Abstract
OBJECTIVE
Ethnic minorities with diabetes typically have lower rates of cardiovascular outcomes and higher rates of end-stage renal disease (ESRD) compared with whites. Diabetes outcomes among Asian and Pacific Islander subgroups have not been disaggregated.
RESEARCH DESIGN AND METHODS
We performed a prospective cohort study (1996–2006) of patients enrolled in the Kaiser Permanente Northern California Diabetes Registry. There were 64,211 diabetic patients, including whites (n = 40,286), blacks (n = 8,668), Latinos (n = 7,763), Filipinos (n = 3,572), Chinese (n = 1,823), Japanese (n = 951), Pacific Islanders (n = 593), and South Asians (n = 555), enrolled in the registry. We calculated incidence rates (means ± SD; 7.2 ± 3.3 years follow-up) and created Cox proportional hazards models adjusted for age, educational attainment, English proficiency, neighborhood deprivation, BMI, smoking, alcohol use, exercise, medication adherence, type and duration of diabetes, HbA1c, hypertension, estimated glomerular filtration rate, albuminuria, and LDL cholesterol. Incidence of myocardial infarction (MI), congestive heart failure, stroke, ESRD, and lower-extremity amputation (LEA) were age and sex adjusted.
RESULTS
Pacific Islander women had the highest incidence of MI, whereas other ethnicities had significantly lower rates of MI than whites. Most nonwhite groups had higher rates of ESRD than whites. Asians had ~60% lower incidence of LEA compared with whites, African Americans, or Pacific Islanders. Incidence rates in Chinese, Japanese, and Filipinos were similar for most complications. For the three macrovascular complications, Pacific Islanders and South Asians had rates similar to whites.
CONCLUSIONS
Incidence of complications varied dramatically among the Asian subgroups and highlights the value of a more nuanced ethnic stratification for public health surveillance and etiologic research.
Individuals of Asian origin comprise ~4.7% of the U.S. population (1), and people from the Pacific Islands comprise another 0.3% of the population (2). It has been estimated that by the year 2050, 10% of the U.S. population will be of Asian or Pacific Islander ancestry (3). Yet, there is little systematic data collection on Asian Americans and Pacific Islanders and almost no long-term outcome studies among these ethnic groups by country of origin.
Both Asians (4,5) and Pacific Islanders (6) have been recognized as having higher rates of type 2 diabetes than whites and other ethnic minority groups in the U.S. (3). Explanations for this higher diabetes prevalence have included cultural, socioeconomic, behavioral, and genetic factors (4,5). However, among those with diabetes, it is unclear whether Asians and Pacific Islanders have similar incidence of complications relative to whites or other ethnic groups. In previous diabetes research, data for Asians and Pacific Islanders was aggregated, and this heterogeneous group had a significantly lower incidence of cardiovascular disease outcomes and lower-extremity amputations (LEAs) and higher end-stage renal disease (ESRD) rates over 2 years of follow-up compared with whites (7). However, the insufficient numbers of individuals in each ethnic category and short follow-up time precluded examination of specific subgroups.
We disaggregated data from East Asians, South Asians, Filipinos, and Pacific Islanders from a large, diverse cohort of diabetic patients enrolled in the Kaiser Permanente managed care organization in northern California and determined the incidence of major diabetes complications after ~7 ± 3 years of follow-up or 413,500 person-years. We compared the risk of each complication in four separate Asian groups and Pacific Islanders with that in whites, African Americans, and Latinos after adjusting for several potential explanatory factors. We hypothesized that the incidence of complications will differ significantly between each specific Asian and Pacific Islander subgroup compared with whites, and aggregation of all Asians together obscures this variation.
RESEARCH DESIGN AND METHODS
The study sampling frame was derived from a well-characterized population with diabetes in the Kaiser Permanente Northern California Diabetes Registry (n = ~225,000) (7). Kaiser Permanente Northern California is a fully integrated health care delivery system that provides comprehensive medical care to >3 million members (30% of the catchment area). Except for the extremes of income, the demographic characteristics of the patient population are similar to those of the overall population of the region.
During 1994–1997, all noninstitutionalized Diabetes Registry members aged >19 years were mailed a questionnaire or contacted for a computer-assisted telephone interview in English, Spanish, Mandarin, or Cantonese (n = 95,953). After excluding those who denied having diabetes and those who had left the health plan, there were 81,286 eligible individuals for survey administration. Of these, 69,722 (86%) completed the survey. We excluded another 5,511 people with unknown race/ethnicity, mixed racial/ethnic background, or those belonging to racial/ethnic groups with insufficient size for analysis (e.g., Vietnamese, Koreans, and Indonesians), leaving a total study population of 64,211 individuals. In our analyses, we present each racial/ethnic group separately and also aggregate the four Asian groups (Chinese, Filipino, Japanese, and South Asian) together to address our hypothesis.
Measures
Race/ethnicity of the respondents was based on self-report. Socioeconomic status was captured by self-reported educational attainment. Neighborhood deprivation index was calculated using the 1990 U.S. Census with a validated methodology. Limited English proficiency, categorized as always or often having problems speaking and/or understanding English, was categorized using administrative records. Behavioral variables included current smoking status and alcohol use and whether the subject reported using exercise to treat their diabetes at the time of the survey. BMI was calculated based on self-reported height and weight at the time of the survey. We calculated multi-interval, continuous-medication gaps, a well-validated metric of medication adherence (percentage of time without sufficient medications) based on pharmacy utilization for oral glucose-lowering medication.
