Abstract
OBJECTIVE
To identify distinct developmental patterns of diabetic retinopathy (DR) and assess the risk factor levels of patients in these clusters.
RESEARCH DESIGN AND METHODS
A cohort of 3,343 patients with type 2 diabetes mellitus (T2DM) monitored and treated in the Diabetes Care System West-Friesland, the Netherlands, was followed from 2 to 6 years. Risk factors were measured, and two-field fundus photographs were taken annually and graded according to the EURODIAB study group. Latent class growth modeling was used to identify distinct developmental patterns of DR over time.
RESULTS
Five clusters of patients with distinct developmental patterns of DR were identified: A, patients without any signs of DR (88.9%); B, patients with a slow regression from minimal background to no DR (4.9%); C, patients with a slow progression from minimal background to moderate nonproliferative DR (4.0%); D, patients with a fast progression from minimal or moderate nonproliferative to (pre)proliferative or treated DR (1.4%); and E, patients with persistent proliferative DR (0.8%). Patients in clusters A and B were characterized by lower risk factor levels, such as diabetes duration, HbA1c, and systolic blood pressure compared with patients in progressive clusters (C–E).
CONCLUSIONS
Clusters of patients with T2DM with markedly different patterns of DR development were identified, including a cluster with regression of DR. These clusters enable a more detailed examination of the influence of various risk factors on DR.
Diabetic retinopathy (DR) is a serious complication of type 2 diabetes mellitus (T2DM) and one of the main causes of blindness in the Western working population (1). Treatment of DR with photocoagulation and prevention of onset of DR through treatment of hyperglycemia and other risk factors are effective (2,3). Therefore, international guidelines recommend regular screening for DR in patients with diabetes (4). Several studies have shown that the prevalence of retinopathy as a complication of diabetes decreased in recent years compared with the 1980s. It is hypothesized that early detection of DR and adequate treatment of both DR and diabetes might have caused this decline in prevalence (5,6). Nonetheless, because the prevalence of T2DM is still increasing (7), a heavy burden on health care will be imposed because of increasing costs for diabetic treatment and prevention of complications (8,9). Previous longitudinal cohort studies, such as the Wisconsin Epidemiological Study of Diabetic Retinopathy, the UK Prospective Diabetes Study, and the Hoorn Study, have identified important associations between risk factors for and onset of DR or progression of DR (10–12). These studies considered DR as an end point with varying definitions, but none of the previous studies distinguished groups of patients with a different course of development of DR in time. To acknowledge these differential courses during the development of DR, time-dependent descriptions of the grading of DR in different groups of patients are needed to help guide determination of screening intervals. The aims of the current study were to identify and quantify distinct time-dependent developmental patterns of DR and to examine risk factors associated with these patterns.
RESEARCH DESIGN AND METHODS
Study population
Data were derived from a cohort (n = 4,933) of diabetic patients participating in the Diabetes Care System West-Friesland (DCS), the Netherlands, in the period from 1998 to 2005. The DCS coordinates regional diabetic care and provides additional care to diabetic care given by general practitioners. Details on this care system have been published (13). In brief, this system provides for annual physical examinations, with assessment of glucose control, cardiovascular risk profile, and complications of diabetes, including fundus photography, and supports self-management. Patient data of this annual visit and therapeutic advice are provided to the general practitioner of the patient to implement. In the study period between 1998 and 2005, patients entered the DCS in different years and with different diabetic duration. For each patient, the year of entry was considered baseline measurement (T0). Thus, patients who entered in the year 1998 could provide for up to eight visits. However, because only 349 of the 3,343 included patients had data at T7, we excluded the T7 visit and used data from T0 to T6 in the analysis. For the present analysis of the developmental patterns of DR, we excluded patients with type 1 diabetes (n = 49) and patients with only one or no visit with graded fundus photographs (n = 1,541). Although statistically significant, small differences were seen between included (n = 3,343) and excluded (n = 1,590) patients at T0; the excluded patients were 5.6 years older, included 6.2% more women, had a 1.8-year longer duration of diabetes, entered the DCS 1.7 years later, had a 2 mmHg lower diastolic blood pressure, had a 4 mmHg higher systolic blood pressure, had a 0.6 lower BMI, had a slightly more favorable lipid profile, and had 10% more insulin use than patients who were included in the study. No significant differences were observed in fasting plasma glucose (FPG), HbA1c, retinopathy prevalence, and smoking behavior.
