpha and nutritional status in pancreatic cancer patients. Anticancer Res. 2001;21:1335–1358. [PubMed] [Google Scholar]
- 34.Tracey KJ, Wei H, Manogue KR, et al. Cachectin/tumor necrosis factor induces cachexia, anemia, and inflammation. J Exp Med. 1988;167:1211–1227. doi: 10.1084/jem.167.3.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garcia-Martinez C, Lopez-Soriano FJ, Argiles JM. Acute treatment with tumour necrosis factor—a induces changes in protein metabolism in rat skeletal muscle. Mol Cell Biochem. 1993;125:11–18. doi: 10.1007/BF00926829. [DOI] [PubMed] [Google Scholar]
- 36.Tessitore L, Costelli P, Baccino FM. Humoral mediation for cachexia in tumour-bearing rats. Br J Cancer. 1993;67:15–23. doi: 10.1038/bjc.1993.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y-P, Schwartz RJ, Waddell ID, Holloway BR, Reid MB. Skeletal muscle myocytes undergo protein loss and reactive oxygen-mediated NF-kB activation in response to tumor necrosis factor α. FASEB J. 1998;12:871–880. doi: 10.1096/fasebj.12.10.971. [DOI] [PubMed] [Google Scholar]
- 38.Dalla Libera L, Sabbadini R, Renken C, Ravara B, Sandri M, Betto R, et al. Apoptosis in the skeletal muscle of rats with heart failure is associated with increased serum levels of TNF-alpha and sphingosine. J Mol Cell Cardiol. 2001;33:1871–1878. doi: 10.1006/jmcc.2001.1453. [DOI] [PubMed] [Google Scholar]
- 39.Sabbadini RA, Danieli-Betto D, Betto R. The role of sphingolipids in the control of skeletal muscle function: a review. Ital J Neurol Sci. 1999;20:423–430. doi: 10.1007/s100720050062. [DOI] [PubMed] [Google Scholar]
- 40.Figueras M, Busquets S, Carbó N, Almendro V, Argilés JM, López-Soriano FJ. Cancer cachexia results in an increase in TNF-alpha receptor gene expression in both skeletal muscle and adipose tissue. Int J Oncol. 2005;27:855–860. [PubMed] [Google Scholar]
- 41.Ramamoorthy S, Donohue M, Buck M. Decreased Jun-D and myogenin expression in muscle wasting of human cachexia. Am J Physiol Endocrinol Metab. 2009;297:392–401. doi: 10.1152/ajpendo.90529.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brass EP. Supplemental carnitine and exercise. Am J Clin Nutr. 2000;72:618S–623S. doi: 10.1093/ajcn/72.2.618S. [DOI] [PubMed] [Google Scholar]
- 43.Spagnoli LG, Palmieri G, Mauriello A, Vacha GM, D’Iddio S, Giorcelli G, et al. Morphometric evidence of the trophic effect of L-carnitine on human skeletal muscle. Nephron. 1990;55:16–23. doi: 10.1159/000185912. [DOI] [PubMed] [Google Scholar]
- 44.Giovenali P, Fenocchio D, Montanari G, Cancellotti C, D’Iddio S, Buoncristiani U, et al. Selective trophic effect of L-carnitine in type I and IIa skeletal muscle fibers. Kidney Int. 1994;46:1616–1619. doi: 10.1038/ki.1994.460. [DOI] [PubMed] [Google Scholar]
- 45.Mantovani G, Macciò A, Madeddu C, Mura L, Gramignano G, Lusso Mr, et al. Quantitative evaluation of oxidative stress, chronic inflammatory indices and leptin in cancer patients: correlation with stage and performance status. Int J Cancer. 2002;98:84–91. doi: 10.1002/ijc.10143. [DOI] [PubMed] [Google Scholar]
- 46.Mantovani G, Macciò A, Madeddu C, Mura L, Massa E, Gramignano G, et al. Reactive oxygen species, antioxidant mechanisms, and serum cytokine levels in cancer patients: impact of an antioxidant treatment. J Environ Pathol Toxicol Oncol. 2003;22:17–28. doi: 10.1615/JEnvPathToxOncol.v22.i1.20. [DOI] [PubMed] [Google Scholar]
- 47.Mantovani G, Macciò A, Madeddu C, Mura L, Massa E, Mudu MC, et al. Serum values of proinflammatory cytokines are inversely correlated with serum leptin levels in patients with advanced stage cancer at different sites. J Mol Med. 2001;79:406–414. doi: 10.1007/s001090100234. [DOI] [PubMed] [Google Scholar]