We determined type and duration of diabetes and family history of diabetes. We assessed a history of hypertension using a self-reported measure and pharmacy records for antihypertensive drug use. HbA1c levels, LDL cholesterol, HDL cholesterol, triglycerides, microalbuminuria, and estimated glomerular filtration rate (eGFR) were ascertained from Kaiser’s regional laboratory within 1 year of baseline individual survey date.
Outcome measures
We evaluated the incidence of five diabetes complications: myocardial infarction (MI), congestive heart failure (CHF), stroke (ischemic or hemorrhagic), ESRD, and nontraumatic LEA over 7 ± 3 years of follow-up. The ICD-9-CM codes listed as either the primary hospitalization discharge diagnosis or the ICD-10-CM code for underlying cause of death on the death certificate were used to identify MI, CHF, and stroke (Supplementary Data). ESRD was identified from Kaiser Permanente’s ESRD treatment registry or defined by chronic renal failure listed as the underlying cause of death on the death certificate. The LEA procedures were identified from discharge codes and/or current procedural terminology codes. Emergency events serviced by non–Kaiser Permanente hospitals were captured via a claims reimbursement database for outside medical services. Mortality and cause of death were ascertained with a validated program, the California Automated Mortality Linkage System. We have previously reported validation studies of these end points in this population (7).
Statistical analyses
We used a direct adjustment method, with the whole diabetic cohort as the standard population to determine age- and sex-adjusted incidence densities for each outcome by race. The incidence densities are presented as the number of events per 1,000 person-years with 95% CIs. We calculated age- and sex-adjusted rates and fully adjusted rate ratios comparing each ethnic group to whites using Poisson regression for those with complete data.
Cox proportional hazards models were specified to calculate adjusted hazard ratios (HRs) for each ethnic minority group versus the reference category (whites). We excluded individuals with a prevalent history of the same diagnosis for each of the outcomes analyzed, focusing only on incident events. We pooled the data for men and women because the interaction between ethnicity and sex was not significant for all outcomes except for MI. We specified a series of Cox regression models in sequence to assess potentially explanatory variables after verifying that there were no violations of the proportionality assumption. First, we created a base model that was adjusted for sex and age (demographic model). Then, we added socioeconomic factors (education, English-language proficiency, and neighborhood deprivation score) for the second model (SES model). The third model added BMI. A fourth model (behavior model) added smoking status, alcohol intake, self-reported use of exercise as a treatment for diabetes, and medication adherence for oral diabetes medications. The fifth and final model (clinical model) added characteristics specific to diabetes to the behavior model, including type of diabetes, diabetes duration, hypertension history, baseline HbA1c (<7, 7–8, 8–10, and >10%), LDL cholesterol (<100 vs. ≥100 mg/dL), elevated urinary albumin excretion (microalbuminuria or proteinuria vs. normoalbuminuria), and chronic kidney disease stages based on standard cut points for eGFR.
Not all study participants answered all the relevant survey questions. Moreover, in the beginning of the study (1996), the clinical assessments (LDL cholesterol, HbA1c, and others) were not collected as frequently or routinely as is common today. Because the analyses were restricted to complete cases, which can introduce bias if the data are not missing completely at random, we used a multiple-imputation method to replace the missing variables of our study. We used the Markov Chain Monte Carlo method (8), which assumes multivariate normality to impute all missing values to make 10 complete datasets, as implemented in SAS Proc MI. After the 10 complete datasets were analyzed using standard SAS procedures (Proc TPHREG), the MIANALYZE procedure was used to generate valid statistical inferences by combining results from the 10 analyses. In addition, we performed a sensitivity analysis using observations for which no data were missing.
RESULTS
Of 64,211 diabetic patients, ~63% were white, 13% were African American, 12% were Latino, 6% were Filipino, 3% were Chinese, 1% were Japanese, 1% were Pacific Islanders, and 1% were South Asians. There were a total of 6,901 (11%) Asian participants in aggregate and an additional 593 (1%) Pacific Islanders included in this analysis. The total follow-up time was ~413,500 person-years or a mean of 7.2 ± 3.3 years from 1996 to 2006.
Each of the eight ethnic groups were ~50% women, except for the Chinese (42% women) and South Asian (30% women) groups (Table 1). Mean age differed somewhat by ethnicity, with Japanese respondents being oldest (aged 62 ± 11 years) and South Asians being the youngest (aged 53 ± 11 years). College graduation rates were highest among South Asians (55%), Filipino (47%), Chinese (37%), and Japanese (33%) and lowest among Pacific Islanders (14%) and Latinos (12%). There were high proportions of African Americans (47%) and Latinos (31%) living in the most deprived neighborhoods. Chinese Americans (33%) were most likely to have limited English proficiency. The average BMI was similar for whites, African Americans, Latinos, and Pacific Islanders (~30 ± 6 kg/m2 for each) and lower for the other four Asian subgroups (mean 25–26 kg/m2 per group). The prevalence of smoking was highest among African Americans (16%) and Pacific Islanders (14%) and lowest among the Chinese and South Asian (≤5%) groups. The mean duration of diagnosed diabetes was similar for whites, African Americans, Latinos, and Japanese (10 ± 10 years for each group) but lower for Chinese (9 ± 11 years), Filipinos (8 ± 8 years), Pacific Islanders (8 ± 9 years), and South Asians (8 ± 7 years). More than half of all participants in each ethnic group were using oral hypoglycemic medications for diabetes treatment, had a family history of diabetes, and had hypertension.
