Abstract
OBJECTIVE
To evaluate the incidence and relative risk of type 2 diabetes defined by the newly proposed HbA1c diagnostic criteria in groups categorized by different baseline HbA1c levels.
RESEARCH DESIGN AND METHODS
Using data from the European Prospective Investigation of Cancer (EPIC)-Norfolk cohort with repeat HbA1c measurements, we estimated the prevalence of known and previously undiagnosed diabetes at baseline (baseline HbA1c ≥6.5%) and the incidence of diabetes over 3 years. We also examined the incidence and corresponding odds ratios (ORs) by different levels of baseline HbA1c. Incident diabetes was defined clinically (self-report at follow-up, prescribed diabetes medication, or inclusion on a diabetes register) or biochemically (HbA1c ≥6.5% at the second health assessment), or both.
RESULTS
The overall prevalence of diabetes was 4.7%; 41% of prevalent cases were previously undiagnosed. Among 5,735 participants without diabetes at baseline (identified clinically or using HbA1c criteria, or both), 72 developed diabetes over 3 years (1.3% [95% CI 1.0–1.5]), of which 49% were identified using the HbA1c criteria. In 6% of the total population, the baseline HbA1c was 6.0–6.4%; 36% of incident cases arose in this group. The incidence of diabetes in this group was 15 times higher than in those with a baseline HbA1c of <5.0% (OR 15.5 [95% CI 7.2–33.3]).
CONCLUSIONS
The cumulative incidence of diabetes defined using a newly proposed HbA1c threshold in this middle-aged British cohort was 1.3% over 3 years. Targeting interventions to individuals with an HbA1c of 6.0–6.4% might represent a feasible preventive strategy, although complementary population-based preventive strategies are also needed to reduce the growing burden of diabetes.
Type 2 diabetes is a major public health concern worldwide. An estimated 439 million people will have the disease by 2030 (1). It is possible to halve the incidence of type 2 diabetes among individuals at high risk through lifestyle and pharmacologic interventions (2–4). However, it is unlikely that population screening for impaired glucose tolerance using an oral glucose tolerance test (OGTT) is a feasible method of identifying those at high risk in clinical practice (5) because it is time- and resource-consuming and has poor reproducibility (6). If a measure of blood glucose were to be used to define the risk of developing diabetes, then it would seem logical to use the same test for diagnosis and informing treatment decisions (7).
Glycated hemoglobin (HbA1c) is a reliable measure of long-term glycemic exposure (8) that correlates well with the risk of microvascular and macrovascular complications of diabetes (9,10). It does not necessitate fasting or timed blood samples. Previous concerns regarding the standardization of assays have largely been resolved (11). Consequently, the American Diabetes Association (ADA) recently recommended that HbA1c be included as a diagnostic test for diabetes, with a diagnostic threshold of ≥6.5% (12).
To better estimate the burden of the disease and potential benefits of preventive interventions, it is necessary to have accurate data on incidence. Reported estimates of incidence in adult populations have varied considerably, from 2 to 25 per 1,000 person-years (13–16). However, many of the studies were restricted to high-risk populations (13) and defined diabetes using a clinical rather than a biochemical diagnosis (14). Fewer studies have investigated the incidence of diabetes based on longitudinal repeat blood glucose measurements in population-based samples (15,16), and none have examined diabetes incidence using repeated measures of HbA1c.
In this study we estimated the prevalence and incidence of diabetes defined using the newly proposed HbA1c cutoff of 6.5% in a population-based British cohort. To inform the choice of appropriate HbA1c thresholds to identify individuals at high risk to whom preventive interventions might be offered, we used data on longitudinal repeat HbA1c values at baseline and after 3 years of follow-up to examine the incidence and relative risk of clinically diagnosed diabetes and diabetes defined using HbA1c diagnostic criteria in groups defined by different baseline HbA1c values.
RESEARCH DESIGN AND METHODS
Study design and population
The European Prospective Investigation of Cancer (EPIC)-Norfolk is a population-based prospective study that monitors 25,639 men and women aged 40–74 years residing in the Norfolk region, U.K. Details of the study have been described elsewhere (17). In brief, between 1993 and 1997, 77,630 individuals were recruited from general practice to participate in the study, and 25,639 (33%) consented and attended a baseline health assessment.