Measurements
Height and weight were measured in barefoot patients wearing only light clothes. Systolic and diastolic blood pressures were measured on the right arm after 5 min of rest in a seated position using a random-zero sphygmomanometer (Hawksley-Gelman, Lancing, Sussex, UK); from 2003 on, an oscillometric device was used (Colin Press-Mate BP-8800, Komaki City, Japan). HbA1c was measured with high-performance liquid chromatography. FPG was measured by means of a hexokinase method (Roche Diagnostics GmbH, Mannheim, Germany). Levels of total cholesterol, HDL cholesterol, and triglycerides were measured using enzymatic techniques (Boehringer-Mannheim, Mannheim, Germany). Urinary albumin-creatinine ratio in milligrams per millimole was determined in an overnight first-voided urine sample. Urinary albumin was measured by rate nephelometry (Array Protein System; Beckman Coulter, Fullerton, CA), with an assay threshold of 2 mg/L. Urinary and serum creatinine were measured by a modified Jaffé test. Information on current medication use, smoking (yes/no), and year of onset of diabetes was obtained by self-report.
Retinopathy
Until 2000, fundus photography of both eyes was performed with a Kowa Pro Fundus camera with green filter (Kowa Optical Industry, Torrance, CA). Black and white 35-mm photographs were taken 30 min after mydriasis with 0.5% tropicamide and 2.5% phenylephrine eye drops. From the beginning of 2000 to 2004, fundus photography of both eyes was performed with a nonmydriatic Canon CR5 camera (Canon Inc., Tokyo, Japan). In 2004, fundus photography of both eyes was performed with a nonmydriatic Topcon TRC NW 100 camera (Topcon, Tokyo, Japan). All fundus photographs were 45 degrees of two fields: one field centered on the macula and one nasal field with the optic disc positioned on a disc-diameter from the temporal edge of the field, according to the EURODIAB protocol (14). If fundus photography at the DCS had failed or was missing, data on DR were retrieved from the patient’s medical file at the local hospital. All photographs were graded by an ophthalmologist according to the EURODIAB Study grading system, in which grade 0 is “no retinopathy,” grade 1 is “minimal nonproliferative retinopathy,” grade 2 is “moderate nonproliferative retinopathy,” grade 3 is “severe nonproliferative or preproliferative retinopathy,” grade 4 is “photocoagulated retinopathy,” and grade 5 is “proliferative retinopathy.” The EURODIAB grading does not provide for more detailed distinctions of specific diabetic changes in the retina, such as macular edema. In the DCS, the EURODIAB grades 4 and 5 have been combined in one grade, grade 4. In case of photocoagulation at the local hospital, any existing grade in the data of the DCS was changed to EURODIAB grade 4 at all time points after this therapy. If results of the grading of both eyes were available, the grading of the worst eye was used.
Statistical analysis
The year of entry in the DCS of each individual was considered as the baseline measurement (T0). The prevalence of DR per grade was calculated at baseline, as well as the prevalence of any DR (grades 1–4) at T0 to T6. Further analyses were conducted in two parts.
In part one, latent class growth modeling (LCGM) was used to identify distinct developmental patterns of DR (15). LCGM is a relatively new statistical technique used to analyze heterogeneity in the time course of, for example, DR. The underlying aim of the technique is to model this heterogeneity by identifying k number of distinct developmental patterns of DR called “clusters.” Individuals are allocated to one cluster on the basis of a similar pattern of development of retinopathy at all measurements. The allocation is done only once for each individual. To determine the optimal number of clusters, a “forward” approach was taken starting with a model with one developmental pattern, implying that all individuals in the study had the same course of DR. Subsequently, one cluster at a time was added, and the model fit was assessed by the Bayesian Information Criterion (BIC), which is often used when conducting such analyses (16). After each step of adding a new cluster, the model fit was considered better if the BIC decreased. The final number of clusters was derived on the basis of the forward approach assessed by a low BIC score and clinically relevant differences between clusters. If addition of a new cluster led to a model with two clinically indistinguishable developmental clusters, the model was not considered to be improved.
