Abstract
Head louse infestation (HLI) is one of the most frequently occurring parasitic diseases in children. This study was conducted to investigate the socioeconomic and personal factors influencing HLI in the Republic of Korea. A total of 2,210 questionnaires about various factors related to HLI were obtained from children in 17 primary schools throughout the country. The rate of HLI was significantly lower in children who lived together with mother or in a family where both parents worked. In addition, HLI was lower in children whose fathers or mothers were public officers or teachers. However, HLI was higher in children who had small families and washed their hair less often. Education levels of parents and the number of children in family were not significant. Improvement of socioeconomic factors and personal hygiene will be helpful for reducing HLI.
Keywords: Pediculus humanus capitis, head louse, risk factor, socioeconomic factor
Pediculus humanus capitis is an obligate parasite of humans that usually infests the scalp of children. Head louse infestation (HLI) is endemic worldwide with no strict limitation as to age, sex, and race [1,2]. HLI causes scalp itching, irritability, and occasional secondary bacterial infection as a result of scratching [3]. HLI also causes emotional and social distress because children believe that HLI is a result of poor personal hygiene. Although a recent report has shown that the overall prevalence of HLI in the Republic of Korea decreased to 4.1%, it is still estimated that more than 100,000 Korean children are plagued by the head louse [4].
Socioeconomic factors are important determinants of the occurrence of transmissible skin diseases. For example, low education and sharing beds are risk factors for scabies [5]. A growing body of evidence suggests that host factors, such as family income, hygiene, and the number of family, are related with HLI [6,7]. Although HLI is still a problem, there are currently limited data about human risk factors associated with HLI in Korea. The aim of this study was to examine socioeconomic conditions and personal factors influencing HLI.
The present study was carried out from September to December 2007 in 17 primary schools throughout the country. Six schools were in urban areas; 1 each in Seoul, Busan, Daejeon, Gyeonggi-do, Chungcheongnam-do, and Jeollabuk-do, and 11 schools in rural areas: 1 in Gyeonggi-do, 5 in Chungcheongbuk-do, 3 in Chungcheongnam-do, 1 in Jeollanam-do, and 1 in Gyeongsangnam-do. For the diagnosis of HLI, students were examined carefully by visual inspection of the scalp and hair for the presence of adult lice, nymphs, or viable nits. Nits which were within 1 cm from the scalp and plump, shiny and tan to coffee-colored with an intact operculum were considered viable. The students were subjected to questionnaire and data were obtained from the questionnaire. This included several questions on living together with parents, source of family income, parents' education levels and occupation, the number of family members and number of children in a family, the number of people sharing a room, and the number of hair washing per week. A total of 334 questionnaires were obtained from children with HLI and 1,876 questionnaires from children without HLI. Incomplete answers were excluded from the data. Statistical analysis was performed using chi-square test and the Student's t-test. P-values of <0.05 were considered significant.
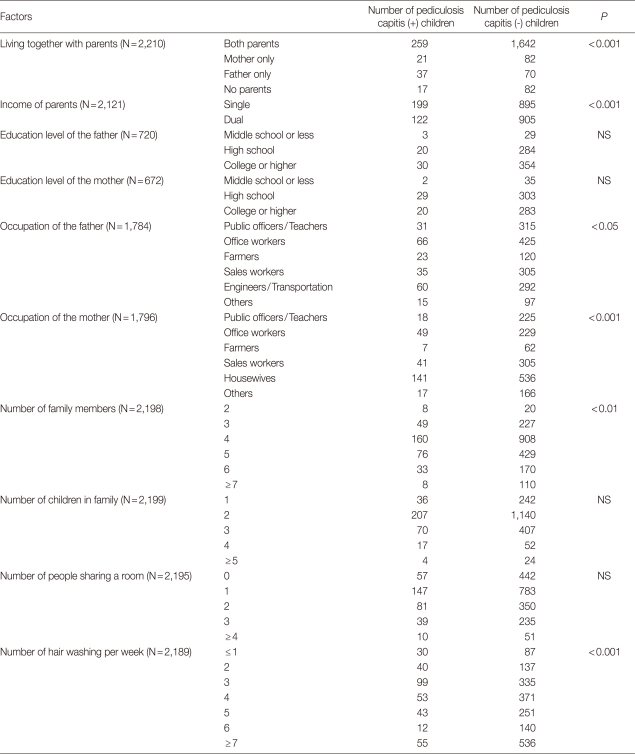
The socioeconomic and personal factors associated with HLI are presented in Table 1. Whether children were living together with parents was a significant factor associated with HLI. This is partial agreement with a previous report demonstrating that the infestation rate among children living with both parents was lower than that among children not living with both parents [8]. However, it is interesting to note that an important factor related to HLI is mother but not father. The children living with mother had lower infestation rates (P<0.001) but the children living with father did not (P=0.124). Mothers usually pay more attention to their children, which might be associated with this result. The rate of HLI was significantly decreased in 2-income family (P<0.001). Occupation of parents also affected the prevalence of HLI (P=0.018 for father's job; P<0.001 for mother's job). HLI was lower in children whose fathers or mothers were public officers or teachers, whereas HLI was higher in children whose mothers were housewives. Ciftci et al. [9] also found that the children whose mothers are housewives are easily infested by head lice. This indicates that stable jobs decrease the prevalence of HLI. There were no significant differences between education levels of parents and HLI. The number of family members living with the child was inversely correlated with HLI, while the number of children in a family did not affect HLI. The number of people sharing a room had a positive effect on HLI. However, the difference was not statistically significant (P=0.064). Previous reports showed that the increase in the size of family is the main factor facilitating the transmission of HLI [6,10]. It has been proposed that larger families may pay less attention to their children due to lack of support and financial limitations [11]. Contrary to common belief, our results indicate that large family decreases the risk of HLI. A previous report has shown that the infestation rates were positively correlated with the number of persons sleeping in a room. For example, the rates of infestation were 2% for living 2 persons, 3.5% for 3 persons, 4.8% for 4 persons, and 5.8% for 5 persons in a room, respectively [12]. Our results also showed a low correlation between the number of people sharing a room and HLI. These suggest that the increase in the number of people sharing a room but not the number of family member is a risk factor for HLI in Korea. A strong negative correlation was indicated between the number of hair washing per week and HLI (P<0.001). The average frequency of hair washing per week was 3.9 for infested children and 4.7 for not infested children. Our data confirmed previous findings that a low frequency of hair washing is responsible for HLI [13]. As expected, hygiene conditions in the house, such as consumption of water and washing facility, are known to affect the prevalence of HLI [7,14]. Hygiene education for children may be helpful in reducing HLI.