Participants completed questionnaires about their personal and family history of disease, medication, and lifestyle factors, including smoking habits. They were asked whether a physician had ever told them that they had any of the conditions in a list that included diabetes, heart attack, and stroke. Baseline diabetes status was ascertained by 1) self-report of diabetes medication, 2) diabetes medication brought to the baseline examination, 3) participants indicating modification of their diet in the past year because of diabetes, or 4) participants indicating adherence to a diabetic diet. Anthropometric and blood pressure measurements, as well as nonfasting blood samples were taken at the health assessment.
Because funding for measurement of HbA1c only became available in 1995, about 50% of all participants had information on this measure at baseline. HbA1c was measured on fresh EDTA blood samples using high-performance liquid chromatography (Diamat Automated Glycated Hemoglobin Analyzer; Bio-Rad Laboratories Ltd., Hemel Hemstead, U.K.), which was standardized to the Diabetes Control and Complications Trial (DCCT) assay.
Participants were invited to attend a second health assessment after 3 years (1998–2001), at which identical measurements were taken, and 15,028 participants (59%) attended. General practitioners of participants whose HbA1c test results exceeded ≥7.0% were notified so that they could assume responsibility for confirming diagnosis and arranging treatment. The study was approved by the Norwich District Health Authority Ethics Committee. All participants gave signed informed consent.
Individuals who live the Norfolk area are slightly healthier than those in the general U.K. population, with a standardized mortality ratio of 93 (Office for National Statistics death registration data, 2008). However, EPIC-Norfolk participants are similar to a nationally representative sample regarding anthropometric indices, blood pressure, and serum lipid levels (17).
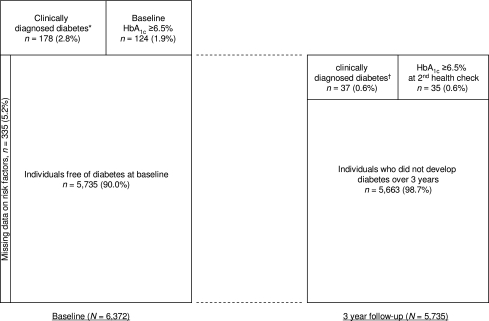
We report results for follow-up at the second health assessment, a median of 3 years. We limited our analyses to the 6,372 individuals with HbA1c measurements at baseline and at the second health assessment. We used this study sample to estimate the prevalence of known (clinically diagnosed diabetes, self-reported physician-diagnosed diabetes, and diabetes medication) and previously undiagnosed diabetes at baseline (baseline HbA1c ≥6.5%). After excluding those with diabetes at baseline (clinically diagnosed diabetes and diabetes defined using HbA1c diagnostic criteria), we further excluded 335 individuals with missing data for other metabolic risk factors, including age, sex, a family history of diabetes, smoking, the use of corticosteroids and antihypertensive drugs, BMI, waist circumference, systolic blood pressure, cholesterol, and triglyceride, leaving 5,735 individuals for analyses of the incidence and risk of diabetes (Fig. 1).
Figure 1.
Schematic diagram demonstrates the numbers and percentages of individuals with prevalent and incidence diabetes in a cohort of 6,372 men and women over 3 years. Individuals with clinically diagnosed diabetes and HbA1c ≥6.5% were considered to have clinically diagnosed diabetes in this diagram. *Self-reported diabetes, evidence of diabetes medications, and dietary modification due to diabetes. †Self-reported diabetes, evidence of diabetes medication, diabetes registers, hospitalizations with diabetes, and diabetes codes on death certificates.
Ascertainment of incident diabetes
Participants were identified as having incident diabetes if 1) they reported physician-diagnosed diabetes or diabetes medication, or brought diabetes medication to the second health assessment (clinical diagnosis), 2) they were identified on medical records, diabetes registers, or death certificates (clinical diagnosis) or 3) they had an HbA1c of ≥6.5% at the second health assessment (HbA1c-defined diabetes). Participants were identified through their general practice diabetes register or the Norfolk and Norwich Hospital diabetes register. Participants admitted to a hospital with a diabetes-related condition were identified by their National Health Service number. Hospitals were linked to the East Norfolk Health Authority database, which identifies all hospital contacts throughout England and Wales for Norfolk residents. Vital status for all EPIC-Norfolk participants was obtained through death certification at the Office for National Statistics, and death certification with coding for diabetes was identified. Previous validation studies in this cohort using capture–recapture analysis indicated that the use of multiple sources of ascertainment information for diabetes detected 99% of incident cases when comparing with diagnostic information from a comprehensive review of medical records (18).