Individuals within each of the clusters have a probability of having each of the five EURODIAB grades of retinopathy. This probability varies over time and reflects the prevalence of DR. Identification of the retinopathy grade with the highest probability at each time point was used to derive a descriptive name of each cluster. The LCGM analyses were conducted with Mplus 5.21.
In part two of our analyses, differences between clusters in baseline characteristics (mean [SD] or proportion) were tested with an ANOVA with post hoc Bonferroni or χ2 tests. Baseline characteristics with a skewed distribution were calculated as median (interquartile range) within each cluster, and differences between clusters were analyzed by Kruskal–Wallis test. Trends in mean levels of HbA1c, systolic blood pressure, and total cholesterol were graphically compared between the clusters during follow-up (SPSS 15.0.2, SPSS Inc., Chicago, IL).
RESULTS
Prevalence of retinopathy stages
At baseline, our population with a mean age of 61.0 years (SD 11.3), 52.7% of whom were male, and a mean age at diagnosis of diabetes of 56.9 years (SD 11.5 years) (Table 1) had a prevalence of the separate EURODIAB grades of 87.4% for grade 0, 9.1% for grade 1, 2.0% for grade 2, 1.2% for grade 3, and 0.4% for grade 4. The prevalence of any DR (grades 1–4) was 12.7% at baseline, 14.3% at T1, 15.1% at T2, 14.6% at T3, 18.7% at T4, 14.6% at T5, and 16.9% at T6 (P value for trend = 0.001).
Table 1.
Differences in baseline characteristics between clusters of distinct developmental patterns of DR in the DCS population, the Netherlands
| Total DCS population | Cluster A: “persistent no DR” | Cluster B: “slow regression” | Cluster C: “slow progression from minimal to moderate DR” | Cluster D: “fast progression NPDR to PDR or treated DR” | Cluster E: “persistent PDR or treated DR” | P < 0.05 between clusters | |
|---|---|---|---|---|---|---|---|
| n (%) | 3,343 (100) | 2,971 (88.9) | 165 (4.9) | 135 (4.0) | 47 (1.4) | 25 (0.8) | |
| Age, years | 61.0 ± 11.3 | 60.7 ± 11.3 | 63.6 ± 10.6 | 62.7 ± 12.4 | 62.2 ± 10.1 | 63.3 ± 13.7 | A < B |
| Male, % | 52.7 | 52.9 | 60.6 | 47.4 | 40.4 | 36.0 | P = 0.023 |
| Diabetes duration, years | 2 (1–5) | 2 (1–5) | 4 (1–8.3) | 5 (3–10) | 9 (3.5–13) | 12.5 (7.75–19) | P < 0.001 |
| HbA1c, % | 7.7 ± 1.8 | 7.6 ± 1.8 | 7.8 ± 1.7 | 8.4 ± 1.8 | 9.1 ± 1.9 | 9.0 ± 1.8 | A < C/D/E, B < D/E |
| FPG, mmol/L | 8.9 ± 2.5 | 8.7 ± 2.5 | 9.1 ± 2.6 | 10.2 ± 2.8 | 10.5 ± 3.3 | 11.3 ± 4.2 | A < C/D/E, B < C/D/E |
| Systolic blood pressure, mmHg | 142 ± 21 | 142 ± 21 | 145 ± 22 | 150 ± 23 | 143 ± 23 | 153 ± 25 | A < C |
| Diastolic blood pressure, mmHg | 84 ± 11 | 84 ± 11 | 84 ± 10 | 86 ± 11 | 83 ± 11 | 83 ± 15 | NS |
| BMI, kg/m2 | 30.0 ± 5.3 | 30.1 ± 5.3 | 28.7 ± 4.9 | 29.5 ± 4.6 | 29.8 ± 5.4 | 32.6 ± 5.5 | B < A/E |
| Creatinine | 93.0 ± 16.4 | 93.0 ± 16.2 | 94.7 ± 17.3 | 92.3 ± 16.7 | 91.5 ± 20.1 | 97.8 ± 21.6 | NS |
| Albumin--creatinine ratio | 3.7 ± 14.9 | 3.2 ± 14.0 | 5.9 ± 19.9 | 7.0 ± 19.8 | 9.5 ± 24.2 | 12.6 ± 23.3 | A < C/D/E |
| Total cholesterol, mmol/L | 5.5 ± 1.1 | 5.5 ± 1.1 | 5.4 ± 0.9 | 5.8 ± 1.1 | 5.8 ± 1.2 | 5.9 ± 1.0 | B < C |
| HDL cholesterol, mmol/L | 1.20 ± 0.34 | 1.19 ± 0.32 | 1.23 ± 0.33 | 1.25 ± 0.62 | 1.17 ± 0.32 | 1.24 ± 0.37 | NS |
| LDL cholesterol, mmol/L | 3.4 ± 1.0 | 3.4 ± 1.0 | 3.4 ± 0.8 | 3.7 ± 1.0 | 3.7 ± 1.0 | 3.6 ± 0.9 | NS |