- 48.Laviano A, Meguid MM, Preziosa I, Rossi Fanelli F. Oxidative stress and wasting in cancer. Curr Opin Clin Nutr Metab Care. 2007;10:449–456. doi: 10.1097/MCO.0b013e328122db94. [DOI] [PubMed] [Google Scholar]
- 49.Reid MB. Nitric oxide, reactive oxygen species, and skeletal muscle contraction. Med Sci Sports Exerc. 2001;33:371–376. doi: 10.1097/00005768-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 50.Barreiro E, de la Puente B, Busquets S, López-Soriano FJ, Gea J, Argilés JM. Both oxidative and nitrosative stress are associated with muscle wasting in tumour-bearing rats. FEBS Lett. 2005;579:1646–1652. doi: 10.1016/j.febslet.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 51.Gomes-Marcondes MC, Tisdale MJ. Induction of protein catabolism and the ubiquitin-proteasome pathway by mild oxidative stress. Cancer Lett. 2002;180:69–74. doi: 10.1016/S0304-3835(02)00006-X. [DOI] [PubMed] [Google Scholar]
- 52.Murr C, Fuith LC, Widner B, Wirleitner B, Baier-Bitterlich G, Fuchs D. Increased neopterin concentrations in patients with cancer: indicator of oxidative stress? Anticancer Res. 1999;19:1721–1728. [PubMed] [Google Scholar]
- 53.Butterfield DA, Poon HF, St Clair D, Keller JN, Pierce WM, Klein JB, et al. Redox proteomics identification of oxidatively modified hippocampal proteins in mild cognitive impairment: insights into the development of Alzheimer’s disease. Neurobiol Dis. 2006;22:223–232. doi: 10.1016/j.nbd.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 54.Powers SK, Kavazis AN, McClung JM. Oxidative stress and disuse muscle atrophy. J Appl Physiol. 2007;102:2389–2397. doi: 10.1152/japplphysiol.01202.2006. [DOI] [PubMed] [Google Scholar]
- 55.Breitkreutz R, Babylon A, Hack V, Schuster K, Tokus M, Böhles H, et al. Effect of carnitine on muscular glutamate uptake and intramuscular glutathione in malignant diseases. Br J Cancer. 2000;82:399–403. doi: 10.1054/bjoc.1999.0933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ushmorov A, Hack V, Dröge W. Differential reconstitution of mitochondrial respiratory chain activity and plasma redox state by cysteine and ornithine in a model of cancer cachexia. Cancer Res. 1999;59:3527–3534. [PubMed] [Google Scholar]
- 57.Hack V, Gross A, Kinscherf R, Bockstette M, Fiers W, Berke G, et al. Abnormal glutathione and sulfate levels after interleukin 6 treatment and in tumor-induced cachexia. FASEB J. 1996;10:1219–1226. doi: 10.1096/fasebj.10.10.8751725. [DOI] [PubMed] [Google Scholar]
- 58.Gramignano G, Lusso MR, Madeddu C, Massa E, Serpe R, Deiana L, et al. Efficacy of l-carnitine administration on fatigue, nutritional status, oxidative stress, and related quality of life in 12 advanced cancer patients undergoing anticancer therapy. Nutrition. 2006;22:136–145. doi: 10.1016/j.nut.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 59.Fatouros IG, Douroudos I, Panagoutsos S, Pasadakis P, Nikolaidis MG, Chatzinikolaou A, Sovatzidis A, Michailidis Y, Jamurtas AZ, Mandalidis D, Taxildaris K, Vargemezis V. L-carnitine Effects on Oxidative Stress Responses in Patients With Renal Disease. Med Sci Sports Exerc 2010 [Epub ahead of print] [DOI] [PubMed]
- 60.Sitta A, Barschak AG, Deon M, de Mari JF, Barden AT, Vanzin CS, et al. L-carnitine blood levels and oxidative stress in treated phenylketonuric patients. Cell Mol Neurobiol. 2009;29:211–218. doi: 10.1007/s10571-008-9313-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malaguarnera M, Gargante MP, Russo C, Antic T, Vacante M, Malaguarnera M, Avitabile T, Li Volti G, Galvano F. L-Carnitine Supplementation to Diet: A New Tool in Treatment of Nonalcoholic Steatohepatitis-A Randomized and Controlled Clinical Trial. Am J Gastroenterol. 2010 [Epub ahead of print]. [DOI] [PubMed]