Statistical analyses
In 5,735 participants free of diabetes at baseline with data on HbA1c for the baseline and second health assessments, we calculated the incidence of diabetes defined clinically and by using HbA1c diagnostic criteria in the whole cohort and separately for different categories of baseline HbA1c. Baseline characteristics were summarized for groups defined by different categories of baseline HbA1c (<5.0, 5.0–5.4, 5.5–5.9, and 6.0–6.4%). We tested for differences between groups using the χ2 test for categoric variables and ANOVA or Kruskal-Wallis tests for normally or nonnormally distributed continuous variables, respectively.
We used logistic regression to estimate the risk of developing diabetes as measured by the odds ratios (ORs) for every 0.5% increase in HbA1c as well as for different categories of HbA1c compared with the lowest HbA1c category of <5.0%. We examined ORs adjusted for age only, age and sex only, and multiple risk factors, including age, sex, self-reported family history of diabetes, smoking, the use of antihypertensive drugs or corticosteroids, BMI, waist circumference, systolic blood pressure, and total cholesterol, HDL cholesterol, and triglyceride values. To inform alternative screening strategies, we investigated risk factors associated with incident diabetes in those with a baseline HbA1c of <6.0%.
We also performed a sensitivity analysis using a more restricted definition of incident diabetes in which participants were not classified as having incident diabetes unless a self-reported diagnosis was supported by information on diabetes-specific medication or confirmed by information from clinical records, death certificates, or HbA1c.
RESULTS
Table 1 summarizes baseline characteristics of participants in the EPIC-Norfolk cohort by different HbA1c categories. Participants (45% men) had a mean age of 57.4 (SD 9.4) years. Participants with a higher HbA1c value were older, more likely to be male, obese, current smokers, and to come from a lower socioeconomic class than those with a lower HbA1c value. They were also more likely to have higher blood pressure, higher total cholesterol and triglyceride values, and lower HDL cholesterol values. There was no difference in family history of diabetes and the use of corticosteroids among the groups.
Table 1.
Comparison of baseline characteristics across categories of baseline HbA1c in 5,735 participants in the EPIC-Norfolk cohort
| Variable | Total | HbA1c level |
P for difference* | |||
|---|---|---|---|---|---|---|
| <5.0% | 5.0–5.4% | 5.5–5.9% | 6.0–6.4% | |||
| N (%) | 5,735 (100) | 1,849 (32.2) | 2,119 (36.9) | 1,397 (24.4) | 370 (6.5) | |
| Age (years) | 57.4 (9.4) | 54.1 (9.2) | 57.4 (9.1) | 60.3 (8.7) | 62.4 (8.2) | <0.001 |
| Men, n (%) | 2,481 (43.3) | 746 (40.4) | 932 (44.0) | 634 (45.4) | 169 (45.7) | 0.016 |
| Social class,†n (%) | <0.001 | |||||
| Class I–IIIa | 3,694 (64.4) | 1,255 (67.9) | 1,358 (64.1) | 861 (61.6) | 220 (59.5) | |
| Class IIIb–V | 2,041 (35.6) | 594 (32.1) | 761 (35.9) | 536 (38.4) | 150 (40.5) | |
| Current smokers, n (%) | 525 (9.2) | 141 (7.6) | 165 (7.8) | 165 (11.8) | 54 (14.6) | <0.001 |
| Family history of diabetes, n (%) | 697 (12.2) | 217 (11.7) | 250 (11.8) | 177 (12.7) | 53 (14.3) | 0.469 |
| Medication use, n (%) | ||||||
| Corticosteroids | 156 (2.7) | 44 (2.4) | 61 (2.9) | 37 (2.7) | 14 (3.8) | 0.454 |