| Triglycerides, mmol/L | 2.0 ± 1.4 | 2.1 ± 1.4 | 1.8 ± 0.9 | 2.1 ± 1.5 | 2.2 ± 1.6 | 2.3 ± 1.2 | NS |
| Smoking, % | 21.2 | 21.6 | 23.6 | 14.1 | 14.9 | 12.6 | NS |
| OAD use, % | 67.8 | 67.0 | 73.4 | 82.0 | 59.1 | 70.8 | P = 0.002 |
| Insulin use, % | 7.7 | 6.0 | 13.9 | 20.3 | 36.4 | 41.7 | P < 0.001 |
| Both OAD medication and insulin, % | 3.9 | 3.3 | 7.0 | 11.7 | 6.8 | 12.5 | P < 0.001 |
| Antihypertensive use, % | 47.7 | 47.7 | 56.3 | 45.3 | 27.3 | 41.7 | P = 0.13 |
| Antilipid use, % | 22.4 | 23.3 | 17.1 | 13.3 | 15.9 | 16.7 | P = 0.22 |
Data represent mean ± SD, proportions, or median (interquartile range). Between-cluster differences were tested with ANOVA and post hoc Bonferroni for mean values, with χ2 tests for proportions and Kruskal–Wallis test for median values. NPDR, nonproliferative DR; PDR, proliferative DR; NS, nonsignificant; OAD, oral antidiabetic.
Course of retinopathy
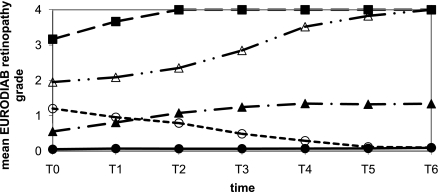
On the basis of the lower Bayes’ Information Criterion of a model with five clusters compared with a model with six clusters, the optimal number of clusters with distinct developmental patterns of DR was five (clusters A–E). This optimal number was also confirmed by clinical interpretation of the patterns of development of DR, which were distinct in the five cluster model. A model with six clusters did not provide a further clinically distinguishable developmental pattern.
These patterns of DR are depicted as mean EURODIAB grades per cluster in Fig. 1. The largest cluster A (n = 2,971, 88.9%) was characterized by “persistent no retinopathy.” Within cluster A, the probability for patients having no retinopathy (grade 0) was 0.92 or more at each of the 7 time points. The probabilities are shown in Supplementary Fig. 1. Cluster B (n = 165, 4.9%) was characterized as “slow regression.” Within cluster B, the highest probability for these patients was 0.81 of having either grade 0 or grade 1 retinopathy at T0, with a higher probability of having grade 1 (0.56) than grade 0 (0.25). Not only did the probability of having either grade 0 or 1 gradually increase over time to 0.99 at T6, but after T2, the probability of having grade 0 started being higher than the probability of having grade 1. Cluster C (n = 135, 4.0%) was characterized as “slow progression from minimal to moderate retinopathy,” including patients with a slow and gradual progression. Within cluster C, patients had a probability of 0.92 of having grade 0 or 1 at T0. This probability decreased gradually over time, and after T4 the probability of having a higher grade (grade 2 or 3) had increased to 0.22, which further increased to 0.35 at T6. Another cluster of progression was cluster D (n = 47, 1.4%), characterized as “fast progression from minimal or moderate to (pre)proliferative or treated retinopathy.” After 1 year the probability of having retinopathy grade 0, 1, or 2 already decreased for these patients from 0.81 to 0.62, with a further decrease through T2 and T3. After T4, the probability of having retinopathy grade 3 or 4 was 0.91 or more in cluster D. The final cluster E (n = 25, 0.8%) was characterized as “persistent proliferative or treated retinopathy.” The probability of having retinopathy grade 3 or 4 for these patients was 0.78 at T0, which even increased after 1 year to ≥0.95.
