Abstract
Loa loa (commonly known as the ‘African eye worm’) is a nematode commonly found in areas in and around the rainforests and swamps of Western and Central Africa. In recent years, due to an increase in international travel and migration various ‘exotic’ tropical diseases are being reported all over the world especially in Europe and North America. So far there have been no recent cases reported from the UK. This case report highlights one such case of Loa loa diagnosed recently in the UK. These filarial diseases should be considered in patients who present with unusual ocular or systemic symptoms if they have migrated or travelled from endemic areas in the recent past.
Background
In recent years, due to an increase in international travel and migration, various ‘exotic’ tropical diseases have been reported all over the world especially in Europe and North America. So far there have been no recent cases reported from the UK. This case report highlights one instance of Loa loa seen in the UK recently. These parasitic diseases should be kept in mind as a differential diagnosis for patients presenting with an acute red eye particularly when dealing with patients who have recently lived, worked or travelled through the affected regions.
Case presentation
A 37-year-old female French patient of African descent presented with an acute, painful, red, right eye of 3 days duration. There was no discharge, photophobia nor any visual disturbance. The patient, a native of the Congo, had been living in the UK for the past 6 months. She was HIV positive.
On examination, the right eye had severe conjunctival injection and chemosis. A live, long, thread-like worm was seen moving in the temporal subconjunctival space (video 1, figure 1A,B). The anterior chamber did not show any signs of inflammation and the posterior segment was normal. The left eye was unremarkable. The visual acuity in both eyes was 6/6 (0.0 LogMAR units).
Figure 1.

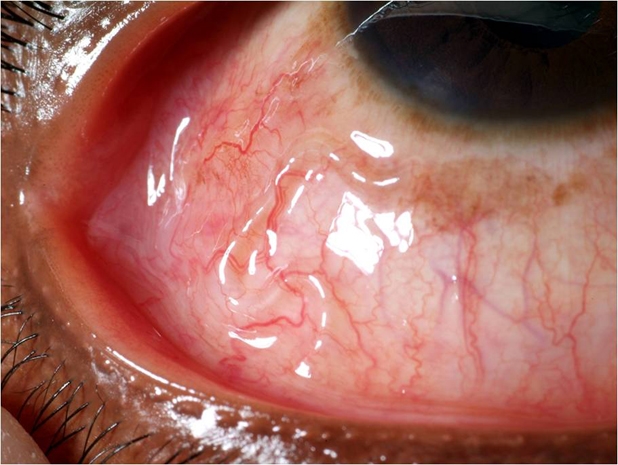
(A), (B) Right eye showing presence of Loa loa worm in temporal subconjunctival space.
There were no other systemic findings such as calabar swellings or skin nodules.
Video 1.
Live, mobile subconjunctival Loa loa in right eye.
Investigations
The worm was removed live and intact from the subconjunctival space under topical anaesthesia and sent for histopathological examination (figure 2). The parasite was later positively identified as a female Loa loa worm. The microbiological examination of day and night peripheral blood sample was done to identify the presence of microfilaria. The day time blood sample confirmed the presence of microfilariae of Loa loa. The microfilarial load, however, was low (55 per 20 ml of blood). There were no microfilaraemia in a night time sample.
Figure 2.

Female Loa loa after extraction from the eye.
The serological screening was done for other parasites before commencing treatment. The serology for strongyloidiasis, schistosomiasis, filariasis and toxoplasmosis was negative.
‘Skin snips’ from iliac crest, calf and ankle were done to look for any coexistent onchocerciasis. However, its microfilariae were not detected.
The patient had low haemoglobin (10.6 g/dl) and low ferritin (6.0 µg/l). No abnormal haemoglobinopathies were identified and patient was diagnosed with iron-deficiency anaemia. A differential blood count revealed eosinophilia.
The patient tested positive for HIV 1 and 2 antigen–antibodies. HIV RNA was not detected in the blood sample. The viral load was below the lowest detectable levels of 40 copies/ml of blood. The CD4 count was 495 cells/ µl (25%).
Serological tests for other infections such as cytomegalovirus, Epstein–Barr virus, hepatitis A, B and C, syphilis, cryptococcus and brucella were negative. Chest x-ray was unremarkable.
Differential diagnosis
Onchocerciasis: the parasitic infection caused by nematode Onchocerca volvulus. Ocular onhocerciasis may affect any part of the eyeball and may cause keratitis, iridocyclitis, choroiditis, glaucoma and optic neuritis and cause blindness (commonly known as ‘river blindness’). Loa loa, on the other hand, mainly involves subcutaneous and subconjunctival tissues.
Onchocerca is usually smaller in size than Loa loa.
The pattern of microfilaraemia in onchocerciasis is opposite to that in Loa loa.
The microfilaria of Loa loa is usually found in day blood sample. It is known to migrate to the skin and other tissues at night, which causes itchiness commonly reported in ‘night guards’ infested with the disease.
The microfilariae of onchocerciasis migrate from tissues to the blood at night, which makes it ideal to take a blood sample at night. Both parasitic infections may coexist in endemic regions.
Treatment
The worm was removed from the subconjunctival space under topical anaesthesia. A 2 mm incision was made in conjunctiva and the worm was removed live and intact with forceps. The light used for the procedure drew the parasite to bulbar conjunctiva and pilocarpine drops paralysed it, both of which aided the removal (pilocarpine is known to paralyse lashes lice before forceps removal, hence the analogy to try it here). Postoperatively, chloramphenicol eye drops were used four times a day for a week. Ocular inflammation subsided.