| Antihypertensive drugs | 811 (14.1) | 188 (10.2) | 301 (14.2) | 243 (17.4) | 79 (21.4) | <0.001 |
| BMI (kg/m2) | 25.9 (3.7) | 25.4 (3.5) | 25.9 (3.6) | 26.3 (3.8) | 26.6 (4.0) | <0.001 |
| BMI category, n (%) | <0.001 | |||||
| <25 kg/m2 | 2,528 (44.1) | 935 (50.6) | 906 (42.8) | 553 (39.6) | 134 (36.2) | |
| 25–29.9 kg/m2 | 25,24 (44.0) | 738 (39.9) | 956 (45.1) | 657 (47.0) | 173 (46.8) | |
| ≥30 kg/m2 | 683 (11.9) | 176 (9.5) | 257 (12.1) | 187 (13.4) | 63 (17.0) | |
| Waist circumference, cm | 86.9 (12.2) | 84.8 (12.2) | 87.1 (11.9) | 88.6 (11.9) | 90.0 (13.0) | <0.001 |
| Systolic blood pressure, mmHg | 133.4 (17.5) | 130.6 (17.1) | 133.4 (17.1) | 135.7 (18.1) | 138.9 (17.3) | <0.001 |
| Diastolic blood pressure, mmHg | 82.0 (10.8) | 80.9 (10.6) | 82.1 (10.8) | 82.9 (11.1) | 84.1 (10.9) | <0.001 |
| Total cholesterol, mmol/L | 6.1 (1.1) | 5.8 (1.1) | 6.1 (1.1) | 6.3 (1.1) | 6.4 (1.2) | <0.001 |
| HDL cholesterol, mmol/L | 1.5 (0.4) | 1.5 (0.4) | 1.5 (0.4) | 1.4 (0.4) | 1.4 (0.4) | 0.001 |
| TG, median (IQR), mmol/L | 1.4 (1.0–2.1) | 1.3 (0.9–1.8) | 1.5 (1.0–2.1) | 1.6 (1.1–2.2) | 1.7 (1.2–2.5) | <0.001 |
Data are presented as the mean (SD), unless specified otherwise.
IQR, interquartile range; TG, triglyceride.
*Differences between groups using χ2 tests for categoric variables, and ANOVA or Kruskal-Wallis tests for normally or nonnormally distributed continuous variables.
†Registrar General's Social Class: class I = professional, etc. occupations; II = managerial and technical occupations; IIIa = skilled occupations (nonmanual); IIIb = skilled occupations (manual); IV = partly-skilled occupations; V = unskilled occupations.
Prevalence of diabetes at baseline
Among 6,372 individuals with HbA1c measurements at both health assessments, 302 (4.7%) had prevalent diabetes at baseline (Fig. 1). Among these individuals, 178 (2.8%) had known diabetes (those identified clinically), and 124 (1.9%) had previously undiagnosed diabetes (those identified using HbA1c criteria).
Incidence of diabetes over 3 years
Among 5,735 participants free of diabetes at baseline, 72 developed diabetes over 3 years (Fig. 1). The cumulative incidence was 1.3% (95% CI 1.0–1.5) over 3 years, an annual incidence of 0.4%. Among these new cases of diabetes, 37 individuals (51%) were identified clinically (e.g., by their response to the questionnaire at the second health check or through linkage to clinical records or diabetes registers), with an incidence of 0.6% (0.4–0.9). The remaining 35 individuals (49%) with incident diabetes were identified by their HbA1c results at the second health assessment.
Risk of developing diabetes in groups defined by different HbA1c levels
Table 2 reports the incidence of diabetes by baseline HbA1c levels for clinical diagnosis only and for clinical or HbA1c-defined diagnosis, or both. The incidence of diabetes increased progressively with increasing baseline HbA1c levels. In those with a baseline HbA1c of 6.0–6.4%, the incidence of clinically diagnosed or HbA1c-defined diabetes was three times higher than that of clinically diagnosed diabetes, at 7.0 (95% CI 4.8–10.1) and 2.4 (1.3–4.6), respectively. Thirty-six percent of incident cases of diabetes arose from individuals with a baseline HbA1c of 6.0–6.4% (6% of the total population), and just over 35% of incident cases arose among individuals with a baseline HbA1c of <5.5% (69% of the total population).
Table 2.