Figure 1.
Course of DR over 6 years in type 2 diabetic patients in the DCS, the Netherlands, 1998–2005. The year of entry in the DCS was considered baseline (T0). ●, cluster A “persistent no DR.” ○, cluster B “slow regression.” ▲, cluster C “slow progression from minimal to moderate nonproliferative DR.” △, cluster D “fast progression nonproliferative DR to PDR or treated DR.” ■, cluster E “persistent PDR or treated DR.” PDR, proliferative DR.
Characteristics
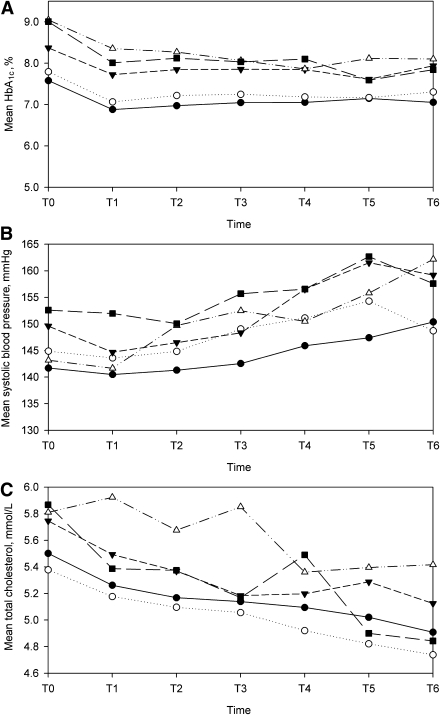
Between cluster differences of baseline characteristics can be seen in Table 1. At T0, patients in cluster A with “persistent no retinopathy” had a statistically significantly lower diabetes duration than patients in the other clusters. Mean HbA1c levels were lower in cluster A patients with at least 0.8% compared with patients in other clusters except for patients in cluster B “slow regression.” HbA1c in patients of cluster B “slow regression” was not statistically different from the HbA1c of patients in cluster C “slow progression from minimal to moderate retinopathy,” but the HbA1c in patients of cluster B was 1.3% lower than in patients of clusters D and E. Mean FPG was lower in patients of both clusters A and B compared with patients in clusters C, D, and E. In cluster A, 67% of the patients used oral antidiabetic medication, which was higher than in the “fast progressing” cluster D but lower than in all other clusters. Insulin use was highest in the progressive clusters C, D, and E, and lowest in cluster A. Combination therapy of insulin and oral antidiabetic medication was also significantly lower in cluster A compared with all other clusters. An 8 mmHg lower systolic blood pressure was seen in patients in cluster A “persistent no retinopathy” compared with patients in cluster C “slow progression from minimal to moderate retinopathy” at baseline. In both clusters A and C, a similar proportion of patients used antihypertensive medication (47.7 vs. 45.3%) at baseline. HbA1c, systolic blood pressure, and total cholesterol are shown per cluster as means at each time point in Fig. 2. For HbA1c and total cholesterol, a decrease was seen in all clusters over time. Patients in clusters A and B, the nonprogressive clusters, had lower mean values of HbA1c and total cholesterol than patients in the progressive clusters C, D, and E over time. An increase over time for all clusters was seen in systolic blood pressure. For patients in cluster C, who started to show an increase in retinopathy severity after T4, an increase of systolic blood pressure with ±15 mmHg was seen between T3 and T5. Patients in cluster D, with an increase in retinopathy severity after T1, showed an increase in systolic blood pressure of ∼10 mmHg after T1. Systolic blood pressure also increased in clusters A and B, but this increase never exceeded 5 mmHg in 1 year.
Figure 2.
Course of risk factors of DR over time. Mean HbA1c (A), systolic blood pressure (B), and total cholesterol (C) by clusters of the development of DR. ●, cluster A “persistent no DR.” ○, cluster B “slow regression.” ▲, cluster C “slow progression from minimal to moderate nonproliferative DR.” △, cluster D “fast progression nonproliferative DR to PDR or treated DR.” ■, cluster E “persistent PDR or treated DR.” PDR, proliferative DR.