Table 1.
Baseline characteristics of 64,211 participants with diabetes by race/ethnic group*
| Characteristics | White | African American | Latino | Filipino | Chinese | Japanese | South Asian | Pacific Islander |
|---|---|---|---|---|---|---|---|---|
| n | 40,286 | 8,668 | 7,763 | 3,572 | 1,823 | 951 | 555 | 593 |
| Follow-up time (mean ± SD) | 7.0 ± 8.9 | 7.3 ± 3.2 | 7.5 ± 3.2 | 7.5 ± 3.2 | 7.8 ± 3.1 | 8.0 ± 3.3 | 7.4 ± 3.3 | 7.0 ± 3.3 |
| Female sex | 45 | 53 | 49 | 51 | 42 | 52 | 30 | 44 |
| Age (years) (mean ± SD) | 61 ± 13 | 59 ± 12 | 58 ± 12 | 56 ± 11 | 60 ± 12 | 63 ± 11 | 53 ± 11 | 54 ± 10 |
| Education achieved | ||||||||
| <High school | 13 | 17 | 36 | 13 | 19 | 9 | 13 | 26 |
| High school graduate/GED | 30 | 26 | 28 | 15 | 20 | 30 | 14 | 33 |
| Some college | 32 | 38 | 24 | 25 | 24 | 29 | 18 | 27 |
| College graduate or higher | 25 | 18 | 12 | 47 | 37 | 33 | 55 | 14 |
| Neighborhood deprivation index | ||||||||
| Fourth quartile (poorest) | 11.6 | 47.4 | 31.0 | 19.5 | 13.2 | 12.0 | 12.8 | 21.8 |
| Limited English proficiency | ||||||||
| No English spoken | 0.7 | 0.1 | 13.9 | 8.2 | 33.5 | 5.8 | 9.5 | 6.8 |
| BMI (kg/m2) | ||||||||
| Underweight (<19.0) | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 |
| Normal (19.0–24.9) | 21 | 14 | 16 | 21 | 27 | 19 | 28 | 22 |
| Overweight (25.0–29.9) | 36 | 36 | 39 | 23 | 23 | 21 | 21 | 37 |
| Obese (≥30.0) | 43 | 48 | 45 | 55 | 48 | 59 | 50 | 40 |
| Current smoker (%) | 12 | 16 | 11 | 9 | 4 | 9 | 5 | 14 |
| Alcohol (drinks/week) | ||||||||
| Moderate use (7–19) | 7 | 4 | 5 | 2 | 2 | 2 | 7 | 4 |
| Heavy use (≥20) | 2 | 1 | 2 | 0 | 0 | 1 | 1 | 1 |
| Uses exercise as part of treatment | 48 | 50 | 47 | 59 | 47 | 52 | 52 | 57 |
| Diabetes type | ||||||||
| Type 1 | 7 | 4 | 3 | 1 | 2 | 1 | 5 | 3 |
| Type 2, using insulin | 20 | 26 | 20 | 12 | 13 | 17 | 13 | 19 |
| Type 2, oral hypoglycemic | 51 | 54 | 56 | 66 | 47 | 58 | 62 | 60 |
| Type 2, diet controlled | 22 | 16 | 21 | 20 | 27 | 23 | 20 | 18 |
| First-degree family history of diabetes | 51 | 65 | 72 | 59 | 53 | 57 | 69 | 72 |
| Diabetes duration (years) | ||||||||
| 0–9 | 61 | 61 | 62 | 72 | 65 | 62 | 69 | 69 |
| 10–19 | 24 | 25 | 25 | 20 | 22 | 22 | 34 | 21 |
| ≥20 | 16 | 14 | 13 | 8 | 12 | 16 | 8 | 10 |
| HbA1c category (%) | ||||||||
| <7 | 28 | 25 | 23 | 18 | 28 | 25 | 20 | 16 |
| 7–8 | 24 | 20 | 19 | 21 | 23 | 26 | 25 | 17 |
| 8–10 | 30 | 28 | 31 | 33 | 31 | 33 | 34 | 32 |
| ≥10 | 18 | 27 | 27 | 28 | 18 | 16 | 21 | 35 |
| Self-monitored blood glucose per guidelines | 46 | 34 | 38 | 33 | 34 | 42 | 38 | 29 |
| History of hypertension | 68 | 72 | 56 | 61 | 63 | 65 | 47 | 62 |
| HDL <45 mg/dL for women or <35 mg/dL for men | 63 | 43 | 62 | 56 | 50 | 54 | 58 | 62 |
| LDL ≥100 mg/dL | 87 | 89 | 87 | 91 | 86 | 89 | 89 | 91 |
| Triglycerides ≥200 mg/dL | 46 | 20 | 46 | 38 | 38 | 47 | 37 | 43 |
| Taking a cholesterol-lowering medication | 14 | 10 | 10 | 15 | 14 | 21 | 11 | 15 |
| Microalbuminuria | 14 | 15 | 14 | 17 | 15 | 18 | 10 | 17 |
| eGFR (mL/min) | ||||||||
| ≥90 | 16 | 29 | 29 | 26 | 22 | 22 | 27 | 24 |
| 60–89 | 53 | 49 | 50 | 51 | 54 | 55 | 60 | 50 |
| 30–59 | 28 | 17 | 17 | 19 | 20 | 19 | 11 | 19 |
| 15–29 | 2 | 3 | 2 | 2 | 3 | 3 | 1 | 3 |
| <15 | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 5 |
*Values represent % unless otherwise stated.