Incidence and risk (OR) of diabetes over 3 years by baseline HbA1c categories in the EPIC-Norfolk cohort (N = 5,735)
| Variable | Total | HbA1c level |
P for trend | |||
|---|---|---|---|---|---|---|
| <5.0% | 5.0–5.4% | 5.5–5.9% | 6.0–6.4% | |||
| Clinically diagnosed diabetes | ||||||
| N (% of total participants) | 5,735 | 1,849 (32) | 2,119 (37) | 1,397 (24) | 370 (6) | — |
| Incident cases (% of total cases) | 37 | 7 (19) | 6 (16) | 15 (41) | 9 (24) | — |
| Three-year cumulative incidence, % | 0.6 (0.4–0.9) | 0.4 (0.2–0.8) | 0.3 (0.1–0.6) | 1.1 (0.6–1.8) | 2.4 (1.3–4.6) | — |
| Unadjusted OR | 1.0 | 0.7 (0.3–2.2) | 2.9 (1.2–7.0) | 6.6 (2.4–17.7) | <0.001 | |
| Age-adjusted OR | 1.0 | 0.8 (0.3–2.4) | 3.3 (1.3–8.4) | 8.0 (2.8–22.7) | <0.001 | |
| Age- and sex-adjusted OR | 1.0 | 0.8 (0.3–2.4) | 3.3 (1.3–8.3) | 7.9 (2.8–22.4) | <0.001 | |
| Multivariable-adjusted OR* | 1.0 | 0.8 (0.3–2.3) | 3.0 (1.2–7.8) | 6.8 (2.3–20.1) | <0.001 | |
| Clinically diagnosed and/or HbA1c-defined diabetes | ||||||
| N (% of total participants) | 5,735 | 1,849 (32) | 2,119 (37) | 1,397 (24) | 370 (6) | — |
| Incident cases (% of total cases) | 72 | 9 (13) | 16 (22) | 21 (29) | 26 (36) | — |
| Three-year cumulative incidence, % | 1.3 (1.0–1.5) | 0.5 (0.3–0.9) | 0.8 (0.5–1.2) | 1.5 (1.0–2.3) | 7.0 (4.8–10.1) | — |
| Unadjusted OR | 1.0 | 1.6 (0.7–3.5) | 3.1 (1.4–6.8) | 15.5 (7.2–33.3) | <0.001 | |
| Age-adjusted OR | 1.0 | 1.6 (0.7–3.8) | 3.5 (1.6–7.8) | 18.0 (8.1–40.0) | <0.001 | |
| Age- and sex-adjusted OR | 1.0 | 1.6 (0.7–3.7) | 3.4 (1.5–7.7) | 17.7 (8.0–39.5) | <0.001 | |
| Multivariable-adjusted OR* | 1.0 | 1.6 (0.7–3.6) | 3.3 (1.5–7.4) | 15.6 (6.9–35.7) | <0.001 | |
*Adjusted for age, sex, social class, self-reported family history of diabetes, smoking, use of corticosteroids and antihypertensive drugs, BMI, waist circumference, systolic blood pressure, cholesterol, HDL cholesterol, and triglyceride.
Significant positive associations were found between HbA1c and the risk of developing diabetes (Table 2). A 0.5% increase in baseline HbA1c was associated with more than a twofold increase in the risk of clinically diagnosed or HbA1c-defined diabetes, or both (age-adjusted OR 2.7 [95% CI 2.1–3.5]). Participants with a baseline HbA1c of 6.0–6.4% had about a sevenfold higher risk of clinically diagnosed diabetes than those with an HbA1c of <5.0%. The highest risk of clinically diagnosed or HbA1c-defined diabetes was observed in the highest baseline HbA1c category compared with those with a baseline HbA1c of <5.0% (OR 15.5 [7.2–33.3]). These ORs remained unchanged after adjustment for other risk factors.
Among individuals with a baseline HbA1c <6.0%, a family history of diabetes and waist circumference were the strongest nonlaboratory predictors of incident diabetes over 3 years.
In the sensitivity analysis using a more restricted definition of incident diabetes, 59 individuals developed diabetes (Supplementary Table 1). The incidence was 1.0 (95% CI 0.8–1.3) over 3 years, an annual incidence of 0.3%. Incident cases in 37 individuals (63%) were identified using HbA1c diagnostic criteria. Approximately 40% of incident cases of diabetes developed in individuals with a high baseline HbA1c of 6.0–6.4% (6% of total population). A 27-fold higher risk of diabetes was observed in those with a baseline HbA1c of 6.0–6.4% compared with those with a baseline HbA1c of <5.0%.
CONCLUSIONS
We used data from a large population-based British prospective cohort to estimate the prevalence and incidence of diabetes defined clinically or by HbA1c, or both, over 3 years. The HbA1c diagnostic threshold of 6.5% identified 50% of new cases. The incidence of diabetes increased progressively across baseline HbA1c levels, with 36% of incident cases developing in individuals with a baseline HbA1c of 6.0–6.4%.