CONCLUSIONS
In this study on the course of DR, we identified five clusters of developmental patterns of DR in patients with T2DM and assessed the risk factor levels of these clusters. The largest cluster (A) represents diabetic patients who did not develop any DR over a time period of 6 years. One cluster showing regression (B) represented patients who had a high probability of having minimal DR, which disappeared over time. Two progressive clusters (C and D) were identified that differed from each other in severity and in speed of developing DR. The smallest cluster (E) consisted of patients who had persistently (pre)proliferative DR or photocoagulation scars. Thus, in a large cohort of patients with T2DM, the majority of patients did not develop DR. Of the 372 patients in clusters B, C, D, and E who did develop DR, more than 44% (n = 165) showed regression in cluster B. The two progressive clusters C and D had persistently higher levels of risk factors than clusters A and B, with no or little retinopathy. Steep increases in systolic blood pressure in these progressive clusters were observed, which seemed to coincide with the point in time at which progression of DR occurred.
To our knowledge, LCGM has never been applied to longitudinal data on DR. LCGM is applicable because of the heterogeneous nature of DR. These analyses were performed in a large population of patients with T2DM, representative of 85% of the diabetic patients in the region with a maximum follow-up of 6 years. We accurately measured important risk factors within a standardized care system and at yearly time intervals. We used the EURODIAB grading system to assess DR, a grading system recommended for large epidemiologic studies (14). However, a limitation of our study is the use of one combined grade for EURODIAB grades 4 and 5; thus, no distinction can be made between progression to proliferative DR (PDR) or treatment of DR with photocoagulation. Furthermore, because the EURODIAB was not designed to assess maculopathy, this study does not provide details on different causes of progression. Nonetheless, to obtain an impression of clinically relevant progression of DR, the use of the EURODIAB grading with 4/5 combined without more detailed grading seems to be sufficient.
The current study was performed in a diabetic population of mainly Caucasian origin, with a mean age of 61.0 years. Therefore, these results may not be representative of a younger or non-Caucasian population. Furthermore, the study population consisted of patients with T2DM with a variety of diabetic duration and relatively well treated hyperglycemia. However, the prevalence of an HbA1c >8.0% at some point between T0 and T6 was 47%, and the prevalence of an HbA1c >10.0% was 17%. Nonetheless, less heterogeneous clusters or different clusters of developmental patterns might be found if analyses would be repeated in different populations, e.g., with type 1 diabetes or new-onset T2DM, with a longer follow-up than the time frame of 6 years in our study or with higher levels of blood glucose.
Several important longitudinal studies, which have studied risk factors influencing the onset or the progression of DR, differ from the current study. First, the aim of these studies was to describe the associations of onset or progression of DR with risk factors, but none of these studies were designed to study the developmental pattern of DR based on yearly measurements. Second, some of these studies used more than two follow-up measures (10,17), but most had only retinopathy data on baseline and one follow-up measurement (11,18), and thus the outcome was incidence of new-onset DR or incidence of a certain degree of progression of DR. This hampers a sound analysis of progression and regression, because the possibility of regression of DR was not taken in account. We show that regression does occur in a small subgroup of patients, cluster B. Although small, this cluster is the second largest cluster after cluster A with “persistent no retinopathy.” Previous cross-sectional studies on DR prevalence have also shown that most diabetic patients have no DR or mild background DR. We also found that the majority of diabetic patients (88.9%) do not develop DR in a 6-year period. This might have consequences for advice on differential possible screening intervals in selected patients.
In the current study, clusters with progressive or stable high levels of DR have high levels of some risk factors compared with nonprogressive clusters. These results are in line with the aforementioned cohort studies, such as the UK Prospective Diabetes Study, EURODIAB, and Wisconsin Epidemiological Study of Diabetic Retinopathy, which showed associations of incidence and progression of DR among others with HbA1c, blood pressure, and diabetic duration. The steep increases of systolic blood pressure in the progressive clusters, coinciding with the time at which retinopathy progressed, suggest that progression of DR is influenced to a large extent by blood pressure and diabetes duration. Nonetheless, these clusters also have high levels of blood glucose and other risk factors. Thus, future research should focus on the influence of risk factors on both progression and regression of DR.