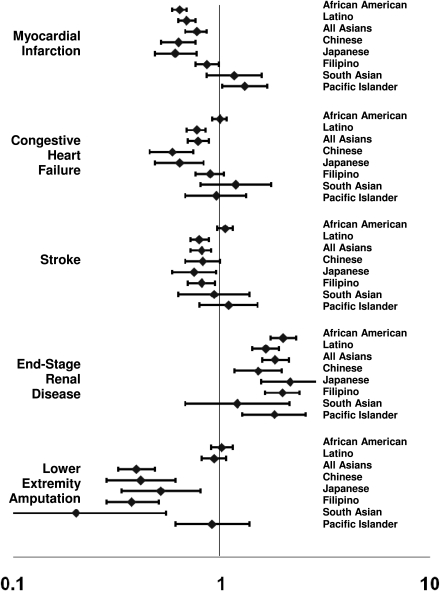
We calculated the crude and age- and sex-adjusted incidence rates per ethnic group for each of the five diabetes complications (Table 2). We also show the aggregated rates of the four Asian subgroups together for comparison with the individual Asian subgroups. The fully adjusted rate ratios comparing each ethnic group to whites are displayed. The table shows the HR (95% CI) for each ethnic group compared with whites for each of the diabetes complications.
Table 2.
Crude age- and sex-adjusted incidence rates and fully adjusted rate ratios* of each outcome by racial subgroup, DISTANCE study, 1996–2006
| Outcomes | White | African American | Latino | All Asians | Filipino | Chinese | Japanese | South Asian | Pacific Islander |
|---|---|---|---|---|---|---|---|---|---|
| MI: n/N | 4,276/36,185 | 658/8,131 | 559/7,257 | 529/6,550 | 287/3,399 | 124/1,743 | 74/899 | 44/509 | 66/537 |
| Total person-years of follow-up | 249,426 | 58,336 | 53,160 | 49,010 | 24,956 | 13,460 | 7,031 | 3,563 | 3,572 |
| Unadjusted rate (95% CI) | 17.1 (16.6–17.7) | 11.3 (10.4–12.2) | 10.5 (9.7–11.4) | 10.8 (9.9–11.8) | 11.5 (10.2–12.9) | 9.2 (7.7–11.0) | 10.5 (8.3–13.2) | 12.3 (9.0–16.6) | 18.5 (14.3–23.5) |
| Age- and sex-adjusted rate (95% CI) | 5.9 (5.7–6.2) | 4.3 (3.9–4.8) | 4.2 (3.8–4.7) | 4.1 (3.7–4.6) | 4.7 (4.0–5.4) | 3.6 (2.6–4.8) | 3.3 (2.3–4.4) | 5.9 (3.3–9.1) | 10.1 (6.8–14.0) |
| Fully adjusted rate ratio (95% CI) | 1.0 (reference) | 0.66 (0.47–0.91) | 0.63 (0.43–0.91) | 0.58 (0.40–0.85) | 0.40 (0.21–0.77) | 0.41 (0.18–0.93) | 0.67 (0.34–1.31) | 1.99 (0.97–4.09) | 1.05 (0.39–2.84) |
| CHF: n/N | 3,400/36,995 | 794/8,021 | 478/7,420 | 355/6,602 | 193/3,415 | 81/1,744 | 55/908 | 26/535 | 35/547 |
| Total person-years of follow-up | 261,568 | 57,636 | 55,154 | 50,407 | 25,624 | 13,662 | 7,243 | 3,878 | 3,804 |
| Unadjusted rate (95% CI) | 13.0 (12.6–13.4) | 13.8 (12.8–14.8) | 8.7 (7.9–9.5) | 7.0 (6.3–7.8) | 7.5 (6.5–8.7) | 5.9 (4.7–7.4) | 7.6 (5.7–9.9) | 6.7 (4.4–9.8) | 9.2 (6.4–12.8) |
| Age- and sex-adjusted rate (95% CI) | 4.2 (4.1–4.4) | 5.2 (4.7–5.8) | 3.5 (3.1–4.0) | 2.8 (2.4–3.3) | 3.5 (2.9–4.2) | 2.5 (1.0–4.3) | 2.6 (1.7–3.6) | 4.4 (0.9–9.2) | 4.0 (2.4–5.9) |
| Fully adjusted rate ratio (95% CI) | 1.0 (reference) | 1.24 (0.92–1.68) | 0.64 (0.42–0.99) | 0.80 (0.53–1.21) | 0.79 (0.43–1.46) | 0.74 (0.35–1.56) | 0.55 (0.22–1.33) | 2.29 (0.92–5.65) | 0.73 (0.18–2.96) |