To the best of our knowledge, this study is the first to report the incidence of diabetes based on HbA1c diagnostic criteria using repeated assessment of HbA1c. Our prevalence estimate is comparable with the prevalence of diabetes in England (4.4%) estimated from an epidemiologic model in which individuals with known and previously undiagnosed diabetes were included (19). We also found that approximately 40% of prevalent cases were identified using HbA1c diagnostic criteria and, hence, were previously undiagnosed. This is consistent with previous studies using an OGTT as a screening test (20).
A number of studies have estimated diabetes incidence by using longitudinal repeat OGTT or fasting plasma glucose measurements (15,16). The incidence of diabetes in these studies varied from 6 to 10% over 9 to 10 years. Data from a British population in Ely, Cambridgeshire, showed that the cumulative incidence of diabetes using repeat OGTT measurements was 5.9% over 10 years, corresponding to an annual incidence of 0.6% (16). This is comparable with the low annual incidence of 0.4% in the current study. The higher incidence in the earlier study may be explained by enhanced case detection from repeated testing by OGTT over a longer period (OGTT testing at baseline, 4.5, and 10 years in the earlier Ely study vs. HbA1c at baseline and after 3 years of follow-up in the EPIC-Norfolk study) and the different contributions of the “healthy volunteer effect” in each study (response rates of 74% in the Ely study and 33% in the EPIC-Norfolk study).
Few studies have examined the incidence and relative risk of diabetes in individuals or groups defined by different baseline HbA1c levels. Selvin et al. (21) examined the incidence of self-reported diabetes in American men and women with different baseline HbA1c values. The 15-year cumulative incidence of diabetes was 6, 12, 21, and 44% in individuals with an HbA1c of <5.0, 5.0–5.4, 5.5–5.9, and 6.0–6.4%, respectively. The estimated annual incidence was higher than those observed across all HbA1c categories in our study. This might be explained by the differences in levels of other risk factors (higher BMI, smoking, and family history of diabetes in the Selvin study), follow-up time (15 vs. 3 years, if incidence rates are not consistent across different durations of follow-up), and in particular, the different definitions of diabetes used in each study.
HbA1c has been shown to be a useful tool for the early detection of diabetes (21). A few studies have demonstrated that HbA1c predicts future risk of diabetes in high-risk individuals with glucose intolerance (22). We have shown that HbA1c predicts risk of diabetes in healthy middle-aged men and women. An HbA1c of 6.0–6.4% identified 24% of clinically incident diabetes, and 36% of clinically incident or HbA1c-defined diabetes. These figures were even higher when a more restricted definition of incident diabetes was used. Recent evidence shows that this predictive ability also holds true in low-risk nondiabetic men and women (21) and in elderly individuals (23). However, given that the associations between HbA1c and the risk of diabetes were hardly changed after adjustment for multiple risk factors, there may not be much to gain from including data on multiple risk factors alongside HbA1c for prediction of diabetes risk.
ADA suggested that there was no specific threshold that defines individuals who might be offered preventive interventions and that any such threshold would vary between countries with different heath care priorities (12). However, ADA suggested that individuals with an HbA1c between 6.0 and 6.4% might represent a group in whom the risk of development of diabetes was very high and who could therefore be targeted for individual prevention interventions (12). ADA also suggested that this range should not be considered an absolute threshold and that interventions may be appropriate in other individuals on the basis of other risk information. Our findings support this statement by demonstrating that most new cases of diabetes developed in those with a baseline HbA1c of <6.0%.
The selection of a population for a high-risk prevention strategy is by the level of risk identified, the proportion of the population to be targeted, and the proportion of future cases that might therefore be prevented. Our study showed that 36% of new cases of diabetes arose from the 6% of the study population who had the highest glycemic levels (HbA1c 6.0–6.4%). Indeed, if previously proven intensive prevention interventions (2,3) were targeted at this middle-aged population, approximately 20% of new cases of diabetes could be prevented over 3 years. Strategies for identifying which individuals should have an HbA1c measurement, including simple risk scores using easily measured or routinely available risk factors, are needed.