Table 1.
Association of pediculosis capitis with socioeconomic and personal factors in Korea
NS, not significant.
This is the first study describing in detail the risk factors related to HLI in Korea. In conclusion, we have presented evidence that several factors, such as living together with mother, family income, parents' occupation, size of family, and frequency of hair washing, were associated with HLI. These data could give rise to a baseline for monitoring children who are susceptible to HLI.
ACKNOWLEDGEMENTS
This work was supported by Konkuk University in 2010.
References
- 1.Gratz NG. Human lice. Their prevalence, control and resistance to insecticides-a review 1985-1997. 1997. Report WHO/CTD/WHOPES/978. [Google Scholar]
- 2.Nash B. Treating head lice. Brit Med J. 2003;326:1256–1257. doi: 10.1136/bmj.326.7401.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberts RJ. Clinical practice. Head lice. N Engl J Med. 2002;346:1645–1650. doi: 10.1056/NEJMcp012640. [DOI] [PubMed] [Google Scholar]
- 4.Oh JM, Lee IY, Lee WJ, Seo M, Park SA, Lee SH, Seo JH, Yong TS, Park SJ, Shin MH, Pai KS, Yu JR, Sim S. Prevalence of pediculosis capitis among Korean children. Parasitol Res. 2010;107:1415–1419. doi: 10.1007/s00436-010-2016-6. [DOI] [PubMed] [Google Scholar]
- 5.Raza N, Qadir SN, Agha H. Risk factors for scabies among male soldiers in Pakistan: case-control study. East Mediterr Health J. 2009;15:1105–1110. [PubMed] [Google Scholar]
- 6.Soultana V, Euthumia P, Antonios M, Angeliki RS. Prevalence of pediculosis capitis among schoolchildren in Greece and risk factors: a questionnaire survey. Pediatr Dermatol. 2009;26:701–705. doi: 10.1111/j.1525-1470.2009.01016.x. [DOI] [PubMed] [Google Scholar]
- 7.Buczek A, Markowska-Gosik D, Widomska D, Kawa IM. Pediculosis capitis among schoolchildren in urban and rural areas of eastern Poland. Eur J Epidemiol. 2004;19:491–495. doi: 10.1023/b:ejep.0000027347.76908.61. [DOI] [PubMed] [Google Scholar]
- 8.Sim S, Lee IY, Lee KJ, Seo JH, Im KI, Shin MH, Yong TS. A survey on head lice infestation in Korea (2001) and the therapeutic efficacy of oral trimethoprim/sulfamethoxazole adding to lindane shampoo. Korean J Parasitol. 2003;41:57–61. doi: 10.3347/kjp.2003.41.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciftci IH, Karaca S, Dogru O, Cetinkaya Z, Kulac M. Prevalence of pediculosis and scabies in preschool nursery children of Afyon, Turkey. Korean J Parasitol. 2006;44:95–98. doi: 10.3347/kjp.2006.44.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silva L, Alencar R de A, Madeira NG. Survey assessment of parental perceptions regarding head lice. Int J Dermatol. 2008;47:249–255. doi: 10.1111/j.1365-4632.2008.03570.x. [DOI] [PubMed] [Google Scholar]
- 11.Koch T, Brown M, Selim P, Isam C. Towards the eradication of head lice: literature review and research agenda. J Clin Nurs. 2001;10:364–371. doi: 10.1046/j.1365-2702.2001.00512.x. [DOI] [PubMed] [Google Scholar]
- 12.Ebomoyi EW. Pediculosis capitis among urban school children in Ilorin, Nigeria. J Natl Med Assoc. 1994;86:861–864. [PMC free article] [PubMed] [Google Scholar]
- 13.Ríos SM, Fernández JA, Rivas F, Sáenz ML, Moncada LI. Pediculosis prevalence and associated risk factors in a nursery school, Bogotá, Colombia. Biomedica. 2008;28:245–251. [PubMed] [Google Scholar]
- 14.Schenonel H, Lobos M. Pediculosis capitis, a permanent and renewed problem. Bol Chil Parasitol. 1997;52:73–76. [PubMed] [Google Scholar]