| Stroke: n/N | 3,212/38,376 | 713/8,325 | 445/7,531 | 417/6,668 | 194/3,455 | 130/1,757 | 67/913 | 26/543 | 38/579 |
| Total person-years of follow-up | 266,344 | 59,168 | 55,446 | 50,324 | 25,710 | 13,527 | 7,134 | 3,953 | 3,961 |
| Unadjusted rate (95% CI) | 12.1 (11.6–12.5) | 12.1 (11.2–13.0) | 8.0 (7.3–8.8) | 8.3 (7.5–9.1) | 7.5 (6.5–8.7) | 9.6 (8.0–11.4) | 9.4 (7.3–11.9) | 6.6 (4.3–9.6) | 9.6 (6.8–13.2) |
| Age- and sex-adjusted rate (95% CI) | 3.9 (3.6–4.1) | 5.0 (4.2–5.8) | 3.1 (2.8–3.6) | 3.1 (2.7–3.6) | 3.2 (2.6–3.9) | 3.2 (2.5–4.0) | 2.8 (1.7–4.3) | 3.4 (1.5–5.8) | 5.2 (2.8–8.3) |
| Fully adjusted rate ratio (95% CI) | 1.0 (reference) | 0.73 (0.50–1.06) | 0.59 (0.39–0.90) | 0.58 (0.38–0.87) | 0.65 (0.37–1.14) | 0.28 (0.11–0.70) | 0.85 (0.45–1.61) | 0.52 (0.13–2.10) | 0.53 (0.13–2.14) |
| ESRD: n/N | 1,080/39,898 | 528/8,519 | 356/7,648 | 337/6,797 | 188/3,512 | 79/1,801 | 57/937 | 13/547 | 39/576 |
| Total person-years of follow-up | 279,802 | 61,040 | 56,507 | 51,465 | 26,128 | 13,932 | 7,379 | 4,025 | 3,955 |
| Unadjusted rate (95% CI) | 3.9 (3.6–4.1) | 8.7 (7.9–9.4) | 6.3 (5.7–7.0) | 6.5 (5.9–7.3) | 7.2 (6.2–8.3) | 5.7 (4.5–7.1) | 7.7 (5.9–10.0) | 3.2 (1.7–5.5) | 9.9 (7.0–13.5) |
| Age- and sex-adjusted rate (95% CI) | 2.4 (2.1–2.8) | 4.8 (3.5–6.1) | 3.0 (2.4–3.7) | 2.9 (2.0–4.0) | 3.9 (2.3–5.7) | 1.9 (1.4–2.5) | 3.0 (1.6–4.6) | 1.1 (0.5–2.1) | 5.0 (2.7–7.8) |
| Fully adjusted rate ratio (95% CI) | 1.0 (reference) | 3.37 (2.09–5.43) | 1.30 (0.65–2.59) | 1.77 (0.98–3.21) | 2.09 (0.93–4.67) | 1.47 (0.51–4.23) | 2.09 (0.81–5.40) | 0.0 | 0.0 |
| LEA: n/N | 1,477/39,659 | 390/8,503 | 293/7,656 | 107/6,872 | 53/3,561 | 29/1,812 | 21/946 | 4/553 | 24/589 |
| Total person-years of follow-up | 277,454 | 61,304 | 56,698 | 52,526 | 26,793 | 14,105 | 7,547 | 4,081 | 4,058 |
| Unadjusted rate (95% CI) | 5.3 (5.1–5.6) | 6.4 (5.7–7.0) | 5.2 (4.6–5.8) | 2.0 (1.7–2.5) | 2.0 (1.5–2.6) | 2.1 (1.4–3.0) | 2.8 (1.7–4.3) | 1.0 (0.3–2.5) | 5.9 (3.8–8.8) |
| Age- and sex-adjusted rate (95% CI) | 2.4 (2.1–2.6) | 2.6 (2.2–3.1) | 2.1 (1.8–2.5) | 0.9 (0.5–1.2) | 0.7 (0.5–1.0) | 0.7 (0.3–1.1) | 1.3 (0.5–2.4) | 1.0 (−0.1 to 3.5) | 2.6 (1.5–4.0) |
| Fully adjusted rate ratio (95% CI) | 1.0 (reference) | 0.75 (0.40–1.40) | 1.17 (0.65–2.10) | 0.29 (0.12–0.69) | 0.34 (0.10–1.14) | 0.18 (0.02–1.31) | 0.26 (0.04–1.90) | 0.38 (0.05–3.11) | 0.0 |
*Fully adjusted rate ratio comparing the rate in each ethnic group with that of whites using a Poisson regression model.