Although the category of people with an HbA1c of 6.0–6.4% identifies a high-risk group, most new cases of diabetes developed in individuals whose baseline HbA1c values were <6%. Complementary strategies to identify high-risk individuals among those without raised HbA1c may therefore be necessary. Our subgroup analysis in individuals with an HbA1c of <6.0% suggested that those with central obesity and a family history of diabetes might represent another relatively easily identifiable subgroup to whom preventive interventions could be targeted. This also suggests that in addition to high-risk approaches, we need to develop a complementary population-based strategy aimed at shifting the whole distribution of HbA1c in the population to reduce the risk of both diabetes and its complications (24). However, although there is some evidence for the cost-effectiveness of prevention interventions among high risk individuals (25), evidence on the cost-effectiveness of population-based strategies is very limited, making judgments about the balance of investment in high-risk and population-based approaches difficult.
We have reported the incidence of diabetes in a large prospective British cohort using clinical ascertainment and newly proposed HbA1c diagnostic criteria. Participants included in this analysis were healthier than those excluded; hence, our findings are likely to underestimate the incidence of diabetes in the whole cohort. Given the 33% recruitment rate in this study, it is possible that participants might be more health-conscious and more likely to engage in healthy behaviors and to take up existing preventive services compared with nonparticipants. We might therefore have underestimated the overall incidence of diabetes in the population, which might consequently influence estimates of the relative risk for HbA1c.
Because the EPIC-Norfolk study collected nonfasting blood samples, it is not possible to compare the predictive ability for incident diabetes of different measures of glycemia. Similar to other diagnostic tests, the use of a single measure of HbA1c for diagnosing diabetes might lead to some degree of misclassification. However, given that HbA1c is more reliable compared with an OGTT and the fasting plasma glucose test, the misclassification is likely to be only modest. A relatively short follow-up period and relatively small number of events mean that our finding should be interpreted with caution. However, our study is one of the largest incidence studies reported.
Furthermore, the follow-up of 3 years is still a plausible and important timeframe for identifying those at high risk of diabetes, because in addition to long-term risk information, one might also be interested in and more persuaded for behavior modification by information on the short-term risk of diabetes. Our findings were specific to a population aged 40–74 years, and may not represent the burden and risk of diabetes in relation to HbA1c levels in younger people. Lastly, most of the EPIC-Norfolk participants are of European descent, which limits the generalizability of our findings to other ethnic groups and populations.
In conclusion, the cumulative incidence of diabetes defined using a newly proposed HbA1c threshold in this middle-aged British cohort was 1.3% over 3 years (0.4% per year). HbA1c independently predicted the risk of incident diabetes, with each 0.5% difference in HbA1c being associated with more than doubling of the risk of diabetes. Because 36% of incident cases of diabetes came from the 6% of the population with a baseline HbA1c of between 6 and 6.5%, this may be an easily identifiable subgroup to whom preventive interventions could be targeted. Alternative strategies to identify high-risk individuals may be necessary, however, and complementary population-based approaches need to be developed to shift the underlying distribution of glycemia.
Supplementary Material
Acknowledgments
Funding support was provided by the Medical Research Council, Cancer Research UK, British Heart Foundation, European Union (Europe Against Cancer Programme), Stroke Association, Wellcome Trust, Research into Ageing, and Academy of Medical Science. P.C. is supported by a Royal Thai Government scholarship. S.J.G. receives support from the National Institute for Health Research programme grant funding scheme (RP-PG-0606-1259). The views expressed in this publication are those of the authors and not necessarily those of the NHS, National Institute for Health Research, or Department of Health. The sponsors did not participate in the design or conduct of this study; in the collection, management, analysis, or interpretation of data; in the writing of the manuscript; or in the preparation, review, approval, or decision to submit this manuscript for publication.
No potential conflicts of interest relevant to this article were reported.
P.C. researched data, contributed to discussion, wrote the manuscript, and reviewed and edited the manuscript. R.K.S., N.G.F., and R.N.L. researched data, contributed to discussion, and reviewed and edited the manuscript. K.-T.K. researched data and reviewed and edited the manuscript. N.J.W. and S.J.G. researched data, contributed to discussion, and reviewed and edited the manuscript.
Parts of this study were presented at the 45th Annual Meeting of the European Diabetes Epidemiology Group, Porto Heli, Greece, 15–18 May 2010.
The authors thank the EPIC-Norfolk participants and the EPIC-Norfolk team for their contributions.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc09-2326/-/DC1.