- 62.Mansour HH. Protective role of carnitine ester against radiation-induced oxidative stress in rats. Pharmacol Res. 2006;54:165–171. doi: 10.1016/j.phrs.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 63.Shaker ME, Houssen ME, Abo-Hashem EM, Ibrahim TM. Comparison of vitamin E, L-carnitine and melatonin in ameliorating carbon tetrachloride and diabetes induced hepatic oxidative stress. J Physiol Biochem. 2009;65:225–233. doi: 10.1007/BF03180575. [DOI] [PubMed] [Google Scholar]
- 64.Augustyniak A, Skrzydlewska E. L-Carnitine in the lipid and protein protection against ethanol-induced oxidative stress. Alcohol. 2009;43:217–223. doi: 10.1016/j.alcohol.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 65.Kilgour RD, Vigano A, Trutschnigg B, Hornby L, Lucar E, Bacon SL, et al. Cancer-related fatigue: the impact of skeletal muscle mass and strength in patients with advanced cancer. J Cachexia Sarcopenia Muscle. 2010;1:177–185. doi: 10.1007/s13539-010-0016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stasi R, Abriani L, Beccaglia P, Terzoli E, Amadori S. Cancer-related fatigue: evolving concepts in evaluation and treatment. Cancer. 2003;98:1786–1801. doi: 10.1002/cncr.11742. [DOI] [PubMed] [Google Scholar]
- 67.Carroll JK, Kohli S, Mustian KM, Roscoe JA, Morrow GR. Pharmacologic treatment of cancer-related fatigue. Oncologist. 2007;1:43–51. doi: 10.1634/theoncologist.12-S1-43. [DOI] [PubMed] [Google Scholar]
- 68.Portenoy RK, Itri LM. Cancer-related fatigue: guidelines for evaluation and management. Oncol. 1999;4:1–10. [PubMed] [Google Scholar]
- 69.Peluso G, Nicolai R, Reda E, Benatti P, Barbarisi A, Calvani M. Cancer and anticancer therapy-induced modifications on metabolism mediated by carnitine system. J Cell Physiol. 2000;182:339–350. doi: 10.1002/(SICI)1097-4652(200003)182:3<339::AID-JCP4>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 70.Neri B, Cini-Neri G, Bartalucci S, Bandinelli M. Protective effect of L-carnitine on cardiac metabolic damage induced by doxorubicin in vitro. Anticancer Res. 1986;6:659–662. [PubMed] [Google Scholar]
- 71.Brady LJ, Brady OS. Hepatic and cardiac carnitine palmitoytransferase activity: effects of adriamycin and galactosamine. Biochem Pharmacol. 1987;36:3419–3423. doi: 10.1016/0006-2952(87)90320-0. [DOI] [PubMed] [Google Scholar]
- 72.Kashfi K, Israel M, Sweatman TW, Seshadri R, Cook GA. Inhibition of mitochondrial carnitine palmitoytransferases by adriamycin and adriamycin analogues. Biochem Pharmacol. 1990;40:1441–1448. doi: 10.1016/0006-2952(90)90438-Q. [DOI] [PubMed] [Google Scholar]
- 73.Velasco G, Sanchez C, Geelen MJ, Guzman M. Are cytoskeletal components involved in the control of hepatic carnitine palmitoytransferase I activity? Biochem Biophys Res Commun. 1996;224:754–759. doi: 10.1006/bbrc.1996.1095. [DOI] [PubMed] [Google Scholar]
- 74.Visarius TM, Bahler H, Kupfer A, Cerny T, Lauterburg BH. Thiodiglycolic acid is excreted by humans receiving ifosfamide and inhibits mitochondrial function in rats. Drug Metab Dispos. 1998;26:193–196. [PubMed] [Google Scholar]
- 75.Cruciani RA, Dvorkin E, Homel P, Malamud S, Culliney B, Lapin J, et al. Safety, tolerability and symptom outcomes associated with L-carnitine supplementation in patients with cancer, fatigue, and carnitine deficiency: a phase I/II study. J Pain Symptom Manage. 2006;32:551–559. doi: 10.1016/j.jpainsymman.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 76.Mantovani G, Macciò A, Madeddu C, Gramignano G, Serpe R, Massa E, et al. Randomized phase III clinical trial of five different arms of treatment for patients with cancer cachexia: interim results. Nutrition. 2008;24:305–313. doi: 10.1016/j.nut.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 77.Steffen BT, Lees SJ, Booth FW. Anti-TNF treatment reduces rat skeletal muscle wasting in monocrotaline-induced cardiac cachexia. J Appl Physiol. 2008;105:1950–1958. doi: 10.1152/japplphysiol.90884.2008. [DOI] [PubMed] [Google Scholar]