There were a total of 6,088 people with incident MI during the follow-up period. The aggregated Asian incidence rate (10.8 [95% CI 9.9–11.8]) completely obscured the wide range of rates across the four Asian subgroups. The highest incidence of MI occurred in Pacific Islanders (18.5 [14.3–23.5] per 1,000 person-years), and the lowest incidence was in Chinese (9.2 [7.7–11.0] per 1,000 person-years). After age and sex adjustment, the rates were attenuated, but Pacific Islanders had the highest incidence of MI (10.1 per 1,000 person-years) of all groups, whereas Japanese (3.3 per 1,000 person-years) had the lowest incidence of MI, with whites in the middle of this range (5.9 per 1,000 person-years). These differences between subgroups persisted despite multivariate adjustment for several potentially explanatory factors (Fig. 1). In fully adjusted models, compared with whites, most racial/ethnic groups had significantly lower hazards of MI. However, Pacific Islanders had significantly higher risk (HR 1.29 [1.01–1.66]), and South Asians were not significantly different from whites. Furthermore, sex did not modify the association between ethnicity and MI risk, except for Pacific Islanders where women had a markedly higher risk (1.94 [1.40–2.68]) than men (0.87 [0.59–1.27]; P for interaction = 0.001).
Figure 1.
HRs and 95% CIs for each ethnic group (vs. whites [reference group]) for each diabetes complication.
The total number of first-time diagnoses for CHF was 5,062 during follow-up. The highest age- and sex-adjusted incidence was among African Americans (5.2 per 1,000 person-years), and the lowest incidence was among Chinese (2.5 per 1,000 person-years). The range of CHF incidence rates among the four Asian groups was narrower for CHF than for MI (from 2.4 to 3.3). In fully adjusted models, there was no significant difference between African Americans, Filipinos, Pacific Islanders, and South Asians compared with whites. The risk of CHF was significantly lower for Latinos, Japanese, and Chinese compared with whites.
There were 4,825 strokes during follow-up. Similar to CHF, the age- and sex-adjusted incidence was highest among African Americans, and the lowest rates occurred among Japanese (2.8 per 1,000 person-years). The fully adjusted comparison with whites showed a similar pattern as CHF, with Latinos, Japanese, Chinese, and Filipinos having significantly lower risk than whites and the other ethnic groups having similar risk to whites.
There were 2,340 new cases of ESRD. The adjusted incidence of ESRD was not uniformly higher for all ethnic minority groups compared with whites; the incidence was lower among South Asians (1.1 per 1,000 person-years) and Chinese (1.9 per 1,000 person-years) compared with whites (2.4 per 1,000 person-years) and higher among all of the other groups. Aggregating all four Asian groups together (2.9 per person-year [95% CI 2.0–4.0]) obscured the wide range of ESRD outcomes among each of the subgroups. However, after adjusting for all potentially explanatory groups of variables, the hazards of ESRD were significantly higher for each ethnic group compared with whites, except for South Asians for whom the ESRD risk was similar to whites.
There were a total of 2,291 first-time cases of LEA. The highest age- and sex-adjusted incidence was among African Americans and Pacific Islanders (2.6 per 1,000 person-years for each), and the lowest rates were among Chinese and Filipinos (0.7 per 1,000 person-years for each). Compared with whites, all four Asian subgroups had significantly lower risk of LEAs, whereas risk for Pacific Islanders, African Americans, and Latinos was not significantly different than that in whites.
Restricting our Cox models to those with complete data on all covariates, we found some change in risk estimates among the ethnic groups with smaller numbers of patients (Pacific Islanders and South Asians), mainly for the macrovascular disease outcomes. For MI, the risk among Pacific Islanders compared with whites was attenuated (HR 1.03 [95% CI 0.38–2.81]), and the risk became somewhat stronger among South Asians (2.00 [0.97–4.12]). For CHF, the risk was strengthened among South Asians (2.26 [0.91–5.60]). Estimates for stroke, ESRD, and LEAs did not change substantively.
CONCLUSIONS
In a large, integrated, managed care organization, where participants have uniform access to health care, we found that Asians and Pacific Islanders have substantial variation in the incidence of diabetes complications that differs significantly from whites or other ethnic minority groups. The difference in diabetes complications among the ethnic groups was not fully explained by demographic, socioeconomic, behavioral, and disease-related clinical measures. Although most ethnic minority groups with diabetes have significantly lower risk of MI compared with whites, women from the Pacific Islands have almost twice the risk of MI compared with white women. The four Asian subgroups had ~60–70% lower risk of LEAs compared with whites or other ethnic groups. For most complications, the incidence rates observed in Chinese and Japanese were similar to each other. For the three cardiovascular disease outcomes, Pacific Islanders and South Asians had incidence similar to whites, with the exception that Pacific Islander women had substantively higher MI risk. Outcomes in Filipinos were intermediate to those in the other Asian groups.
MI outcomes among diabetic patients of various ethnic groups have been examined in previous studies (9), but most have either not included several different Asian subgroups or have not disaggregated data for their Asian subgroups. Our findings are consistent with a previous report from the Kaiser Diabetes Registry with only 2 years of follow-up that found that all Asians, blacks, and Latinos had significantly lower risk of MI compared with whites after adjustment for several covariates (7). Other U.S. studies have shown higher MI rates among African Americans. Several studies from the U.K. (10–12) have compared diabetic South Asians with white Europeans, finding equal risk of MI complications between these two ethnic groups, consistent with our findings. Singaporian studies have compared heart disease between three separate Asian groups: Chinese, Malay, and Asian Indians and found that the Asian Indians with diabetes had higher heart disease risk than the Chinese or Malay (13). Little outcome data are available for diabetic Pacific Islanders; studies from New Zealand have reported significantly higher rates of cardiovascular risk factors, cardiovascular disease, and mortality compared with Europeans (14). Similarly, native Hawaiian and other Pacific Islanders have very high rates of cardiometabolic disease compared with other U.S. ethnic groups (3,15,16). To our knowledge, this is the first report of significantly higher risk of MI among diabetic Pacific Islander women compared with all ethnic groups. Higher rates of traditional cardiovascular risk factors have been reported among Pacific Islander women (16), which may explain the higher MI risk.