References
- 1.International Diabetes Federation The Diabetes Atlas. 4th ed. Brussels, International Diabetes Federation, 2009 [Google Scholar]
- 2.Tuomilehto J, Lindström J, Eriksson JG, et al. Finnish Diabetes Prevention Study Group Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–1350 [DOI] [PubMed] [Google Scholar]
- 3.Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008;371:1783–1789 [DOI] [PubMed] [Google Scholar]
- 5.Ruge T, Nyström L, Lindahl B, et al. Recruiting high-risk individuals to a diabetes prevention program: how hard can it be? Diabetes Care 2007;30:e61. [DOI] [PubMed] [Google Scholar]
- 6.Ko GT, Chan JC, Woo J, et al. The reproducibility and usefulness of the oral glucose tolerance test in screening for diabetes and other cardiovascular risk factors. Ann Clin Biochem 1998;35:62–67 [DOI] [PubMed] [Google Scholar]
- 7.Colagiuri S, Borch-Johnsen K, Wareham NJ. Back to the future—do IGT and IFG have value as clinical entities? Diabetes Res Clin Pract 2008;81:131–133 [DOI] [PubMed] [Google Scholar]
- 8.Nathan DM, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia 2007;50:2239–2244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sabanayagam C, Liew G, Tai ES, et al. Relationship between glycated haemoglobin and microvascular complications: is there a natural cut-off point for the diagnosis of diabetes? Diabetologia 2009;52:1279–1289 [DOI] [PubMed] [Google Scholar]
- 10.Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med 2004;141:413–420 [DOI] [PubMed] [Google Scholar]
- 11.Kahn R, Fonseca V. Translating the A1C Assay. Diabetes Care 2008;31:1704–1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl. 1):S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Söderberg S, Zimmet P, Tuomilehto J, et al. High incidence of type 2 diabetes and increasing conversion rates from impaired fasting glucose and impaired glucose tolerance to diabetes in Mauritius. J Intern Med 2004;256:37–47 [DOI] [PubMed] [Google Scholar]
- 14.Geiss LS, Pan L, Cadwell B, Gregg EW, Benjamin SM, Engelgau MM. Changes in incidence of diabetes in U.S. adults, 1997-2003. Am J Prev Med 2006;30:371–377 [DOI] [PubMed] [Google Scholar]
- 15.Bonora E, Kiechl S, Willeit J, et al. Bruneck study Population-based incidence rates and risk factors for type 2 diabetes in white individuals: the Bruneck study. Diabetes 2004;53:1782–1789 [DOI] [PubMed] [Google Scholar]
- 16.Forouhi NG, Luan J, Hennings S, Wareham NJ. Incidence of Type 2 diabetes in England and its association with baseline impaired fasting glucose: the Ely study 1990-2000. Diabet Med 2007;24:200–207 [DOI] [PubMed] [Google Scholar]
- 17.Day N, Oakes S, Luben R, et al. EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer 1999;80(Suppl. 1):95–103 [PubMed] [Google Scholar]
- 18.Harding AH, Day NE, Khaw KT, et al. Dietary fat and the risk of clinical type 2 diabetes: the European prospective investigation of Cancer-Norfolk study. Am J Epidemiol 2004;159:73–82 [DOI] [PubMed] [Google Scholar]
- 19.Forouhi NG, Merrick D, Goyder E, et al. Diabetes prevalence in England, 2001—estimates from an epidemiological model. Diabet Med 2006;23:189–197 [DOI] [PubMed] [Google Scholar]
- 20.King H, Rewers M, WHO Ad Hoc Diabetes Reporting Group Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. Diabetes Care 1993;16:157–177 [DOI] [PubMed] [Google Scholar]
- 21.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Little RR, England JD, Wiedmeyer HM, et al. Glycated haemoglobin predicts progression to diabetes mellitus in Pima Indians with impaired glucose tolerance. Diabetologia 1994;37:252–256 [DOI] [PubMed] [Google Scholar]
- 23.Motta M, Bennati E, Cardillo E, Ferlito L, Malaguarnera M. The value of glycosylated hemoglobin (HbA1c) as a predictive risk factor in the diagnosis of diabetes mellitus (DM) in the elderly. Arch Gerontol Geriatr 2010;50:60–64 [DOI] [PubMed] [Google Scholar]
- 24.Simmons RK, Griffin SJ, Wareham NJ. Researching how to realize the potential of diabetes prevention. Diabet Med 2007;24:1055–1057 [DOI] [PubMed] [Google Scholar]
- 25.Herman WH, Hoerger TJ, Brandle M, et al. Diabetes Prevention Program Research Group The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 2005;142:323–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.