The systemic treatment was commenced to treat disseminated microfilariae. Initially the patient received a single dose of ivermectin to treat possible coexistent onchocerciasis as it cannot be completely ruled out by tests. A month later, diethylcarbamazine (DEC) was given for 21 days as a specific treatment for Loa loa. Ivermectin and DEC treatment were given under cover of steroid to suppress any inflammatory reaction.
The patient did not require any antiretroviral treatment for her HIV-positive status as her CD4 count was high and viral load was lower than the minimal detectable limit.
She also received oral ferrous sulphate for iron-deficiency anaemia.
Outcome and follow-up
The patient had no recurrence of ocular or systemic symptoms of Loa loa filariasis during the follow-up period of over a year. There were no microfilariae in subsequent blood samples. The HIV viral load continued to remain low, and high CD4 count was maintained. The patient is on regular monitoring for her immunological status.
Discussion
Loa loa, (commonly known as the ‘African eye worm’) is a nematode commonly found in areas around rainforests and swamps of Western and Central Africa. It is transmitted to humans by vectors, the deerfly (Chrysops silicea and C dimidiata) and mangofly found in these regions. The adult parasite is commonly seen in eye or within the subcutaneous tissues as itchy red swellings called ‘Calabar swellings’. The larval stage ‘microfilariae’ may be detected in blood. Ocular manifestations commonly involve the subconjunctival space; however, the worm has been reported to infest the eyelids and the anterior chamber.1 2 The management involves removal of adult worm and treatment of disseminated microfilariae. The treatment of systemic filariasis may be associated with severe inflammatory reaction, anaphylaxis and even encephalopathy caused by dying microfilariae. This response may be exaggerated in patients with high microfilarial load and those who are immunocompromised. Therefore, a steroid cover is necessary before and after treatment with DEC and ivermectin.
In 1996, Churchill et al3 reviewed the records of 100 cases of loiasis and reported on their clinical and laboratory features for the ‘Hospital for Tropical Diseases, London, UK’. The article reported the presence of the eyeworm as one of the causes of loiasis and stated the prevalence as being higher in African races.
In recent years, with an increase in world travel and migration, tropical diseases have been reported from European countries. Loa loa eye infestations specifically have been reported from Germany,4 Belgium,5 Italy,6 Spain,7 Norway8 and the Netherlands.9
There haven't been any recent case reports from the UK. The purpose of this case report is to complement the ever growing pool of information into the diagnosis of ocular parasitosis in the Western world.
Filarial diseases should be considered in patients with unusual ocular or systemic presentations, if they have migrated from, or travelled to, endemic areas in the recent past. A close liaison with parasitologists and a tropical medicine team are required for overall systemic management.
Learning points.
-
▶
This case of subconjunctival Loa loa from the UK reinforces the spread of ocular parasitosis in European nations.
-
▶
These parasitic diseases should be considered as a differential diagnosis for acute red eye when dealing with patients who have recently lived or travelled through endemic areas.
-
▶
The day and night blood sampling should be done to detect microfilarial load and other coexistent parasitic diseases.
-
▶
The treatment of filarial diseases in immunocompromised patients poses a unique challenge and requires special consideration.
Acknowledgments
I would like to acknowledge the support of Medical Illustration Department at Rotherham General Hospital in taking high quality video and photographs of this rare case. My special thanks to Mrs Joanne Carmichael, Mr Liam Carmichael and Mr Barry Farmer for their contribution.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Barua P, Barua N, Hazarika NK, et al. Loa loa in the anterior chamber of the eye: a case report. Indian J Med Microbiol 2005;23:59–60 [DOI] [PubMed] [Google Scholar]
- 2.Satyavani M, Rao KN. Live male adult Loa loa in the anterior chamber of the eye–a case report. Indian J Pathol Microbiol 1993;36:154–7 [PubMed] [Google Scholar]
- 3.Churchill DR, Morris C, Fakoya A, et al. Clinical and laboratory features of patients with loiasis (Loa loa filariasis) in the U.K. J Infect 1996;33:103–9 [DOI] [PubMed] [Google Scholar]
- 4.Stemmle J, Markwalder KA, Zinkernagel AS, et al. Loa loa infection of the eye - a case series. Klin Monatsbl Augenheilkd 2005;222:226–30 [DOI] [PubMed] [Google Scholar]
- 5.Carbonez G, Van De Sompel W, Zeyen T. Subconjunctival Loa loa worm: case report. Bull Soc Belge Ophtalmol 2002;45–8 [PubMed] [Google Scholar]
- 6.Aiello F, Palma S, Varesi C, et al. A rare case report of Loa loa ocular filariasis. Eur J Ophthalmol 2010;20:237–9 [DOI] [PubMed] [Google Scholar]
- 7.Herrero-Morín JD, Fernández González MN, González Rodríguez F, et al. Ocular filariasis due to Loa-loa. An emerging tropical parasitosis in Europe? An Pediatr (Barc) 2006;65:168–70 [DOI] [PubMed] [Google Scholar]
- 8.Varhaug P. Subconjunctival Loa loa: first case report from Norway. Acta Ophthalmol 2009;87:929–30 [DOI] [PubMed] [Google Scholar]
- 9.van Kortenhof NM, Jaspers CA, Sanders CJ. A patient with loiasis following a trip to Central Africa. Ned Tijdschr Geneeskd 2003;147:1327–9 [PubMed] [Google Scholar]