ESRD is a well-recognized microvascular complication of diabetes. Several studies have found that most ethnic minority groups have a higher risk of ESRD compared with whites (9), but there is less known about Asian subgroups. Studies from Europe have reported that South Asians have higher risk of diabetic ESRD than whites in the U.K. (17,18) and in the Netherlands (19), which was not apparent in our analysis possibly as a result of the small numbers of South Asians.
LEAs were significantly less common in the Asian subgroups than all other ethnic groups. Previous studies (20,21) have identified a lower risk of diabetic foot ulcers and amputations among South Asians compared with Europeans, with potential explanations including better preservation of nerve function, peripheral vascular function, low smoking rates, and shorter height (22). Higher rates of diabetic foot–related complications have been reported in indigenous people of western Australia compared with nonindigenous people (23), but that study did not adjust for differences in socioeconomic, behavioral, and disease-related variables.
We were limited in using data collected from a self-administered questionnaire for many covariates and to individuals who could speak English, Spanish, or Chinese languages. Ethnicity was self-reported in narrower categories than most studies but still did not include specific nationality of origin. We did not have information about nativity, generational status, length of time since immigration to the U.S., cultural beliefs, or acculturation to the U.S., which may explain some of the differences in diabetes outcomes. We also did not have data on dietary patterns, stress, secondhand smoke exposure, and other environmental determinants of disease outcomes.
Exercise was assessed by a question asking whether the patient used exercise to treat their diabetes but did not capture intensity or frequency and may underestimate the effect of physical activity as an explanatory factor. BMI was calculated by self-reported weight and height, which may underestimate the effect of adiposity. We did not measure waist circumference, which may be a better indicator of adiposity in Asians (24). Diabetes severity and control were measured at baseline using available laboratory data and self-reported measures. Although all participants in this study population were enrolled in Kaiser Permanente and therefore had access to medical care, we did not have data on the number of primary care visits or other health care utilization measures, which may explain the differences in diabetes outcomes. However, previous studies from this health care setting have shown uniform offering of care by ethnic group (25). Limitations with using diagnostic and procedural codes for classification of our diabetes outcomes have been discussed previously (7). Misclassification of outcomes should not differ by ethnic group and would tend to bias our results toward the null.
In a health care system offering uniform access to care, we found widely disparate rates of diabetes complications among the four Asian groups and Pacific Islanders. This large, diverse cohort allowed comparison of eight racial/ethnic groups, which has not been reported previously. Pacific Islander women were at highest risk of MI compared with all other groups. Similar to whites, Pacific Islanders and South Asians had high rates of all cardiovascular complications. All Asian groups had significantly lower LEA rates than all other groups. Classifying all Asian ethnic groups as a single group greatly obscures the sometimes substantial ethnic differences and may preclude identification of particularly vulnerable subgroups that deserve intensified disease management. Disaggregating Asian and Pacific Islander subgroups is imperative for disease surveillance and may enhance understanding of disease etiology.
Supplementary Material
Acknowledgments
The DISTANCE study was supported and funded by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01-DK-065664 and R01-DK-081796) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01-HD-46113). A.M.K. was supported by National Institutes of Health Grants 1RO1-HL-093009-01 and 1R01-AT-004569-01. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; and preparation, review, or approval of the manuscript.
No potential conflicts of interest relevant to this article were reported.
A.M.K. takes responsibility for the integrity of data and the accuracy of data analysis and the study concept and design, contributed to the analysis and interpretation of data, contributed to the drafting of the manuscript, contributed to the critical revision of the manuscript for important intellectual content, obtained funding, and contributed to the study supervision. N.A. and H.H.M. contributed to the analysis and interpretation of data, and to the critical revision of the manuscript for important intellectual content. J.L. contributed to the acquisition of data, to the analysis and interpretation of data, to the drafting of the manuscript, to the statistical analysis, and to the administrative, technical, or material support. D.S., A.A., and A.T.A. contributed to the critical revision of the manuscript for important intellectual content. A.J.K. takes responsibility for the integrity of data and the accuracy of data analysis and the study concept and design; contributed to the acquisition of data; contributed to the analysis and interpretation of data; contributed to the critical revision of the manuscript for important intellectual content; obtained funding; contributed to the administrative, technical, or material support; and contributed to the study supervision.
Parts of this study were presented in abstract form at the 70th Scientific Sessions of the American Diabetes Association, Orlando, Florida, 25–29 June 2010.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc10-1964/-/DC1.