- 78.Miguel-Carrasco JL, Mate A, Monserrat MT, Arias JL, Aramburu O, Vázquez CM. The role of inflammatory markers in the cardioprotective effect of L-carnitine in L-NAME-induced hypertension. Am J Hypertens. 2008;21:1231–1237. doi: 10.1038/ajh.2008.271. [DOI] [PubMed] [Google Scholar]
- 79.De Simone C, Tzantzoglou S, Famularo G, Moretti S, Paoletti F, Vullo V, et al. High dose L-carnitine improves immunologic and metabolic parameters in AIDS patients. Immunopharmacol Immunotoxicol. 1993;15:1–12. doi: 10.3109/08923979309066930. [DOI] [PubMed] [Google Scholar]
- 80.Savica V, Santoro D, Mazzaglia G, et al. L-carnitine infusions may suppress serum C-reactive protein and improve nutritional status in maintenance hemodialysis patients. J Ren Nutr. 2005;15:225–230. doi: 10.1053/j.jrn.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 81.Duranay M, Akay H, Yilmaz FM, Senes M, Tekeli N, Yücel D. Effects of L-carnitine infusions on inflammatory and nutritional markers in haemodialysis patients. Nephrol Dial Transplant. 2006;21:3211–3214. doi: 10.1093/ndt/gfl356. [DOI] [PubMed] [Google Scholar]
- 82.Izgüt-Uysal VN, Ağaç A, Derin N. Effect of L-carnitine on carrageenan-induced inflammation in aged rats. Gerontology. 2003;49:287–292. doi: 10.1159/000071709. [DOI] [PubMed] [Google Scholar]
- 83.Alesci S, De Martino MU, Mirani M, Benvenga S, Trimarchi F, Kino T, et al. L-carnitine: A nutritional modulator of glucocorticoid receptor functions. FASEB J. 2003;17:1553–1555. doi: 10.1096/fj.02-1024fje. [DOI] [PubMed] [Google Scholar]
- 84.Yamashita AS, Lira FS, Rosa JC, Paulino EC, Brum PC, Negrão CE, Dos Santos RV, Batista ML Jr, Oller do Nascimento C, Oyama LM, Seelaender M. Depot-specific modulation of adipokine levels in rat adipose tissue by diet-induced obesity: The effect of aerobic training and energy restriction. Cytokine 2010 [Epub ahead of print]. [DOI] [PubMed]
- 85.Rosa Neto JC, Lira FS, Oyama LM, Zanchi NE, Yamashita AS, Batista ML, Jr, et al. Exhaustive exercise causes na anti-inflammatory effect in skeletal muscle and a pro-inflammatory effect in adipose tissue in rats. Eur J Appl Physiol. 2009;106:697–704. doi: 10.1007/s00421-009-1070-1. [DOI] [PubMed] [Google Scholar]
- 86.Lira FS, Rosa JC, Zanchi NE, Yamashita AS, Lopes RD, Lopes AC, et al. Regulation of inflammation in the adipose tissue in cancer cachexia: effect of exercise. Cell Biochem Funct. 2009;27:71–75. doi: 10.1002/cbf.1540. [DOI] [PubMed] [Google Scholar]
- 87.Machado AP, Costa Rosa LF, Seelaender MC. Adipose tissue in Walker 256 tumour-induced cachexia:possible association between decreased leptin concentration and mononuclear cell infiltration. Cell Tissue Res. 2004;318:503–514. doi: 10.1007/s00441-004-0987-2. [DOI] [PubMed] [Google Scholar]
- 88.Nachiappan V, Curtiss D, Corkey BE, Kilpatrick L. Cytokines inhibit fatty acid oxidation in isolated rat hepatocytes: synergy among TNF, IL-6, and IL-1. Shock. 1994;1:123–129. doi: 10.1097/00024382-199402000-00007. [DOI] [PubMed] [Google Scholar]
- 89.Laviano A, Inui A, Marks DL, Meguid MM, Pichard C, Fanelli FR, et al. Neural control of the anorexia-cachexia syndrome. Am J Physiol Endocrinol Metab. 2008;295:E1000–E1008. doi: 10.1152/ajpendo.90252.2008. [DOI] [PubMed] [Google Scholar]
- 90.von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle 2010;1:7–8. [DOI] [PMC free article] [PubMed]