In summary, we have described five clusters of distinct developmental patterns of DR that enable a more detailed examination of the influence of various risk factors on the course of retinopathy. The majority of patients with T2DM in this population did not or only minimally developed retinopathy over a period of 6 years. These patients showed lower risk factor levels of diabetic duration, HbA1c, FPG, and systolic blood pressure compared with patients in the two other small clusters of diabetic patients who showed progression of DR. Patients in these two progressive clusters are at high risk of persistent PDR and are therefore in need of strict and regular screening. Further research is needed to investigate how to distinguish patients in progressive developmental clusters from patients with no or minimal background DR.
Supplementary Material
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
H.Z. researched data, wrote the article, contributed to discussion, and reviewed and edited the article. T.H. researched data, contributed to discussion, and reviewed and edited the article. M.A., L.M.C.W., G.N., A.C.M., H.C.W.V., B.C.P.P., and J.M.D. contributed to discussion and reviewed and edited the article.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc10-1741/-/DC1.
See accompanying editorial, p. 1066.
References
- 1.Kempen JH, O’Colmain BJ, Leske MC, et al. Eye Diseases Prevalence Research Group The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol 2004;122:552–563 [DOI] [PubMed] [Google Scholar]
- 2.Stratton IM, Cull CA, Adler AI, Matthews DR, Neil HA, Holman RR. Additive effects of glycaemia and blood pressure exposure on risk of complications in type 2 diabetes: a prospective observational study (UKPDS 75). Diabetologia 2006;49:1761–1769 [DOI] [PubMed] [Google Scholar]
- 3.The Diabetic Retinopathy Study Research Group Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. Ophthalmology 1981;88:583–600 [PubMed] [Google Scholar]
- 4.Rodbard HW, Blonde L, Braithwaite SS, et al. AACE Diabetes Mellitus Clinical Practice Guidelines Task Force American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract 2007;13(Suppl. 1):1–68 [DOI] [PubMed] [Google Scholar]
- 5.Wong TY, Mwamburi M, Klein R, et al. Rates of progression in diabetic retinopathy during different time periods: a systematic review and meta-analysis. Diabetes Care 2009;32:2307–2313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sjølie AK, Klein R, Porta M, et al. DIRECT Programme Study Group Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet 2008;372:1385–1393 [DOI] [PubMed] [Google Scholar]
- 7.Unwin N, Gan D, Whiting D. The IDF Diabetes Atlas: providing evidence, raising awareness and promoting action. Diabetes Res Clin Pract 2010;87:2–3 [DOI] [PubMed] [Google Scholar]
- 8.Jönsson B, CODE-2 Advisory Board Revealing the cost of type II diabetes in Europe. Diabetologia 2002;45:S5–S12 [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596–615 [DOI] [PubMed] [Google Scholar]
- 10.Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology 1998;105:1801–1815 [DOI] [PubMed] [Google Scholar]
- 11.Stratton IM, Kohner EM, Aldington SJ, et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia 2001;44:156–163 [DOI] [PubMed] [Google Scholar]
- 12.van Leiden HA, Dekker JM, Moll AC, et al. Risk factors for incident retinopathy in a diabetic and nondiabetic population: the Hoorn study. Arch Ophthalmol 2003;121:245–251 [DOI] [PubMed] [Google Scholar]
- 13.Welschen LM, van Oppen P, Dekker JM, Bouter LM, Stalman WA, Nijpels G. The effectiveness of adding cognitive behavioural therapy aimed at changing lifestyle to managed diabetes care for patients with type 2 diabetes: design of a randomised controlled trial. BMC Public Health 2007;7:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aldington SJ, Kohner EM, Meuer S, Klein R, Sjølie AK. Methodology for retinal photography and assessment of diabetic retinopathy: the EURODIAB IDDM complications study. Diabetologia 1995;38:437–444 [DOI] [PubMed] [Google Scholar]
- 15.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass 2008;2:302–317 [Google Scholar]
- 16.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res 2000;24:882–891 [PubMed] [Google Scholar]
- 17.Younis N, Broadbent DM, Vora JP, Harding SP, Liverpool Diabetic Eye Study Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the Liverpool Diabetic Eye Study: a cohort study. Lancet 2003;361:195–200 [DOI] [PubMed] [Google Scholar]
- 18.Porta M, Sjoelie AK, Chaturvedi N, et al. EURODIAB Prospective Complications Study Group Risk factors for progression to proliferative diabetic retinopathy in the EURODIAB Prospective Complications Study. Diabetologia 2001;44:2203–2209 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.