References
- 1.The Asian population [Internet], 2000. Washington, DC, U.S. Census Bureau. Available from http://www.census.gov/prod/2002pubs/c2kbr01-16.pdf. Accessed 6 June 2010
- 2.The native Hawaiian and other Pacific Islander population [Internet], 2000. Washington, DC, U.S. Census Bureau. Available from http://www.census.gov/prod/2001pubs/c2kbr01-14.pdf. Accessed 6 June 2010
- 3.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the Asian adult population: United States, 2004-2006. Adv Data 2008;(394):1–22 [PubMed] [Google Scholar]
- 4.Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–2140 [DOI] [PubMed] [Google Scholar]
- 5.Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet 2010;375:408–418 [DOI] [PubMed] [Google Scholar]
- 6.Grandinetti A, Kaholokula JK, Theriault AG, Mor JM, Chang HK, Waslien C. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawaii. Ethn Dis 2007;17:250–255 [PubMed] [Google Scholar]
- 7.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA 2002;287:2519–2527 [DOI] [PubMed] [Google Scholar]
- 8.Schafer J. Analysis of Incomplete Multivariate Data. London, Chapman and Hall, 1997 [Google Scholar]
- 9.Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care 2005;28:2280–2288 [DOI] [PubMed] [Google Scholar]
- 10.Chaturvedi N, Jarrett J, Morrish N, Keen H, Fuller JH. Differences in mortality and morbidity in African Caribbean and European people with non-insulin dependent diabetes mellitus: results of 20 year follow up of a London cohort of a multinational study. BMJ 1996;313:848–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.K. Prospective Diabetes Study Group Ethnicity and cardiovascular disease: the incidence of myocardial infarction in white, South Asian, and Afro-Caribbean patients with type 2 diabetes (U.K. Prospective Diabetes Study 32). Diabetes Care 1998;21:1271–1277 [DOI] [PubMed] [Google Scholar]
- 12.Soljak MA, Majeed A, Eliahoo J, Dornhorst A. Ethnic inequalities in the treatment and outcome of diabetes in three English Primary Care Trusts. Int J Equity Health 2007;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeo KK, Tai BC, Heng D, et al. Ethnicity modifies the association between diabetes mellitus and ischaemic heart disease in Chinese, Malays and Asian Indians living in Singapore. Diabetologia 2006; 49:2866–2873 [DOI] [PubMed] [Google Scholar]
- 14.Joshy G, Colonne CK, Dunn P, Simmons D, Lawrenson R. Ethnic disparities in causes of death among diabetes patients in the Waikato region of New Zealand. N Z Med J 2010;123:19–29 [PubMed] [Google Scholar]
- 15.Mau MK, Sinclair K, Saito EP, Baumhofer KN, Kaholokula JK. Cardiometabolic health disparities in native Hawaiians and other Pacific Islanders. Epidemiol Rev 2009;31:113–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bitton A, Zaslavsky AM, Ayanian JZ. Health risks, chronic diseases, and access to care among US Pacific Islanders. J Gen Intern Med 2010;25:435–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burden AC, McNally PG, Feehally J, Walls J. Increased incidence of end-stage renal failure secondary to diabetes mellitus in Asian ethnic groups in the United Kingdom. Diabet Med 1992;9:641–645 [DOI] [PubMed] [Google Scholar]
- 18.Samanta A, Burden AC, Jagger C. A comparison of the clinical features and vascular complications of diabetes between migrant Asians and Caucasians in Leicester, U.K. Diabetes Res Clin Pract 1991;14:205–213 [DOI] [PubMed] [Google Scholar]
- 19.Chandie Shaw PK, Vandenbroucke JP, Tjandra YI, et al. Increased end-stage diabetic nephropathy in Indo-Asian immigrants living in the Netherlands. Diabetologia 2002;45:337–341 [DOI] [PubMed] [Google Scholar]
- 20.Abbott CA, Garrow AP, Carrington AL, Morris J, Van Ross ER, Boulton AJ, North-West Diabetes Foot Care Study Foot ulcer risk is lower in South-Asian and African-Caribbean compared with European diabetic patients in the U.K.: the North-West Diabetes Foot Care Study. Diabetes Care 2005;28:1869–1875 [DOI] [PubMed] [Google Scholar]
- 21.Chaturvedi N, Abbott CA, Whalley A, Widdows P, Leggetter SY, Boulton AJ. Risk of diabetes-related amputation in South Asians vs. Europeans in the UK. Diabet Med 2002;19:99–104 [DOI] [PubMed] [Google Scholar]
- 22.Abbott CA, Chaturvedi N, Malik RA, et al. Explanations for the lower rates of diabetic neuropathy in Indian Asians versus Europeans. Diabetes Care 2010;33:1325–1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norman PE, Schoen DE, Gurr JM, Kolybaba ML. High rates of amputation among Indigenous people in Western Australia. Med J Aust 2010;192:421. [DOI] [PubMed] [Google Scholar]
- 24.Hayashi T, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Visceral adiposity, not abdominal subcutaneous fat area, is associated with an increase in future insulin resistance in Japanese Americans. Diabetes 2008;57:1269–1275 [DOI] [PubMed] [Google Scholar]
- 25.Moffet HH, Adler N, Schillinger D, et al. Cohort Profile: the Diabetes Study of Northern California (DISTANCE): objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol 2009;38:38–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.